Abstract
Structural abnormalities in frontal, limbic and subcortical regions have been noted in adults with both major depressive disorder (MDD) and bipolar disorder (BD). In the current study, we examined regional brain morphology in youth with MDD and BD as compared to controls. Regional brain volumes were measured in 32 MDD subjects (15.7 ± 2.1 years), 14 BD subjects (16.0 ± 2.4 years) and 22 healthy controls (16.0 ± 2.8 years) using magnetic resonance imaging (MRI). Regions of interest included the hippocampus, dorsolateral prefrontal cortex (DLPFC), anterior cingulate cortex (ACC), caudate, putamen and thalamus. Volumetric differences between groups were significant (F26,80 = 1.80, p = 0.02). Post-hoc analyses indicated that individuals with MDD showed reduced left hippocampus volumes (p = 0.048) as well as right ACC white and gray matter volumes (p = 0.003; p = 0.01) compared to controls. BD participants also displayed reduced left hippocampal and right/left putamen volumes compared to controls (p < 0.001; p = 0.015; p = 0.046 respectively). Interestingly, right and left ACC white matter volumes were smaller in MDD than in BD participants (p = 0.019; p = 0.045 respectively). No volumetric group differences were observed for the DLPFC and thalamus. Discriminant analysis was able to correctly classify 81.0 % of subjects as having BD or as MDD based on imaging data. Confirmation and extension of our findings requires larger sample sizes. Our findings provide new evidence of distinct, specific regional brain volumetric differences between MDD and BD that may be used to distinguish the two disorders.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Major depressive disorder (MDD) or unipolar depression is a common mental illness affecting adolescents. The lifetime prevalence of MDD in youth is approximately 15–20 %, consistent with adulthood rates (Lewinsohn et al. 1986). Furthermore, evidence suggests that child and adolescent depression is continuous with adult MDD (Lewinsohn et al. 1986). Bipolar disorder (BD), has a lifetime prevalence of 1.5 %, and exerts similar (if not more pronounced and persistent) negative impacts on social, academic and long-term health outcomes as MDD (Murray and Lopez 1996; Greenberg et al. 1993). Typically, the first presentation of BD in adolescents manifests as a depressive episode in 75 % of cases (Kutcher et al. 1998). Bipolar disorder and MDD, though similar, require divergent courses of treatment in order to achieve good outcomes. Effective and timely treatment of BD is limited by difficulties in distinguishing the two disorders.
Bipolar disorder and MDD do display many salient differences. With respect to presentation, individuals with BD may demonstrate the presence of psychosis or psychotic-like symptoms, diurnal mood variation, hypersomnia during depressive episodes, and a greater number of shorter depressive episodes than typically seen in MDD (Forty et al. 2008). Large multicenter studies found that compared with MDD, BD was more strongly associated with a family history of the disorder, had an earlier age of onset, was associated with a greater number of previous depressive episodes and was linked with eight different individual symptom items on the Montgomery-Asberg Depression Rating Scale (MADRS) and the Hamilton Anxiety Rating Scale (HAMA) (Perlis et al. 2006). While these distinct clinical manifestations between BD and MDD suggest that the brain regions involved in the two disorders may be different, the biological/neural etiologies between the two remain elusive (Yatham et al. 1997; Konarski et al. 2008). Few studies have directly compared the underlying neurobiology of MDD and BD using magnetic resonance imaging (MRI) within adolescent psychiatric populations, though some studies have investigated putative differences between the two disorders in adult populations (Konarski et al. 2008; Kempton et al. 2011). Assessing whether neuroanatomical differences characterize MDD and BD during the early stages of the disease (i.e., during adolescence) may help in distinguishing between the two disorders and allow for earlier diagnosis and timely decisions regarding effective treatment.
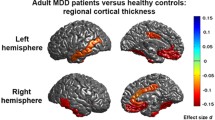
Despite the paucity of work assessing the neural correlates of MDD versus BP directly in adolescents, a substantial body of literature has examined the neural correlates of each disorder independently. Previously, smaller hippocampal volumes were found in early-onset MDD in adolescents (MacMaster and Kusumakar 2004). This finding was replicated in an independent sample and extended by focusing on depressed subjects with a family history of MDD (MacMaster et al. 2008a). Lower concentrations of the neuronal marker N-acetyl-aspartate (NAA) in the hippocampus were also noted in MDD youth as compared to healthy controls (MacMaster et al. 2008b). Similar findings have been shown in two studies of adolescents with BD; one of the studies consisted of predominantly euthymic BD adolescents (Bearden et al. 2008), while patient status at time of assessment was not specified in the other (Bearden et al. 2008; Frazier et al. 2008). In the dorsolateral prefrontal cortex (DLPFC), increased choline concentrations (which tend to index neural membrane synthesis and breakdown, thus reflecting decreased cell integrity) have been noted in pediatric MDD (Farchione et al. 2002). More recently, our group has documented increased cortical thickness within the rostral middle frontal gyrus, an aspect of the DLPFC, in youth with MDD versus controls (Reynolds et al., submitted). In adolescents with BD, Dickstein et al. (2005) found reduced gray matter in the left DLPFC. In the anterior cingulate (ACC), increases in cytosolic choline and reduced glutamate concentrations have been noted in youth with MDD (MacMaster and Kusumakar 2006; Rosenberg et al. 2005). A greater decrease in ACC volume over a 2-years period was found in adolescents with BD as compared to healthy controls (Kalmar et al. 2009). Smaller left ACC volume was also noted in BD versus control subjects (Chiu et al. 2008). On the other hand, increased gray matter density was noted in first episode individuals with BD as compared to controls (Adler et al. 2007). Changes in frontal-limbic circuits are consistent with some of the noted cognitive (i.e., attention/concentration as well as memory deficits) as well as emotive symptoms (i.e., depressed mood, putative hypersensitivity to emotive, particularly, negative cues, impaired emotive control, rumination) associated with mood disorders.
Evidence suggesting changes in subcortical structures in either of the two disorders remains controversial. In pediatric MDD, smaller right striatum structures—specifically the caudate—were observed compared to controls (Matsuo et al. 2008). Increases in left caudate choline were also noted in adolescent MDD participants (Gabbay et al. 2007). Conversely, in BD, a larger left thalamus (Adler et al. 2007; Wilke et al. 2004), caudate and putamen were found relative to controls (Wilke et al. 2004). Traditionally, basal ganglia structures were principally implicated in motor regulation; as such, morphometric changes in these regions may be associated with symptoms such as psychomotor retardation in MDD (Sobin and Sackeim 1997). However, emerging evidence has also implicated basal ganglia structures in aspects related to cognition and emotive processing, specifically in guiding actions towards motivationally significant stimuli, and in regulating the motoric expressions associated with emotive states (i.e., facial expressions) (Ring and Serra-Mestres 2002; Camara et al. 2008). These findings are consistent with the fact that basal ganglia structures are richly interconnected with the DLPFC, orbitofrontal cortex as well as the ACC (fronto-striatal loops) (Alexander et al. 1986; Clark et al. 2009). Taken together, this evidence suggests involvement of both cortical and subcortical structures in specific symptoms of MDD and BD.
In the current study, we examined the volumes of the hippocampus, DLPFC, ACC, caudate, putamen, and thalamus using MRI in adolescents with MDD and BD as well as healthy controls. Studies of younger patients with mood disorders are critical in our efforts to delineate the neurobiological substrates of the disorders and to minimize confounds related to various interventions or resilience factors. We hypothesize that adolescents with MDD or BD will demonstrate similar reductions in DLPFC, ACC, and hippocampal volumes compared with controls, but demonstrate distinctions with respect to subcortical structures including the putamen, caudate and thalamus.
Experimental procedures
Participants
Thirty-two participants with MDD aged 12–18 years (10 males, 22 females), 14 patients with bipolar disorder (BD) aged 11–19 years (7 males, 7 females) and 22 healthy controls aged 9–21 years (9 males, 13 females) were recruited. All subjects with a mood disorder diagnosis had to be currently depressed for inclusion in the study. Patient participants were recruited from those referred to the Izaak Walton Killam (IWK) Health Center’s Department of Psychiatry. Controls were recruited through advertisements within the community. Both patients and controls were paid a small honorarium for study participation. The study psychiatrist used the Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present Lifetime version (K-SADS-PL; (Kaufman et al. 1997) to establish diagnostic group. Exclusion criteria for participation in this study were: a history of neurological disorders, serious medical condition, claustrophobia, age greater than 21 years, or the presence of a ferrous implant or pacemaker. Depression symptom severity was assessed using the Childhood Depression Rating Scale (CDRS) (Poznanski et al. 1979). All MDD and BD participants had a CDRS score above 40, indicative of significant dysfunction. Of the 14 BD, 10 had BD-I, one had BD-II, and 3 had BD not otherwise specified (BD-NOS). Two MDD participants had a comorbid diagnosis of substance abuse; one had oppositional defiant disorder (ODD), and another attention deficit hyperactivity disorder (ADHD). The remaining subjects had a single diagnosis of MDD. Four MDD participants had recently (<1 week) started medication (two with the selective serotonin reuptake inhibitor sertraline, one with the reversible monoamine oxidase inhibitor mocolobide, and one with the stimulant dexedrine). One BD participant had recently started taking the atypical antipsychotic risperidone (<1 week). The remaining participants were medication naïve. Nine of the MDD participants had a confirmed parent with a past history of depression (Andreasen et al. 1977). Structured family history data for the BD participants is not available. Four of the BD participants and three of the MDD participants had a past suicide attempt. Controls did not have any psychiatric illness. Written informed consent was obtained prior to initiating the study in compliance with the IWK Research Ethics Board. See Table 1.
Imaging acquisition
The MRI studies were conducted with a 1.5 Tesla Siemens Magnetom Vision magnetic resonance system (Germany). A sagittal scout series was acquired to test image quality. A three-dimensional fast low angle shot (FLASH) sequence was used to acquire data from 124 1.5 mm thick contiguous coronal slices through the entire brain (echo time = 5 ms, repetition time = 25 ms, acquisition matrix = 256 × 256 pixels, field of view = 24 cm and flip angle = 40°). Positioning was done in a standardized manner in order to ensure consistency of acquisitions, along the anterior- and posterior-commissure line. Volumetric structural measurements were made by trained and reliable raters (F.P.M., P.E., C.R.; inter- and intra-class r < 0.90 for all structures), blind to subject identification and clinical status. Furthermore, some subjects had their scans randomly flipped (along the y axis: switching the left and right sides) prior to manual tracing in order to limit measurement bias. Manual tracing was done using the MEDx software program.
Regional brain volumetric measurements
Hippocampus
Special care was taken to separate the anterior boundary of the hippocampus from the amygdala. The appearance of the mammillary bodies was used as a guide to determine the posterior-anterior border of the amygdala. More anteriorly, amygdala gray matter in slices begins to extend superiorly to the hippocampus. This observation was aided by the sagittal view. The posterior hippocampal boundary was marked by the clearest appearance of the fornix. The lateral hippocampal border was defined by the temporal horn of the lateral ventricle and or the white matter adjacent to the hippocampal gray matter. The inferior border was demarcated by the white matter of the parahippocampal gyrus (MacMaster and Kusumakar 2004).
Anterior cingulate cortex (ACC)
The anterior boundary was the tip of the cingulate sulcus. The posterior boundary was marked by the connection of the superior and precentral sulci. The ventral boundary was denoted by the callosal sulcus. The dorsal boundary was the cingulate sulcus (Szeszko et al. 2004a).
Dorsolateral prefrontal cortex (DLPFC)
The location of the most anterior part of the genu of the corpus callosum was used as the first slice for measuring the DLPFC. The superior boundary was denoted by the superior frontal sulcus. The inferior boundary was marked by the posterior lateral fissure and horizontal ramus of the anterior lateral fissure. The lateral border was represented by the edge of the cerebral cortex. The medial border was delineated by the connection of the deepest parts on the superior frontal sulcus and the lateral fissure (Rosenberg and Keshavan 1998).
Thalamus
The left and right thalami were measured separately. The mammillary bodies and interventricular foramen marked the anterior boundary. The internal capsule acted as the lateral boundary. The third ventricle acted as the medial boundary. The hypothalamus marked the inferior boundary. The posterior boundary was demarcated by where the thalamus merged under the crux of the fornix. The superior boundary was the main body of the lateral ventricle (Gilbert et al. 2000b).
Caudate nucleus
Tracing began at the most anterior slice where the caudate was visible and continued in posteriorly until the pons was first visible. The medial boundary was the lateral ventricle. The lateral boundary was the internal capsule. Using the coronal slice where the anterior commissure was the most visible, the inferior border of the caudate was established as the inferior border of the lateral ventricles. This excluded the nucleus accumbens (Matsuo et al. 2008).
Putamen
Tracing began at the most anterior slice where the putamen was first visible. The medial boundary was the internal capsule. The lateral boundary was the external capsule. The superior boundary was the corona radiata. The most posterior boundary was where the putamen was no longer visible in the corona radiata (Matsuo et al. 2008).
Statistics
To test overall group comparisons, a multivariate analysis of variance (MANOVA) test of significance for planned comparisons was used. Planned comparisons were MDD vs. controls (−1 vs. 1) and bipolar vs. controls (−1 vs. 1). For post-hoc analysis, Tukey HSD tests were used (p < 0.05). To examine the relationship between clinical and demographic variables and regional brain volumes, Pearson’s correlations were used. In an exploratory analysis, a series of repeated measures ANCOVAs controlling for whole brain volume (WBV, which included all gray and white matter of the frontal, parietal, temporal, and occipital lobes) were conducted for group comparisons on variables of interest, and a discriminant analysis was conducted on the BD and MDD participants to determine group membership based on a combination of regional brain volume variables. T-tests were used to compare children who were misclassified. No differences in WBV were noted between groups (F2,67 = 1.19, p = 0.31).
Results
The overall MANOVA between groups was significant (F26,80 = 1.80, p = 0.02). Post-hoc analysis revealed smaller left hippocampal volumes in both MDD (p = 0.048) and BD (p = 0.005) groups compared to controls; no such differences were noted in the right hippocampus. BD and MDD hippocampal volumes did not differ. Right ACC gray matter volume was smaller in MDD versus control groups (p = 0.003) and demonstrated a trend for being smaller than BD participants (p = 0.07). Right ACC white matter volume was smaller in MDD compared to both controls (p = .01) and BD (p = 0.019). Left gray ACC matter volume did not differ between groups. Left ACC white matter was smaller in MDD participants compared to BD patients (p = 0.045) but not controls. Right and left putamen volume was smaller in BD participants compared to controls (p = 0.014, p = 0.046 respectively). MDD did not differ from controls or BD groups in putamen volumes. No differences were observed for the caudate, DLPFC, and thalamus between any of the groups. When the BP-NOS subjects were removed, the results did not change significantly. No correlations between clinical/demographic variables (i.e., CDRS, age, BDI) and regional brain volumes passed the correction for multiple comparisons to reach significance. See Fig. 1 and Tables 2 and 3. We examined sex differences in an exploratory manner. For both the left hippocampus and right ACC, the effect appeared driven more so by the males (F = 9.85, p = 0.001, males vs. F = 0.83, p = 0.44, females and F = 8.12, p = 0.003, males vs. F = 2.05, p = 0.14, females respectively). Interestingly, in the right and left putamen, it was the females driving the effect (F = 1.21, p = 0.32, males vs. F = 7.65, p = 0.002, females and F = 1.73, p = 0.20, males vs. F = 5.09, p = 0.01, females respectively). Within diagnostic groups, we found that in controls left hippocampal volumes were larger in females than males (t = 3.40, p = 0.003) but not in the other groups. In the BD group, right and left putamen volumes were larger in males than females (t = 3.34, p = 0.008 and t = 3.75, p = 0.004 respectively) but not in the other groups. Finally, in the MDD group, no significant sex differences were noted.
Exploratory discriminant analysis
Results of a series of repeated measures analysis of covariance (ANCOVAs) (controlling for intracranial volume – described in (Rosenberg et al. 1997)) for each variable of interest revealed a significant group×hemisphere interaction for the right and left hippocampi (F1,43 = 6.89, p = 0.012). Results also showed a significant group difference for left and right ACC volumes (F1,39 = 6.74, p = 0.013), but no significant hemisphere effect and no significant group×hemisphere interaction. Repeated measures ANCOVAs for the caudate, putamen, thalamus, DLPFC and PFC did not reveal any significant effects. Given the relatively small sample size of the two clinical groups, the next analysis incorporated a discriminant function analysis using the right and left hippocampus, and the right and left ACC along with WBV as potential variables for discriminating between the two clinical groups. Results revealed a significant overall discriminant function (X 2(5) = 18.67, p = 0.002), with the volumes of the right ACC and left hippocampus being the two significant discriminating variables in terms of group (BD/MDD) membership. Overall, 88.5 % of children were correctly classified as having BD or MDD. When the groups were considered separately, 88.2 % of the MDD group was correctly classified. 88.9 % of the BD group was correctly classified. When the split-half model was tested with the remainder of the sample for cross validation, results were similar: a significant overall discriminant function (X 2(5) = 15.42, p = 0.003), with the volumes of the right ACC and left hippocampus being the two significant discriminating variables; overall, 81.3 % of children were correctly classified (83.3 % of the MDD and 75.0 % of the BD group were correctly classified).
Participants in the BD who were misclassified as MDD had significantly larger left hippocampus volume values (M = 2.69 cm3, SD = 0.29) compared to BD patients who were correctly classified (M = 2.17 cm3, SD = 0.37, t11 = −2.63, p = 0.023). Compared to correctly classified BD participants, group members who were misclassified as MDD also tended (trend level) to have lower volume values of the right ACC (M = 3.40 cm3, SD = 0.46 versus M = 3.96 cm3, SD = 0.48 for correctly classified; t11 = 2.08, p = 0.061) and higher values of the left prefrontal cortex (M = 40.22 cm3, SD = 6.36 compared to M = 32.31 cm3, SD = 6.71 for correctly classified; t11 = −2.11, p = 0.059), as compared to correctly classified BP participants.
Individuals in the MDD group who were misclassified as BD had significantly larger volume values of the right ACC (M = 3.94 cm3, SD = 0.26) than participants in this group who were classified correctly (M = 3.09 cm3, SD = 0.53; t27 = −2.74, p = 0.011). Participants in the MDD group who were misclassified also tended to have a larger left putamen (M = 4.96 cm3, SD = 0.78) compared to correctly classified participants (M = 4.19 cm3, SD = 0.60, t27 = −2.05, p = 0.050).
Discussion
In this study, we found smaller hippocampal volumes in both MDD and BD adolescent participants compared to controls. ACC gray and white matter volumes were smaller in MDD participants than controls and differentiated MDD patients from BD patients. Furthermore, we found smaller putamen volumes only in BD subjects compared to controls. Regions like the DLPFC, thalamus and caudate did not differ between groups.
Our finding of smaller hippocampal volumes is consistent with studies in youth with BD (Bearden et al. 2008; Blumberg et al. 2003) and MDD in adolescents (MacMaster and Kusumakar 2004; MacMaster et al. 2008a). It is important to note that further studies assessing morphometric brain changes are needed due to the small number of existing reports, especially during late adolescence and early adulthood when differences in hippocampal volume appear less robust (McKinnon et al. 2009). Given that reduced hippocampal volumes have also been noted in adults with MDD (Campbell et al. 2004), hippocampal volume reductions may be a trait marker of depression and/or the hippocampus may be one of the earliest structures to be negatively impacted by the disorder. Although hippocampal volume reductions in adults with BD are less consistently documented, this may be related to lithium treatment, which may have neuroprotective effects (Hajek et al. 2012), thus, both MDD and BD appear to be associated with hippocampal volume decreases that emerge early in the disorder. In healthy adolescents, rostral ACC volume was smaller in boys with subclinical depressive symptoms and correlated negatively with symptoms. This finding was particularly robust in those with a family history of MDD (Boes et al. 2008). In children and adolescents with MDD, increases in cytosolic choline (suggesting greater cell turnover) and reduced glutamate concentrations have also been noted in the ACC (MacMaster and Kusumakar 2006; Rosenberg et al. 2005). Our findings of decreased ACC volumes (in both the grey and white matter aspects) in MDD versus BD patients are consistent with some previous work examining brain structure and chemistry in similar populations.
Our finding of a smaller putamen in BD versus controls is novel. However, the presence of comorbid attentional issues may influence putamen volume (Liu et al. 2011) and, contrary to our findings, greater putamen volumes were noted in medicated adults with BD (Hallahan et al. 2011). Other studies in pediatric BD reported no differences in putamen volume (Ahn et al. 2007; Sanches et al. 2005). Increased activation in the putamen was noted during facial emotional processing in BD adults compared to controls (Hulvershorn et al. 2012). This was also observed in children with BD (Rich et al. 2006). Our study suggests that putamen volumes may discriminate unipolar and bipolar depression, however, further study is warranted.
The exploratory discriminant analysis demonstrated that imaging data could be used to distinguish MDD and BD patients (81 % correctly classified). The analysis was more successful in classifying MDD (89.7 %) than the BD (61.5 %) group. Based on these findings, regional brain volume data show promise for diagnostic purposes, which have been attempted in other disorders (Soliva et al. 2010). Our selection of candidate regions was based upon findings in our primary analysis and then testing the viability of each region as a potential discriminating factor.
The inconsistency of some of our findings pertaining to BD compared with precedent research may be due to a number of factors. First, there are indications that the brain changes in BD are progressive (Lisy et al. 2011). The BD participants may have been at different stages of their illness course, leading to varying degrees of observed brain changes. Furthermore, our sample was largely treatment naïve at the time of their scan, which could account for some of our discrepant findings from previous published work (which tend to assess medicated participants). The effect of treatment on regional brain volumes has been well documented in BD (Baykara et al. 2012; Hallahan et al. 2011) and in other conditions treated with psychotropic medications (Gilbert et al. 2000a; Szeszko et al. 2004b; Chakos et al. 1994; Keshavan et al. 1994). The influence of comorbidity may be another factor that contributed to the variability of our findings compared with precedent literature, especially with respect to the putamen (Liu et al. 2011). Given the results of the exploratory analysis of sex differences, the influence of sex on brain morphometry in the context of mood disorders warrants further exploration. Replication of this study with a larger sample size and taking the above-mentioned factors into account will be necessary in comparable future work. With larger samples, some trends may achieve significance (ACC gray matter between MDD and BP subjects for example), and age, bipolar type and gender matching would be more viable. Lastly, because some of our participants were undergoing treatment, this may have affected our findings.
There are several limitations that must be acknowledged: (1) the small sample size, (2) the presence of subjects with a prior treatment history (even if only for a short time), (3) the heterogeneity in the BD group, (4) the potential instability (and hence validity) of the diagnosis, and (5) the wide age range used. However, these limitations are offset by the novel nature of the study design directly comparing BD, MDD and healthy control participants with regard to regional brain volumes. Developing more accurate neurobiological profiles of MDD and BD may eventually lead to methods for distinguishing these patient groups. Indeed, our exploratory discriminant analysis was fairly successful in distinguishing the two disorders, despite some significant clinical similarities (both groups presenting in a depressive episode).
In conclusion, data from this study indicated both similar and distinct regions of brain volume changes in MDD and BD adolescent participants. An exploratory discriminant analysis revealed that imaging data could successfully classify 81 % of MDD individuals. Further work is needed to develop biomarkers that can distinguish MDD and BD early on in the course of illness.
References
Adler, C. M., DelBello, M. P., Jarvis, K., Levine, A., Adams, J., & Strakowski, S. M. (2007). Voxel-based study of structural changes in first-episode patients with bipolar disorder. [Research Support, N.I.H., Extramural Research Support, Non-U.S. Gov’t]. Biological Psychiatry, 61(6), 776–781. doi:10.1016/j.biopsych.2006.05.042.
Ahn, M. S., Breeze, J. L., Makris, N., Kennedy, D. N., Hodge, S. M., Herbert, M. R., et al. (2007). Anatomic brain magnetic resonance imaging of the basal ganglia in pediatric bipolar disorder. Journal of Affective Disorders, 104(1–3), 147–154. doi:10.1016/j.jad.2007.04.015.
Alexander, G. E., DeLong, M. R., & Strick, P. L. (1986). Parallel organization of functionally segregated circuits linking basal ganglia and cortex. Annual Review of Neuroscience, 9, 357–381. doi:10.1146/annurev.ne.09.030186.002041.
Andreasen, N. C., Endicott, J., Spitzer, R. L., & Winokur, G. (1977). The family history method using diagnostic criteria. Reliability and validity. Archives of General Psychiatry, 34(10), 1229–1235.
Baykara, B., Inal-Emiroglu, N., Karabay, N., Cakmakci, H., Cevher, N., Senturk Pilan, B., et al. (2012). Increased hippocampal volumes in lithium treated adolescents with bipolar disorders: A structural MRI study. Journal of Affective Disorders, 138(3), 433–439. doi:10.1016/j.jad.2011.12.047.
Bearden, C. E., Soares, J. C., Klunder, A. D., Nicoletti, M., Dierschke, N., Hayashi, K. M., et al. (2008). Three-dimensional mapping of hippocampal anatomy in adolescents with bipolar disorder. [Research Support, N.I.H., Extramural]. Journal of the American Academy of Child and Adolescent Psychiatry, 47(5), 515–525. doi:10.1097/CHI.0b013e31816765ab.
Blumberg, H. P., Kaufman, J., Martin, A., Whiteman, R., Zhang, J. H., Gore, J. C., et al. (2003). Amygdala and hippocampal volumes in adolescents and adults with bipolar disorder. [Research Support, Non-U.S. Gov’t Research Support, U.S. Gov’t, Non-P.H.S. Research Support, U.S. Gov’t, P.H.S.]. Archives of General Psychiatry, 60(12), 1201–1208. doi:10.1001/archpsyc.60.12.1201.
Boes, A. D., McCormick, L. M., Coryell, W. H., & Nopoulos, P. (2008). Rostral anterior cingulate cortex volume correlates with depressed mood in normal healthy children. Biological Psychiatry, 63(4), 391–397. doi:10.1016/j.biopsych.2007.07.018.
Camara, E., Rodriguez-Fornells, A., & Munte, T. F. (2008). Functional connectivity of reward processing in the brain. Frontiers in Human Neuroscience, 2, 19. doi:10.3389/neuro.09.019.2008.
Campbell, S., Marriott, M., Nahmias, C., & MacQueen, G. M. (2004). Lower hippocampal volume in patients suffering from depression: a meta-analysis. The American Journal of Psychiatry, 161(4), 598–607.
Chakos, M. H., Lieberman, J. A., Bilder, R. M., Borenstein, M., Lerner, G., Bogerts, B., et al. (1994). Increase in caudate nuclei volumes of first-episode schizophrenic patients taking antipsychotic drugs. The American Journal of Psychiatry, 151(10), 1430–1436.
Chiu, S., Widjaja, F., Bates, M. E., Voelbel, G. T., Pandina, G., Marble, J., et al. (2008). Anterior cingulate volume in pediatric bipolar disorder and autism. [Comparative Study Research Support, N.I.H., Extramural Research Support, Non-U.S. Gov’t]. Journal of Affective Disorders, 105(1–3), 93–99. doi:10.1016/j.jad.2007.04.019.
Clark, L., Chamberlain, S. R., & Sahakian, B. J. (2009). Neurocognitive mechanisms in depression: implications for treatment. [Research Support, Non-U.S. Gov’t Review]. Annual Review of Neuroscience, 32, 57–74. doi:10.1146/annurev.neuro.31.060407.125618.
Dickstein, D. P., Milham, M. P., Nugent, A. C., Drevets, W. C., Charney, D. S., Pine, D. S., Leibenluft, E. (2005) Frontotemporal alterations in pediatric bipolar disorder: results of a voxel-based morphometry study. Arch Gen Psychiatry, 62(7):734–741. doi:10.1001/archpsyc.62.7.734.
Farchione, T. R., Moore, G. J., & Rosenberg, D. R. (2002). Proton magnetic resonance spectroscopic imaging in pediatric major depression. Biological Psychiatry, 52(2), 86–92.
Forty, L., Smith, D., Jones, L., Jones, I., Caesar, S., Cooper, C., et al. (2008). Clinical differences between bipolar and unipolar depression. British Journal of Psychiatry, 192(5), 388–389. doi:10.1192/bjp.bp.107.045294.
Frazier, J. A., Hodge, S. M., Breeze, J. L., Giuliano, A. J., Terry, J. E., Moore, C. M., et al. (2008). Diagnostic and sex effects on limbic volumes in early-onset bipolar disorder and schizophrenia. Schizophrenia Bulletin, 34(1), 37–46. doi:10.1093/schbul/sbm120.
Gabbay, V., Hess, D. A., Liu, S., Babb, J. S., Klein, R. G., & Gonen, O. (2007). Lateralized caudate metabolic abnormalities in adolescent major depressive disorder: a proton MR spectroscopy study. [Comparative Study Research Support, N.I.H., Extramural Research Support, Non-U.S. Gov’t]. The American Journal of Psychiatry, 164(12), 1881–1889. doi:10.1176/appi.ajp.2007.06122032.
Gilbert, A. R., Moore, G. J., Keshavan, M. S., Paulson, L. A., Narula, V., Mac Master, F. P., et al. (2000). Decrease in thalamic volumes of pediatric patients with obsessive-compulsive disorder who are taking paroxetine. Archives of General Psychiatry, 57(5), 449–456.
Greenberg, P. E., Stiglin, L. E., Finkelstein, S. N., & Berndt, E. R. (1993). The economic burden of depression in 1990. [Research Support, Non-U.S. Gov’t]. Journal of Clinical Psychiatry, 54(11), 405–418.
Hajek, T., Cullis, J., Novak, T., Kopecek, M., Hoschl, C., Blagdon, R., et al. (2012). Hippocampal volumes in bipolar disorders: opposing effects of illness burden and lithium treatment. [Comparative Study Multicenter Study Research Support, Non-U.S. Gov’t]. Bipolar Disorders, 14(3), 261–270. doi:10.1111/j.1399-5618.2012.01013.x.
Hallahan, B., Newell, J., Soares, J. C., Brambilla, P., Strakowski, S. M., Fleck, D. E., et al. (2011). Structural magnetic resonance imaging in bipolar disorder: an international collaborative mega-analysis of individual adult patient data. [Meta-Analysis]. Biological Psychiatry, 69(4), 326–335. doi:10.1016/j.biopsych.2010.08.029.
Hulvershorn, L. A., Karne, H., Gunn, A. D., Hartwick, S. L., Wang, Y., Hummer, T. A., et al. (2012). Neural activation during facial emotion processing in unmedicated bipolar depression, euthymia, and mania. Biological Psychiatry, 71(7), 603–610. doi:10.1016/j.biopsych.2011.10.038.
Kalmar, J. H., Wang, F., Spencer, L., Edmiston, E., Lacadie, C. M., Martin, A., et al. (2009). Preliminary evidence for progressive prefrontal abnormalities in adolescents and young adults with bipolar disorder. Journal of International Neuropsychological Society, 15(3), 476–481. doi:10.1017/S1355617709090584.
Kaufman, J., Birmaher, B., Brent, D., Rao, U., Flynn, C., Moreci, P., et al. (1997). Schedule for affective disorders and schizophrenia for school-age children-present and lifetime version (K-SADS-PL): initial reliability and validity data. Journal of the American Academy of Child and Adolescent Psychiatry, 36(7), 980–988. doi:10.1097/00004583-199707000-00021.
Kempton, M. J., Salvador, Z., Munafo, M. R., Geddes, J. R., Simmons, A., Frangou, S., et al. (2011). Structural neuroimaging studies in major depressive disorder. Meta-analysis and comparison with bipolar disorder. [Comparative Study Meta-Analysis Research Support, Non-U.S. Gov’t]. Archives of General Psychiatry, 68(7), 675–690. doi:10.1001/archgenpsychiatry.2011.60.
Keshavan, M. S., Bagwell, W. W., Haas, G. L., Sweeney, J. A., Schooler, N. R., & Pettegrew, J. W. (1994). Changes in caudate volume with neuroleptic treatment. Lancet, 344(8934), 1434.
Konarski, J. Z., McIntyre, R. S., Kennedy, S. H., Rafi-Tari, S., Soczynska, J. K., & Ketter, T. A. (2008). Volumetric neuroimaging investigations in mood disorders: bipolar disorder versus major depressive disorder. [Research Support, Non-U.S. Gov’t Review]. Bipolar Disorders, 10(1), 1–37. doi:10.1111/j.1399-5618.2008.00435.x.
Kutcher, S., Robertson, H. A., & Bird, D. (1998). Premorbid functioning in adolescent onset bipolar I disorder: a preliminary report from an ongoing study. [Research Support, Non-U.S. Gov’t]. Journal of Affective Disorders, 51(2), 137–144.
Lewinsohn, P. M., Duncan, E. M., Stanton, A. K., & Hautzinger, M. (1986). Age at first onset for nonbipolar depression. Journal of Abnormal Psychology, 95(4), 378–383.
Lisy, M. E., Jarvis, K. B., DelBello, M. P., Mills, N. P., Weber, W. A., Fleck, D., et al. (2011). Progressive neurostructural changes in adolescent and adult patients with bipolar disorder. [Research Support, N.I.H., Extramural Research Support, Non-U.S. Gov’t]. Bipolar Disorders, 13(4), 396–405. doi:10.1111/j.1399-5618.2011.00927.x.
Liu, I. Y., Howe, M., Garrett, A., Karchemskiy, A., Kelley, R., Alegria, D., et al. (2011). Striatal volumes in pediatric bipolar patients with and without comorbid ADHD. [Research Support, N.I.H., Extramural Research Support, Non-U.S. Gov’t]. Psychiatry Research, 194(1), 14–20. doi:10.1016/j.pscychresns.2011.06.008.
MacMaster, F. P., & Kusumakar, V. (2004). Hippocampal volume in early onset depression. BMC Medicine, 2, 2. doi:10.1186/1741-7015-2-2.
MacMaster, F. P., & Kusumakar, V. (2006). Choline in pediatric depression. Mcgill Journal of Medicine, 9(1), 24–27.
MacMaster, F. P., Mirza, Y., Szeszko, P. R., Kmiecik, L. E., Easter, P. C., Taormina, S. P., et al. (2008a). Amygdala and hippocampal volumes in familial early onset major depressive disorder. Biological Psychiatry, 63(4), 385–390. doi:10.1016/j.biopsych.2007.05.005.
MacMaster, F. P., Moore, G. J., Russell, A., Mirza, Y., Taormina, S. P., Buhagiar, C., et al. (2008b). Medial temporal N-acetyl-aspartate in pediatric major depression. Psychiatry Research, 164(1), 86–89. doi:10.1016/j.pscychresns.2007.12.022.
Matsuo, K., Rosenberg, D. R., Easter, P. C., MacMaster, F. P., Chen, H. H., Nicoletti, M., et al. (2008). Striatal volume abnormalities in treatment-naive patients diagnosed with pediatric major depressive disorder. Journal of Child and Adolescent Psychopharmacology, 18(2), 121–131. doi:10.1089/cap.2007.0026.
McKinnon, M. C., Yucel, K., Nazarov, A., & MacQueen, G. M. (2009). A meta-analysis examining clinical predictors of hippocampal volume in patients with major depressive disorder. Journal of Psychiatry and Neuroscience, 34(1), 41–54.
Murray, C. J. L., & Lopez, A. D. (1996). Global burden of disease and injury series (Vol. 1). Cambridge: Harvard University Press.
Perlis, R. H., Brown, E., Baker, R. W., & Nierenberg, A. A. (2006). Clinical features of bipolar depression versus major depressive disorder in large multicenter trials. [Comparative Study Meta-Analysis Research Support, N.I.H., Extramural Research Support, Non-U.S. Gov’t]. The American Journal of Psychiatry, 163(2), 225–231. doi:10.1176/appi.ajp.163.2.225.
Poznanski, E. O., Cook, S. C., & Carroll, B. J. (1979). A depression rating scale for children. Pediatrics, 64(4), 442–450.
Rich, B. A., Vinton, D. T., Roberson-Nay, R., Hommer, R. E., Berghorst, L. H., McClure, E. B., et al. (2006). Limbic hyperactivation during processing of neutral facial expressions in children with bipolar disorder. [Research Support, N.I.H., Intramural]. Proceedings of the National Academy of Sciences of the United States of America, 103(23), 8900–8905. doi:10.1073/pnas.0603246103.
Ring, H. A., & Serra-Mestres, J. (2002). Neuropsychiatry of the basal ganglia. [Review]. Journal of Neurology, Neurosurgery and Psychiatry, 72(1), 12–21.
Rosenberg, D. R., & Keshavan, M. S. (1998). A.E. Bennett research award. Toward a neurodevelopmental model of of obsessive–compulsive disorder. Biological Psychiatry, 43(9), 623–640.
Rosenberg, D. R., Keshavan, M. S., O’Hearn, K. M., Dick, E. L., Bagwell, W. W., Seymour, A. B., et al. (1997). Frontostriatal measurement in treatment-naive children with obsessive-compulsive disorder. Archives of General Psychiatry, 54(9), 824–830.
Rosenberg, D. R., MacMaster, F. P., Mirza, Y., Smith, J. M., Easter, P. C., Banerjee, S. P., et al. (2005). Reduced anterior cingulate glutamate in pediatric major depression: a magnetic resonance spectroscopy study. Biological Psychiatry, 58(9), 700–704.
Sanches, M., Roberts, R. L., Sassi, R. B., Axelson, D., Nicoletti, M., Brambilla, P., et al. (2005). Developmental abnormalities in striatum in young bipolar patients: a preliminary study. [Research Support, N.I.H., Extramural Research Support, Non-U.S. Gov’t Research Support, U.S. Gov’t, P.H.S.]. Bipolar Disorders, 7(2), 153–158. doi:10.1111/j.1399-5618.2004.00178.x.
Sobin, C., & Sackeim, H. A. (1997). Psychomotor symptoms of depression. [Research Support, Non-U.S. Gov’t Research Support, U.S. Gov’t, P.H.S. Review]. The American Journal of Psychiatry, 154(1), 4–17.
Soliva, J. C., Fauquet, J., Bielsa, A., Rovira, M., Carmona, S., Ramos-Quiroga, J. A., et al. (2010). Quantitative MR analysis of caudate abnormalities in pediatric ADHD: proposal for a diagnostic test. Psychiatry Research, 182(3), 238–243. doi:10.1016/j.pscychresns.2010.01.013.
Szeszko, P. R., MacMillan, S., McMeniman, M., Chen, S., Baribault, K., Lim, K. O., et al. (2004a). Brain structural abnormalities in psychotropic drug-naive pediatric patients with obsessive-compulsive disorder. The American Journal of Psychiatry, 161(6), 1049–1056.
Szeszko, P. R., MacMillan, S., McMeniman, M., Lorch, E., Madden, R., Ivey, J., et al. (2004b). Amygdala volume reductions in pediatric patients with obsessive-compulsive disorder treated with paroxetine: preliminary findings. Neuropsychopharmacology, 29(4), 826–832. doi:10.1038/sj.npp.1300399.
Wilke, M., Kowatch, R. A., DelBello, M. P., Mills, N. P., & Holland, S. K. (2004). Voxel-based morphometry in adolescents with bipolar disorder: first results. Psychiatry Research, 131(1), 57–69. doi:10.1016/j.pscychresns.2004.01.004.
Yatham, L. N., Srisurapanont, M., Zis, A. P., & Kusumakar, V. (1997). Comparative studies of the biological distinction between unipolar and bipolar depressions. [Comparative Study Review]. Life Sciences, 61(15), 1445–1455.
Acknowledgements
The authors would like to acknowledge Vivek Kusumakar, MD (1951–2009) for his contribution to the study. Dr. MacMaster received support for this research in part from the Cuthbertson and Fischer Chair in Paediatric Mental Health, the Alberta Children’s Hospital Foundation, Alberta Children’s Hospital Research Institute for Child and Maternal Health, the Mathison Centre for Mental Health Research & Education, the Hotchkiss Brain Institute, and the University of Calgary.
Conflict of Interest
No authors of this manuscript have fees and grants from, employment by, consultancy for, shared ownership in, or any close relationship with, an organization whose interests, financial or otherwise, may be affected by the publication of the paper.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
MacMaster, F.P., Carrey, N., Langevin, L.M. et al. Disorder-specific volumetric brain difference in adolescent major depressive disorder and bipolar depression. Brain Imaging and Behavior 8, 119–127 (2014). https://doi.org/10.1007/s11682-013-9264-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11682-013-9264-x