Abstract
Background
Depression treatment requires close monitoring to achieve optimal, long-term control. Use of multiple sources of health care can affect coordination and continuity of treatment for depression.
Objectives
To assess levels of non-Veterans Health Administration (VA) use among depressed primary care patients by service type and examine patient factors associated with non-VA use.
Design
Cross-sectional comparison of dual and VA-only users among depressed primary care patients. Depression was defined as PHQ-9 ≥10.
Subjects
Five hundred fifty depressed patients from the baseline sample of a group-randomized trial of collaborative care for depression in ten VA primary care practices.
Measurements
VA and non-VA outpatient utilization for physical and emotional health problems in the prior 6 months, patient demographics, and co-morbid conditions. All measures were self-reported and obtained at the baseline interview.
Results
Overall, 46.8% of VA depressed primary care patients utilized non-VA care. Dual users were more likely to use acute care services (emergency room or inpatient), especially for physical health problems. Dual users of physical health services had more total visits, but fewer VA visits than VA-only users, while dual users of emotional health services had fewer total and VA visits. Factors associated with dual use were urban clinic location, having other insurance coverage, and dissatisfaction with physical health care in general.
Conclusions
Almost half of depressed primary care patients used non-VA care, with most of their non-VA use for physical rather than emotional health problems. Care management strategies for depressed patients should include communication and coordination with non-VA providers.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
Many individuals have access to more than one health-care system through multiple insurance programs, such as private insurance plans, Medicare, and Medicaid. In the Veterans Health Administration (VA), a significant proportion of veterans who receive VA care also utilize non-VA health-care sources1–6. Dual use may provide some veterans with increased choice, access, and flexibility in their health care7–9, or provide services that are unavailable in their local VA systems7,9–11. However, negative effects on continuity and coordination of care could be critical for individuals with chronic conditions requiring on-going, effective management and medication. Dual use may lead to duplication of care, resulting in inefficient allocation of financial resources and underestimation of health-care costs12–14. Finally, provider- or system-level performance measures may be affected by missing non-VA services.
Depression, the second most prevalent medical condition in VA, affects quality of life in up to 30% of outpatients15,16 and is associated with higher comorbidity, major functional impairment, and higher health-care utilization and costs than many other chronic conditions17–20. Patients with depression are commonly treated in primary care. Depression treatment requires close monitoring to achieve optimal, long-term control. Use of multiple sources of health care can significantly affect coordination and continuity of care. For example, veterans with depression who obtain care from both VA and non-VA sources may have difficulty maintaining an ongoing relationship with primary care providers who can monitor their health over time. Younger veterans and returning veterans of the Iraq and Afghanistan wars show a significantly higher burden of depression than other VA patients21,22. When these veterans transition to civilian life and seek care in the VA system, dual use could be a critical issue in coordination of depression care.
Use of non-VA care varies with the veteran population studied5,23. Among VA-enrolled veterans aged 65 or older, up to 22% were dual users. Among VA primary care patients, approximately 28% were dual users1,24, while 11–23% reported dual use among veterans in VA mental health specialty clinics25,26. For acute conditions, such as hip fracture and myocardial infarction, 17–54% of VA-enrolled veterans were admitted to non-VA hospitals5,23.
Dual users of VA and non-VA primary care tend to be older, with a smaller burden of illness and more education, income, access to health-care insurance, and expressed dissatisfaction with VA services compared to VA-only primary care patients1. In VA mental health specialty clinics, dual use has been linked to lower global functioning, specific mental health diagnoses (e.g., post-traumatic stress disorder, obsessive compulsive disorder, substance abuse, and dual mental health diagnoses), and more health-care utilization than veterans using VA services only25,26. These dual users are also more likely to be women, younger, white, and lacking a military service-connected disability than VA-only users25,26.
Improving depression treatment in primary care is a main VA focus. However, little is known about use of non-VA services and factors associated with non-VA use among depressed primary care patients. If dual use is prevalent, cost benefit analyses and performance measures based on the VA system could be inaccurate or misleading. Further, examining types of care is important for identifying specific health-care services that may be affected by dual use and targeting these care types for programs promoting coordination of care across systems. Given the importance of effectively coordinating care for depression, this study had two aims: (1) to assess levels and types of non-VA services used by depressed VA primary care patients and (2) to examine patient factors associated with non-VA health-care utilization.
METHODS
We present baseline analyses from a group-randomized clinical trial for depression quality improvement, the Well-being Among Veterans Enhancement Study (WAVES). This study evaluated the effect of collaborative care on depression outcomes in VA primary care.
Setting
WAVES included veterans from ten VA primary care clinics in rural/semi-rural areas or small cities in five states. The clinics were part of three VA regional health-care systems. Three clinics were randomized to provide usual depression care, and seven clinics implemented a collaborative care intervention. Clinics served between 1,512 and 11,506 patients annually.
Recruitment
A contracted survey firm conducted computer-assisted telephone interviews to determine eligibility and collect baseline data from June 2003 to June 2004. To be eligible for the study, patients must have had major depressive symptomatology, attended a study clinic within the previous 12 months, and had an upcoming appointment at the time of enrollment. Depression was defined as Patient Health Questionnaire-9 item (PHQ-9) ≥ 1027 (see measure description below). Exclusion criteria included acute suicidality and other acute problems or serious communication difficulties.
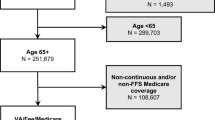
WAVES used consecutive sampling of participating sites’ primary care visitors. Of 28,474 eligible veterans, 10,929 were screened for depression or dysthymia using PHQ-9, and 1,313 screened positive. WAVES consented and enrolled 761 participants. We excluded 210 patients who reported no VA use in the previous 6 months and one patient with incomplete utilization data. The final study sample included 550 patients (Fig. 1). The present study examined participants from both intervention and control clinics. Study protocols were approved by Institutional Review Boards and Research and Development Services at the project’s clinical and administrative sites.
Measures
The 50-min baseline interview included the following measures:
Dual use
The primary dependent variable was dual use, defined as at least one non-VA outpatient visit, inpatient admission, or ER visit during the previous 6 months for a physical or emotional health problem. VA-only users were defined as veterans who used only VA health-care services in the last 6 months.
Demographic characteristics
Demographic data included gender, age, ethnicity (white vs. nonwhite), relationship status (married/living as married vs. single), education (high school or less vs. some college or more), insurance status, current employment (full or part-time, unemployed, disabled, retired, or other), and clinic location (urban/rural).
Depressive symptomatology
The PHQ-9 assessed depressive symptom severity. DSM-IV major depressive symptoms frequency (during the past 2 weeks) was indicated using a 4-point scale (“0= not at all” to “3 = every day/nearly every day”)27–29.
Post-traumatic stress disorder (PTSD)
The Primary Care PTSD Screen (PC-PTSD) assessed PTSD symptomatology30–32. Participants received 0-4 points for presence during the previous month of each of four PTSD symptoms (re-experiencing, avoidance, hypervigilance, and emotional numbing related to past trauma). Scores of 3 and 4 represented positive PTSD screens30.
Alcohol consumption
The Alcohol Use Disorders Identification Test consumption questions (AUDIT-C)33–35 evaluated alcohol consumption. Summed AUDIT-C responses result in an index of 0-12, predicting poor alcohol-related outcomes; scores greater than eight are associated with mortality36.
General health
The following Health Status Questionnaire15 item provided an indicator of general health: “In general would you say your health is...” Response options ranged from “1= excellent” to “5= poor.”
Medical comorbidity
The Seattle Index of Comorbidity (SIC) assessed medical comorbidity37 using presence/absence of seven chronic illness conditions, cigarette smoking status, and participant age. The SIC summary score predicts hospitalization and mortality.
Self-reported care utilization
Utilization was assessed using questions adapted from the Partners in Care Study38. Participants reported frequency of medical care received in the previous 6 months in VA and non-VA. Questions asked about health services used for physical and emotional health problems, but did not define these terms for the respondent.
Care satisfaction
Two questions from the Partners in Care study39 were used to assess participants’ satisfaction with health-care services available in the past 6 months for physical health and emotional problems. Response options ranged from “1= very satisfied” to “6= very dissatisfied.”
Data Analysis
We evaluated the association of patient characteristics with each of the dependent variables (odds of any visit/admission and number of visits/admissions) for dual users and VA only users using bivariate and multivariate analyses. In descriptive analyses, we used t-tests for normally distributed continuous variables, Wilcoxon tests for variables with skewed distributions, and chi-square tests for categorical variables. For utilization measures we used two-part models to examine whether a significant difference in utilization was due to the odds of using services or the level of use among users. The first part model estimated the odds of any visit/admission using logistic regressions. The second part model estimated the number of visits/admissions among users, using negative binomial regressions. We used logistic regression to estimate odds ratios for dual use for all patient factors. All analyses were adjusted for survey design and population weights using STATA version 1040.
RESULTS
Patient Characteristics
In this study sample, 46.8% of patients were dual users of VA and non-VA care. Among dual users, 94.9% used both VA and non-VA care for physical health problems and 20.3% for emotional health problems. Table 1 summarizes patient characteristics by dual use status. Compared to VA-only users, dual users were more likely to be older (65 years vs. 62 years, p = 0.017), white (90% vs. 85%, p = 0.048), retired (46% vs. 28%, p < 0.001), and have other health insurance (86% vs. 50%, p < 0.001).
VA-only users were more likely to report being satisfied or very satisfied with physical health-care services than dual users (74% vs. 65%, p = 0.036). Dual users had a higher level of medical comorbidity measured by the SIC score than VA-only users (8.0 vs. 7.1, p = 0.006), but a lower level of alcohol use measured by the AUDIT-C score (1.7 vs. 2.2, p = 0.048).
Unadjusted Health-Care Utilization
VA-only users and dual users were equally likely to have any outpatient visit for physical health (88% vs. 88%, p = 0.873) (Table 2). Dual users had more total outpatient visits (6.15 vs. 4.17, p < 0.001) but fewer VA visits (2.64 vs. 4.17, p < 0.001) for physical health than VA-only users. Dual users for physical health were more likely to have any ER visit (43% vs. 14%, p < 0.001) and any inpatient admission (32% vs. 16%, p < 0.001) than VA-only users. Dual users had more total ER visits (2.07 vs. 1.37, p < 0.001), but fewer VA ER visits (0.44 vs. 1.37, p < 0.001) for physical health than VA-only users. A similar trend of more overall use but less VA use for dual users was observed for inpatient physical health-care services.
Similarly, VA-only users and dual users were equally likely to have any outpatient visit for emotional health (44% vs. 46%, p = 0.639). There was no significant difference in total outpatient visits for emotional health (4.54 vs. 5.14, p = 0.715), but dual users had fewer VA visits than VA-only users (4.91 vs. 5.14, p < 0.001). Dual users for emotional health had a greater likelihood of having any ER visit (11% vs. 1%, p < 0.001) or inpatient admission (9% vs. 2%, p < 0.001). There were no significant differences in utilization between dual users and VA-only users of ER and inpatient emotional health care.
Adjusted Health-Care Utilization
For physical health, dual users had higher odds of any ER visit [odds ratio (OR) = 7.41, p < 0.001] and any inpatient admission (OR = 2.34, p < 0.01) than VA-only users, controlling for patient characteristics (Table 3). Dual users of outpatient care for physical health had 1.88 more total visits (p < 0.01), but 1.35 fewer VA visits (p < 0.01) than VA-only users. Dual users also had 0.61 more total ER visits (p < 0.01) and 1.22 fewer VA ER visits (p < 0.001) for physical health. There was no significant difference in total inpatient admissions for physical health between the two groups, but dual users had 1.03 fewer VA admissions than VA-only users (p < 0.001).
For emotional health, dual users had higher odds of having any ER visit (OR = 14.64, p < 0.001) and any inpatient admission (OR = 5.38, p < 0.001). Dual users of outpatient care for emotional health had 1.10 fewer total visits (p < 0.05) and 1.47 fewer VA visits (p < 0.01) than VA-only users. There was no significant difference between the two groups in total ER visits for emotional health, but dual users had 1.30 fewer VA ER visits (p < 0.05). Among emotional health inpatient users , there were no significant differences in total inpatient admissions or VA inpatient admissions for emotional health care between the two groups.
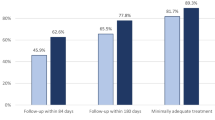
Patient Factors Associated with Dual Use
Table 4 presents patient factors associated with dual use identified using logistic regressions. Factors are presented separately for overall use, outpatient visits for physical health problems, and outpatient visits for emotional health problems.
Any Dual Use
Factors associated with higher odds of dual use included being retired (OR = 2.90, p < 0.001), using an urban VA primary care clinic (OR = 1.91, p < 0.001), and having other health insurance (OR = 6.90, p < 0.001). However, patients who were younger (OR = 0.97, p < 0.05) and were satisfied/very satisfied with physical health care were less likely to be dual users (OR = 0.67, p < 0.05).
Dual use of outpatient care for physical health
Patient factors significantly associated with dual use of outpatient care for physical health problems were using an urban VA primary care clinic (OR = 1.18, p < 0.001) and having other health insurance (OR = 5.59, p < 0.001). Patients who were satisfied/very satisfied with physical health-care services were less likely to be dual users (OR = 0.58, p < 0.05).
Dual use of outpatient care for emotional health
Patient factors associated with dual use of outpatient services for emotional health problems were using an urban VA primary care clinic (OR = 3.29, p = 0.007), having other health insurance (OR = 2.33, p = 0.024), and having current PTSD (OR = 2.12, p = 0.03). Patients who had a higher level of alcohol use measured by AUDIT-C score (OR = 0.88, p < 0.05) were less likely to be dual users.
DISCUSSION
The results show substantial dual use among depressed primary care patients. In this study, nearly half (47%) of VA primary care patients with significant depressive symptoms had also utilized non-VA health-care sources in the previous 6 months. This proportion of dual users among depressed primary care patients was much higher than previously reported in the VA general primary care or mental health specialty care populations1,25,26. Dual users were particularly likely to use acute care services (ER or inpatient), especially for physical health problems. Dual use also differed for physical and emotional health problems: patients using non-VA physical health services had more total visits, but fewer VA visits, and those using non-VA emotional health services had fewer total and VA visits.
The results show that dual use is more common for physical health problems than emotional health problems among depressed primary care patients, consistent with prior studies showing that VA and Medicare dual users were more reliant on VA for mental health care8. Lower dual use of emotional health services may reflect limited public and private coverage for these services outside the VA. Differences in dual use for physical and emotional health services may reflect differences in needs for different types of services among depressed primary care patients, which could be important for care planning. Further investigation is warranted to determine the drivers and needs associated with each of these types of dual use.
This study shows that ability to access other health-care resources and lower satisfaction with physical health-care services in general are associated with dual use of VA and non-VA care. Using a VA primary care clinic in an urban location (a proxy for patient residence in an urban area) and having other health insurance are significant factors associated with dual use for all types of services. These findings are consistent with previous studies1,41,42. Additionally, this study also corroborated prior findings1,10 that satisfaction with physical health-care services is associated with lower dual use of outpatient care for physical health problems. These results suggest the need for further research to determine the causes for dissatisfaction. For example, increasing overall patient satisfaction with care may help decrease the extent of dual use of health-care services. However, patients may be dissatisfied because needed services are not available in the VA, or the level of coordination between VA and non-VA is suboptimal.
This study shows that health status, medical comorbidity, and depression PHQ-9 score are not associated with dual use, with the exception that lower levels of alcohol use and presence of PTSD are significant factors associated with use of non-VA outpatient care for emotional health services. Prior studies of veterans43,44 have shown that PTSD patients are more severely depressed, more likely to have suicidal thoughts, and more likely to report higher anxiety and panic symptoms than patients with depression alone. As soldiers return from Iraq and Afghanistan, we may see an increase in depressed patients with PTSD seeking care in both VA and non-VA settings.
Several limitations of this study should be noted in evaluating the results. First, the study relied on self-report to assess health-care utilization and medical history. However, recall bias was minimized by a 6-month follow-up within the optimal recall period for self-report utilization45. Second, the study results cannot be generalized to other VA primary care clinics or to non-veteran populations. Future studies should focus on over-sampling women and minorities to determine patterns of dual use for these patients. Third, the participating primary care clinics were located in rural/semi-rural areas or small cities. Veterans residing in more urban locations may have different utilization patterns, because more non-VA health-care resources are available in urban areas, especially for mental health care. Fourth, the consecutive sampling approach of clinic visitors has been shown to under-sample low users of care and cannot be generalized to the broader clinic population46. Our purposeful sampling of primary care patients with significant depressive symptoms did, however, provide important information on the dual use patterns of this unique patient population. Fifth, the cross-sectional study design does not allow us to determine causation. Finally, this study did not address community or organizational factors that may be associated with dual use of health-care services.
In summary, this study found that a significant proportion of depressed primary care patients in the VA also use non-VA services. Dual users were high health-care users compared to VA-only users, with most of their non-VA outpatient care for physical rather than emotional health problems. Further studies of cost and quality of VA depression care should account for non-VA use, particularly analyses of physical health services. Care management strategies for depressed patients should recognize the need for communication and coordination with non-VA providers.
References
Borowsky SJ, Cowper DC. Dual use of VA and non-VA primary care. J Gen Intern Med. 1999;14:274–80.
Hynes DM, Koelling K, Stroupe K, et al. Veterans’ access to and use of Medicare and Veterans Affairs health care. Med Care. 2007;45:214–23.
Ross JS, Keyhani S, Keenan PS, et al. Dual use of Veterans Affairs services and use of recommended ambulatory care. Med Care. 2008;46:309–16.
Shen Y, Hendricks A, Zhang S, Kazis LE. VHA enrollees’ health care coverage and use of care. Med Care Res Rev. 2003;60:253–67.
Wright SM, Daley J, Fisher ES, Thibault GE. Where do elderly veterans obtain care for acute myocardial infarction: Department of Veterans Affairs or Medicare? Health Serv Res. 1997;31:739–54.
Wright SM, Petersen LA, Lamkin RP, Daley J. Increasing use of Medicare services by veterans with acute myocardial infarction. Med Care. 1999;37:529–37.
Petersen LA, Wright SM. Does the VA provide "primary" primary care? J Gen Intern Med. 1999;14:318–9.
Weeks WB, Bott DM, Lamkin RP, Wright SM. Veterans Health Administration and Medicare outpatient health care utilization by older rural and urban New England veterans. J Rural Health. 2005;21:167–71.
Weeks WB, Mahar PJ, Wright SM. Utilization of VA and Medicare services by Medicare-eligible veterans: the impact of additional access points in a rural setting. J Healthcare Manage / Am Coll Healthcare Exec. 2005;50:95–106.
Bean-Mayberry B, Chang CC, McNeil M, Hayes P, Scholle SH. Comprehensive care for women veterans: indicators of dual use of VA and non-VA providers. J Am Med Women’s Assoc. (1972). 2004;59:192–7.
Hoff RA, Rosenheck RA. The use of VA and non-VA mental health services by female veterans. Med Care. 1998;36:1524–33.
Hester EJ, Cook DJ, Robbins LJ. The VA and Medicare HMOs — complementary or redundant? N Engl J Med. 2005;353:1302–3.
Rosen AK, Gardner J, Montez M, Loveland S, Hendricks A. Dual-system use: are there implications for risk adjustment and quality assessment? Am J Med Qual. 2005;20:182–94.
Boyd CM, Darer J, Boult C, Fried LP, Boult L, Wu AW. Clinical practice guidelines and quality of care for older patients with multiple comorbid diseases: implications for pay for performance. JAMA. 2005;294:716–24.
Kazis LE, Ren XS, Lee A, et al. Health status in VA patients: results from the Veterans Health Study. Am J Med Qual. 1999;14:28–38.
Liu CF, Campbell DG, Chaney EF, Li YF, McDonell M, Fihn SD. Depression diagnosis and antidepressant treatment among depressed VA primary care patients. Adm Policy Ment Health. 2006;33:331–41.
Ormel J, VonKorff M, Ustun TB, Pini S, Korten A, Oldehinkel T. Common mental disorders and disability across cultures. Results from the WHO Collaborative Study on Psychological Problems in General Health Care. JAMA. 1994;272:1741–8.
Spiro A 3rd, Hankin CS, Mansell D, Kazis LE. Posttraumatic stress disorder and health status: the Veterans Health Study. J Ambul Care Manage. 2006;29:71–86.
Hankin CS, Spiro A 3rd, Mansell D, Miller DR, Kazis LE. Mental disorders and medical care utilization of VA ambulatory care patients: the Veterans Health Study. J Ambul Care Manage. 2006;29:51–60.
Simon G, Ormel J, VonKorff M, Barlow W. Health care costs associated with depressive and anxiety disorders in primary care. Am J Psychiatry. 1995;152:352–7.
Payne SM, Lee A, Clark JA, et al. Utilization of medical services by Veterans Health Study (VHS) respondents. J Ambul Care Manage. 2005;28:125–40.
Hoge CW, Auchterlonie JL, Milliken CS. Mental health problems, use of mental health services, and attrition from military service after returning from deployment to Iraq or Afghanistan. JAMA. 2006;295:1023–32.
Fleming C, Fisher ES, Chang CH, Bubolz TA, Malenka DJ. Studying outcomes and hospital utilization in the elderly. The advantages of a merged data base for Medicare and Veterans Affairs hospitals. Med Care. 1992;30:377–91.
Cowper DC, Manheim LM, Weaver FM, Pawlow AJ. Mix and Match: VA and Non-VA Care for Elderly Veterans. VA Practitioner; 1993:41–4.
Desai RA, Rosenheck RA, Rothbard A. Cross-system service use among VA mental health patients living in Philadelphia. Adm Policy Ment Health. 2001;28:299–309.
Hoff RA, Rosenheck RA. Cross-system service use among psychiatric patients: data from the Department of Veterans Affairs. J Behav Health Serv Res. 2000;27:98–106.
Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–13.
Lowe B, Kroenke K, Herzog W, Grafe K. Measuring depression outcome with a brief self-report instrument: sensitivity to change of the Patient Health Questionnaire (PHQ-9). J Affect Disord. 2004;81:61–6.
Lowe B, Spitzer RL, Grafe K, et al. Comparative validity of three screening questionnaires for DSM-IV depressive disorders and physicians’ diagnoses. J Affect Disord. 2004;78:131–40.
Prins A, Ouimette P, Kimerling R, et al. The primary care PTSD screen (PC-PTSD): development and operating characteristics. Prim Care Companion J Clin Psychiatry. 2004;9:9–14.
Bliese PD, Wright KM, Adler AB, Cabrera O, Castro CA, Hoge CW. Validating the primary care posttraumatic stress disorder screen and the posttraumatic stress disorder checklist with soldiers returning from combat. J Consult Clin Psychol. 2008;76:272–81.
Ouimette P, Wade M, Prins A, Schohn M. Identifying PTSD in primary care: comparison of the Primary Care-PTSD screen (PC-PTSD) and the General Health Questionnaire-12 (GHQ). J Anxiety Disord. 2008;22:337–43.
Bush K, Kivlahan DR, McDonell MB, Fihn SD, Bradley KA. The AUDIT alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking. Ambulatory Care Quality Improvement Project (ACQUIP). Alcohol Use Disorders Identification Test. Arch Int Med. 1998;158:1789–1795.
Bradley KA, Bush KR, Epler AJ, et al. Two brief alcohol-screening tests from the Alcohol Use Disorders Identification Test (AUDIT): validation in a female Veterans Affairs patient population. Arch Intern Med. 2003;163:821–9.
Bradley KA, DeBenedetti AF, Volk RJ, Williams EC, Frank D, Kivlahan DR. AUDIT-C as a brief screen for alcohol misuse in primary care. Alcohol Clin Exp Res. 2007;31:1208–17.
Bradley KA, Maynard C, Kivlahan DR, McDonell MB, Fihn SD. The relationship between alcohol screening questionnaires and mortality among male veteran outpatients. J Studies Alcohol. 2001;62:826–33.
Fan VS, Au D, Heagerty P, Deyo RA, McDonell MB, Fihn SD. Validation of case-mix measures derived from self-reports of diagnoses and health. J Clin Epidemiol. 2002;55:371–380.
Wells KB, Sherbourne C, Schoenbaum M, et al. Impact of disseminating quality improvement programs for depression in managed primary care: a randomized controlled trial. JAMA. 2000;283:212–20.
Meredith LS, Orlando M, Humphrey N, Camp P, Shelbourne CD. Are better ratings of the patient-provider relationship associated with higher quality care for depression? Med Care. 2001;39:349–60.
StataCorp. Version 10. College Station, TX: StataCorp LP; 2007.
Long JA, Polsky D, Metlay JP. Changes in veterans’ use of outpatient care from 1992 to 2000. Am J Public Health. 2005;95:2246–51.
Kashner TM, Muller A, Richter E, Hendricks A, Lukas CV, Stubblefield DR. Private health insurance and veterans use of Veterans Affairs care. RATE Project Committee. Rate Alternative Technical Evaluation. Med Care. 1998;36:1085–97.
Hoff RA, Rosenheck RA. Female veterans’ use of Department of Veterans Affairs health care services. Med Care. 1998;36:1114–9.
Campbell DG, Felker BL, Liu CF, et al. Prevalence of depression-PTSD comorbidity: implications for clinical practice guidelines and primary care-based interventions. J Gen Intern Med. 2007;22:711–8.
Bhandari A, Wagner T. Self-reported utilization of health care services: improving measurement and accuracy. Med Care Res Rev. 2006;63:217–35.
Lee ML, Yano EM, Wang M, Simon BF, Rubenstein LV. What patient population does visit-based sampling in primary care settings represent? Med Care. 2002;40:761–70.
Acknowledgements
This material is based upon work supported by the Department of Veterans Affairs, Veterans Health Administration, Office of Research and Development, Health Services Research and Development (HSR&D) Service, grant MHI 99-375.
Drs. Liu, Balkan, and Chaney are at the Northwest Center for Outcomes Research in Older Adults at the Seattle VA. Drs. Rubenstein and Yano are presently at the Center for the Study for Healthcare Provider Behavior at Greater Los Angeles VA. Dr. Chan is at the Department of Department of Psychiatry and Behavioral Sciences, University of Washington School of Medicine.
The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs, or the US government, or other affiliated institutions.
Conflict of Interest
None disclosed.
Other Disclosures
No.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Liu, CF., Bolkan, C., Chan, D. et al. Dual Use of VA and Non-VA Services Among Primary Care Patients with Depression. J GEN INTERN MED 24, 305–311 (2009). https://doi.org/10.1007/s11606-008-0867-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-008-0867-7