ABSTRACT
BACKGROUND
The use of computers to deliver education and support strategies has been shown to be effective in a variety of conditions. We conducted a systematic review and meta-analysis to evaluate the impact of computer-based technology on interventions for reducing weight.
METHODS
We searched MEDLINE, CENTRAL, CINAHL, PsycINFO, Google Scholar and ClinicalTrials.gov (all updated through June 2010) for randomized controlled trials evaluating the effect of computer-based technology on education or support interventions aimed at reducing weight in overweight or obese adults. We calculated weighted mean differences (WMD) and 95% confidence intervals (CI) using random effects models.
RESULTS
Eleven trials with 13 comparisons met inclusion criteria. Based on six comparisons, subjects who received a computer-based intervention as an addition to the standard intervention given to both groups lost significantly more weight (WMD −1.48 kg, 95% CI −2.52, –0.43). Conversely, based on six comparisons, subjects for whom computer-based technology was substituted to deliver an identical or highly comparable intervention to that of the control group lost significantly less weight (WMD 1.47 kg, 95% CI 0.13, 2.81). Significantly different weight loss seen in “addition” comparisons with less than six months of follow-up (WMD −1.95 kg, 95% CI −3.50, –0.40, two comparisons) was not seen in comparisons with longer follow-up (−1.08 kg, 95% CI −2.50, 0.34, four comparisons). Analyses based on quality and publication date did not substantially differ.
CONCLUSIONS
While the addition of computer-based technology to weight loss interventions led to statistically greater weight loss, the magnitude (<1.5 kg) was small and unsustained.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
BACKGROUND
Obesity is a significant problem in the United States and the world. According to the Centers for Disease Control and Prevention, 68% of adults in the U.S. are overweight or obese.1 More globally, the World Health Organization estimates that 1.5 billion adults are overweight and that nearly 500 million are obese.2 These rates have increased dramatically since the 1970s for individuals of all ages, sexes, ethnic groups, and educational levels.3 Overweight and obesity in adults are linked to increased risk for a number of serious conditions, including heart disease, diabetes, hypertension, hyperlipidemia, and certain types of cancers.4 Expenditures related to overweight and obesity are estimated to account for greater than 9% of annual spending on health care in the U.S.5
There is general agreement that population-based, multi-level approaches that focus on prevention are needed to treat the obesity epidemic.6,7 Such approaches recognize and address the social, behavioral, and economic determinants of obesity in terms of both interventions and policy.7 However, at the level of individual patients, primary health care plays an increasingly important role in identifying and treating overweight and obesity.8 Most approaches rely on changes in diet and physical activity aimed at decreasing energy consumption while increasing energy expenditure.7,8 Studies have suggested that incorporating behavior modification or principles of social learning, such as goal-setting and self-monitoring, can improve the efficacy of these approaches.9–11 While the U.S. Preventive Services Task Force has recommended that, “clinicians screen all adult patients for obesity and offer intensive counseling and behavioral interventions to promote sustained weight loss for obese adults,”12 fewer than 50% of obese patients are actually counseled by their health care providers to lose weight.13,14 Numerous barriers to implementing these recommendations have been described, including lack of time and training on the part of health care providers, lack of reimbursement, lack of interest and motivation on the part of patients, and perhaps most discouraging, lack of proven interventions.15–18
To overcome some of these barriers, an increasing number of weight loss interventions have used computer technology to deliver education, support, and self-monitoring strategies.19–22 It has been suggested that the interactive nature of computers provides a persuasive advantage when compared to other media23 and assists social learning by providing users with feedback, modeling of desired attitudes or behaviors, and social dynamics and support.24,25 Such interventions have been found to be useful in treating a variety of conditions including depression26 and post-traumatic stress disorder,27 and in promoting self-management of chronic disease.28 Additionally, a meta-analysis of the effectiveness of Web-based interventions found an improvement in behavioral change outcomes.29 Based on these findings, some have hypothesized that using computer-based technology to deliver or facilitate current weight loss interventions in overweight and obese adults could improve their often modest efficacy.29 This potential, along with calls for providers to use computer-and Web-based resources as supplements to patient care,30,31 begs the question: should providers consider computer-based interventions to promote weight loss for their overweight or obese patients?
While a handful of narrative or systematic reviews9,32–34 and one meta-analysis35 of computer-based interventions to assist in weight loss already exist, none has explicitly focused on evaluating the independent effect a computer delivery modality might have on the effectiveness of a weight loss intervention. To more closely address this objective, we conducted a systematic review and meta-analysis of randomized controlled trials comparing the effectiveness of computer-based interventions versus non-computer-based interventions for reducing weight or BMI among overweight and obese adults.
METHODS
We utilized the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) statement, explanation and elaboration document,36,37 and checklist to guide our methodology and reporting.
Review Protocol
We modified and expanded an existing protocol38 to structure our review and analysis of potential studies. Appendix 1 (available online) details changes to this protocol over the period of this systematic review.
Study Eligibility Criteria
Studies were included for analysis if they met the following criteria: 1) the design was a randomized controlled trial; 2) the intervention included computer-based education or support aimed at reducing weight or body mass index (BMI); 3) the comparison group received a non-computer-based intervention; 4) the study participants were adults who were overweight or obese as defined by the CDC39 and 5) the study evaluated change in weight and/or BMI, our primary outcomes of interest. While assessing study eligibility, we noted that there were two general approaches to evaluating the effect of computer-based technology on weight loss interventions—either as an additional modality (both groups receive an identical or highly comparable non-computer-based intervention but one group also receives a supplementary computer-based intervention), or as a substituted modality (an identical or highly comparable intervention is delivered to both groups, either with or without a computer). We allowed studies taking either approach as both were relevant to our study question and each might provide different insights. We excluded studies that required subjects to have lost weight before participating as these studies focused on weight maintenance, not reduction, and their populations may be less representative of the general population of adults who are overweight or obese. Appendix 2 (available online) provides a detailed list and description of our study inclusion criteria and outcomes of interest.
Search Methods
We searched MEDLINE (1950–June Week 2, 2010), the Cochrane Central Register of Controlled Trials (CENTRAL), the Cumulative Index of Nursing and Allied Health Literature (CINAHL) (1982–May, 2010), and PsycINFO (1806- June Week 2, 2010) during June, 2010 using three clusters of search terms describing ‘computer-assisted’ 'interventions’ for ‘obesity or overweight’. Appendix 3 (available online) provides details of the search strategy that was applied to each electronic database. These searches utilized no constraints on language, date, or publication status. The searches were supplemented by searches of Google Scholar and a clinical trials registry (ClinicalTrials.gov). The abstract of each study identified by our search was assessed for eligibility by one of four reviewers using a standardized approach. For studies that could not be excluded by abstract review, full text versions (n = 98) were obtained and assessed by two independent reviewers using the same standardized approach. Disagreements between reviewers were resolved via consensus. Lastly, the reference sections of studies that met our inclusion criteria were scanned for additional studies.
Data Collection
For studies that met our inclusion criteria, two teams of two independent reviewers extracted relevant information (each pair independently extracted data from half the included articles). We used a standard data extraction template, shown in Appendix 4 (available online) which was first pilot-tested on six randomly selected articles and refined accordingly. Information extracted from each study included: 1) characteristics of trial participants; 2) descriptions of the intervention and comparison; 3) results and duration of follow-up; and 4) assessment of risk of bias using the Risk of Bias tool recommended in the Cochrane Handbook for Systematic Reviews of Interventions.40 This tool includes six items shown to be important for assessing the risk of bias in randomized trials, each of which is scored as “yes” (low risk of bias), “no” (high risk of bias), or “unclear” (not enough information to assess the risk of bias), as shown in Appendix 5 (available online). Disagreements during the data extraction phase were resolved by discussion and consensus among each pair of reviewers. If additional input was needed, one or both of the other reviewers was consulted.
Analysis
Measure of Effect and Data Synthesis
We followed recommendations from the Cochrane Collaboration41 for data synthesis and used RevMan 5 software42 to perform all meta-analytic statistics. The primary outcome measures were change from baseline in weight and BMI. After conversion to a standard metric (e.g., pounds to kilograms), we used random effects models to calculate pooled weighted mean differences (WMD) and 95% confidence intervals (95% CI). A p-value <0.05 for the test of overall effect was considered statistically significant. Because several studies did not provide standard deviations (SD) for the mean changes from baseline (required for pooling the WMDs), we used a formula recommended for estimating these values by using the means and SDs for the baseline and final measures and a correlation coefficient (R), which we set at 0.5.41 Similarly, when studies reported variance using standard errors or confidence intervals, we converted these to SDs using appropriate formulas.41
Missing Data
We contacted the authors of three studies43–45 that met inclusion criteria but did not report adequate outcome data to be included in the meta-analysis. While two provided the needed data, for the third (Agras et al.)45 we imputed pre- and post-intervention standard deviations by generating a conservative estimate based upon pre- and post-standard deviations of the other study populations included in this review.
Assessment of Heterogeneity
We assessed for statistical variability among the studies contributing to each summary estimate by evaluating the p-value and I2 percentage provided with the test of heterogeneity in RevMan 5.42 We considered studies to be heterogeneous if the p-value was less than 0.10 or the I2 value41 exceeded 50%. If heterogeneity was present, we evaluated the results of the individual studies in an effort to identify obvious outliers, and performed sensitivity analyses in an effort to identify the largest group of studies that passed the test of heterogeneity.
Reporting Biases
We assessed for publication bias by plotting each study’s sample size by its effect size for both change in weight and change in BMI. We visually inspected the resulting funnel plots for evidence of publication bias.46
Subgroup Analyses
We performed a post hoc analysis based on the two methodological approaches we had identified during the study eligibility process—adding versus substituting a computer-based technology. Because the analysis suggested the two approaches led to statistically different findings, we performed three pre-specified subgroup analyses within these broader subgroups.
First, we assessed studies according to the duration of the intervention (less than six months versus six months or longer), since previous work suggests that interventions are more likely to be successful if they enhance participants’ long-term adherence and motivation.47 Second, we assessed studies according to the duration of follow-up (less than six months versus six months or longer), since it is known that early weight loss benefits are often not sustained over time.48,49 Third, we also grouped studies by publication date, considering those published prior to 1995 as one group and those published in 1995 or after as another. This cut-off was based on criteria utilized by other reviews34,35 that considered 1995 a pivotal year in terms of Internet availability.
Sensitivity Analyses
In order to evaluate the effect of methodological quality on the summary estimates for our primary outcomes, we conducted sensitivity analyses based on each of the six methodological quality items contained in the Risk of Bias tool.40 Each analysis was restricted to the studies judged to have “low risk of bias” for the item of interest.
RESULTS
Study Selection
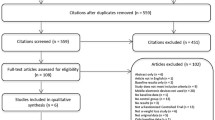
The search yielded a total of 2,832 titles. The initial screen identified 542 duplicates and 2,192 studies that did not fulfill one or more inclusion criteria based on abstract review. The remaining 98 studies were retrieved for full-text review. Ultimately, 11 randomized trials43–45,50–57 with 13 comparisons (two multi-arm studies43,44) met the inclusion criteria and provided usable data for meta-analysis. Complete information regarding the process from search results to included studies is provided in the Study Selection Flow Diagram (Fig. 1).
Study Characteristics
The 11 included studies (described in Table 1) involved 1866 participants, of which 990 received computer-based interventions and 876 received interventions delivered through modalities that did not include a computer. The interventions ranged from 2–12 months in length. Six studies (one multi-arm, leading to seven comparisons) added a computer-based tool to the intervention (“addition studies”) while five (one multi-arm, leading to six comparisons) substituted a computer-based tool (“substitution studies”). The addition studies included one that studied the effect of a computer program plus a workbook compared to use of the workbook alone,50 and six comparisons that examined the effect of behaviorally-based information or therapy delivered via the computer or Internet plus in-person sessions compared to in-person sessions that may have utilized additional paper materials.44,45,52–54
The substitution studies included three comparisons that studied use of a website, computer program, or PDA diary compared to a paper diary for self-monitoring,43,56 one comparison that studied the effect of information delivered via computer compared with the same information delivered in a classroom program,55 one comparison that examined the effect of information delivered via the Internet combined with e-mail counseling compared to paper-based information accompanied by phone counseling, 57 and one comparison that examined the effect of behaviorally-based information delivered via a website plus in-person sessions compared to in-person sessions with paper materials.51
Risk of Bias in Included Studies
Figure 2 provides the risk of bias findings for the included studies. Nine of the 11 studies provided insufficient information to adequately assess three or more bias categories. Seven studies did not provide adequate discussion of randomization techniques to assess potential selection bias, and only one study54 published their protocol on a publicly available trial registration site (clinicaltrials.gov), allowing for assessment of selective reporting. The most common reasons for “Other risks of bias” included requiring recipients of the intervention to pay a refundable deposit for technology, materials, or participation44,50,55 and potential conflicts of interest in which authors were involved in developing the computer product being studied.53
Risk of bias summary for included studies. + Study has a low risk of bias. - Study has a high risk of bias. ? Unclear or uncertain risk of bias. See Appendix 5 for more information.
Effects of Interventions
Change in Weight
Figure 3 displays the findings for change in weight, subgrouped by methodological approach. Based on six comparisons evaluating the effect of adding a computer-based intervention as a supplement to the standard weight loss intervention given to both study arms, subjects in the computer group lost significantly more weight (WMD −1.48 kg, 95% CI −2.52, –0.43, I2 = 0%). Based on six comparisons evaluating the effect of substituting a computer-based technology to deliver an identical or highly comparable intervention to that given to the control group, there was no difference between groups (WMD 0.36 kg, 95% CI −1.80, 2.53), however there was significant heterogeneity (p < 0.01, I2 = 65%). Sensitivity analysis revealed that removal of the Burnett study,56 the oldest (1985) and smallest (12 participants) study, resolved the heterogeneity (I2 = 0%) and revealed significant differences between subgroups suggesting that subjects in the computer “substitution” group lost significantly less weight (WMD 1.47 kg, 95% CI 0.13, 2.81). The test for subgroup differences comparing “addition” studies to the homogeneous group of “substitution” studies was highly significant (p = 0.0007).
Overall change in weight (kg), subgrouped by methodological approach (addition versus substitution of computer-based intervention). Test for subgroup differences comparing "addition of computer "to "substitution of computer-all studies": p = 0.07. Test for subgroup differences comparing "addition of computer" to "substitution of computer-excluding Burnett": p = 0.0007. kg = kilograms, SD = standard deviation, IV = inverse variance, CI = confidence interval.
Given the finding that only the “addition” studies resulted in a significant increase in weight lost, further subgroup analyses were performed only on this group of studies. These analyses revealed that an effect was seen in studies with less than six months of intervention (five comparisons) but was not seen in the one comparison that lasted longer (Fig. 4). Similarly, short-term follow-up (lasting less than six months) revealed an effect (two comparisons) that was not present in comparisons with longer follow-up (four comparisons) (Fig. 5). While the findings for comparisons published in 1995 or later had more favorable results than those published prior to 1995, the findings across subgroups were homogeneous (I2 = 0%), and the difference between subgroups was small (<1 kg) and non-significant (p = 0.82) (Fig. 6).
Change in BMI
Figure 7 shows the findings for BMI. Based on three comparisons evaluating the effect of adding a computer-based intervention as a supplement to the standard weight loss intervention given to both study arms, subjects in the computer group had a significantly greater reduction in BMI (WMD −0.43 kg/m2, 95% CI −0.83, –0.03, I2 = 0%). Based on three comparisons evaluating the effect of substituting a computer-based technology to deliver an identical or highly comparable intervention to that given to the control group, there was no difference between groups (WMD 0.44, 95% CI −1.15, 2.03, I2 = 0%). There were not adequate studies within the primary subgroups (addition versus substitution) to allow further subgroup analyses for the BMI outcome.
Sensitivity analyses restricted to studies with low risk of bias for each methodological quality item did not meaningfully change the magnitude or direction any of the summary estimates. Finally, the funnel plots for change in weight and BMI (Appendix 6, available online) were not suggestive of publication bias.
DISCUSSION
In recent years, it has been suggested that obesity is a chronic disease58 that could benefit from the types of management strategies inherent in the Chronic Care Model, including support for self-management.59 Use of the Internet for counseling has been included in a list of model components that have shown promising results.13 Griffiths and colleagues have noted that, “Evaluation of the effectiveness of a health care intervention delivered by the Internet needs to include comparison with more traditional modes of delivery to answer the following question: What are the added benefits or disadvantages of Internet use that are particular to this mode of delivery?”60 This systematic review and meta-analysis addresses this question more broadly by considering computer-assisted delivery with regard to the treatment of overweight and obesity. Our meta-analysis indicates that the addition of computer-based interventions as a supplement to standard weight loss interventions produces significantly more weight loss, while the substitution of computer-based technology results in significantly less weight loss. This may not be surprising given that participants received additional tools in the addition studies, but the substitution findings of less weight loss raises questions about the effectiveness of the computer-based tools compared to non-computer-based modalities. It should also be noted that, while the addition studies demonstrated a statistically significant benefit favoring the use of computers, the magnitude of the difference (<1.5 kilograms) is unlikely to be clinically relevant in overweight and obese populations and its sustainability is questionable.
Eleven randomized trials met our inclusion criteria. While some might be concerned that the variations in the components and intensity of interventions across trials might have contributed to the mixed findings, the overall lack of heterogeneity in the results suggests that computer-based interventions will not produce substantially different results compared to non-computer-based interventions regardless of content, intensity, or delivery mechanism. That said, the predominantly white make up of participants in most included studies decreases the generalizability of the findings to minority populations. Similarly, there were relatively fewer men (33%) than women, and some of the studies excluded individuals with chronic conditions (e.g., diabetes).51,52 The requirement that participants in three studies have a computer and Internet connection at home51,53,57 and that participants in three studies make a monetary refundable deposit to participate in the study,44,50,55 further limits applicability to persons of lower socio-economic status.
Turning to the internal validity of the included trials, incomplete reporting greatly limited our ability to formally assess important potential sources of bias. That said, detection bias seems less likely based on the objective nature of the outcomes, and while performance bias is possible due to the challenges of blinding this intervention, it may have been mitigated by the fact that both study arms had to receive some intervention. On the other hand, conflicts of interest were identified and inadequate detail regarding randomization techniques and attrition precluded assessment of selection and attrition biases.
With regard to the review itself, every effort was made in the search, selection, data collection and analysis portions to reduce bias, including independent review of articles and use of a standard data extraction template. Authors were contacted for missing data, but one failed to respond. We imputed standard deviations using a formula that includes a correlation coefficient (R), which we set at 0.5.41 In trying various values of R, from 0.4 to 0.8, we found no substantial change in the summary estimate. We also performed a post hoc analysis based on the two methodological approaches we had identified during the study eligibility process—adding versus substituting a computer-based technology. Lastly, while selective reporting was difficult to assess due to lack of trial registration, the funnel plots did not suggest publication bias.
Studies have found that approximately 20% of overweight or obese adults are able to achieve and maintain long-term weight loss, defined as losing at least 10% of body weight and maintaining that loss for at least 12 months.48,49 Factors found to be associated with success include long-term behavior change (such as eating a diet that is low in calories and fat, and engaging in high levels of physical activity) and self-monitoring of weight (an explicit component of several studies included in this review).43,53,54,56,57 Computers might seem an ideal tool for reinforcing such factors because they incorporate potential advantages such as persistence, anonymity, scalability, ubiquity, and the abilities to manage large amounts of data and to utilize a variety of modalities.23 However, the findings of this meta-analysis suggest that the use of computers themselves adds little to the success of many weight loss interventions. The advent of numerous portable electronic devices (e.g., smart phones) and new applications, such as social networking sites, might add additional capabilities or effects, but we only found two qualifying studies43,45 that included such devices. This is not surprising given the time required to conduct and publish studies that include newer devices. Lag time between the conduct of such studies and their availability for inclusion in meta-analysis is a recognized limitation of the technique.61As more studies are conducted that include such devices, a review of their effectiveness can be conducted.
In their 2010 article on “Motivational technologies to promote weight loss—From Internet to gadgets,”62 Svensson and Lagerros noted that, “modern technology may not curb the obesity epidemic alone – fighting against obesity requires a long-term and intense effort…. [in which] these tools may not replace, but rather serve as a complement to conventional healthcare.” This is congruent with the notion of utilizing the Chronic Care Model,59 with its consideration of multiple levels of focus and interventions to treat obesity. Indeed, it may be that computer-based interventions add value through other outcomes not assessed by this meta-analysis, such as patient and provider satisfaction, convenience, and cost-effectiveness but these are yet to be determined.
References
Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999–2008. JAMA. 2010;303(3):235–41.
World Health Organization. Obesity and Overweight: What are overweight and obesity? 2006; http://www.who.int/mediacentre/factsheets/fs311/en/index.html. Accessed April 25, 2011.
Wyatt SB, Winters KP, Dubbert PM. Overweight and obesity: prevalence, consequences, and causes of a growing public health problem. Am J Med Sci. 2006;331(4):166–74.
Centers for Disease Control and Prevention. Overweight and Obesity: Health Consequences. 2009; http://www.cdc.gov/obesity/causes/health.html. Accessed April 25, 2011.
Finkelstein EA, Fiebelkorn IC, Wang G. National medical spending attributable to overweight and obesity: how much, and who's paying? Health Aff (Millwood). Jan-Jun 2003;Suppl Web Exclusives:W3-219-226.
Kumanyika SK, Obarzanek E, Stettler N, et al. Population-based prevention of obesity: the need for comprehensive promotion of healthful eating, physical activity, and energy balance: a scientific statement from American Heart Association Council on Epidemiology and Prevention, Interdisciplinary Committee for Prevention (formerly the expert panel on population and prevention science). Circulation. 2008;118(4):428–64.
Huang TT, Drewnosksi A, Kumanyika S, Glass TA. A systems-oriented multilevel framework for addressing obesity in the 21st century. Prev Chronic Dis. 2009;6(3):A82.
Lyznicki JM, Young DC, Riggs JA, Davis RM. Obesity: assessment and management in primary care. Am Family Physician. 2001;63(11):2185–96.
Baulch J, Chester A, Brennan L. Treatment alternatives for overweight and obesity: the role of online interventions. Behav Change. 2008;25(1):1–14.
Baker RC, Kirschenbaum DS. Self-monitoring may be necessary for successful weight control. Behav Ther Sum. 1993;24(3):377–94.
Shaw K, O'Rourke P, Del Mar C, Kenardy J. Psychological interventions for overweight or obesity. Cochrane Database Syst Rev. 2005;2:CD003818.
U.S. Preventive Services Task Force Clinical guidelines. Screening for obesity in adults: recommendations and rationale. Ann Intern Med. 2003;139(11):930.
Kushner RF. Tackling obesity: is primary care up to the challenge? Arch Intern Med. 2010;170(2):121–3.
Ma J, Xiao L, Stafford RS. Underdiagnosis of obesity in adults in US outpatient settings. Arch Intern Med. 2009;169(3):313–4.
Rippe JM, Crossley S, Ringer R. Obesity as a chronic disease: modern medical and lifestyle management. J Am Diet Assoc. 1998;98(10 Suppl 2):S9–15.
Frank A. A multidisciplinary approach to obesity management: the physician's role and team care alternatives. J Am Diet Assoc. 1998;98(10 Suppl 2):S44–8.
Leverence RR, Williams RL, Sussman A, Crabtree BF. Obesity counseling and guidelines in primary care: a qualitative study. Am J Prev Med. 2007;32(4):334–9.
Foster GD, Wadden TA, Makris AP, et al. Primary care physicians' attitudes about obesity and its treatment. Obes Res. 2003;11(10):1168–77.
Tate DF, Jackvony EH, Wing RR. Effects of Internet behavioral counseling on weight loss in adults at risk for type 2 diabetes: a randomized trial. JAMA. 2003;289(14):1833–6.
Carr LJ, Bartee RT, Dorozynski C, Broomfield JF, Smith ML, Smith DT. Internet-delivered behavior change program increases physical activity and improves cardiometabolic disease risk factors in sedentary adults: results of a randomized controlled trial. Prev Med. 2008;46(5):431–8.
Gold BC, Burke S, Pintauro S, Buzzell P, Harvey-Berino J. Weight loss on the web: a pilot study comparing a structured behavioral intervention to a commercial program. Obesity (Silver Spring). 2007;15(1):155–64.
Cussler EC, Teixeira PJ, Going SB, et al. Maintenance of weight loss in overweight middle-aged women through the Internet. Obesity. 2008;16(5):1052–60.
Fogg BJ. Persuasion in the digital age. In: Fogg BJ, ed. Persuasive technology: using comuters to change what we think and do. San Francisco: Morgan Kaufmann Publishers; 2003:1–14.
Fogg BJ. Computers as persuasive social actors. In: Fogg BJ, ed. Persuasive technology: using computers to change what we think and do. San Francisco: Morgan Kaufmann Publishers; 2003:89–120.
Cassell MM, Jackson C, Cheuvront B. Health communication on the Internet: an effective channel for health behavior change? J Health Commun. 1998;3(1):71–9.
Andersson G, Bergstrom J, Hollandare F, Carlbring P, Kaldo V, Ekselius L. Internet-based self-help for depression: randomised controlled trial. Br J Psychiatry. 2005;187:456–61.
Lange A, Rietdijk D, Hudcovicova M, van de Ven JP, Schrieken B, Emmelkamp PM. Interapy: a controlled randomized trial of the standardized treatment of posttraumatic stress through the internet. J Consult Clin Psychol. 2003;71(5):901–9.
Lorig KR, Ritter PL, Laurent DD, Plant K. Internet-based chronic disease self-management: a randomized trial. Med Care. 2006;44(11):964–71.
Wantland DJ, Portillo CJ, Holzemer WL, Slaughter R, McGhee EM. The effectiveness of web-based vs. non-web-based interventions: a meta-analysis of behavioral change outcomes. J Med Internet Res. 2004;6(4):e40.
Krishna S, Balas EA, Spencer DC, Griffin JZ, Boren SA. Clinical trials of interactive computerized patient education: implications for family practice. J Fam Pract. 1997;45(1):25–33.
Biermann JS, Golladay GJ, Peterson RN. Using the internet to enhance physician-patient communication. J Am Acad Orthop Surg. 2006;14(3):136–44.
Weinstein PK. A review of weight loss programs delivered via the Internet. J Cardiovasc Nurs. 2006;21(4):251–8. quiz 259–260.
Saperstein SL, Atkinson NL, Gold RS. The impact of internet use for weight loss. Obes Rev. 2007;8(5):459–65.
Neville LM, Milat AJ, O'Hara B. Computer-tailored weight reduction interventions targeting adults: a narrative systematic review. Health Promot J Austr. 2009;20(1):48–57.
Neve M, Morgan PJ, Jones PR, Collins CE. Effectiveness of web-based interventions in achieving weight loss and weight loss maintenance in overweight and obese adults: a systematic review with meta-analysis. Obes Rev. Sep 14 2009.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151(4):264–9. W264.
Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Ann Intern Med. 2009;151(4):W65–94.
Brodney FS, ]Falzon L, Trudeau KJ, Sciamanna CN, Schwartz JE, Davidson KW. Computer-based interventions for weight loss or weight maintenance in overweight or obese people (Protocol). The Cochrane Library. 2009;(3).
Centers for Disease Control and Prevention: Obesity and Overweight. 2010; http://www.cdc.gov/obesity/defining.html. Accessed April 25, 2011.
Higgins J, Altman D. Assessing risk of bias in included studies. In: Higgins J, Green S, eds. Cochrane Handbook for Systematic Reviews of Interventions Version 5.0.1: The Cochrane Collaboration; 2008.
Higgins J, Green Se. Cochrane handbook for systematic reviews of interventions Version 5.0.2 [updated September 2009]2008.
Review Manager (RevMan) [Computer program]. Version 5.0 [computer program]. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration; 2008.
Shay LE, Seibert D, Watts D, et al. Adherence and weight loss outcomes associated with food-exercise diary preference in a military weight management program. Eat Behav. 2009;10(4):220–7.
DeLucia JL, Kalodner CR, Horan JJ. The effect of two nutritional software programs used as adjuncts to the behavioral treatment of obesity. J Subst Abuse. 1988;1(2):203–8.
Agras WS, Taylor CB, Feldman DE, Losch M, et al. Developing computer-assisted therapy for the treatment of obesity. Behavior Therapy Win. 1990;21(1):99–109.
Duval S, Tweedie R. Trim and fill: a simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics. 2000;56(2):455–63.
Perri MG, McAdoo WG, McAllister DA, et al. Effects of peer support and therapist contact on long-term weight loss. J Consult Clin Psychol. 1987;55(4):615–7.
Wing RR, Hill JO. Successful weight loss maintenance. Annu Rev Nutr. 2001;21:323–41.
Wing RR, Phelan S, Wing RR, Phelan S. Long-term weight loss maintenance. Am J Clin Nutr. 2005;82(1 Suppl):222S–5.
Wylie-Rosett J, Swencionis C, Ginsberg M, et al. Computerized weight loss intervention optimizes staff time: the clinical and cost results of a controlled clinical trial conducted in a managed care setting. J Am Diet Asso. 2001;101(10):1155–62. quiz 1163–1154.
Womble LG, Wadden TA, McGuckin BG, et al. A randomized controlled trial of a commercial internet weight loss program. Obes Res. 2004;12(6):1011–8.
Turnin MC, Bourgeois O, Cathelineau G, et al. Multicenter randomized evaluation of a nutritional education software in obese patients. Diab Metab. 2001;2(Pt 1):139–47.
Polzien KM, Jakicic JM, Tate DF, et al. The efficacy of a technology-based system in a short-term behavioral weight loss intervention. Obesity. 2007;15(4):825–30.
Morgan PJ, Lubans DR, Collins CE, et al. The SHED-IT randomized controlled trial: evaluation of an internet-based weight-loss program for men. Obesity. 2009;17(11):2025–32.
Jones KS, Burkett LN. A comparison of instructional methods for weight loss in women. Health Promot Pract. 2002;3(4):501–6.
Burnett KF, Taylor CB, Agras WS. Ambulatory computer-assisted therapy for obesity: a new frontier for behavior therapy. J Consult Clin Psychol. 1985;53(5):698–703.
van Wier MF, AriÎns GA, Dekkers JC, Hendriksen IJ, Smid T, van Mechelen W. Phone and e-mail counselling are effective for weight management in an overweight working population: a randomized controlled trial. BMC Public Health. 2009:6.
Managing the Global Epidemic: Report of a WHO Consultation on Obesity. Geneva, Switzerland: World Health Organization;1998.
Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness. JAMA. 2002;288(14):1775–9.
Griffiths F, Lindenmeyer A, Powell J, Lowe P, Thorogood M. Why are health care interventions delivered over the internet? A systematic review of the published literature. J Med Internet Res. 2006;8(2):e10.
Patsopoulos NA, Ioannidis JP. The use of older studies in meta-analyses of medical interventions: a survey. Open Med. 2009;3(2):e62–8.
Svensson M, Lagerros YT. Motivational technologies to promote weight loss—from internet to gadgets. Patient Educ Couns. Jun;79(3):356–36.
Acknowledgement of Funding Source
This work was supported in part by tuition scholarships for two of the authors from the Dartmouth Institute for Health Policy and Clinical Practice.
Conflict of Interest
None disclosed.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Appendix 1
Protocol changes (PDF 21 kb)
Appendix 2
Inclusion criteria (PDF 23 kb)
Appendix 3
Search strategies (PDF 33 kb)
Appendix 4
Data collection form (PDF 47 kb)
Appendix 5
Methodological quality assessment tool (PDF 223 kb)
Appendix 6
Supplemental Figures (PDF 23 kb)
Rights and permissions
About this article
Cite this article
Reed, V.A., Schifferdecker, K.E., Rezaee, M.E. et al. The Effect of Computers for Weight Loss: A Systematic Review and Meta-analysis of Randomized Trials. J GEN INTERN MED 27, 99–108 (2012). https://doi.org/10.1007/s11606-011-1803-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-011-1803-9