Abstract
Summary
To evaluate the case-finding strategy for osteoporosis in Norway, a questionnaire concerning risk factors for osteoporosis and history of osteodensitometry was mailed to a population-based cohort of 6000 men and 6000 women. Suboptimal examination rates among high risk and reallocation of scanning capacity to seemingly low-risk individuals was found.
Purpose
In Norway, a case-finding strategy for osteoporosis has been used. No data exist regarding the efficacy of this approach. The aim was to examine the prevalence of risk factors for osteoporosis and factors related to the use of dual X-ray absorptiometry (DXA) in Norway.
Methods
Questionnaires regarding previous history of DXA, risk factors for osteoporosis and fracture were sent to an age-stratified, nationwide cross-sectional sample of 6000 men and 6000 women aged 40–90 years, drawn from the Norwegian Civil Registration System.
Results
Valid responses (6029) were included. Twenty-two point three percent of women and 3.8 % of men had been examined by DXA. Suboptimal examination rates among high risk (e.g., current/previous glucocorticoid treatment or previous low-energy fracture) and reallocation of scanning capacity to seemingly low-risk individuals was found. Of all DXA, 19.5 % were reported by women without any risk factor for osteoporosis, similarly by 16.2 % of men. Distance to DXA facilities and current smoking were inversely related to probability of reporting a DXA.
Conclusions
Suboptimal examination rates among high risk and reallocation of scanning capacity to seemingly low-risk individuals were found. Distance to DXA, current smoking, and male sex constituted possible barriers to the case-finding strategy employed. Cheap and more available diagnostic tools for osteoporosis are needed, and risk stratification tools should be employed more extensively.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis is an important public health issue due to the combination of high prevalence, fracture-associated morbidity and mortality as well as its financial burden on society [1]. The disease is without symptoms until a fracture as a complication occurs. Therefore, preventive diagnostic measurements of bone mineral density (BMD) are reimbursed in many countries, with dual-energy X-ray absorptiometry (DXA) as the reference diagnostic standard [2]. Its usage is recommended either for universal screening of women and men over the age of 65 and 70, respectively [3], uniformly recommended for diagnosis in clinical high-risk groups [4] or after risk stratification by algorithms based on risk factors such as Fracture Risk Assessment Tool (FRAX) [5, 6]. But even in high-income countries with full reimbursement for DXA examinations, social disparities remain in the uptake of DXA, with an inverse association between income and level of education on one hand and the utilization of DXA on the other [7]. As lower socioeconomic status is associated with an increased risk of hip fracture in most [8–10], though not all studies [11], the outcome is less than ideal examination rates for osteoporosis among high-risk individuals with lower socioeconomic status.
Previously, Danish studies have reported less than optimal uptake of BMD measurements in populations with increasing number of clinical risk factors [12, 13].
The Norwegian background population comprised 4.85 million citizens as of 2010 [14]. Norway is the second-least population dense country in Europe. Due to its length (longest land distance of 1789 km) and mostly rugged countryside, rather long distances to the nearest health institution are a fact of life for Norwegians living outside city limits. The unique Norwegian geography means that research findings in other Scandinavian countries are not always readily transferable.
In Norway, the public health system provides tax-funded universal health care to the population with a smaller co-payment for medical consultations for individuals older than 16 years of age. For the year 2010, the set amounts were NOK 136 (EUR 17) for a visit at a general practitioner and NOK 307 (EUR 37) for an outpatient consultation at a hospital, up to a maximum of NOK 2040 per year (USD 342/EUR 253), after which further treatment was free of charge (www.helsenorge.no/betaling-for-helsehjelp/betaling-hos-lege#Egenandeler). In 2010, examinations with DXA were available at a total of 26 different centers. Most DXA machines are located on and owned by public hospitals; however, some are also operated by private radiology centers or private health institutions with public reimbursement agreements. Generally, diagnosis and treatment of secondary osteoporosis are handled by endocrinologists or rheumatologists while primary physicians are caretakers of primary osteoporosis.
In Norway, a case-finding strategy for osteoporosis has been employed, focusing on patients at risk of secondary osteoporosis, with previous low-energy fractures or two or more risk factors for osteoporosis (smoking, known alcohol abuse, menopause before age 45, parental low-energy fractures, supraphysiologic glucocortioid treatment, BMI < 19 kg/m2 or medical conditions associated with increased risk of osteoporosis) [15]. As of today, the concept of Fracture Liaison Service has only been implemented in the Hospital of Southern Norway in Kristiansand. Thus, only DXA on individuals with manifest osteoporosis or 2+ risk factors were partly reimbursed by the Norwegian health authorities (individual co-payment as for outpatient consultation as previously described), but individuals not fulfilling these criteria could also be examined if agreeing to pay market price, typically around NOK 600 (EUR 72) for a DXA.
No data, however, exist regarding the effectiveness of this approach.
The aim of the present study was to determine the use of DXA scans in Norway in relation to clinical risk factors and to elucidate whether age, sex, or distance to DXA clinics constitute potential barriers for the case-finding strategy in Norway.
Methods
Design
The study was a nationwide, population-based cross-sectional study of 6000 men and 6000 women aged 40–90 years, drawn from the Norwegian Civil Registration System. Due to the expectation that participants in the lowest and in the two highest age decades (40–49, 70–79, and 80–89 years of age) would have lower than average participation rates, the sample was stratified by age decades so that appropriately large populations for each decade were available for statistical analysis. For the age groups 40–49/50–59/60–69/70–79/80–89 years of age, randomly selected samples of 1250/1000/1000/1250/1500 participants were drawn from the Civil Registration System. These numbers were chosen as power calculations showed the need for 579 responses in each age group in order to achieve 80 % power (alfa 0.05) to detect a difference in prevalence between groups of risk factors with a prevalence of 0.5 vs. 2.5 % (e.g., use of glucocorticoids).
In January 2010, participants were mailed a personal letter with an invitation to participate in the study and a prepaid return envelope. A questionnaire concerning risk factors for fractures was attached. Returned and signed questionnaires were considered informed consent for inclusion in data analysis. A single reminder including a questionnaire was mailed to non-responders after 8 weeks.
Sources of data
Questionnaire
The questionnaire was based on known risk factors for osteoporosis and included all risk factors incorporated in but not limited to the WHO FRAX (www.shef.ac.uk/FRAX/), containing the following items: body weight, height, ethnicity, history of osteoporosis, DXA scans and anti-osteoporotic treatment, personal and first degree relatives’ history of fractures, history of falls and immobilization, smoking habits and alcohol consumption, use of oral glucocorticoids (GCs), and conditions associated with secondary osteoporosis (rheumatoid arthritis, osteogenesis imperfecta, diabetes, hyperthyroidism, chronic malnutrition or malabsorption, chronic liver diseases, hyperparathyroidism, hypogonadism and history of hormone replacement therapy). The questionnaire for women was identical to the questionnaire used in Denmark by Rubin et al. [12], translated to Norwegian by the first author (MPH) and tested in a pilot version on 25 unselected men and 25 unselected women within the appropriate age group with outpatient appointments at the Hospital of Southern Norway for various reasons. All 50 participants were interviewed after completing the questionnaire, and some questions were rephrased in the final questionnaire to ensure optimal understanding of the questions. Most questions (apart from height and weight) were categorical of nature and divided into “yes,” “no,” or “don’t know.”
The reliability of the questionnaire was examined by comparison of answers from 117 participants completing the questionnaire twice within an 8-week interval. Testing agreement with Cohen’s kappa for categorical variables, values between 0.833 and 1.000 were achieved, with a mean of 0.938, indicating overall excellent agreement [16].
Returned questionnaires were digitalized by optical character recognition using a Kodac i640 scanner and AnyDoc 5.0 software. The accuracy of this setup was previously found to be optimal by Rubin et al. [12].
Scanned questionnaires containing equivocal digitalized values were reexamined manually by MPH in order to optimize validity of data.
FRAX calculation
The 10-year probability of a major osteoporotic fracture was calculated using the desktop version of FRAX (FRAX version 3.8) for Norway, based on self-reported risk factors from the questionnaires.
Casewise deletion was applied for missing values when weight or height values were missing, as FRAX calculations were impossible. For other dichotome values incorporated in FRAX, missing values and the answer category “don’t know” were regarded as non-existence of the respective risk factor for the individual participant in question. Finally, casewise deletion was applied for weight outside the allowable range for FRAX (25–125 kg), as FRAX calculation was impossible for this group.
Distance to osteodensitomety (DXA) facilities
The distance from the participant’s postal address to nearest DXA facility was determined for each participant by a programmed call to a Norwegian route planner web site (www.langtved.dk).
Statistics
Due to stratification and the use of survey data, survey mode (STATA prefix: svy) and weights corrected for the relative proportion of age- and sex-specific strata as compared to the background population of Norway were applied. Data are shown as mean ± SD or median (range) as appropriate. Differences between groups were analyzed using chi-squared test for binary and categorical data and t test for continuous data. Univariate and multivariate logistic regression analyses were performed with reported history of DXA scan as the dependent variable, taking account of interaction terms. Independent variables were dichotomized in accordance with FRAX’ definition of risk factors (www.shef.ac.uk/FRAX/). Distance to DXA clinic was arbitrarily categorized to <10 km, 10–100 km, and >100 km. Age groups of <65, ≥65, and ≥80 years of age as well as FRAX 10-year fracture risk groups (<15, 15–19.9, 20–24.9, and 25+ %) were arbitrarily defined. Finally, participants were grouped according to the multitude of reported risk factors (0, 1, 2, 3+) as defined by the national Norwegian health authorities [15]. Hosmer and Lemeshow goodness-of-fit test was used to assess the adequacy of the model used in the multivariate logistic regression analysis.
Ethics
The study was approved by the Regional Ethics Committee of South-Eastern Norway (REK Sør-Øst B reference number: 2009/1809b).
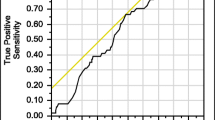
Results
As illustrated in Fig. 1, a total of 6332 (52.8 %) responses were registered. Among these were 97 written refusals to participate and 41 letters from spouses or children explaining why participation was impossible (dementia as the numerically most important reason), 117 responses were double responses and another 48 were incomplete and also excluded. A total of 3038 (50.6 %) questionnaires from women and 2991 (49.9 %) from men were included in the study.
Prevalence of risk factors
Prevalence of risk factors for osteoporosis and likelihood of having been examined by DXA are shown in Table 1.
Current smoking was the most prevalent risk factor reported by 18.3 % of women and 16.2 % of men. More women than men reported conditions associated with secondary osteoporosis and included in the FRAX tool, with prevalence rates of 23.0 and 7.1 %, respectively. This difference in prevalence was primarily due to a higher prevalence of reported premature menopause vs. hypogonadism as well as reported hyperthyroidism, known rheumatoid arthritis, and GC among women. Only reported ethanole intake >36 g/day and previous immobilization >1 month were more prevalent among men than women with 2.1 vs. 0.7 % of men/women reporting increased ethanol intake and 10.6 vs. 7.9 % reporting previous immobilization. Rates of BMI < 19 kg/m2, diabetes type 1, inflammatory bowel disease, celiac disease, chronic liver disease, anorexia nervosa, hypercalcemia, and osteoporosis imperfecta were all less than 4 % and therefore not shown in Table 1.
Risk factors for osteoporosis and history of DXA scan
Table 2 illustrates the distribution of history of DXA according to total number of risk factors for osteoporosis in women and men. Reported DXA scan rates by known risk factor varied widely both for women and men. Overall, the examination rate for men was lower than for women (3.7 vs. 22.3 %, p < 0.001).
As seen in Table 2, more women and men above the age of 65 years reported having had an examination, irrespective of the number of reported risk factors. A significantly larger proportion of intermediate-to-high-risk individuals (two or more risk factors) than low risk (no risk factors) reported an earlier DXA scan. However, 13.2 % of women and 1.5 % of men without known risk factors also reported an earlier DXA scan. Thus, in our population, 19.5 % of reported DXA among women and 16.2 % among men had been performed on subjects without any known risk factor for osteoporosis. Taking account of the age stratification in our population and assuming that our population is a true cross-sectional sample of the Norwegian population, estimated percentages of DXA performed in subjects without any risk factor for osteoporosis was 18.9 % for women and 15.5 % for men, respectively.
Ten-year risk of major osteoporotic fracture (FRAX) and history of DXA
Table 3 describes DXA rates in regards to an integrated estimated risk of future osteoporotic fractures, using the FRAX algorithm. For these figures, 3030 women and 2971 men were available, due to casewise deletions of 8 women and 20 men reporting body weight above the allowable weight range (25–125 kg) for FRAX.
A total of 12.4 % of women with an estimated 10-year fracture risk of <15 % had a history of DXA. Significant increases in reported scanning rates (p < 0.05) with increasing 10-year fracture risk were found for women for all groups except when comparing the intermediate risk groups of 15–19.9 vs. 20–24.9 %. The trend for increasing reported examination rates with increasing 10-year probability of fracture was consistent for women both above and below the age of 65. However, a significantly higher proportion of women <65 years of age with high fracture risk (FRAX 10-year risk >25 %) than women above 65 years of age with the same FRAX risk reported a DXA. The increase in DXA rate for elderly women seemed to be primarily due to examination of more low-risk women (FRAX score <15 %) in this age group.
Reported DXA rates were much lower in men than women for the same FRAX 10-year fracture risk, and no general trend of increasing examination rates with increasing 10-year risk of fracture risk could be found. As in women, higher overall scanning rates for men aged 65 years or more was primarily due to more examinations of men in the low-risk group (FRAX 10-year risk <15 %).
Distance to DXA facility and reported DXA rates
The median distance to nearest DXA facility for women and men was 21.9/23.5 km (interquartile range 7.6–55.5/8.1–57.6 km) with maximum distances of 862/864 km, respectively. Table 4 shows reported DXA examination rates by distance between home address and nearest DXA facility. There was a clear increase in examination rates for women living closer to a DXA facility (<100 km) compared to women living further away for all age groups. The tendency of increasing examination rates with age was independent of distance to DXA facility.
Among women with highest risk of fracture (10-year risk of major osteoporotic fracture as calculated by FRAX > 25 %), 48.4 % of the women living closer to a DXA facility than 10 km had had a DXA examination while only 24.7 % of the women living >100 km away reported an examination (p = 0.02). Similarly, men living closer to the nearest DXA facility than 100 km reporting increased examination rates with age.
Importance of risk factors for osteoporosis for probability of reporting a DXA
Table 5 summarizes calculated odds ratios for reporting a DXA examination, dependent upon risk factors for osteoporosis. For both women and men, history of treatment with GC incurred the highest odds ratio for an earlier DXA examination in both univariate and multivariate analyses. Most other known risk factors for osteoporosis were also associated with an increased likelihood of having been examined by DXA. However, the osteoporotic risk factor current smoking seemed to be a negative predictor for having been examined with DXA (p = 0.001). For men, the examination rate for this subgroup was also numerically lower than average, without reaching significance.
Hosmer Lemeshow goodness of fit (p value of 0.951/0.981 for women/men) showed no evidence against the proposed models in multivariate analyses.
Discussion
This study showed a positive correlation between most known risk factors for osteoporosis and the probability of reporting a DXA examination for both men and women. However, scanning rates for high-risk groups defined by a higher number of prevalent risk factors seemed attenuated, especially so in men. The higher scanning rates in elderly men and women were due to additional examinations performed on low-risk individuals. For similar absolute fracture risk estimated by FRAX, lower scanning rates for men compared to women were found. For women, distance to nearest DXA correlated inversely with the probability of having had a DXA scan.
Overall, this study showed that age, male sex, and distance to DXA clinics all constitutes potential barriers for the case-finding strategy in Norway.
Below, the individual risk factors are discussed in detail.
A statistically significant increased likelihood of reporting a DXA was found with increasing age. This could be due to an increase in the number of prevalent risk factors with age—even though increased scanning rates per se seemed to be attenuated with increasing number of risk factors. Alternatively, this increase in reported DXA examination with age could be due to either awareness of age as an important risk factor for osteoporosis among primary physicians or in the general population or due to a constant and thus additive likelihood of DXA referral with increasing age. Which of these explanatory factors are of importance cannot be elucidated from our dataset as the proposed question in our study was phrased as to whether or not the participant had ever been DXA scanned. Comparing scanning rates with other published studies, our participants with an age above 80 years reported a previous DXA in 32.7 % of cases as compared to Rubin et al.’s 22.8 % [12], and the scanning rate overall at 22.8 % seems higher than the 17.2 % reported from Denmark. Frost et al. reported results from a population-based questionnaire among men aged 60–74 years [13]. Here, a previous scanning was reported by 2.7 % of the participants. In our study, the total scanning rate was higher both for all men at 3.7 % as well as for this particular age group at 4.8 %.
Smoking was reported by 18.3 % of participating women and 16.2 % of participating men, but even though smoking is a well-known risk factor for osteoporosis, a negative effect of smoking on screening rates for osteoporosis was found among women. This finding is in concord with previous findings from Rubin et al. [12]. As prevalence rates of daily smoking also have been shown to be inversely correlated to education in Europe [17], the lower examination rates among smokers is a contributing factor to inequalities in health in Norway. The prevalence of smoking in the study population was in concord with reported rates from the Tromsø VI study [18], even though they were lower than findings from the Statistical Bureau of Norway [19], with reported rates of active smoking of 21 % among both men and women in 2008. However, they were higher than reported rates from other cohorts investigating fracture risk such as the COSHIBA cohort [20], a cohort of females from Puerto Rico [21], the Heartfordshire cohort [22] as well as a regional cohort from Spain [23], even though Norway is known for a restrictive public smoking policy.
In this study, 3.3 % of women and 2.4 % of men reported previous or current GC treatment. The uptake of DXA in this population was 61.0 and 30.1 %, respectively. Rates of reported current or previous GC treatment was in concord with previously reported rates from Denmark (4.5 % among women, [12]) and also comparable to earlier reported rates of previous (4.5 % [24]) and current reported CG use of 0.5–1.2 % [25]. Uptake of DXA among women reporting CG treatment was higher than the 52.3 % reported by Rubin et al. for women [12] and higher than reported rates for men in Denmark of 10–15 % [13].
A total of 14.9 % of women and 5.2 % of men reported a previous low-energy fracture, comparable to rates among women in Denmark of 11.5 % [12] and supporting newly published incidence rates of forearm fractures from Denmark similar to studies from Sweden and Norway [26]. For women above 65 years of age, the reported prevalence was 23.6 %, comparable to 29.7 % of US citizens using Medicare estimates for the USA [27] but higher than official estimates for Denmark and Sweden [28]. In our study, the uptake of DXA was 42.9 % among women and 9.0 % among men with reported low-energy fractures. Significantly lower uptake rates in men than in women suggest that osteoporosis is still viewed as a disease affecting women, even though male–female incidence ratios internationally are relatively stable around 1:2 [29] and men are known to have higher age-adjusted mortality rates than women after a hip fracture [30].
Increasing scanning rates were found for increasing FRAX risk score. Generally, scanning rates were higher than comparable rates for women by Rubin et al. [12]. However, for elderly women, increased scanning rates seemed to be due to increased scanning rates in lower risk participants, a tendency also found in Danish women [12]. Thus, one can speculate as to whether or not age as a risk factor in the currently applied case-finding strategy seems to be overemphasized while other risk factors are overlooked. An objective, low-cost, risk factor-based summarized risk score such as FRAX or others with equal discriminative value [31] would seem to be feasible as a stratification tool for the current case-finding strategy.
Increasing distance to nearest DXA facility was inversely related to the probability of reporting a DXA examination—at least for women. For men, this was not the case, most likely due to lower scanning rates overall and thus lower power to detect a true effect, as calculated odds ratios suggested an effect (however non-significant). Most worrisome was the significantly lower scanning rates for high-risk women with a FRAX 10-year risk of fracture >25 % living >100 km from a DXA facility. The scanning rates for these women were lower than relatively low-risk patients (FRAX score <15 %) living <10 km from a DXA facility. Thus, this study reinforces the need for cheaper and more available diagnostic equipment or stratification tools with high discriminatory power, especially in a country such as Norway, where >10 % of the population in our study lived more than 100 km from the nearest DXA center. Promising equipment for (pre) screening could be phalangeal densitometry [32] or quantitative ultrasound [33]. Several more or less simplistic stratification tools for this purpose are now available as discussed elsewhere [31].
Under-diagnosis of osteoporosis and overuse of DXA in low-risk patients
Osteoporosis remains an under-diagnosed disease in Norway as in other parts of the world, partly due to the fact that the uptake of DXA examinations is far from optimal. As shown in our study, only 30.4 % of all women and 11.9 % of all men reporting three or more known risk factors for osteoporosis reported a previous DXA examination. Using 10-year risk of major osteoporotic fracture as defined by FRAX and defining high-risk groups as participants with a 10-year risk of 25+ %, the examination rates remained low at 39.5 and 12.2 % for women and men, respectively.
Adding to the problem, 19.5 % of all reported examinations in this cross-sectional nationwide study was by women with absolutely no known risk factors for osteoporosis whatsoever. For men, 16.2 % (18/111) of all reported examinations were on participants without known risk factors for osteoporosis. This study is in concord with similar figures reported in Danish women [12] and in Danish men [13].
Limitations
Our study had limitations. The available data on risk factors were self-reported and not double-checked with health records in hospitals or from general practitioners and thus prone to recall bias and information bias. Falsely low and high rates of risk factors or DXA rates could be the result. However, as discussed in the results section, the prevalence of the risk factors smoking, previous/current CG use, and history of low-energy fracture indicated a true population-based sample and thus at the same time decreasing the likelihood of recall and information bias. Secondly, the calculated distances to nearest DXA facility could be biased for the subgroup of participants who reported having had a DXA examination, as participants were not asked to state the location of the examination nor their address at the time of scanning. Migration after the reported examination thus could not be excluded and constituted a possible source of bias.
Selection bias could have been introduced due to the stratification of potential participants in not equally sized age groups. However, this was done to increase potential power in our calculations. Due to the Norwegian Civil Registration System, the total number of inhabitants in Norway for each age group was known, and thus, it was possible, using the reciprocal of the probability for an individual to be sampled as a factor, to cancel the effect of this possible selection bias on a statistical level.
Rates of participation were modest, however comparable with other studies [34–36]. Due to restrictions by the Norwegian Civil Registration system, more than one letter of reminder was not allowed and incentives were not provided.
Participants with missing values for height and weight were dropped. An imputation model, using values from next case or mean/mode substitution, was considered but were judged to be associated with possibly very falsely BMI and FRAX values, and as the number of missing cases was low, casewise deletion was performed instead. Potential bias by this method could not be excluded, but we estimated the risk to be low due to the low number of missing values.
Results for FRAX and distance to DXA were reported using arbitrarily chosen cutoff values. Using categorical variables for FRAX introduced a possible loss of information in our data analysis. However, this did not seem to be of importance, as our findings suggest differences in FRAX risk categories for women between those who had reported a DXA and those who did not. For men, this was not the case, most likely due to small numbers.
For our study, the non-response rate could pose problems with generalizing data. However, reported rates of smoking indicate that participants were representable for the whole population, and reported use of corticosteroids as an indicator of the generalizability of the survey results was comparable to other studies.
Our study, however, also had a number of strengths. Firstly, this is the first national population-based survey of risk factors for osteoporosis in Norway. Secondly, it includes both men and women while the majority of earlier research has been on women. Finally, the applied questionnaire had been validated in a pilot study, and optical character recognition was used for data entry in order to reduce erroneous entries.
Conclusion
Our study showed suboptimal screening rates for osteoporosis among Norwegian high-risk individuals, especially so for men. Furthermore, increased distance to nearest DXA facility reduced the probability of having undertaken a DXA scan. A high proportion of DXA scans were performed in people not included in the Norwegian screening strategy aimed at high-risk individuals.
Our study reinforces the need to (a) develop cheap and more available diagnostic tools for osteoporosis and/or (b) use easily accessible non-interventional stratification tools to improve the pretest probability of osteoporosis and thus increase the gradient of risk for examined individuals. A number of stratification tools based on one or more anamnestic risk factors already exist and should be employed more extensively.
References
(2003) Prevention and management of osteoporosis. World Health Organ Tech Rep Ser 921:1–164, back cover
Kanis JA, Gluer CC (2000) An update on the diagnosis and assessment of osteoporosis with densitometry. Committee of scientific advisors, international osteoporosis foundation. Osteoporos Int: J Establish Res Coop Eur Found Osteoporos Natl Osteoporos Found USA 11:192–202
Lim LS, Hoeksema LJ, Sherin K (2009) Screening for osteoporosis in the adult U.S. population: ACPM position statement on preventive practice. Am J Prev Med 36:366–375
Watts NB, Adler RA, Bilezikian JP, Drake MT, Eastell R, Orwoll ES, Finkelstein JS (2012) Osteoporosis in men: an endocrine society clinical practice guideline. J Clin Endocrinol Metab 97:1802–1822
Kanis JA, McCloskey EV, Johansson H, Cooper C, Rizzoli R, Reginster JY (2013) European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos Int: J Establish Res Coop Eur Found Osteoporos Natl Osteoporos Found USA 24:23–57
Compston J, Cooper A, Cooper C, Francis R, Kanis JA, Marsh D, McCloskey EV, Reid DM, Selby P, Wilkins M (2009) Guidelines for the diagnosis and management of osteoporosis in postmenopausal women and men from the age of 50 years in the UK. Maturitas 62:105–108
Brennan SL, Wluka AE, Gould H, Nicholson GC, Leslie WD, Ebeling PR, Oldenburg B, Kotowicz MA, Pasco JA (2012) Social determinants of bone densitometry uptake for osteoporosis risk in patients aged 50yr and older: a systematic review. J Clin Densitom Off J Int Soc Clin Densitom 15:165–175
Brennan SL, Henry MJ, Kotowicz MA, Nicholson GC, Zhang Y, Pasco JA (2011) Incident hip fracture and social disadvantage in an Australian population aged 50 years or greater. Bone 48:607–610
Guilley E, Herrmann F, Rapin CH, Hoffmeyer P, Rizzoli R, Chevalley T (2011) Socioeconomic and living conditions are determinants of hip fracture incidence and age occurrence among community-dwelling elderly. Osteoporos Int: J Establish Res Coop Eur Found Osteoporos Natl Osteoporos Found USA 22:647–653
Icks A, Haastert B, Wildner M, Becker C, Rapp K, Dragano N, Meyer G, Rosenbauer J (2009) Hip fractures and area level socioeconomic conditions: a population-based study. BMC Public Health 9:114
Johnell O, Borgstrom F, Jonsson B, Kanis J (2007) Latitude, socioeconomic prosperity, mobile phones and hip fracture risk. Osteoporos Int: J Establish Res Coop Eur Found Osteoporos Natl Osteoporos Found USA 18:333–337
Rubin KH, Abrahamsen B, Hermann AP, Bech M, Gram J, Brixen K (2011) Prevalence of risk factors for fractures and use of DXA scanning in Danish women. A regional population-based study. Osteoporos Int: J Establish Res Coop Eur Found Osteoporos Natl Osteoporos Found USA 22:1401–1409
Frost M, Gudex C, Rubin KH, Brixen K, Abrahamsen B (2012) Pattern of use of DXA scans in men: a cross-sectional, population-based study. Osteoporos Int: J Establish Res Coop Eur Found Osteoporos Natl Osteoporos Found USA 23:183–191
Statistisk-Sentralburå (2010) Statistisk Årbok 2010. https://lovdata.no/dokument/SF/forskrift/2007-12-19-1761#KAPITTEL_4. Accessed Jun 2014
Helsedirektoratet (2006) Faglige retningslinjer for forebygging og behandling av osteoporose og osteoporotiske brudd. Sosial-og helsedirektoratet, Avdeling for primærhelsetjenester, Pb 7000, N-0130 Oslo
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33:159–174
Huisman M, Kunst AE, Mackenbach JP (2005) Inequalities in the prevalence of smoking in the European Union: comparing education and income. Prev Med 40:756–764
Waterloo S, Nguyen T, Ahmed LA, Center JR, Morseth B, Nguyen ND, Eisman JA, Sogaard AJ, Emaus N (2012) Important risk factors and attributable risk of vertebral fractures in the population-based tromso study. BMC Musculoskelet Disord 13:163
Statistisk-Sentralburå (2014) Røykevaner, 2013. http://ssb.no/royk/. Accessed 20 Feb 2014
Clark EM, Gould VC, Morrison L, Masud T, Tobias J (2012) Determinants of fracture risk in a UK-population-based cohort of older women: a cross-sectional analysis of the cohort for skeletal health in bristol and avon (COSHIBA). Age Ageing 41:46–52
Haddock L, Ortiz V, Vazquez MD, Aguilo F, Bernard E, Ayala A, Mejias N (1996) The lumbar and femoral bone mineral densities in a normal female Puerto Rican population. P R Health Sci J 15:5–11
Edwards MH, Jameson K, Denison H, Harvey NC, Sayer AA, Dennison EM, Cooper C (2013) Clinical risk factors, bone density and fall history in the prediction of incident fracture among men and women. Bone 52:541–547
Sanfelix-Gimeno G, Sanfelix-Genoves J, Hurtado I, Reig-Molla B, Peiro S (2013) Vertebral fracture risk factors in postmenopausal women over 50 in Valencia, Spain. A population-based cross-sectional study. Bone 52:393–399
Kanis JA, Johansson H, Oden A et al (2004) A meta-analysis of prior corticosteroid use and fracture risk. J Bone Miner Res Off J Am Soc Bone Miner Res 19:893–899
Overman RA, Toliver JC, Yeh JY, Gourlay ML, Deal CL (2014) U.S. adults meeting 2010 American College of Rheumatology criteria for treatment and prevention of glucocorticoid-induced osteoporosis. Arthritis Care Res
Abrahamsen B, Jorgensen NR, Schwarz P (2014) Epidemiology of forearm fractures in adults in Denmark: national age- and gender-specific incidence rates, ratio of forearm to hip fractures, and extent of surgical fracture repair in inpatients and outpatients. Osteoporos Int: J Establish Res Coop Eur Found Osteoporos Natl Osteoporos Found USA
Cheng H, Gary LC, Curtis JR, Saag KG, Kilgore ML, Morrisey MA, Matthews R, Smith W, Yun H, Delzell E (2009) Estimated prevalence and patterns of presumed osteoporosis among older Americans based on Medicare data. Osteoporos Int: J Establish Res Coop Eur Found Osteoporos Natl Osteoporos Found USA 20:1507–1515
Svedbom A, Hernlund E, Ivergard M, Compston J, Cooper C, Stenmark J, McCloskey EV, Jonsson B, Kanis JA (2013) Osteoporosis in the European Union: a compendium of country-specific reports. Arch Osteoporos 8:137
Kanis JA, Oden A, McCloskey EV, Johansson H, Wahl DA, Cooper C (2012) A systematic review of hip fracture incidence and probability of fracture worldwide. Osteoporos Int: J Establish Res Coop Eur Found Osteoporos Natl Osteoporos Found USA 23:2239–2256
Haentjens P, Magaziner J, Colon-Emeric CS, Vanderschueren D, Milisen K, Velkeniers B, Boonen S (2010) Meta-analysis: excess mortality after hip fracture among older women and men. Ann Intern Med 152:380–390
Rubin KH, Abrahamsen B, Friis-Holmberg T, Hjelmborg JV, Bech M, Hermann AP, Barkmann R, Gluer CC, Brixen K (2013) Comparison of different screening tools (FRAX(R), OST, ORAI, OSIRIS, SCORE and age alone) to identify women with increased risk of fracture. A population-based prospective study. Bone 56:16–22
Dhainaut A, Rohde G, Hoff M, Syversen U, Haugeberg G (2011) Phalangeal densitometry compared with dual energy X-ray absorptiometry for assessment of bone mineral density in elderly women. J Women’s Health 20:1789–1795
Pisani P, Renna MD, Conversano F, Casciaro E, Muratore M, Quarta E, Paola MD, Casciaro S (2013) Screening and early diagnosis of osteoporosis through X-ray and ultrasound based techniques. World J Radiol 5:398–410
Kmetic A, Joseph L, Berger C, Tenenhouse A (2002) Multiple imputation to account for missing data in a survey: estimating the prevalence of osteoporosis. Epidemiology (Cambridge, Mass) 13:437–444
Christensen AI, Ekholm O, Glumer C, Andreasen AH, Hvidberg MF, Kristensen PL, Larsen FB, Ortiz B, Juel K (2012) The Danish national health survey 2010. Study design and respondent characteristics. Scand J Public Health 40:391–397
Langhammer A, Krokstad S, Romundstad P, Heggland J, Holmen J (2012) The HUNT study: participation is associated with survival and depends on socioeconomic status, diseases and symptoms. BMC Med Res Methodol 12:143
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Høiberg, M.P., Rubin, K.H., Gram, J. et al. Risk factors for osteoporosis and factors related to the use of DXA in Norway. Arch Osteoporos 10, 16 (2015). https://doi.org/10.1007/s11657-015-0220-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11657-015-0220-9