Abstract
Background
Few pay for performance schemes have been subject to rigorous evaluation, and their impact on disparities in chronic disease management is uncertain.
Objective
To examine disparities in coronary heart disease management and intermediate clinical outcomes within a multiethnic population before and after the introduction of a major pay for performance initiative in April 2004.
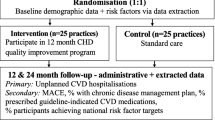
Design
Comparison of two cross-sectional surveys using electronic general practice records.
Setting
Thirty-two family practices in south London, United Kingdom (UK).
Patients
Two thousand eight hundred and ninety-one individuals with coronary heart disease registered with participating practices in 2003 and 3,101 in 2005.
Measurements
Percentage achievement by ethnic group of quality indicators in the management of coronary heart disease
Results
The proportion of patients reaching national treatment targets increased significantly for blood pressure (51.2% to 58.9%) and total cholesterol (65.7% to 73.8%) after the implementation of a major pay for performance initiative in April 2004. Improvements in blood pressure control were greater in the black group compared to whites, with disparities evident at baseline being attenuated (black 54.8% vs. white 58.3% reaching target in 2005). Lower recording of blood pressure in the south Asian group evident in 2003 was attenuated in 2005. Statin prescribing remained significantly lower (p < 0.001) in the black group compared with the south Asian and white groups after the implementation of pay for performance (black 74.8%, south Asian 83.8%, white 80.2% in 2005).
Conclusions
The introduction of pay for performance incentives in UK primary care has been associated with better and more equitable management of coronary heart disease across ethnic groups.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
INTRODUCTION
The use of pay for performance incentive schemes as a quality improvement tool is increasing, particularly in North America and the United Kingdom.1–3 Such schemes aim to improve the quality of health care for all patients so that care meets established standards. Pay for performance, therefore, provides an important opportunity to address disparities in chronic disease management between ethnic and socio-economic groups.4,5 Equally, it has been argued that pay for performance programmes have the potential to worsen health care disparities.6 Despite this few pay for performance schemes have been subject to rigorous evaluation and their impact on ethnic disparities in the quality of chronic disease management remains unclear.7,8
A new family practitioner contract, introduced in 2004 by the United Kingdom’s National Health Service, designates that around 25% of a family practitioner’s income would be determined by performance against targets in a new Quality and Outcomes Framework. The framework contains a large number of evidence-based quality indicators that were agreed between the government and family practitioners. The introduction of the new contract in the UK offers the opportunity to examine the impact of pay for performance in a healthcare system that offers universal access to health care. Statistics from the first year (2004–05) of the family practitioner contract suggest that most practices reached many of the higher Quality and Outcome Framework targets for Coronary Heart Disease (CHD).9,10 However, Quality and Outcomes Framework data, published by the Department of Health in England, are aggregated to practice level and do not permit examination of the impact of performance incentives on variations in care around key demographic variables such as age, gender and ethnicity.
Ethnic group disparities in cardiovascular disease prevalence and related health outcomes have been well documented in North America and the United Kingdom (UK).11–13 South Asians (people with ancestry in countries from the Indian sub-continent) comprise more than one-fifth of the global population and have particularly high rates of CHD related morbidity and mortality. In the UK, mortality from CHD is up to 40% higher in south Asians but appears lower in black African and Caribbean groups when compared to white groups.14
These disparities may result from inequitable access to high quality care. There is considerable evidence highlighting inequity in access to cardiovascular care between ethnic groups in the United States.15,16 Fewer studies have been conducted in the UK and in particular there is little research on the quality and appropriateness of CHD management amongst black groups. In a prospective cohort study of patients deemed appropriate for coronary artery bypass grafting attending a tertiary cardiac centre in London, south Asian patients were found to be less likely than white patients to receive surgery.17 However, in a study of over 10,000 civil servants based in London, south Asian ethnicity was not associated with lower use of cardiac procedures or drugs, independently of clinical need.18 In this paper, we test the hypothesis that pay for performance programmes reduce disparities in CHD management and outcomes within a multiethnic population.
METHODS
Pay for Performance in UK Primary Care
CHD is one of 19 disease areas within the clinical domain of the Quality and Outcomes Framework introduced in 2004.19 Of the 89 points available for CHD care, 36 are allocated for the achievement of treatment targets (blood pressure ≤ 150/90 mm Hg [19 points], cholesterol ≤ 5 mmol/L/193 mg/dl [17 points]) and the remainder to the ten prescribing and process of care measures. These include recording of blood pressure [7 points], prescribing of aspirin [7 points] and beta-blockers [7 points].
Study Setting
In England, the provision of primary care services is the responsibility of primary care trusts. There are approximately 150 primary care trusts in the country which typically cover a population of 300,000 to 400,000 people. Within each primary care trust, primary care services are delivered by family practitioners working in National Health Service (NHS) family practices. Wandsworth Primary Care Trust, located in south-west London, has established comprehensive primary care-based coronary heart disease registers. Data for the present study were collected in two cross-sectional surveys, conducted both before (June-Oct 2003) and after (Nov 2005-Jan 2006) the introduction of the new family practitioner contract in the UK in April 2004. Ethical approval for the study was granted by Wandsworth Local Research Ethics Committee.
The study area contained 36 family practices with a registered population of 243,519. The population of Wandsworth is younger than that of England, with 74% under 45 years (compared with 60% nationally). Around one in five Wandsworth residents (22%) belong to a non-white ethnic group and the borough has higher levels of socio-economic deprivation than elsewhere in England.
Identification of Patients with Coronary Heart Disease
The methods we used to develop our disease register for CHD in Wandsworth have been described previously.20 In brief, all practices in the study area were asked to participate and all patients with CHD were identified by searching for diagnoses of CHD or a repeat prescription for nitrates. Patients with management codes for a positive angiography test or for cardiac bypass surgery and coronary angioplasty were also identified. Medical records were then checked to confirm the diagnosis of CHD.
Study Variables
We examined ten quality indicators covering process of care, prescribing and intermediate clinical outcome indicators for CHD in 2003 and 2005. Eight indicators were incentivised under the family practitioner contract (smoking status recorded, cholesterol measured, blood pressure measured, prescribed aspirin, prescribed beta-blockers, prescribed angiotensin converting enzyme (ACE) inhibitors, cholesterol control, blood pressure control) and two were not (BMI measured, prescribed statins). We employed a tighter target for blood pressure (140/80 mm Hg) than that used in the new contract, in line with evidence-based guidance. Each indicator is based on clinical information recorded on the practice computer in the previous 15 months. Patients self-identified their ethnic origin from closed categories which map to classifications used in the 2001 UK census21, either at registration or during a consultation at the general practice. The main ethnic categories of the census are: white (British, Irish, other), black (African, Caribbean, other), south Asian (Indian, Pakistani, Bangladeshi, other) and Chinese. We collapsed ethnicity into three groups (white, black, south Asian) for our analyses. We excluded Chinese patients from our analysis as they were too few in number. Where ethnicity was not recorded in 2003, the 2005 status was used if present. We assigned neighbourhood socio-economic status (SES) to individual patients based on their postcode (zip code) using the Index of Multiple Deprivation (IMD) 2004.22 The Index of Multiple Deprivation is the most commonly used method of measuring neighbourhood socio-economic status in the UK and is compiled from a variety of sources, including the 2001 UK census and unemployment and social security benefits records.
Statistical Analyses
We describe percentage achievement for indicators in each ethnic group in both 2003 and 2005 and absolute percentage difference between years. We undertook multivariate logistic regression to determine the association of ethnicity (reference group: white) with the indicator variables’ odds ratios, with 95% confidence intervals, for both periods. Other independent variables in the model include age group, sex and socio-economic status. For each ethnic group, the regression was run over both years with an indicator variable for observations from 2005. Clustering of patients within family practices was taken into account by estimating robust standard errors23 as patients from the same practice are assumed to share characteristics in common, thus violating the assumption of independence. For example, south Asian patients may be more likely to register with a family practitioner who speaks their own language. The results were confirmed using a pooled random effects panel data regression (results not shown). We also assessed whether differences in achievement between the white/black and white/south Asian groups converged or diverged for each measure between 2003 and 2005. A convergence is where the ethnic group difference was significant in 2003 and is no longer significant in 2005. A divergence is where the 2005 ethnic group difference was significant and 2003 not so. Statistical analyses were performed using Stata 8.2 (College Station, TX, USA: Stata Corporation) in Microsoft Windows XP.
RESULTS
We identified 2,891 individuals with known CHD registered with the 32 participating practices in 2003 and 3,101 in 2005 (Table 1). The age standardised prevalence of CHD in 2003 was 2.1% in men and 1.5% in women. Ethnicity was recorded in 88.1% of the sample. In 2003, the mean age of the white, black and south Asian groups was 71, 68 and 66 years respectively. As the overall percentage of missing data was low (3.1%), all analyses were restricted to patients with complete information, with missing data having little bearing on our conclusions. Overall, the four practices that did not participate in the study accounted for less than 6% of the registered population in the study area. Non-participating practices were smaller (3 of 4 had fewer than 3000 patients) and located in more deprived areas than participating practices.
Process of Care Measures
Significantly more patients had their body mass index (BMI) (87.3% to 90.9%), smoking status (71.2% to 90.4%), cholesterol (83.5% to 89.7%) and blood pressure (90.6% to 97.1%) recorded in 2005 than in 2003 (Table 2). These changes were statistically significant within each ethnic group, with the exception of BMI and cholesterol. Recording of BMI did not increase significantly in black and white patients and cholesterol did not increase significantly in black and south Asian patients over this time. The recording of BMI and smoking status increased in the south Asian group such that they were significantly more likely than the white group to have this recorded in 2005. Lower recording of blood pressure in south Asian patients evident in 2003 was attenuated in 2005 (Table 3).
Prescribing
Prescribing of aspirin (81.7% to 87.6%), statins (69.3% to 80.2%), beta blockers (39.8% to 45.4%) and angiotensin converting enzyme (ACE) inhibitors (57.6% to 65.1%) all increased significantly between 2003 and 2005. These increases were statistically significant within the white and black groups. Prescribing rates also increased in the south Asian group but the increases were not statistically significant for aspirin, beta blockers and ACE inhibitors. Lower prescribing of statins in the black group evident in 2003 was not attenuated in 2005.
Intermediate Clinical Outcomes
Significantly more patients met national treatment targets for cholesterol (73.8% from 65.7%) and blood pressure (58.9% from 51.2%) in 2005 than in 2003 (Table 2). These measures improved within ethnic groups, with the exception of cholesterol which did not improve significantly in south Asian patients. However, south Asian patients were significantly more likely to meet treatment targets for cholesterol and blood pressure than white patients in 2005. Differences in blood pressure control between the black and white groups evident in 2003 were attenuated in 2005.
DISCUSSION
Principal Findings
Significantly more patients achieved established quality indicators for CHD after the implementation of a major pay for performance programme in UK primary care. The distribution of improvements between ethnic groups was such that some of the existing disparities in prescribing and intermediate clinical outcomes were attenuated. For example, worse blood pressure control in black patients relative to whites evident in 2003 was attenuated in 2005. However, black patients remained significantly less likely to be prescribed a statin after implementation of the UK pay for performance scheme.
Comparison with Previous Research
Few studies have examined the impact of pay for performance incentives on ethnic disparities in chronic disease management and outcomes.7,8 Prescribing of secondary prevention drugs increased significantly after the introduction of the new contract but levels were broadly similar between ethnic groups in both 2003 and 2005; the only exception being lower prescribing of statins in black patients in both years. These findings are in keeping with previous UK studies, including Whitehall II18 and Health Survey for England 199924, which did not identify variations in access to secondary prevention drugs between ethnic groups. However, these studies did not examine access to lipid-lowering treatments in black patients. Lower use of lipid lowering drugs in black patients with CHD and diabetes has been documented in previous studies.25,26 Our finding of poorer blood pressure control amongst black patients during 2003 is consistent with previous studies.27–29 Superior control of blood pressure and cholesterol in south Asians compared to whites confirms previous findings that conventional risk factors do not explain elevated levels of CHD in this group.12
Strengths and Limitations
We are cautious in attributing changes seen to pay for performance incentives, given the limitations of our study design; an observational study with two time points and no control group. Because the new contract for family practitioners in the UK was introduced nationally, evaluation of these incentives using a more rigorous study design, such as a randomised controlled trial, was not feasible. Recent observational studies indicate that the management of CHD in UK primary care was improving before the introduction of the contract.30 Hence, changes reported here may, in part, reflect a general trend toward higher quality care unrelated to the implementation of pay for performance incentives. In a recent study, Campbell et al.31 found pay for performance was associated with a significant increase in the overall rate of improvement for asthma and diabetes management but not for coronary heart disease management in 42 volunteer family practices in six geographical areas in England.
Our population-based study covered virtually all of the registered population in one area of south London. Hence our findings provide a comprehensive picture of the care provided in this diverse, inner city location. We employed an established and validated search strategy to identify known CHD cases. Our findings may represent a more complete picture of CHD management than that derived from national contract data, which determine individual practice income and may exclude a considerable proportion of patients who have been exception reported by practices for poor treatment compliance.10 The high percentage of patients with their ethnicity coded on practice computers (88.1%) in this study is unique in a primary care setting. We combined Indians, Pakistanis and Bangladeshis into a single ethnic category of “south Asians” and black African and Caribbeans into a combined “black” group, due to insufficient numbers in subgroups. This may have masked differences in CHD management and outcomes in what are known to be culturally and epidemiologically heterogeneous groups.32,33 We examined changes in quality using a broad range of indicators; some of which were incentivised under the family practitioner contract (measurement of total cholesterol, prescribing of aspirin and beta blockers) and others which were not (measurement of BMI, prescribing of statins). Use of routine clinical data means that there may have been some variability in the completeness and accuracy of the information collected.34 We were also unable to adjust for certain patient factors, such as duration of CHD and presence or severity of complications, which may have been confounders in the relationship between ethnicity and CHD management. Finally, given the major differences between the UK and US health care systems, the findings may not all be transferable to the US. For example, the UK’s National Health Service provides universal coverage with access to primary care services free at the point of use. This means that patients from ethnic minority groups in the UK, who are often from lower socio-economic groups, do not face financial barriers in accessing primary healthcare services.
Policy Implications
The introduction of pay for performance incentives in UK primary care has been deemed a major success, with most practices reaching many of the higher Quality and Outcome Framework targets. However, there has been little assessment of the impact of the new contract on known disparities in access to health care35–37 and health outcomes, which is a key requirement of all new government policies in the UK.38 This is largely due to the absence of patient level data in the national reporting system for the contract. Our findings suggest that pay for performance incentives in UK primary care coincided with marked improvements in CHD management and intermediate clinical outcomes, which increased equity across ethnic groups. Moreover, we found that a pay for performance programme improved chronic disease management across a range of quality indicators (both incentivised and non-incentivised), which is consistent with other studies.31 Whilst the management of CHD remains suboptimal in many patients, improvements in the quality of care seen since the new contract are impressive.
Conclusions
The introduction of a major pay for performance scheme in UK primary care was associated with marked improvements in the management of coronary heart disease. Most patients, including those from ethnic minority groups and living in areas of low socio-economic status, appear to have benefited from the scheme. Whether these improvements in process measures and intermediate outcome measures will translate into improved clinical outcomes and a further reduction in health care disparities remains to be evaluated. Healthcare planners in other countries may wish to consider the introduction of similar pay for performance schemes for their own primary care physicians.
References
Rosenthal MB, Frank RG, Li Z, Epstein AM. Early experience with pay-for-performance: from concept to practice. JAMA. 2005;294:1788–93.
Epstein AM. Paying for performance in the United States and abroad. N Engl J Med. 2006;355:406–8.
Roland M. Linking physicians’ pay to the quality of care — a major experiment in the United Kingdom. NEJM. 2004;351:1448–54.
Department of Health. (June 2004) NHS Improvement plan: Putting people at the heart of public services. London. Available at: http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_4084476 Accessed 01 October 2008.
British Medical Association (June 2005) Improving health - general practice. Available at: http://www.bma.org.uk/ap.nsf/content/ManifestoGPs. Accessed 01 October 2008
Casalino LP, Elster A. Will pay-for-performance and quality reporting affect health care disparities? Health Aff. 2007;26(3):w405–14.
Chien AT, Chin MH, Davis AM, Casalino LP. Pay for performance, public reporting, and racial disparities in health care: how are programs being designed? Med Care Res Rev. 2007;64(5 Suppl):283S–304S. Review, Oct.
Peterson L, Woodard L, Urech T, Daw C, Sookanan S. Does pay-for-performance improve the quality of health care? Ann Intern Med. 2006;145:265–72.
Health and Social Care Information Centre. National quality and outcomes framework statistics for England 2004/05. Statistical Bulletin [4], 23. 2005. Available at: http://www.ic.nhs.uk Accessed 01 October 2008
Doran T, Fullwood C, Gravelle H, et al. Pay-for-performance programs in family practices in the United Kingdom. NEJM. 2006;355(4):375–84.
Sheth T, Nair C, Nargundkar M, Anand S, Yusuf S. Cardiovascular and cancer mortality among Canadians of European, south Asian and Chinese origin from 1979 to 1993. CMAJ. 1999;161(2):132–8.
Forouhi N, Sattar N, Tillin T, McKeigue P, Chaturvedi N. Do known risk factors explain the higher coronary heart disease mortality in South Asian compared with European men? Prospective follow-up of the Southall and Brent studies, UK. Diabetologia. 2006;49(11):2580–8. Nov.
Mensah G, Mokdad A, Ford E, Greenlund K, Croft J. State of disparities in cardiovascular health in the United States. Circulation. 2005;111(10):1233–41. Mar 15.
Balarajan R. Ethnic differences in mortality from ischaemic heart disease and cerebrovascular disease in England and Wales. BMJ. 1991;3026776560–4. Mar 9.
Fiscella K, Franks P, Gold MR, Clancy CM. Inequality in quality: addressing socioeconomic, racial, and ethnic disparities in health care. JAMA. 2000;283(19):2579–84. May 17.
Institute of Medicine. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: National Academy Press; 2002. http://www.iom.edu/?id = 16740 Accessed 01 October 2008.
Feder G, Crook A, Magee P, Banerjee S, Timmis A, Hemingway H. Ethnic differences in invasive management of coronary disease: prospective cohort study if patients undergoing angiography. BMJ. 2002;324:511–6.
Britton A, Shipley M, Marmot M, Hemingway H. Does access to cardiac investigation and treatment contribute to social and ethnic differences in coronary heart disease? Whitehall II prospective cohort study. BMJ. 2004;329:318–23.
British Medical Association. General medical services contract. Available at: http://www.bma.org.uk/ap.nsf/Content/Hubthenewgmscontract Accessed 01 October 2008
Gray J, Majeed A, Kerry S, Rowlands G. Identifying patients with ischaemic heart disease in general practice: cross sectional study of paper and computerised medical records. BMJ. 2000;321:548–50.
UK 2001 Census Available at: http://www.ons.gov.uk/census/index.html Accessed 01 October 2008
Department of Communities and Local Government. Index of Multiple Deprivation 2004. Available at: http://www.communities.gov.uk/archived/general-content/communities/indicesofdeprivation/216309/ Accessed 01 October 2008
Froot KA. Consistent covariance matrix estimation with cross-sectional dependence and heteroskedasticity in financial data. J Financ Quant Anal. 1989;24:333–355.
Gill P, Quirke T, Mant J, Allan T. The use of lipid-lowering drugs across ethnic groups in the secondary prevention of ischaemic heart disease: analysis of cross-sectional surveys in England. BJGP. 2004;54:442–3.
Ferdinand K. Coronary heart disease and lipid-modifying treatment in african american patients. Heart. 2004;147(5):774–82.
Millett C, Gray J, Saxena S, Netuveli G, Khunti K, Majeed A. Ethnic Disparities in Diabetes Management and Pay-for-Performance in the UK: The Wandsworth Prospective Diabetes Study. PLoS Medicine. 2007;4(6):e191. doi:10.1371/journal.pmed.0040191.
Chaturvedi N, McKeigue P, Marmot M. Resting and ambulatory blood pressure differences in Afro-Caribbeans and Europeans. Hypertension. 1993;22:90–96.
Wolfe C, Smeeton N, Coshall C, Tilling K, Rudd A. Survival differences after stroke in a multiethnic population: follow-up study with the south London stroke register. BMJ. 2005;331(7514):431. Aug 20.
Mensah G, Mokdad A, Ford E, Greenlund K, Croft J. State of disparities in cardiovascular health in the United States. Circulation. 2005;111(10):1233–41. Mar 15.
Campbell S, Roland M, Middleton E, Reeves D. Improvements in quality of clinical care in English general practice 1998–2003: longitudinal observational study. BMJ. 2005;331:1121–5.
Campbell S, Reeves D, Kontopantelis E, Middleton E, Sibbald B, Roland M. Quality of primary care in England with the introduction of pay for performance. N Engl J Med. 2007;357:181.
Nazroo J. The health of Britain’s ethnic minorities. London: Policy Studies Institute; 1997.
Bhopal R, Unwin N, White M, et al. Heterogeneity of coronary heart disease risk factors in Indian, Pakistani, Bangladeshi and European origin populations: cross sectional study. BMJ. 1999;319:215–20.
Majeed A. Sources, uses, strengths and limitations of data collected in primary care in England. Health Stat Q. 2004;21:5–14.
Hippisley-Cox J, Pringle M, Crown N, Meal A, Wynn A. Sex inequalities in ischaemic heart disease in general practice: cross sectional survey. BMJ. 2001;322:832–8.
Ramsay S, Morris R, Papacosta O, et al. Secondary prevention of coronary heart disease in older British men: extent of inequalities before and after implementation of the National Service Framework. Am J Publ Health. 2005;27(4):338–43.
Hippisley-Cox J, Pringle M, Cater R, Coupland C, Meal A. Coronary heart disease prevention and age inequalities: the first year of the National Service Framework for CHD. BJGP. 2005;55:369–75.
Department of Health. Tackling health inequalities. A programme for action. London: Department of Health; 2003 Available at: http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_4008268 Accessed 01 October 2008.
Acknowledgments
We wish to thank practices who participated in the study. Christopher Millett is supported by a grant from the National Institute for Health Research Service Delivery and Organisation Programme. The Wandsworth Primary Care Research Centre has received funding from the Department of Health and also received support from the Medical Research Council through the VOTES (Virtual Organisation of Trials and Epidemiological Studies) project. The Department of Primary Care & Social Medicine at Imperial College is grateful for support from the National Institute for Health Research Biomedical Research Centre Scheme and the National Institutes of Health Collaboration for Leadership in Applied Health Research and Care program.
Contributors
JG, CM and AM conceived the study. MW performed the statistical analyses. All authors contributed to the data interpretation. CM wrote the first draft of the manuscript and all authors contributed to the revision and approved the final version. CM is the guarantor for the study.
Conflict of Interest
None disclosed.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Millett, C., Gray, J., Wall, M. et al. Ethnic Disparities in Coronary Heart Disease Management and Pay for Performance in the UK. J GEN INTERN MED 24, 8–13 (2009). https://doi.org/10.1007/s11606-008-0832-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-008-0832-5