Abstract
Background
Port-site and connecting tube complications are usually considered minor problems in the follow-up of obese patients submitted to laparoscopic adjustable gastric banding (LAGB), but the incidence reported in literature ranges from 4.3% to 24%. These complications are mainly because of the mechanical stress of the port and the tube; therefore, their incidence might be time dependent and probably increase during the follow-up.
Methods
We evaluated retrospectively 489 obese patients submitted to LAGB from February 1998 to December 2005, considering all the complications of the connecting tube and port. Their clinical signs, imaging exams, operative reports, and hospitalization files were evaluated.
Results
The mean follow-up of the patients was 41 months. Seventy-one patients (14.5%) presented port and connecting tube complications that required 82 revisional operations. Fifty-four patients had system leaks, 3 had infection problems, and 14 mechanical problems, always requiring surgical revision. In five patients, the system leak was observed twice and required a second surgical repair, while one patient presented three times a leakage of the connecting tube and needed three surgical revisions. All cases of system leakage were related to significant weight regain. In one case of recurrent port infection, we had to remove the band.
Conclusion
Port-site and connecting tube problems are the most common complications after LAGB. Although they are considered marginal complications, they usually cause weight regain; their correction often requires surgical revision and sometimes removal of the band.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Morbid obesity is an increasing problem in Europe and North America and correlates with a high incidence of comorbidities like hypertension, cardiovascular diseases, diabetes, pulmonary diseases, and arthropathy. Laparoscopic adjustable gastric banding (LAGB) is considered an effective treatment for morbid obesity, showing a lower incidence of complications and mortality in comparison with malabsorbitive procedures [1]; it can be easily done in laparoscopy, is easily reversible, and does not require significant surgical modifications of the gastrointestinal tract.
Although the results of LAGB are related to the compliance of the patient, its complications are rather related to the presence of the device, which can be divided between the inflatable balloon of the band and the port with the connecting tube. Band problems (intragastric migration or slippage) are classified as major complications, while port or tube problems (leakage, infection of the port-site, mechanical port problems) are classified as minor complications. The leakage of the system (tube breakage or disconnection) causes weight regain, while port-site infection requires port removal: Both situations lead therefore to failure of LAGB [2].
The incidence of these complications ranges between 4.3% and 24% [2–4]. We observed these complications in a series of our patients, and their incidence, diagnosis, and treatment are discussed.
Patients and Methods
Four hundred eighty-nine obese patients were submitted to LAGB between February 1998 and December 2005. There were 381 women (77.9%) and 108 men (22.1%); mean age was 43 years (range 18–65); mean body mass index (BMI) was 42.5 (range 35–75). In 483 patients, gastric banding was done laparoscopically and in 6 cases laparotomically for conversion from hepatosplenomegaly, intraoperative damage of the gastric wall with the perigastric technique, or adhesions. We followed strictly the 1991 National Institutes of Health Consensus guidelines for surgical indications. In 269 cases, we used the Heliogast® system (Helioscopie, Lyon, France) and in 220 cases the Lap-band® system (Allergan Medical, Irvine, Ca, USA).
After implantation of the band, according to the technique proposed by Belachew [5], the connecting tube is pulled out through the incisional site of the left upper trocar and is connected to the port with two different techniques:
-
In the Lap-band® system, the tube is secured to the port by means of an interposed metallic connector, with non-resorbable stitches on both ends. This metallic device is connected to the port with a short tube.
-
In the Heliogast® system, the tube is directly connected to the port and is covered by a small silicone device.
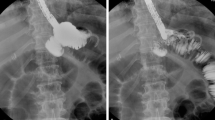
The system function is checked by filling the port with saline solution. All the ports are implanted in the left upper abdomen and firmly fixed to the fascia with three non-resorbable stitches, avoiding any abnormal kinking of the tube in the passage through the abdominal wall. The complications of the connecting tube or the port have been diagnosed either with echography, in case of port-site abscess (Fig. 1), or with X-ray exam. A complete disconnection of the tube can be easily recognized with a plain X-ray exam, while tube leaks can be evaluated by contrast injection in the port.
All data of the patients, including preoperative evaluation, peri-operative course, and long-term follow-up, were recorded in a database; all the patients who presented tube or port complications until August 2006 were considered in this study and reviewed retrospectively.
Results
The mean follow-up of the 489 patients is 41 months (8–95 months). Seventy-one patients (14.5%) presented tube or port complications that required revisional surgery; seven of them were operated twice, and two were operated three times. The mean time between LAGB and revisional surgery was 27.6 months (0–66 months), the mean decrease of BMI was 7.2 ± 4.5, and the mean weight loss was 17.2 ± 12.6 kg. The mean weight loss is less than the average weight loss of our casistic because most of these patients had weight regain. We observed the following complications:
-
System leak: Our most common complications are tube breakage or disconnection, which occurred in 54 cases (11%). They were observed once in 41 patients, twice in five patients, and three times in one patient, requiring 54 surgical revisions in local anesthesia (Table 1). In 47 cases, we observed a tube breakage close to the port or to the metallic connector, and in seven patients, the tube was completely disconnected from the port or from the rod that connects the tube with the port. Table 2 shows the incidence of these complications in relation to different bands (Lap-band® or Heliogast®): The statistical analysis showed no significance (p = 0.50 for breakage, p = 0.51 for disconnection, χ2 analysis). In five of seven cases of complete disconnection, the tube slipped in peritoneal cavity and was retrieved by laparoscopy. In all the other cases, the surgical repair was done in local anesthesia.
-
Port-site infection: We observed this complication in three patients, requiring seven surgical revisions (0.6%); in two cases, port infection followed a reductive abdominoplasty. The presenting symptoms were port-site inflammation or abscess and, in one case, an abscess fistulization to the skin. The patients were treated with surgical drainage and antibiotics, and a gastroscopy was done to exclude band erosion; then, we removed the port, leaving the tube inside the abdominal cavity. It was retrieved 3 months later by laparoscopy, and another port was connected and implanted in the left upper abdomen. This procedure was successful in two cases, but in the third patient, we observed the recurrence of infection, and we had to remove the band.
-
Port rotation: Occurred in seven patients (1.4%), and the diagnosis was confirmed by X-ray exam. This complication was commonly observed during band calibration for the impossibility to inject saline in the port, and its surgical repair was always done in local anesthesia. If port rotation appears early in the follow-up, it may be related to an incorrect port fixation: In one case, we observed port inversion on the first postoperative day during a radiological control. When it occurs later, after some band calibrations, it is probably the consequence of great weight loss that can change the anatomy of the abdominal wall. Port rotation also occurred after abdominoplasty.
-
Port prominence with skin erosion: Occurred in four cases (0.8%), presenting with progressive erosion of the skin above the port without signs of infection and with mild pain. We always observed this complication in patients who had massive weight loss, especially if the port was under the belt, and we replaced it with a pediatric port.
-
Tube kinking: Occurred in one case (0.2%) and presented with pain, induration in the port-site and problems with port injection. The diagnosis was done by contrast injection in the port, which showed an abnormal kinking of the connecting tube in the subcutaneous tissue around the port. The kinking caused the obstruction of the system and the impossibility to calibrate the band and required a surgical revision in local anesthesia.
-
Port-site hernia: Occurred once (0.2%); its symptoms were acute pain and induration in the port-site and was repaired in general anesthesia.
-
Small bowel obstruction by the connecting tube: This complication occurred in one patient (0.2%) who presented recurrent abdominal pain without nausea or vomiting. A plain abdominal X-ray showed a dilated jejunal loop with a small air-fluid level projected near the port site. An abdominal CT scan, realized with a three-dimensional post-processing algorithm, showed that the connecting tube made a loop around a jejunal tract that was consequently enlarged. A laparoscopy confirmed that the connecting tube produced the obstruction rotating and angulating the jejunal tract, inducing a recurrent volvolus. The site of the mechanical obstruction was in correspondence of the entrance of the connecting tube in the abdominal cavity. The tube and the port were repositioned, and the bowel obstruction was solved [11].
Discussion
Although port and connecting tube complications are more common than band complications, they are usually considered minor problems. We should anyway emphasize that tube leakage, the most frequent of these complications, causes a quick weight regain with consequent failure of the bariatric procedure [4]. According to Korenkov [6], the incidence of these complications reported in literature is just the tip of the iceberg, because most of them are related to the mechanical stress of the device and are therefore time dependent. Keidar [2] reports that the incidence of port and tube complications is related to the length of follow-up. The reported incidence ranges between 4.3% and 24% [2–4]; in our experience, with a mean follow-up of 41 months, the incidence was 14.5%.
The first aspect to discuss is the site of port implantation. Two sites are usually proposed: the pre-sternal area and the left upper abdomen, in the site of the left trocar. Korenkov [7] compared these two different sites and observed that the pre-sternal area is easier to puncture, but is associated with persistent pain and frequent complaints of port prominence. For this reason we prefer the left upper abdominal site, even if sometimes we need a radiologic guide during the first calibrations; we observed port prominence with skin erosion only in 4 patients with great weight loss, and we changed the port with a pediatric one.
The most frequent complication is system leakage (54 cases), because of tube breakage or disconnection, and its typical manifestation is weight regain. Leaks can be confirmed by contrast injection in the port, and X-ray exam can also show if the connecting tube is retained in the abdominal wall or is slipped in abdominal cavity [8]. A leak of the system should be suspected when there is a discrepancy between injected and aspirated saline in the port [9]. Leakage or disconnection always occur near the connection between the port and the tube. Szold [2] suggests to choose the site of port implantation aiming to prevent an abnormal angulation of the tube in the passage in the abdominal wall, thus reducing the mechanical stress at the connection between the tube and the port. We are getting used therefore to pass the tube through the abdominal wall in a different way: After removal of the left trocar, a dissecting laparoscopic forceps is inserted in the incisional site with lesser angulation, creating a new straight passage to pull out the tube (Fig. 2).
In the Heliogast® system, the tube is directly connected to the port and is covered by a small silicone device, so the tip of the connecting tube remains more frequently fixed in the abdominal wall, preventing its slippage in peritoneal cavity. In the Lap-band® system, the tube is secured to the port with an interposed metallic connector, which usually remains intra-abdominal; the metallic connector is not exposed to mechanical stress, for instance when the patient changes position, but the disconnected tube may slip in abdominal cavity. In 75% of our cases of disconnection with Lap-band®, the tube slipped in abdominal cavity and required laparoscopic repair, but we had a lower incidence of tube breakage. A statistical analysis between the incidence of tube breakage or disconnection of the bands did not show significance. We observed that the highest incidence occurs during the first 36 months after surgery, corresponding to the period of greatest weight loss (Fig. 3). The main reason is probably the anatomical change of the abdominal wall after massive weight loss. After 36 months port complications have a definitely lower incidence.
Port-site infection is caused either by contamination during band implant or during its calibration. Diagnosis is confirmed by ecography, but a gastroscopy should always be considered to rule out an intragastric band migration; moreover, there were cases of subphrenic abscess after port-site infection [2], and we had to remove a band for relapsing port-site infection. In two patients, it occurred after abdominoplasty, suggesting to avoid mobilizing the port during this operation.
Port rotation can occur early, for an incorrect implant of the port, or later, after one or more port injections for band calibration, probably as a consequence of massive weight loss that can change the anatomy of the abdominal wall. It occurred also after abdominoplasty, when this operation was done by surgeons without specific bariatric experience.
Tube kinking, port-site hernia, and small bowel obstruction caused by the connecting tube are rare complications that should always be considered in the presence of specific symptoms.
In summary, the incidence of tube and port complications after LAGB seems to be time related to the length of follow-up. There is a close correlation between the incidence of these complications and weight loss, probably because the changes of the abdominal wall because of massive weight loss can enhance the mechanical stress of the connecting tube and port; in our experience, the incidence is higher during the first 36 months after surgery, decreasing later but not disappearing. Although they are considered minor complications, they can lead to failure of the bariatric procedure, especially in case of port infection [10]. We can therefore make some recommendations to prevent these occurrences:
-
Carefully fix the port to the fascia, with at least three non-resorbable stitches
-
Give the least possible angulation to the tube in its passage in abdominal cavity, avoiding to pass it through the incisional trocar passage but creating a new straight passage, without tube kinking
-
Leave the port as far as possible from the entrance of the tube in peritoneum, to prevent its slippage in abdominal cavity.
References
Angrisani L, Furbetta F, Doldi SB, et al. Lap band adjustable gastric banding system. The Italian experience with 1863 patients operated in 6 years. Surg Endosc. 2003;17:409–12.
Keidar A, Carmon E, Szold A, Abu-Abeid S. Port complications following laparoscopic adjustable gastric banding for morbid obesity. Obes Surg. 2005:15;361–5.
Busetto L, Segato G, De Marchi F, et al. Outcome predictors in morbidly obese recipients of an adjustable gastric band. Obes Surg. 2003;12:83–92.
Szold A, Abu-Abeid S. Laparoscopic adjustable silicone gastric banding for morbid obesity: results and complications in 715 patients. Surg Endosc. 2002;16:230–3.
Belachew M, Legrand M, Vincent V, et al. Laparoscopic placement of adjustable silicone gastric band in the treatment of morbid obesity: how to do it. Obes Surg. 1995;5:66–70.
Korenkov M, Sauerland S, Yucel N, et al. Port function after laparoscopic adjustable gastric banding for morbid obesity. Obes Surg. 2003;17:1068–71.
Korenkov M, Kneist W, Heintz A, et al. Technical alternatives in laparoscopic placement of an adjustable gastric band: experience of two German university hospitals. Obes Surg. 2004;14:806–10.
Yoffe B, Sapojnikov S, Lebedev V, Goldblum C. Disconnection of port after laparoscopic gastric banding: causes and solution. Obes Surg. 2003;13:784–87.
Weiss H, Nehoda H, Labeck B, et al. Injection port complications after gastric banding: incidence, management and prevention. Obes Surg. 2003;10:259–62.
Chevallier J-M, Zinzindohoué F, Douard R, et al. Complications after laparoscopic adjustable gastric banding for morbid obesity: experience with 1.000 patients over 7 years. Obes Surg. 2004;14:407–14.
Zappa MA, Lattuada E, Mozzi E, Francese M, Antonini I, Radaelli S, Roviaro GC. An unusual complication of gastric banding: recurrent small bowel obstruction caused by the connecting tube. Obes Surg. 2006;16:939–41.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lattuada, E., Zappa, M.A., Mozzi, E. et al. Injection Port and Connecting Tube Complications after Laparoscopic Adjustable Gastric Banding. OBES SURG 20, 410–414 (2010). https://doi.org/10.1007/s11695-008-9561-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-008-9561-4