Abstract
An increasing number of studies suggest chemotherapy for breast cancer may be neurotoxic. Cross-sectional MRI diffusion tensor imaging (DTI) studies suggest a vulnerability of brain white matter to various chemotherapeutic regimens. Up till now, this was confirmed in one prospective DTI study: Deprez et al. (2012) showed a widespread decline in fractional anisotropy (FA) of breast cancer patients after chemotherapy consisting of 5-fluorouracil (5-FU), epirubicin and cyclophosphamide (FEC) +/− taxanes +/− endocrine treatment. Our aim was to evaluate whether similar detrimental effects on white matter integrity would be observed with the currently widely prescribed anthracycline-based chemotherapy for breast cancer (predominantly doxorubicin and cyclophosphamide +/− taxanes +/− endocrine treatment (=BC + SYST; n = 26) compared to no systemic treatment (BC; n = 23) and no-cancer controls (NC; n = 30). Assessment took place before and six months after chemotherapy, and matched intervals for the unexposed groups. DTI data were analyzed using voxel-based tract-based spatial statistics and region of interest (ROI) analysis. Voxel-based analysis did not show an effect of chemotherapy +/− endocrine treatment on white matter integrity. ROI analysis however indicated subtle detrimental effects of chemotherapy +/− endocrine treatment by showing a larger decline in WM integrity in the superior longitudinal fasciculus and corticospinal tract in BC + SYST than BC. Indications for relatively mild neurotoxicity in our study might be explained by patient characteristics and specific aspects of data analysis. The omission of 5-FU in current treatment regimens or the administration of doxorubicin instead of epirubicin is also discussed as an explanation for the observed effects.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cognitive problems frequently occur in breast cancer patients. They may persist into the survivorship period and have a negative impact on quality of life. Many neuropsychological studies show that adjuvant chemotherapy is associated with increased rates of cognitive impairment, while preclinical studies report neurotoxicity of many chemotherapeutic agents (Wefel et al. 2015). Endocrine treatment is another frequently prescribed type of adjuvant systemic treatment that might also contribute to cognitive problems, although few studies have specifically focused on its cognitive side effects (Schilder et al. 2010a, b; Zwart et al. 2015). Neuroimaging studies point to neural correlates of chemotherapy-induced cognitive impairment (Pomykala et al. 2013). Here we prospectively evaluate side effects of a widely used systemic treatment in breast cancer patients on brain white matter integrity with MRI diffusion tensor imaging (DTI). Patients received anthracycline-based chemotherapy +/− taxanes +/− endocrine treatment with tamoxifen.
Two commonly used DTI-derived indices for white matter injury are a decrease in fractional anisotropy (FA), a measure for the directionality of diffusion, and an increase in mean diffusivity (MD), which indexes the average amount of diffusion (Pierpaoli and Basser 1996). In a cross-sectional study Deprez et al. found lower FA and higher MD four months after 5-fluorouracil, epirubicine and cyclophosphamide +/− paclitaxel [abbreviated as FEC(−P)] chemotherapy (n = 17) compared to 10 BC patients not receiving chemotherapy (Deprez et al. 2011), with cognitively impaired patients showing more extensive white matter injury (lower FA values). Another cross-sectional study reported lower FA in the genu but not the splenium of the corpus callosum in 10 breast cancer patients with cognitive complaints almost two years after doxorubicin, cyclophosphamide +/− docetaxel [abbreviated as (T)AC] chemotherapy, compared to no-cancer controls (NC, n = 9) (Abraham et al. 2008a, b). Cross-sectional studies by our group showed that late effects of chemotherapy (≥ 10 years post treatment) depended on the type of regimen administered. Widespread reduced white matter integrity (lower FA/higher MD values) was found in patients randomized to high dose carpoplatin, thiothepa, cyclophosphamide after conventional-dose FEC treatment (FEC + CTC, n = 17) but not conventional-dose FEC chemotherapy (n = 20) compared to 15 BC patients exposed to radiotherapy only (De Ruiter et al. 2012; Stouten-Kemperman et al. 2014). Another study by our group showed no significant differences in FA/MD between 187 BC patients 20 years after exposure to cyclophosphamide, methotrexate and 5-fluorouracil (CMF) chemotherapy compared to 374 NCs (Koppelmans et al. 2014). However, longer time since treatment was associated with reduced global and focal white matter integrity (i.e., lower FA and higher MD) within the patient group, suggesting deterioration of white matter with accumulating time since treatment.
To date, only one prospective longitudinal study assessing white matter integrity in BC patients has been published (Deprez et al. 2012). A decrease in FA was observed that was widespread across brain white matter and included the corpus callosum and frontal, parietal and occipital tracts in 34 patients four months after FEC(−Docetaxel, abbreviated D) chemotherapy (half of the patients were using endocrine treatment). No significant changes in FA were found for the unexposed and NC groups (n = 16, n = 19, respectively). Moreover, decrease in FA was associated with a decline in attention and verbal memory, suggesting that changes in white matter microstructure underlie cognitive impairment after FEC(−D) chemotherapy.
In the present study we used a similar approach to investigate side effects of currently widely used anthracycline-based chemotherapeutic regimens, that are mainly based on doxorubicin instead of epirubicin, do not contain 5-FU and are sometimes combined with taxane treatment and followed by endocrine treatment. Twenty-six BC patients receiving anthracyclin-based adjuvant chemotherapy and in most cases endocrine treatment (BC + SYST) were compared to 30 women without cancer (NC) as well as to 23 BC patients not requiring systemic treatment (BC), to control for possible cancer-related effects. DTI was used to assess change in white matter integrity before and six months after chemotherapy. We hypothesized that patients receiving systemic treatment would show a decrease in white matter integrity compared to BC patients not requiring systemic treatment and compared to no-cancer controls and that this decrease would be associated with cognitive decline.
Materials and methods
Subjects
Participants were patients with BC, who were scheduled to receive adjuvant anthracycline-based chemotherapy with or without endocrine treatment (BC + SYST), or who did not require systemic treatment (BC), and age-matched no-cancer controls (NC). Subjects were eligible if they met the following criteria: female, under the age of 70 years, sufficient command of the Dutch language, no previous malignancies. Additionally, patients had to have a diagnosis of primary breast cancer, no distant metastases and no other treatment than surgery at the time of baseline assessment. Patients scheduled to receive trastuzumab following chemotherapy were not eligible because of the longer treatment duration and unknown cognitive side effects compared to patients receiving chemotherapy without trastuzumab. NCs were recruited via patients, as well as through advertisements in the participating hospitals. The study was approved by the Institutional Review Board of the Netherlands Cancer Institute, serving as the central ethical committee for all participating institutes. Written informed consent was obtained according to the declaration of Helsinki and following institutional guidelines. The study was conducted at the Academic Medical Center of the University of Amsterdam and the Spinoza Centre for Neuroimaging.
Procedures
Baseline data were collected after surgery but before the start of adjuvant treatment (T1). Follow-up assessments took place at approximately six months after the last cycle of chemotherapy for the BC + SYST group and at matched intervals for the BC and the NC group (T2). The assessment included the completion of questionnaires, multimodality MRI and a comprehensive neuropsychological test battery consisting of 18 test indices (see Menning et al. (2015) for a detailed description). Verbal IQ was estimated with the Dutch Adult Reading Test (NART) (Schmand et al. 1992).
The current report focusses on longitudinal DTI analyses. A decline in performance on the cognitive domains of attention and verbal memory was shown to be associated with a decline in white matter integrity in the study of Deprez et al. (Deprez et al. 2012). We therefore correlated performance in these cognitive domains with FA values. The attention domain included the following tests: Eriksen Flanker Test (Eriksen and Eriksen 1974), Visual Reaction Time Test (Alpherts and Aldenkamp 1994) and Digit Span of the WAIS-III (Wechsler 2000) and the verbal memory domain consisted of the Hopkins Verbal Learning Test-Revised (Benedict et al. 1998). More detailed analyses of cognitive performance are described in Menning et al. (2016). Results from other MRI modalities will be described elsewhere. Questionnaires were administered to assess patient-reported outcomes (PROs) on frequently experienced symptoms by cancer patients such as fatigue, emotional and cognitive changes: European Organization for Research and Treatment of Cancer (EORTC) Quality of Life Questionnaire C-30 (QLQ-C30) (Aaronson et al. 1993), Hopkins Symptom Checklist-25 (HSCL-25) (Hesbacher et al. 1980), Profile of Mood States (POMS) (Wald and Mellenbergh 1990), Perceived Stress Scale (PSS) (Cohen et al. 1983), Trauma Screening Questionnaire (TSQ) (Dekkers et al. 2010), Medical Outcomes Study - Cognitive Functioning Scale-revised (MOS-cog) (Stewart et al. 1992), Ten-Item Personality Inventory (TIPI) (Gosling et al. 2003). Next to the questionnaires administered at T1, the Impact of Events Scale (IES) was used to assess distress related to breast cancer at T2 (Weiss and Marmar 1997).
MRI data were acquired using a 3.0 Tesla Intera full-body MRI scanner (AMC Medical Center) and a 3.0 Tesla Achieva full-body MRI scanner (Spinoza Centre for Neuroimaging) (Philips Medical Systems, Best, The Netherlands). A SENSE 8-channel receiver head coil was used at both locations. DTI was acquired in 32 directions (TR/TE = 8136/94 ms, FOV 250 × 250 mm, 64 slices, voxel size 2.23 × 2.23 × 2.00 mm, b-value: 1000 s/mm2), covering the entire brain. Primary brain pathology was evaluated with a T1 weighted three-dimensional magnetization prepared rapid gradient echo (MPRAGE) scan (TR/TE = 6.6/3.0 ms, FOV 270 × 252, 170 slices, voxel size 1.05 × 1.05 × 1.20 mm). In addition, an axial fluid attenuated inversion recovery (FLAIR) scan (TR/TE/TI = 11,000/100/2600 ms, FOV 230 × 230 mm, 27 slices, voxel size 0.9 × 1.4 × 5.0 mm, slice gap 0.5 mm) was acquired to score white matter abnormalities with the visual rating score of Fazekas (range 0–3) (Fazekas et al. 1987). All ratings were performed by a neuroradiologist (L.R.) blind to the clinical data. The scan protocol also consisted of other MRI sequences that are not reported in this article.
Statistical analyses
Demographic and clinical variables, PROs and extracted DTI values were analyzed with SPSS 22 (IBM, Armonk, NY). We assessed differences between groups on PROs at T2 using univariate analysis of covariance (ANCOVA), adjusted for baseline. For these analyses, the critical alpha value was set at 0.01 two-sided. Significant overall group differences were followed by paired group comparisons. For DTI data fractional anisotropy (FA) and mean diffusivity (MD) were calculated. Eddy current induced morphing in our DTI data was corrected by a two-dimensional affine registration of the diffusion-weighted images to the average of four b0 images (Mangin et al. 2002). DTIfit within the FMRIB Diffusion Toolbox (FDT, part of FMRIBs Software Library (FSL) (Smith et al. 2006) was used to fit a diffusion tensor at each voxel. To perform voxel wise comparisons of DTI parameters on “skeletonized” data FA maps were nonlinearly registered to an FA template (FMRIB58_FA) and averaged, using tract-based spatial statistics (TBSS, part of FSL) (Smith et al. 2006). This mean FA map was thinned to create an FA skeleton. Each participant’s FA data were then projected onto the mean skeleton by searching perpendicularly from the skeleton for maximal FA values and were thresholded at FA > 0.2. Next, MD values from the same voxels were also mapped onto the skeleton. To analyze change in FA and MD values between T1 and T2, difference maps were calculated by subtracting a subject’s T1 map from the T2 map. The randomize program within FSL was then used to perform permutation-based nonparametric inference (5000 permutations) on the difference maps within a general linear model framework to investigate group differences in the white matter skeleton (voxel wise analysis) (Nichols and Holmes 2002). In addition, cross-sectional nonparametric analyses were performed for T1 and T2 separately. Age was included as a covariate in all DTI analyses given the well-known relation between age and DTI values. In addition, scan direction was taken into account because DTI scans for three subjects were acquired in the sagittal instead of transversal direction. Because data were collected on two scanners, scan location was taken into account for cross-sectional analyses. However, analyses showed that DTI values did not differ significantly between locations. Voxel-based analyses were considered statistically significant at a cluster level, FWE corrected threshold of p < .05.
Region of interest (ROI) analyses were performed by extracting mean FA and MD from the following white mater tracts: left and right corticospinal tract (CST), left and right superior longitudinal fasciculus (SLF) and the genu and splenium of the corpus callosum. SLF, genu and splenium were chosen based on previous DTI studies (Abraham et al. 2008a, b; Deprez et al. 2012) whereas we additionally selected the CST because previously reported effects of chemotherapy on white matter seem quite diffuse and not confined to white matter tracts intimately involved in cognitive function.
Repeated measures ANCOVAs, correcting for age and scan direction were then performed to assess Group x Time differences. Differences were considered statistically significant at a critical alpha of .01 two-sided. Correlations were calculated for mean DTI values across the white matter skeleton as well as the ROIs. Correlation analyses were only performed for variables for which significant differences were found or when a strong relationship was expected. Therefore, fatigue scores (EORTC QLQ-C30), symptoms of anxiety and depression (HSCL-25), perceived stress (PSS), and cognitive complaints (MOS-cog) were included. Additionally, correlations with time since treatment were calculated. Neuropsychological difference scores (T2-T1) of tests covering the domains of attention and verbal memory were used to calculate correlations with change in DTI values (T2-T1). Correlations were only calculated for patient groups, because lower variance in PRO scores in the NC group was expected.
Results
At T1, before the start of adjuvant treatment, 32 BC + SYST, 33 BC and 38 NC were included. Details about the recruitment are described in our previous report (Menning et al. 2015). At T2, six months post-chemotherapy, or at similar intervals for the BC and NC group, five NCs dropped out because of personal reasons including ‘illness in the family’ and ‘no time’. Our original study plan also involved an analysis to examine the contribution of endocrine therapy on cognition. Due to the unexpected large imbalance in hormonal treatment between and within the two breast cancer groups (BC + SYST, 71%; BC, 27%), this was not feasible. Therefore, we excluded nine BC patients to create a group not receiving any systemic treatment. At T2, four BC + SYSTs and one NC declined to undergo the MRI scans because they were too anxious. DTI data were missing for two BC + SYSTs, 1 BC and 2 NCs, resulting in a final sample of 26 BC + SYST, 23 BC and 30 NC.
Patient characteristics
No significant difference in age between groups was found. Estimated verbal IQ was higher in NCs compared to the patient groups, but this difference did not reach statistical significance (p = .101) (Table 1). Follow-up assessment for BC + SYST subjects took place at approximately 6.5 months after chemotherapy. The interval between T1 and T2 was not significantly different between groups, although the interval in the NC group was somewhat longer compared to the patient groups (p = .119) (Table 1). At T1, 38%, 52%, and 53% of the BC + SYST, BC, and NC subjects respectively, were postmenopausal. All premenopausal women in the BC + SYST group had become postmenopausal after treatment. The majority of patients (65%) received the TAC chemotherapeutic regimen (docetaxel, doxorubicin, cyclophosphamide).
We found significant group differences at T2 adjusted for T1 in physical functioning, fatigue (QLQ-C30) and cognitive complaints (Table 2). Post-hoc analyses demonstrated lower physical functioning in BC + SYST compared to NC (p = .003). Levels of fatigue were significantly higher in BC + SYST compared to BC (p = .001) and marginally higher compared to NC (p = .030). BC + SYST reported more cognitive complaints, as measured with the MOS-cog scale, compared to BC (p = .008) and marginally more complaints compared to NC (p = .012).
White matter macrostructure - FLAIR
FLAIR data at follow-up were excluded for one BC because of an artifact. No severe white matter abnormalities (Fazekas score 3) were identified. No significant group differences in white matter abnormalities were found at T1 (p = .276) or T2 (p = .170) (Table 3), although a clear shift from Fazekas score 0 to 1 was apparent in the patient groups that was absent in the NC group.
White matter microstructure - DTI
Overall, participants showed a decline in FA and an increase in MD at T2 compared to T1 in bilateral white matter tracts with voxel-wise analyses. These effects probably indicate an age-related decline in white matter integrity in approximately one year. No significant differences in change over time between BC + SYST and the other groups were found with voxel-based testing. A smaller increase in MD in BC compared to NC was found, but this did not reach significance.
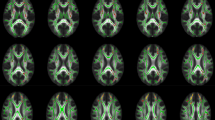
ROI analyses showed a significant decrease in FA in the right SLF (p = .01) and a subthreshold increase in MD in the right CST (p = .015) for BC + SYST vs. BC, both indicating stronger white matter decline in BC + SYST compared to BC (Table 4, Fig. 1). BC showed a smaller subthreshold decrease in FA values in the genu of the corpus callosum than NC (p = .014) (Table 4, Fig. 1). Also, BC showed a significant decrease in MD in the genu, while NCs showed an increase (p = .001) (Table 4, Fig. 1).
Mean FA and MD values from ROIs/ Error bars reflect standard error of the mean. SLF, superior longitudinal fasciculus; CST, corticospinal tract; BC + SYST, BC patients receiving systemic treatment; BC, BC patients not requiring systemic treatment; NC, no-cancer controls. aBC + SYST vs BC, bBC vs NC, *p < .01, **p < .05, corrected for age and scan direction
In line with our findings at T1 (Menning et al. 2015), cross-sectional voxel-based analyses at T2 showed widespread higher MD in BC + SYST and BC compared to NC and lower FA in BC compared to NC. Taken together these results are suggestive fore lower white matter integrity in the patient groups before as well as after treatment.
Correlations
No significant correlations between PROs or neuropsychological test scores and DTI values were found for the BC + SYST group. Also, time since chemotherapy was not significantly correlated with FA or MD. In the BC group, a decrease in the level of fatigue was associated with decreased mean MD across the skeleton (r = .526, p = .010; Fig. 2). Also, a decrease in cognitive complaints, indicated by an increase in scores on the MOS-cog, correlated with decreased MD across the skeleton as well as in the left SLF (r = −.673, p < .001; r = −.640, p = .001; Fig. 2) in the BC group.
Correlations of DTI values with patient-reported outcomes and neuropsychological test scores in the BC group. Values indicate change (T2-T1). SLF, superior longitudinal fasciculus. A positive change score for fatigue indicates higher levels of fatigue at T2 compared to T1. Positive change scores for cognitive complaints indicate less complaints at T2 compared to T1. Changes in MD refer to mean of white matter skeleton except for right panel
Discussion
This prospective study aimed at investigating potential side effects on brain white matter integrity of frequently used, anthracyclin-based adjuvant chemotherapy regimens like TAC for breast cancer patients, often followed by endocrine treatment. Using DTI measures, BC patients receiving systemic treatment (BC + SYST) were compared to BC patients not requiring chemotherapy (BC), and no-cancer controls (NC). Assessments took place before the start of adjuvant treatment and at approximately six months following chemotherapy, or at matched intervals for unexposed groups. Voxel-based analyses of group differences in white matter integrity did not reach significance but ROI analysis showed a larger decline in white matter integrity in BC + SYST in the right superior longitudinal fasciculus and corticospinal tract compared to BC. Further, BC + SYST reported worse physical functioning, higher levels of fatigue and more cognitive complaints compared to BC and NC. Voxel-based analysis of the white matter skeleton indicated a decline in white matter integrity for all groups, but not a stronger decline for the BC + SYST group relative to the BC and NC groups. We also did not find associations between cognitive decline and a decline in white matter integrity. We could therefore not replicate the findings of Deprez et al. (Deprez et al. 2012), who reported a widespread decline in white matter integrity at three to four months after treatment with the anthracyclin-based chemotherapy FEC(−D), and not in the BC or NC group.
Several factors might have contributed to the discrepancy in findings between our study and that of Deprez et al. Although the patients in both studies were comparable with respect to age and education, and both studies evaluated anthracycline-based regimens, the specific cytotoxic regimens in our study differed from the Deprez study. The only agent that was given to all patients both in our study and that of Deprez was cyclophosphamide. However, in our study the mean cumulative dose administered to patients was higher than in the Deprez study (2908 mg/m2 vs approximately 2400 mg/m2, personal communication), so this cannot explain the discrepancy. Taxane was part of chemotherapy in about 2/3 of the patients in both our and Deprez study. The taxane of choice was docetaxel in the Deprez study (not paclitaxel as reported, personal communication) and most of the times in our study as well. Mean cumulative dose was again higher in our study and therefore cannot explain the discrepancy between the studies. With respect to other agents, all chemotherapy-exposed patients in the Deprez et al. study received 5-FU whereas only three patients in the present study received 5-FU. This agent is known to cross the blood brain barrier by simple diffusion and has shown negative effects on brain white matter and cognitive function in rodents and humans (Akitake et al. 2011; Choi et al. 2001; Han et al. 2008; Israel et al. 2000; Seigers et al. 2015; Weng et al. 2014; Winocur et al. 2006). Further, the administered anthracyclins differed in the Deprez et al. study (epirubicin) and our study (mostly doxorubicin). Although not straightforward (Khasraw et al. 2012), epirubicin is possibly associated with more severe neurotoxicity to white matter than doxorubicin. In sum, on the level of treatment characteristics 5-FU administration seems the most likely explanation for the stronger effects on white matter integrity observed in the Deprez compared to our study, although the administration of epirubicin instead of doxorubicin could also have played a role.
Other factors might also explain the discrepancy between our findings and those of Deprez et al. The presently used chemotherapeutic regimens might not only be less neurotoxic to white matter but generally less neurotoxic than other regimens. In agreement with this notion is our finding of relatively low levels of cognitive decline in this sample (Menning et al., 2016): we found cognitive impairment for 16% of the BC + SYST at follow-up, compared to 4% in the BC group and 6% in the NC.
Second, our follow-up assessment after chemotherapy was somewhat longer than that in the Deprez et al. study (on average 142 days in the Deprez study vs. 201 days in our study), which may have led to smaller effects on white matter as measured with DTI. Third, the longer time interval between T1 and T2 in our study compared to that of Deprez et al. may have led to more age-related white matter decline in the participants which may have partially concealed detrimental effects of chemotherapy. These effects are consistent with normal brain aging (Barrick et al. 2010) and have been shown to coincide with age-related cognitive decline (Sullivan et al. 2010). Fourth, our statistics were performed on skeletonized white matter, which may be less sensitive because peripheral areas of white matter tracts are excluded from analysis (Bach et al. 2014). This might also explain why a previous study by our group did not find group differences in white matter integrity (Koppelmans et al. 2014). The purpose of skeletonization is to compensate for registration misalignment, restrict analysis to white matter, and gain statistical power by this dimensionality reduction (Smith et al. 2006). However, more accurate registration algorithms than those provided within the TBSS framework can decrease misalignment and render the skelotonization step unnecessary (Schwarz et al. 2014). Fifth, we used nonparametric analyses as opposed to Deprez et al. who used parametric analyses, which might have been less sensitive.
In contrast to our voxel-based findings, the ROI analyses did provide indications for chemotherapy-associated detrimental effects on white matter tracts supporting cognitive function, such as the superior longitudinal fasciculus. These effects were present when the BC + SYST group was compared to the unexposed BC group, but not the NC group. This might be explained as follows: as mentioned before, we found lower white matter integrity in BC patients compared to NC prior to systemic treatment (in the case of the BC + SYST group) (Menning et al. 2015). This lower white matter integrity might for instance be due to cancer-induced cytokine dysregulation or side-effects of anesthesia for breast surgery. At the second assessment white matter recovery might have occurred in the unexposed BC group, masking effects of normal aging that are present in the NC group. This white matter recovery was possibly suppressed by systemic treatment in the BC + SYST group. As a net result the BC + SYST group resembled the NC group whereas the BC showed less decline in white matter integrity. In agreement with this interpretation, white matter lesions have been reported to recover at least partially in e.g. stroke survivors (Fan et al. 2015) and after alcohol abstinence (Pfefferbaum et al. 2014). Thus far, no studies have assessed the course of changes in white matter after cancer treatment over a longer period of time. However, one study investigating brain grey matter in BC patients reported lower grey matter volume one month post chemotherapy, with partial recovery at one year after treatment (McDonald et al. 2010). The current results indicate that this increase in GM volume may be accompanied by recovery of white matter integrity as well.
The literature points to several mechanisms that may explain the observed subtle changes in patients. For example, these changes could be associated with inflammatory processes in the brain. DTI is usually considered a direct measure of microstructural integrity of myelin sheaths, but other factors besides demyelination have been suggested to affect DTI measures, including edema and inflammation (Assaf and Pasternak 2008). Pro-inflammatory cytokines, such as IL1, IL6, and TNFα, have previously been suggested to play a role in cognitive impairment in cancer patients (Cheung et al. 2013). These same pro-inflammatory cytokines have also been implied to influence DTI measures of white matter through changes in the endothelium of brain micro vessels, which can be assessed as white matter damage using MRI (Briones and Woods 2014). Possibly, altered levels of pro-inflammatory cytokines, triggered by cancer and cancer treatment, returned to normal over time,
Strengths of this study are the longitudinal design, the low attrition rate, and the inclusion of two control groups. Although voxel-based analyses of group differences in white matter integrity did not reach significance, both patient groups showed lower white matter integrity compared to NC. Also, BC + SYST showed a decline in white matter integrity in the SLF and CST compared to BC. Interestingly, BC patients who did not require systemic treatment showed recovery of white matter integrity compared to both BC + SYST and NC. By excluding the BC patients receiving endocrine treatment in the absence of chemotherapy, we can conclude that decline in white matter integrity in BC + SYST compared to BC is most likely due to systemic treatment. However, we were not able to disentangle the effects of chemotherapy and endocrine treatment.
Future studies should include a larger sample to increase power to detect subtle changes over time. In addition, effects of chemotherapeutic regimens should be directly compared to evaluate the specificity of effects for different regimens. In addition, the course of changes over time should be further investigated to determine whether decline continues or whether recovery takes place when time since treatment increases. Finally, the sensitivity of different post-processing and statistical approaches to detect (subtle) side effects of chemotherapy should be evaluated.
In conclusion, the results of this second prospective DTI study published in the field of breast cancer treatment and cognitive functioning suggest much less intense detrimental effects of adjuvant chemotherapy on brain white matter than previously reported. This might indicate that currently used regimens are less neurotoxic for brain white matter than older regimens, although this should be confirmed in future research.
References
Aaronson, N. K., Ahmedzai, S., Bergman, B., Bullinger, M., Cull, A., Duez, N. J., et al. (1993). The European Organization for Research and Treatment of cancer QLQ-C30: A quality-of-life instrument for use in international clinical trials in oncology. Journal of the National Cancer Institute, 85, 365–376. doi:10.1093/jnci/85.5.365.
Abraham, J., Haut, M. W., Moran, M. T., Filburn, S., Lemiuex, S., & Kuwabara, H. (2008a). Adjuvant chemotherapy for breast cancer: Effects on cerebral white matter seen in diffusion tensor imaging. Clinical Breast Cancer, 8(1), 88–91. doi:10.3816/CBC.2008.n.007.
Abraham, J., Haut, M. W., Moran, M. T., Filburn, S., Lemiuex, S., & Kuwabara, H. (2008b). Adjuvant chemotherapy for breast cancer: Effects on cerebral white matter seen in diffusion tensor imaging. Clinical Breast Cancer, 8(1), 88–91.
Akitake, R., Miyamoto, S., Nakamura, F., Horimatsu, T., Ezoe, Y., Muto, M., & Chiba, T. (2011). Early detection of 5-FU-induced acute leukoencephalopathy on diffusion-weighted MRI. Japanese Journal of Clinical Oncology, 41(1), 121–124. doi:10.1093/jjco/hyq157.
Alpherts, W., Aldenkamp, A. P. (1994). FePsy: The iron psyche. Heemstede.
Assaf, Y., & Pasternak, O. (2008). Diffusion tensor imaging (DTI)-based white matter mapping in brain research: A review. Journal of molecular neuroscience : MN, 34(1), 51–61. doi:10.1007/s12031-007-0029-0.
Bach, M., Laun, F. B., Leemans, A., Tax, C. M. W., Biessels, G. J., Stieltjes, B., & Maier-Hein, K. H. (2014). Methodological considerations on tract-based spatial statistics (TBSS). NeuroImage, 100, 358–369. doi:10.1016/j.neuroimage.2014.06.021.
Barrick, T. R., Charlton, R. A., Clark, C. A., & Markus, H. S. (2010). White matter structural decline in normal ageing: A prospective longitudinal study using tract-based spatial statistics. NeuroImage, 51(2), 565–577. doi:10.1016/j.neuroimage.2010.02.033.
Benedict, R. H. B., Schretlen, D., Groninger, L., & Brandt, J. (1998). Hopkins verbal learning test – Revised: Normative data and analysis of inter-form and test-retest reliability. The Clinical Neuropsychologist, 12, 43–55. doi:10.1076/clin.12.1.43.1726.
Briones, T. L., & Woods, J. (2014). Dysregulation in myelination mediated by persistent neuroinflammation: Possible mechanisms in chemotherapy-related cognitive impairment. Brain, Behavior, and Immunity, 35, 23–32. doi:10.1016/j.bbi.2013.07.175.
Cheung, Y. T., Lim, S. R., Ho, H. K., & Chan, A. (2013). Cytokines as mediators of chemotherapy-associated cognitive changes: Current evidence, limitations and directions for future research. PloS One, 8(12). doi:10.1371/journal.pone.0081234.
Choi, S. M., Lee, S. H., Yang, Y. S., Kim, B. C., Kim, M. K., & Cho, K. H. (2001). 5-fluorouracil-induced leukoencephalopathy in patients with breast cancer. Journal of Korean Medical Science. doi:10.3346/jkms.2001.16.3.328.
Cohen, S., Kamarck, T., & Mermelstein, R. (1983). A global measure of perceived stress. Journal of Health and Social Behavior, 24(4), 385–396.
De Ruiter, M. B., Reneman, L., Boogerd, W., Veltman, D. J., Caan, M., Douaud, G., et al. (2012). Late effects of high-dose adjuvant chemotherapy on white and gray matter in breast cancer survivors: Converging results from multimodal magnetic resonance imaging. Human Brain Mapping, 33(12), 2971–2983. doi:10.1002/hbm.21422.
Dekkers, A. M. M., Olff, M., & Näring, G. W. B. (2010). Identifying persons at risk for PTSD after trauma with TSQ in the Netherlands. Community Mental Health Journal, 46(1), 20–25. doi:10.1007/s10597-009-9195-6.
Deprez, S., Amant, F., Yigit, R., Porke, K., Verhoeven, J., Van den Stock, J., et al. (2011). Chemotherapy-induced structural changes in cerebral white matter and its correlation with impaired cognitive functioning in breast cancer patients. Human Brain Mapping, 32(3), 480–493. doi:10.1002/hbm.21033.
Deprez, S., Amant, F., Smeets, A., Peeters, R., Leemans, A., Van Hecke, W., et al. (2012). Longitudinal assessment of chemotherapy-induced structural changes in cerebral white matter and its correlation with impaired cognitive functioning. Journal of Clinical Oncology, 30(3), 274–281. doi:10.1200/JCO.2011.36.8571.
Eriksen, B. A., & Eriksen, C. W. (1974). Effects of noise letters upon the identification of a target letter in a nonsearch task. Perception & Psychophysics. doi:10.3758/BF03203267.
Fan, Y., Lin, K., Liu, H., Chen, Y., & Wu, C. (2015). Changes in structural integrity are correlated with motor and functional recovery after post-stroke rehabilitation. Restorative Neurology and Neuroscience, 33(6), 835–844. doi:10.3233/RNN-150523.
Fazekas, F., Chawluk, J. B., Alavi, A., Hurtig, H. I., & Zimmerman, R. A. (1987). MR signal abnormalities at 1. 5 T in Alzheimer ’ s dementia and normal aging deficiency. AJNR. American Journal of Neuroradiology, 149(August), 351–356. doi:10.2214/ajr.149.2.351.
Gosling, S. D., Rentfrow, P. J., & Swann, W. B. (2003). A very brief measure of the big-five personality domains. Journal of Research in Personality, 37, 504–528. doi:10.1016/S0092-6566(03)00046-1.
Han, R., Yang, Y. M., Dietrich, J., Luebke, A., Mayer-Pröschel, M., & Noble, M. (2008). Systemic 5-fluorouracil treatment causes a syndrome of delayed myelin destruction in the central nervous system. Journal of Biology, 7(4), 12. doi:10.1186/jbiol69.
Hesbacher, P. T., Rickels, K., Morris, R. J., Newman, H., & Rosenfeld, H. (1980). Psychiatric illness in family practice. The Journal of Clinical Psychiatry, 41(1), 6–10.
Israel, Z. H., Lossos, A., Barak, V., Soffer, D., & Siegal, T. (2000). Multifocal demyelinative leukoencephalopathy associated with 5-fluorouracil and levamisole. Acta Oncologica, 39(1), 117–120.
Khasraw, M., Bell, R., & Dang, C. (2012). Epirubicin: Is it like doxorubicin in breast cancer? A clinical review. Breast, 21(2), 142–149. doi:10.1016/j.breast.2011.12.012.
Koppelmans, V., de Groot, M., de Ruiter, M. B., Boogerd, W., Seynaeve, C., Vernooij, M. W., et al. (2014). Global and focal white matter integrity in breast cancer survivors 20 years after adjuvant chemotherapy. Human Brain Mapping, 35(3), 889–899. doi:10.1002/hbm.22221.
Mangin, J.-F., Poupon, C., Clark, C., Le Bihan, D., & Bloch, I. (2002). Distortion correction and robust tensor estimation for MR diffusion imaging. Medical Image Analysis, 6(3), 191–198.
McDonald, B. C., Conroy, S. K., Ahles, T. A., West, J. D., & Saykin, A. J. (2010). Gray matter reduction associated with systemic chemotherapy for breast cancer: A prospective MRI study. Breast Cancer Research and Treatment, 123(3), 819–828. doi:10.1007/s10549-010-1088-4.
Menning, S., de Ruiter, M., Veltman, D., Koppelmans, V., Kirschbaum, C., Boogerd, W., et al. (2015). Multimodal MRI and cognitive function in patients with breast cancer prior to adjuvant treatment - the role of fatigue. NeuroImage: Clinical, 7, 547–554.
Menning, S., de Ruiter, M. B., & Kieffer, J. M. Agelink van Rentergem, J., Veltman, D. J., Fruijtier, A., et al. (2016). Cognitive Impairment in a Subset of Breast Cancer Patients After Systemic Therapy - Results From a Longitudinal Study. Journal of Pain and Symptom Management, 52(4), 560–569.e1. doi:10.1016/j.jpainsymman.2016.04.012.
Nichols, T. E., & Holmes, A. P. (2002). Nonparametric permutation tests for functional neuroimaging: A primer with examples. Human Brain Mapping, 15(1), 1–25.
Pfefferbaum, A., Rosenbloom, M. J., Chu, W., Sassoon, S. A., Rohlfing, T., Pohl, K. M., et al. (2014). White matter microstructural recovery with abstinence and decline with relapse in alcohol dependence interacts with normal ageing: A controlled longitudinal DTI study. The Lancet. Psychiatry, 1(3), 202–212. doi:10.1016/S2215-0366(14)70301-3.
Pierpaoli, C., & Basser, P. J. (1996). Toward a quantitative assessment of diffusion anisotropy. Magnetic Resonance in Medicine, 36(6), 893–906. doi:10.1002/mrm.1910360612.
Pomykala, K. L., de Ruiter, M. B., Deprez, S., McDonald, B. C., & Silverman, D. H. S. (2013). Integrating imaging findings in evaluating the post-chemotherapy brain. Brain Imaging and Behavior, 7(4), 436–452. doi:10.1007/s11682-013-9239-y.
Schilder, C. M., Seynaeve, C., Beex, L. V., Boogerd, W., Linn, S. C., Gundy, C. M., et al. (2010a). Effects of tamoxifen and exemestane on cognitive functioning of postmenopausal patients with breast cancer: Results from the neuropsychological side study of the tamoxifen and exemestane adjuvant multinational trial. Journal of Clinical Oncology, 28(8), 1294–1300. doi:10.1200/JCO.2008.21.3553.
Schilder, C. M. T., Seynaeve, C., Linn, S. C., Boogerd, W., Beex, LVAM., Gundy, C. M., et al. (2010b). Cognitive functioning of postmenopausal breast cancer patients before adjuvant systemic therapy, and its association with medical and psychological factors. Critical Reviews in Oncology/Hematology, 76(2), 133–141. doi:10.1016/j.critrevonc.2009.11.001
Schmand, B., Lindeboom, J., & van Harskamp, F. (1992). De Nederlandse Leestest Voor Volwassenen. Lisse: Swets & Zeitlinger.
Schwarz, C. G., Reid, R. I., Gunter, J. L., Senjem, M. L., Przybelski, S. A., Zuk, S. M., et al. (2014). Improved DTI registration allows voxel-based analysis that outperforms tract-based spatial statistics. NeuroImage, 94, 65–78. doi:10.1016/j.neuroimage.2014.03.026.
Seigers, R., Loos, M., Van Tellingen, O., Boogerd, W., Smit, A. B., & Schagen, S. B. (2015). Cognitive impact of cytotoxic agents in mice. Psychopharmacology, 232(1), 17–37. doi:10.1007/s00213-014-3636-9.
Smith, S. M., Jenkinson, M., Johansen-Berg, H., Rueckert, D., Nichols, T. E., Mackay, C. E., et al. (2006). Tract-based spatial statistics: Voxelwise analysis of multi-subject diffusion data. NeuroImage, 31(4), 1487–1505. doi:10.1016/j.neuroimage.2006.02.024.
Stewart, A. L., Ware, J. E., Sherbourne, C. D., & Wells, K. B. (1992). Psychological distress/well-being and cognitive functioning measures. In A. L. Stewart & J. E. Ware (Eds.), Measuring functioning and well-being: The medical outcomes study approach (pp. 102–142). Durham, NC: Duke University Press.
Stouten-Kemperman, M. M., de Ruiter, M. B., Koppelmans, V., Boogerd, W., Reneman, L., & Schagen, S. B. (2014). Neurotoxicity in breast cancer survivors ≥10 years post-treatment is dependent on treatment type. Brain Imaging and Behavior, 275–284. doi:10.1007/s11682-014-9305-0.
Sullivan, E. V., Rohlfing, T., & Pfefferbaum, A. (2010). Longitudinal study of callosal microstructure in the normal adult aging brain using quantitative DTI fiber tracking. Developmental Neuropsychology, 35(3), 233–256. doi:10.1080/87565641003689556.
Wald, F. D. M., & Mellenbergh, G. J. (1990). De verkorte versie van de Nederlandse vertaling van de Profile of Mood States (POMS). Nederlands Tijdschrift voor de Psychologie, 45, 86–90.
Wechsler, D. (2000). WAIS-III Nederlandstalige bewerking. Technische Handleiding. Lisse: Swets & Zeitlinger.
Wefel, J. S., Kesler, S. R., Noll, K. R., & Schagen, S. B. (2015). Clinical characteristics, pathophysiology, and management of noncentral nervous system cancer-related cognitive impairment in adults. CA: A Cancer Journal for Clinicians, 65(2), 123–138. doi:10.3322/caac.21258.
Weiss, D., & Marmar, C. (1997). The impact of event scale - revised. In J. Wilson & T. Keane (Eds.), Assessing psychological trauma and PTSD (pp. 399–411). New York: Guilford Press.
Weng, Q., Tan, B., Wang, J., Wang, J., Zhou, H., Shi, J., et al. (2014). 5-fluorouracil causes severe CNS demyelination by disruption of TCF7L2/HDAC1/HDAC2 complex in adolescent mice. Toxicology, 325, 144–150. doi:10.1016/j.tox.2014.08.011.
Winocur, G., Vardy, J., Binns, M. A., Kerr, L., & Tannock, I. (2006). The effects of the anti-cancer drugs, methotrexate and 5-fluorouracil, on cognitive function in mice. Pharmacology Biochemistry and Behavior, 85(1), 66–75. doi:10.1016/j.pbb.2006.07.010.
Zwart, W., Terra, H., Linn, S. C., & Schagen, S. B. (2015). Cognitive effects of endocrine therapy for breast cancer: Keep calm and carry on? Nature reviews. Clinical Oncology, 12(10), 597–606. doi:10.1038/nrclinonc.2015.124.
Acknowledgements
This study was funded by the Dutch Cancer Society (KWF 2009-4284). We thank Epie Boven, MD, PhD, Suzan van der Meij, MD, Vera Lustig, MD, and Monique Bos, MD, PhD, for their contributions to the patient recruitment. We are indebted to all patients and controls, as well as physicians and nurses of the Netherlands Cancer Institute-Antoni van Leeuwenhoek Hospital, VU University Medical Center, Flevoziekenhuis, Reinier de Graaf Gasthuis and Academic Medical Center, for providing patients for this study and the research assistants for helping collecting the data.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was funded by the Dutch Cancer Society (grant number KWF 2009–4284).
Conflict of interest
Author Menning declares that she has no conflict of interest. Author de Ruiter declares that he has no conflict of interest. Author Veltman declares that he has no conflict of interest. Author Boogerd declares that he has no conflict of interest. Author Oldenburg declares that she has no conflict of interest. Author Reneman declares that she has no conflict of interest. Author Schagen declares that she has no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Menning, S., de Ruiter, M.B., Veltman, D.J. et al. Changes in brain white matter integrity after systemic treatment for breast cancer: a prospective longitudinal study. Brain Imaging and Behavior 12, 324–334 (2018). https://doi.org/10.1007/s11682-017-9695-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11682-017-9695-x