Abstract
BACKGROUND
Physical examination teaching using actual patients is an important part of medical training. The patient experience undergoing this type of teaching is not well-understood.
OBJECTIVE
To understand the meaning of physical examination teaching for patients.
DESIGN
Phenomenological qualitative study using semi-structured interviews.
PARTICIPANTS
Patients who underwent a physical examination-based teaching session at an urban Veterans Affairs Medical Center.
APPROACH
A purposive sampling strategy was used to include a diversity of patient teaching experiences. Multiple interviewers triangulated data collection. Interviews continued until new themes were no longer heard (total of 12 interviews). Interviews were recorded and transcribed verbatim. Coding was performed by two investigators and peer-checked. Themes were identified and meanings extracted from themes.
KEY RESULTS
Seven themes emerged from the data: positive impression of students; participation considered part of the program; expect students to do their job: hands-on learning; interaction with students is positive; some aspects of encounter unexpected; range of benefits to participation; improve convenience and interaction. Physical examination teaching had four possible meanings for patients: Tolerance, Helping, Social, and Learning. We found it possible for a patient to move from one meaning to another, based on the teaching session experience.
CONCLUSIONS
Physical examination teaching can benefit patients. Patients have the potential to gain more value from the experience based on the group interaction.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
BACKGROUND
Bedside teaching has declined as a response to changes in the clinical environment.1 Compared to the 1960s, when 75% of attending rounds was spent at the patient’s bedside,2 more recent estimates place this percentage at 11–27%. 3–5 Time constraints, faculty pressures, undervaluation of teaching, overvaluation of technology, and concern for patient comfort have been blamed for this change.6–9 Both teachers and learners have suggested ways to overcome barriers.1,7–9 These ideas would benefit from understanding the patients’ point of view: what do patients value; how can bedside teaching be improved?
In the limited literature on patient attitudes towards bedside teaching, most studies refer collectively to any teaching that is done at the patient’s bedside, or focus only on bedside case presentations.10–13 Patients generally hold a positive view of bedside teaching, are not made anxious by bedside teaching, and would recommend the practice to others.11,14 However, it is concerning that even a minority experience discomfort.12,14
In particular, bedside physical examination teaching involves invasion of personal space, concern for potential embarrassment, and risk of objectification. Yet, learners believe bedside teaching is important for learning physical examination skills,5 and lack of formal instruction in these skills results in trainees with poorer proficiency at bedside diagnoses.15 This study seeks to understand the patients’ experience of physical examination teaching. How we can best serve patients while satisfying a critical training need?
OBJECTIVE
To understand the meaning of physical examination teaching for patients.
DESIGN
We used a phenomenological qualitative design16 to address the central research question: What is the patient’s experience undergoing physical examination teaching? Phenomenology is a qualitative research method that attempts to understand the essence of an experience.
PARTICIPANTS AND SETTING
Semi-structured individual interviews were conducted with inpatients who participated in Bedside Rounds, a weekly physical examination-based teaching session for third-year medical students at the Washington DC VA Medical Center between November 2007 and December 2008. Teaching sessions consist of one faculty mentor (among a stable cadre of 6 mentors) with 3–5 medical students who examine 2–3 patients per hour session. Patients are identified as potential Bedside Rounds candidates based on salient physical examination findings noted by members of their care team. Faculty mentors ask for the patient’s permission to have students examine them prior to the teaching session.
APPROACH
Data Collection
An interview guide consisting of open-ended questions was developed, addressing what the experience of being physically examined by the students was like, the benefits of the experience for the participants and the students, and how they would describe the experience if writing about it, among others. Questions were tested and refined during a two-interview pilot study. Pilot study data is not included in this report.
Participants were selected using a purposive sampling strategy (where participants are deliberately selected as opposed to by chance) to maximize diversity of patient experiences captured in the interviews. After each Bedside Rounds session, one of the investigators (KCC) discussed with faculty mentors which patients they saw, time spent in the interaction, and whether faculty mentors deemed patients able to medically tolerate an interview up to one hour long. Potential participants were selected to maximize variation of physical examination foci (e.g. cardiovascular exam, abdominal exam, etc.), faculty mentor facilitators, patient age, and patient sex. Potential participants were approached shortly after their session by one of the investigators. Those who agreed to participate provided written informed consent. They were given a copy of the interview guide to maximize participation and recall. In the majority of cases, they were interviewed the following day, and in no case more than a week after the session. Three trained interviewers conducted the interviews (KCC, KEC, EFG), none of whom were responsible for the care of the patient. Interviews were audiotaped on digital recorders and transcribed verbatim by an external service.
Refinement of the interview guide occurred after interview #7 based on transcript reviews, when it was found that more time spent discussing the participants’ personal history yielded more detailed description. Interviews continued until two authors independently concluded that no new information was being added with subsequent interviews (interview #10), but since two interviews were already scheduled, these were completed.17
This study was approved by the Institutional Review Board of the Washington DC VA Medical Center.
Data Analysis
Transcripts were read and analyzed independently by two investigators with formal training in qualitative research (KCC, EFG), one of whom teaches a graduate-level qualitative research course (EFG). A phenomenological approach to data analysis was followed.17 The investigators coded one transcript together by reading it through in its entirety, identifying statements of interest and assigning codes, and then grouping the coded data into code clusters. First, textual (what happened) and then structural (how the phenomenon was experienced) descriptions of this interview were composed.
This was repeated for a second transcript. A codebook was created with relevant codes from the first two transcripts. Investigators then coded the rest of the transcripts individually with periodic peer checks. Investigators did not code their own interviews. Individual textual and structural descriptions were composed for each interview. Disagreements in coding and new codes were addressed by discussion.
All codes were entered into a codebook spreadsheet. Major themes were determined and representative quotes were highlighted. Meanings were then abstracted from the final themes through discussion. Composite textual-structural descriptions were composed for each of the four meanings by integrating the individual textual-structural descriptions.17
Trustworthiness
Researchers conducted peer debriefing and epoché (a procedure use to bracket away prior assumptions and beliefs about the experience) to limit researcher bias prior to study commencement. To triangulate the data collection, multiple interviewers were used, including clinicians (attending, KCC; senior medical student, KEC) and non-clinicians (EFG). Transcripts were reviewed periodically to identify any biases and to identify means of improving the data collection with feedback exchanged between interviewers. To enhance external validity, the researchers have provided thick descriptions17 (i.e. quotes) to support the themes that emerged so that others can determine the extent to which the findings are transferable.
Procedures used to increase the trustworthiness of data analysis included the use of multiple coders and peer code-checking. In addition, a form of member checks (a verification technique seeking participant feedback on researcher interpretation of the information shared) was completed by asking the participants to react to the interviewer’s summary of the major points at the end of each interview.
KEY RESULTS
Participants were mostly men (11/12), with a mean age of 60 (range 52–79). Only one potential participant declined to be interviewed for the study, with the reason reported as impending hospital discharge. The interviews yielded 134 pages of text for analysis. Seven major themes emerged from the data regarding the patients’ experiences.
Experience of Physical Examination Teaching
Positive Impression of Students
Students were described as being smart, reserved, polite, friendly, and interested.
…they were so smart…the questions that they asked were smart, reasonable questions to ask and they got it… (Participant 8)
They were inquisitive and I enjoyed that. It just told me they were interested in what was going on and how-what they could do to help fix things. (Participant 7)
For some, though, it was unclear exactly who were the students. Some seemed to confuse students with housestaff by reversing the significance of white coat length, while others thought some of the students were nurses.
Participation is Part of the Program
Participants’ belief in education, sense of duty, and wanting to pass the time seemed to underlie their participation in the physical examination teaching session.
I believe in education and the more that anybody, not only in the medical field, the more experience they can get prior to them getting their certification or degree or whatever they’re striving to do, the more experience they can get, my opinion is that it will make them a better professional in their field (Participant 4)
I go along with the program. I don’t cause no trouble… They’re trying to help you. (Participant 5)
They had no problem participating unless they were not feeling up to it physically or there was a potential for embarrassment.
You don’t want to drop your clothes in front of everybody…but you know I thought about it and how important it was to them you know like-I’m going to do this. (Participant 8)
Some days you know you just don’t feel up to it. I’ve had a couple of bad days these past few days feeling nauseated you know but it passes. (Participant 2)
Expect Students to do Their Job: Hands-on Learning
Participants held the expectation that learning is medical students’ job and that there is no substitute for hands-on learning.
Well like I said they get their hands-on experience in. They learn different bedside manner and things of that nature. (Participant 3)
…think they benefited because they hadn’t seen anything like that before. (Participant 9)
They checked you out and checked your liver and stuff like that you know that’s not surprising that’s just them doing their job. They’re doing their job so they can be a doctor or-or a nurse or something or whatever. (Participant 5)
Interaction with Students is Positive
Initially, the interaction may be uncomfortable, but the experience of physical examination teaching was generally positive. Comfort levels were increased when students were smiling or encouraging. Alternatively, when patients realized that they were helping students learn, it became a positive experience.
I was uncomfortable at first and then once things started going then I was just in the throe of things and I was trying to answer questions and like I said what I couldn’t answer the doctor answered. (Participant 8)
They always had a smile and we talked and we didn’t talk just about what was happening. We had our little chuckles now and then and it made you feel more comfortable (Participant 7)
They give me courtesy and respect and I give courtesy and respect. (Participant 10)
Some Aspects of Encounter Unexpected
Participants were surprised by the expressions on students’ faces, students’ interest in them, learning about themselves, and the actual process of the sessions.
Some of the expressions on people’s faces you know like [chuckles] make you wonder: Hey, are you going to make it through this? [Laughter] (Participant 2)
The fact that they would want to come see me [laughter] was probably the biggest surprise (Participant 4)
The only thing that they surprised me was when they started talking about my eyes and stuff because I didn’t know that myself (Participant 9)
Range of Benefits to Participation
Many patients identified benefits associated with participating in physical examination teaching, although some derived minimal to no benefit.
It does you good to talk to those young doctors (Participant 6)
It makes you feel better. It makes you feel like they diagnose if anything is wrong with you. (Participant 5)
I guess just talking to people is what I enjoy doing and that was an opportunity to do so without having to talk to another patient where he’s always moaning about his problems or everything else (Participant 3)
If I know I’ve helped them that makes me feel good you know (Participant 2)
Well, I’m getting a birds-eye view of how doctors work with the team and everybody derives information. (Participant 11)
Improve Convenience and Interaction
Participants gave several suggestions for improving physical examination teaching, shown in the Text Box.
Meanings of Physical Examination Teaching
Looking across all themes and individual textual-structural descriptions (the essence of each encounter),17 four meanings of physical examination teaching were derived.
Tolerance
Patients in this category perceived no benefit from the physical examination teaching encounter. They tolerated the session, understanding this was a normal part of being in a teaching hospital. “Tolerance” can be understood from the following composite description: The doctor asks if she can bring patients by to see some things, so he, the patient, agrees to have them stop by. He knows they do training here so he doesn’t mind, and he realizes the students have to see things to learn. It is pretty informal: he tells them how he got here and then his doctor asks the students questions. No big deal, but he’s glad it’s over quickly.
One participant summarized the feeling with “I don’t get nothing personally out of them. I figure they get …something from me, but I don’t get nothing from them you know because like they’ve got to learn you know…” (Participant 10)
Helping
For others, physical examination teaching gave value to patients by being able to help students. Participating appealed to their sense of altruism.
The composite description of “helping” is: He (the patient) was a training aide so he understands that the students have to learn somewhere on someone. They all come in and feel his stomach. The doctor helps the students who are not so sure of themselves. It does not hurt and he feels like he has done his duty: helped others learn just like someone helped him before.
It was something like they had never seen you know and it made me feel good that I could help them because they hadn’t experienced nothing like that and I gave them the opportunity …to do so. (Participant 9)
Learning
For other patients, participating in the sessions contributed to their own learning about their medical conditions or their bodies. The composite description of “learning” is: He is included as a learner in the educational process. While the students are conducting the examination, looking at his neck, the teacher is explaining what they are doing using terms he can understand the whole time. This is very comforting to him and in the process, he learns some new things about his condition. He felt important to be part of the process, included.
I got a better understanding of…what my problem was…the way the students and the way the teacher broke it down in more layman terms made me—I could understand it more (Participant 12)
Social
Finally, for some patients, physical examination teaching provided needed social interactions during an isolating hospitalization. For these patients, the sessions were welcome and enjoyed on a social level. The composite description of “social” is:
Having the students come in is a very pleasant experience, one of the few times when he is not alone. They are respectful and seem genuinely interested in him as a person as well as skilled to uncover his medical problems. There is a lot of dialogue when the students are there; asking personal questions of him, being asked questions by the teacher and also chatting about non-medical things. It’s an enjoyable social event and it makes him feel important that the students are so interested and caring.
I talked and told them stories and told them things that happened a long time ago or maybe even not that long you know just different things... As a matter of fact it felt real good. Personally I enjoyed them coming in or coming by because for one it was company… I don’t get no company. (Participant 7)
The majority of participants’ experiences fell into either the Tolerance or Helping category. In some instances, patients moved from one meaning to another by the end of the teaching session, based on their interactions with the group. Participant 4 started in the Social category before ending in the Helping category. Participants 6 and 9 went from Tolerance to Helping. Participant 12 described two separate teaching session experiences, one of which typified Tolerance, the other, Learning.
DISCUSSION
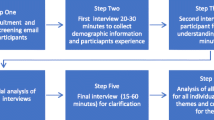
Physical examination teaching is a generally well-perceived experience from the patient perspective. Participants hold a positive impression of medical student education and the patient-student interaction has many potential benefits. Physical examination teaching can have several distinct, non-mutually exclusive meanings for patients: Tolerance, Helping, Social, and Learning (Fig. 1). We have seen the potential to move from a meaning with less patient value (Tolerance) to meanings with possible higher benefit (Social, Learning, Helping), opening the door to more meaningful patient-student-teacher interactions. We can see no reason why a patient could not “enter” with one meaning and “exit” benefiting from others. Past patient experiences, personal values, the nature of the current illness, and health literacy might determine where the patient starts out18,19 and where they have the potential to move. Of course, if conducted in the wrong manner, patients starting out with positive attitudes might end up deriving little to no benefit.
Potential model of patient meanings from physical examination teaching. Individual factors contribute to where a patient starts on the model (H = Helping, T = Tolerance, S = Social, L = Learning), and also mediate potential movement from one meaning to another as a result of the teaching interaction.
This model could be easily applied whenever educators facilitate physical examination teaching. Observation and appraisal of patients before and during sessions might classify patients into one of these four meanings. This could direct educators (and students) to employ strategies to give patients more value, for example, guiding a Tolerant patient to greater learning, social, or helping meanings. Explaining things in layman terms and directly to the patient; asking patients about their histories or hobbies; and emphasizing how helpful their participation has been, are some ways to incorporate these other dimensions.
Patients gave various suggestions for improving physical examination teaching, including logistical (avoiding meal time, giving patient lead times) and procedural considerations (asking the patient more questions, checking for patient comfort during sessions). From our experience, the suggestion to have students introduce themselves and say where they are from, has been an easy, quick, and rapport-building addition to the sessions.
The finding that physical examination teaching can lead to patients learning about their own illnesses may merit special consideration given the growing body of literature linking health literacy to self-efficacy, health behaviors, and participation in medical decision-making.19–21 These encounters could represent important educational opportunities for patients (learning about their own disease processes and symptoms) as well as learners (learning how to communicate and teach patients effectively). Participant 12 described two separate teaching session encounters, one in which the group used medical jargon and excluded him from the discussion (Tolerance) and the other where the group took the time to explain things in layman’s terms to him, causing him to feel actively engaged and empowered (Learning). Thus, the meaning of these teaching sessions for patients may vary depending upon how the session is conducted. Pivotal to improving health literacy is teaching effective patient communication techniques to learners;22 teaching rounds could serve this purpose. This could be an area of future study.
Our study findings are consistent with prior work showing that patients perceive bedside teaching involving patients and physician teams to be a positive experience.12 The majority enjoy having medical students involved in their care.12,13 This study adds to existing literature by providing a focus on the component of bedside teaching that may be the most uncomfortable for patients: physical examination teaching. When Fletcher et al. surveyed Veteran patients on their bedside interactions with physician teams, they found 13% were made uncomfortable when several people examined them at once.12 Physical examination teaching often occurs in the small-group setting, involving multiple student examiners; yet, even the “Tolerant” patients in our study did not describe significant discomfort with the examination process. This may be because examinations during daily bedside rounds are often performed without asking the patient’s permission first; asking for permission in any physical examination teaching setting could improve patient comfort. A prior model on bedside interactions found that information exchange, evidence of caring, involvement in teaching, knowing the team, and bedside manner were important to patients.13 The four possible meanings we identified overlap these themes previously identified; not only are these themes important to patients, but they create meaning for patients.
This study has several limitations. Patients were Veterans who were mostly male and of older age. While the Veteran population, in of itself, is an important population to study given the large role the Veterans Affairs medical system plays in medical education, there may be unique characteristics of Veterans that limit the ability to generalize findings more broadly. Yet, there are likely universal meanings that exist for patients who voluntarily participate in physical examination teaching. Also, as in any qualitative interview study, it is possible that if we had done more interviews, we might have heard new things. However, we believed that there was limited utility of additional interviews based on the variation of physical examination foci of participants (cardiac, abdominal, etc), concurrent data analysis, and consistency with numbers of participants recommended for phenomenological studies (8–15).16 Finally, all of the patients in our study, by definition, agreed to participate in the physical examination teaching sessions in the first place. Thus, our model may only apply to those who voluntarily agree to physical examination teaching and those who are offered a choice.
Future studies should evaluate how attending to this four-meaning model impacts patient, student, and teacher satisfaction with physical examination teaching, as well as how it applies to other patient populations. Encouragingly, student bedside physical examination teaching, which may appear to only benefit students, can also benefit patients in significant ways. Perhaps “patient-centered teaching” should be the ultimate goal, with student learning as an important, but not exclusive, endpoint.
References
LaCombe MA. On bedside teaching. Ann Intern Med. 1997;126:217–20.
Reichsman F, Browning FE, Hinshaw JR. Observations of undergraduate clinical teaching in action. Acad Med. 1964;39:147–63.
Collins GF, Cassie JM, Daggett CJ. The role of the attending physician in clinical training. J Med Educ. 1978;53:429–31.
Miller M, Johnson B, Greene HL, Baier M, Nowlin S. An observational study of attending rounds. J Gen Intern Med. 1992;7:646–8.
Chuang CH, Gonzalo JD, Masters PA, Simons RJ. Attending rounds and bedside case presentations: medical student and medicine resident experiences and attitudes. Teach Learn Med. 2009;21(2):105–10.
Nair BR, Coughlan JL, Hensley MJ. Impediments to bedside teaching. Med Educ. 1998;32:159–62.
Ramani S, Orlander JD, Strunin L, Barber TW. Whither bedside teaching: a focus-group study of clinical teachers. Acad Med. 2003;78:384–90.
Williams KN, Ramani S, Fraser B, Orlander JD. Improving bedside teaching: findings from a focus group study of learners. Acad Med. 2008;83:257–64.
Janick RW, Fletcher KE. Teaching at the bedside: a new model. Medical Teacher. 25:127–30.
Lehmann LS, Brancati FL, Chen M, Roter D, Dobs AS. The effect of bedside case presentations on patients’ perceptions of their medical care. N Engl J Med. 1997;336:1150–5.
Nair BR, Coughlan JL, Hensley MJ. Student and patient perspectives on bedside teaching. Med Educ. 1997;31:341–6.
Fletcher KE, Rankey DS, Stern DT. Bedside interactions from the other side of the bedrail. J Gen Intern Med. 2005;20(1):58–61.
Fletcher KE, Furney SL, Stern DT. Patients speak: what’s really important about bedside interactions with physician teams. Teach Learn Med. 2007;19(2):120–7. Spring.
Romano J. Patients’ attitudes and behavior in ward round teaching. J Am Med Assoc. 1941;117(9):664–7.
Mangione S, Nieman LZ, Gracely E, Kaye D. The teaching and practice of cardiac auscultation during internal medicine and cardiology training: a nationwide survey. Ann Intern Med. 1993;119:47–54.
Creswell JW. Qualitative inquiry and research design: choosing among five traditions. 2nd ed. Thousand Oaks: Sage Publishing; 2006.
Moustakas C. Phenomenological research methods. Thousand Oaks: Sage; 1994.
Hartz MB, Beal JR. Patients’ attitudes and comfort levels regarding medical students’ involvement in obstetrics-gynecology outpatient clinics. Acad Med. 2000;75(10):1010–14.
DeWalt DA, Boone RS, Pignone MP. Literacy and its relationship with self-efficacy, trust, and participation in medical decision making. Am J Health Behav. 2007;31(Suppl 1):S27–35.
DeWalt DA, Berkman ND, Sheridan S, Lohr KN, Pignone MP. Literacy and health outcomes: a systematic review of the literature. J Gen Intern Med. 2004;19(12):1228–39.
VonWagner C, Semmler C, Good A, Wardle J. Health literacy and self-efficacy for participating in colorectal cancer screening: the role of information processing. Patient Educ Couns. 2009;75(3):352–7.
Berkman ND, DeWalt DA, Pignone MP, Sheridan SL, Lohr KN, Lux L, Sutton SF, Swinson T, Bonito AJ. Literacy and Health Outcomes. Summary, Evidence Report/Technology Assessment No. 87 (Prepared by RTI International-University of North Carolina Evidence-based Practice Center under Contract No. 290-02-0016). AHRQ Publication No. 04-E007-1. Rockville, MD: Agency for Healthcare Research and Quality. 2004.
Acknowledgments
We would like to thank the patients who agreed to be interviewed for this study. This work was funded by the non-profit Institute for Clinical Research, Washington, DC.
Presented, in part, at the 2009 SGIM Annual Meeting, Miami, FL.
Conflict of Interest
None disclosed.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chretien, K.C., Goldman, E.F., Craven, K.E. et al. A Qualitative Study of the Meaning of Physical Examination Teaching for Patients. J GEN INTERN MED 25, 786–791 (2010). https://doi.org/10.1007/s11606-010-1325-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-010-1325-x