Abstract
Introduction
Video-based surgical coaching is gaining traction within the surgical community. It has an increasing adoption rate and growing recognition of its utility, especially an advanced continuous professional growth tool, for continued educational purposes. This method offers instructional flexibility in real-time remote settings and asynchronous feedback scenarios. In our first paper, we delineated fundamental principles for video-based coaching, emphasizing the customization of feedback to suit individual surgeon’s needs.
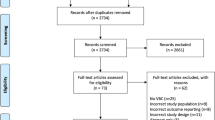
Method
In this second part of the series, we review into practical applications of video-based coaching, focusing on quality improvements in a team-based setting, such as the trauma bay. Additionally, we address the potential risks associated with surgical video recording, storage, and distribution, particularly regarding medicolegal aspects. We propose a comprehensive framework to facilitate the implementation of video coaching within individual healthcare institutions.
Results
Our paper examines the legal and ethical framework and explores the potential benefits and challenges, offering insights into the real-world implications of this educational approach.
Conclusion
This paper contributes to the discourse on integrating video-based coaching into continuous professional development. It aims to facilitate informed decision-making in healthcare institutions, considering the adoption of this innovative educational quality tool.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Video based surgical education and coaching are increasing in adoption and utility. There is a growing body of data and experience for the instructional use of video both for remote real time as well as asynchronous feedback [1]. In minimally invasive surgery, video capture is facilitated through many standard operating rooms (OR). By utilizing the intraoperative video stream, surgeons can obtain direct feedback from another surgeon who is trained in coaching either live or through an asynchronous analysis of the recorded procedures [2]. Wall mounted cameras in the operating room can also be used to assess the OR environment. Also, the recorded video can be used to evaluate performance of the team regarding quality, efficiency, and safety [3, 4].
As we transition to video based virtual surgical education (for trainees and practicing surgeons), the ability to share videos (including external to the institution) is becoming essential. The interpretation of national and state privacy and confidentiality rules regarding the capture, storage, and transmission of videos are not uniform and the policies vary amongst institutions even within the same county. However, for the continuing medical education and pursuit of surgical mastery in modern era, it requires transfer of operative videos. Guidelines for establishing and participating in video based coaching programs do not exist. In our first paper, we discussed several principles of video-based coaching to match individual surgeon’s needs [5]. In this second part in the series, we provide examples in practice, discuss the potential risks, and propose a framework to set up video coaching.
Examples of Video Coaching Program
Team-based coaching has been recognized as essential to team success in many arenas. In sports, for example, the real-time in-person observation and feedback from a coach is effectively utilized to improve team-performance. In the field of surgery, it is transitioning from in-person instructions to a video-based coaching with either remote real-time or asynchronous feedback. The transformation is facilitated by digital video recording and distribution technology [6].
Teamwork Trauma Resuscitation:
The importance of nontechnical skills in determining outcomes of high stakes team interactions has been known for some time, especially in the aviation industry. In the late 1990’s researchers at the University of Aberdeen began to devise a systematic assessment tool of the cognitive and socials skills crucial for aviation crew to manage crises. This resulted in the development of the NOTECHS (non-technical skills) system for assessing crew resource management. Eventually, in the field of surgery, the models developed in aviation became the basis of their safety tools to aid in patient safety. For example, the NOTECHS system has been used as a substrate for the development of surgery specific assessment such as the Observational Teamwork Assessment for Surgery (OTAS) which rates five different non-technical skills at three different stages of surgery (Table 1) [7]. Though the Non-Technical Skills for Surgeons (NOTSS) program is sponsored and deployed by the Royal College of Surgeons of Edinburgh [8], the trauma specific adoption of NOTECHS, T-NOTECHS (Table 2) appears to be one of the most widely employed rating system in adult medicine [9]. One of the benefits of T-NOTECHS and OTAS are the consistent scoring especially among trained scorers [10].
Unlike other forms of video review [11], T-NOTECHS was designed to assess nontechnical skills inherent in trauma resuscitation [12, 13]. This validated instrument was developed by a team of clinicians and researchers in Hawaii in the late 2000’s with this specific goal in mind. In the pursuit of improved trauma care and continuous quality improvement (QI) many trauma centers employ video review as part of their QI program. One of the author’s (VVA) institution, Penn State Milton S. Hershey Medical Center (HMC) a level III Trauma Center routinely employs video recording and subsequent evaluation utilizing the T-NOTECHS behavioral rating system on all trauma activations.
To assess all elements of the trauma resuscitation, video-based review requires the entire encounter to be recorded. In many centers, including HMC – this is done by activating a switch in the trauma bay that triggers a digital recording to start (Fig. 1C); this same switch deactivates recordings at the completion of the encounter. Multiple platforms exist for this type of system, HMC utilizes a system designed for simulation recording (B-Line Medical, Fig. 1B), though security video platform solutions have also been employed in the literature. These most often take the form of secure digital recording on encrypted drives with either standalone or network-based access.
One of the drivers in deciding between standalone vs networked access is federal and local laws as well as institutional policies regarding consent for video recording and potential liability [14]. Federal laws do not directly address this particular use scenario. However due to the obscure overlap of HIPAA and consent guidance from regulatory and accreditation organizations, institutions have adopted individualized solutions to the challenge of recording patients who may not be conscious to provide consent. HMC utilizes video for the singular purpose of quality improvement, eliminating the need for patient consent. Personnel entering the trauma bay are reminded of the possibility of recording by signage posted at all entrances (Fig. 1A). The specific quality improvement review is comprised of process improvement targeting roles, as well as leadership development targeting the trauma team leader. To maintain patient confidentiality, no patient data is linked to recordings, time and date stamps are the sole identifiers and recordings are maintained on a stand-alone workstation.
Quality improvement in this context takes the form of assessing the function of trauma resuscitation as a hospital system. Hence, these trauma bay video recordings can be used for multiple safety reviews. For example, videos can be used to assess how hospital as a whole can improve its system in taking care of trauma patients, and also to discuss specific cases (during Trauma QI case review) in a targeted manner. Also, these videos can be used for education of trauma team and the team leaders. At HMC, T-NOTECHS based review is utilized by Trauma QI review and for leadership development of Faculty and Fellows. Elements of the T-NOTECHS scoring and rubric are included in Fig. 2.
T-NOTECHS [13]. Note: Figure adapted from “Reliability of the assessment of non-technical skills by using video-recorded trauma resuscitations.” By Maarseveen OEC van, Ham WHW, Huijsmans RLN, Dolmans RGF, Leenen LPH. Reliability of the assessment of non-technical skills by using video-recorded trauma resuscitations. Eur J Trauma Emerg S. 2022;48(1):441–447.1007/s00068-020-01401-5 (licensed under the Creative Commons Attribution 4.0 International License)
Technical Education & Coaching – Colorectal specific use case
One author’s (DSK) home institution implemented a global video-based assessment system as part of their graduate medical education strategy. Implementation was facilitated using a commercially available video assessment platform in colorectal surgery (C-SATS, Johnson & Johnson, Seattle, WA). The stated purpose of this program was to develop residents’ technical skills during their surgical training. The platform license was independently purchased by our institution, and a personalized group was established for the trainees and participating attending surgeons. The platform streamlines surgical video capture and storage directly from the OR from any MIS imaging platform, and directly upload to our institution specific secure cloud-based case library.
In this program, the surgeon and the coaches reviewing the cases are usually anonymous to each other, removing the element of ego from the process. In general, all reviewing surgeons are vetted with case logs and video portfolios to ensure they are indeed experts fit to review. However, with an enterprise subscription, an individual group was set up, where the residents were identified, and their videos were sent only to institutional surgeons to review. The images are automatically captured during minimally invasive procedures and uploaded to the company’s cloud-based software into the surgeon’s HITRUST CSF® Certified case library; the videos remain the property of the surgeon who operated in the case. There is artificial intelligence (AI)-assisted removal of any identifier information from the video. Once the surgeon selects the video for review, it is auto segmented, annotated using their proprietary software, and assigned to coaches for review and comment.
As part of our program, trainees are required to upload one video weekly where they performed most steps with graded independence. Before implementation, we had verified the distinct steps of several key operations in each participating surgical specialty; for example, in colorectal surgery, the cases include the right hemicolectomy, sigmoid resection, low anterior resection, subtotal colectomy, and rectopexy. On the back end of the platform, AI algorithms are applied to automatically segment the uploaded videos by key steps and data analytics are used to objectively grade performance of the surgeon by case over time. This allows learners to compare their personal progress over time and to benchmark their performance against others at a comparable level within our personalized group. As part of the subscription, 2–3 verified expert reviewers annotate the key steps of each uploaded video and provide personalized performance improvement suggestions within 48 h of upload. Validated objective analytics GOALS and GEARS are used to assess technical skills, including efficiency, autonomy, bimanual dexterity, tissue handling, and depth perception [15, 16].
Attending surgeons from our program have access to the trainee videos and the ability to review and annotate, but this task is not required. The individual surgeons can prepare for procedures by reviewing their own videos and those of experts beforehand in addition to the post-procedure feedback; the number of times they log in and view a video is recorded and available to the attending surgeons. On the platform, there is also the opportunity for trainees to participate in peer-to-peer support and multiple communities when viewing and commenting on other videos. At the start and end of each 4-week rotation, an attending surgeon reviews the trainee’s overall performance with assistance from their performance improvement report card.
Key considerations in selecting this product were the cost, the convenience and ease of using an established product with external reviewers, auto-segmentation of key steps, and automated scoring of cases for the trainees. We found this system was simple to implement. There was no time or work required to record, store, edit, or annotate videos. There was little additional work for the attendings to watch and grade videos, though most chose to review and comment on their trainees. The platform was convenient for the trainees and trainers, as the app for the program could be accessed on any mobile device. Finally, the report cards were popular with trainees, and with consistent use, performance scores increased after each review/coaching session.
Safely Navigating Setting up Video Coaching
While there are many benefits to establishing a video-based coaching curriculum, it is important to be aware of possible risks and have plans in place to minimize risk. First, the risk of breaching the patient’s confidentiality or accidentally disclosing sensitive information from the operation must be minimized. Additionally, violating the privacy of operating room professionals is also an issue. All the healthcare professionals working in the OR expressed concerns about their privacy being violated and worry about litigation related to recording [17]. The concerns are especially evident when their personal information as well as their audio and/or visual are shared to the third party without their knowledge [18]. The concern could be addressed by utilizing technology that erases the personal identity of OR staff members and patients. Also, logistics around the video need to be considered such as storage, and file sharing policies.
The Legal Framework for Recording Video
To minimize the above risk, the legal framework should address: (1) regulation on privacy specifically on video recording; (2) video storage system such as patient record; and (3) professional secrecy [19]. In the United States, Health Insurance Portability and Accountability Act of 1996 (HIPAA) protects patients’ information, but few know which elements comprise PHI (Table 3) [20]. Also, few physicians can explain when videos become identifiable.
Furthermore, the quality improvement video can be used as evidence against the surgeon in a malpractice suit, since the duty to discover the truth outweighs protecting privacy [21]. Hence, we need to work on securing professional secrecy and de-identification of the videos. Moreover, hospitals may need to screen sensitive information (Table 3) such as financial, legal, and quality data. Hence video acquisition for coaching will be required to obtain additional hospital committee approval.
How to Safely Navigate Video Recording for Coaching?
We recommend a discussion with institutional legal representative and departmental leadership regarding video shooting, storage, and transfer. While video coaching is not specifically noted in the privacy rule under HIPAA, commercial companies have developed recording system to maintain privacy. For example, the OR Black Box can capture 360-degree-images of OR, but the video is made undiscoverable by distorting identifiable features of the individuals and removing the meta data [22]. Also, the crowd-based platforms use AI-assisted PHI removal to pixilate the image outside the body and exclude audio from the recordings [4].
With regards to storing and transfer, the secure institutional medical record system is the safest. If it is not available, acceptable alternatives are deidentified recording to place in an institution approved secure electronic file transmission system. To eliminate meta data completely, we recommend the use of Exif Tool (available at: https://exiftool.org/) on either Mac or Windows or use the native functionality of Windows through the file’s “properties” menu.
Many institutions also have policies in place that allow unrestricted use of deidentified data for the purposes of both research and quality improvement. Despite this, institutions may choose to obtain explicit consent from patients for the use of operative images for academic and training purposes. HMC for instance, includes standard language on all procedural consents authorizing image acquisition for “scientific and teaching purposes”.
Create a Video Coaching Framework
Based on our prior review article [5] and clinical experience, we are proposing the medicolegal guidelines which can be referred to when institution is introducing video coaching in their training (Table 4). Unfortunately, these are still in their infancy, so it is important to protect both coach and mentees legally for safe learning environment [23]. In the absence of guidelines, several points need to be answered by each institution. First, a recognition that images are part of patient care is critical. Patient care and surgical education are inherently connected. There is also clarification required on the definition of patient care, extensions of patient care, and consent needed for transitioning patient care into surgical education, as well as the specific safeguards tailored for specific institution. Before a surgeon takes, receives, or sends images, clear and concise guidelines from the institution should be published on how they are expected to do these tasks for PHI containing images. There should be no need for special considerations for images without PHI; if there are, the institution should also make explicit documentation regarding use and transfer (Table 5).
Additionally, there needs to be consideration for the best location to have the system to go-live. Recently, the Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) has started the MASTERS program for lifelong learning [24]. There are online programs [1, 24,25,26,27] where videos can be sent and reviewed by technical expertise like the Academy for Surgical Coaching [28]. Also, some societies may offer expertise at national or regional conference. As there are varieties of modalities, choosing the best platform for individual institution requires careful evaluation of their needs and feasibility of implementation at their institution.
The legal framework is still in its infancy and some of the questions regarding if surgical videos are free from evidence discovery process in legal cases need to be addressed. A recent review of the medicolegal system in the realm of video recording found that if the data was collected for quality improvement purposes, then the data does not need to be handed to legal team even an adverse event occurs. Interestingly, the surgical videos have been used as evidence in legal cases and many ruled in favor of the surgical team. For instance, in an American surgeon’s malpractice case, the video showed that the critical view was obtained in laparoscopic cholecystectomy operation and ruled in favor of the surgeon. In a UK case regarding retained items inside patient’s body, the video showed that all patient safety practices were followed with the surgical team and the court did not hold them accountable. In recent years, states have been changing their rules, which will affect how videos are utilized in surgical education. For example, Wisconsin state was trying to pass a legislation requiring video recordings to be part of patient’s medical record [29].
Conclusion and Next Steps
In conclusion, the rapid advancement of video-based technology over the past decade has profoundly impacted the field of surgery, enabling crucial improvements in virtual education and technical development for individual surgeons and surgical teams. For example, its implementation in trauma surgery allows for more efficient quality improvements through video review, while AI in colorectal surgery enables precise assessment and personalized feedback for trainees. In 2019, the American Board of Medical Specialties recommended modifying specialty certification with a data-driven approach. The American Board of Obstetrics and Gynecology is studying incorporating video coaching as a lifelong learning method for adult learners through surgical coaching, with both short- and long-term goals in mind. Some of the specific recommendations made for an institution to be successful are that it should set expectations at the initial visit and normalize this at the institutional level. Video feedback is recommended, along with a review on a secure online platform. Lastly, there's a recommendation to establish coaching as a lifelong principle [30].
However, as these technologies continue to evolve, regulations and hospital policies must keep pace, ensuring patient and staff privacy by removing personal identifiers, securing storage, and transferring video data, and establishing clear protocols in the absence of medico-legal guidance. Professional societies' ongoing development of video coaching modalities signifies a positive step towards embracing these innovations in a responsible and ethical manner, ultimately enhancing surgical outcomes and patient care.
Data Availability
Additional details about the programs mentioned herein may be procured from the authors upon formal request.
References
Singh P, Aggarwal R, Tahir M, Pucher PH, Darzi A. A Randomized Controlled Study to Evaluate the Role of Video-based Coaching in Training Laparoscopic Skills. Ann Surg. 2015;261(5):862–869.
Greenberg CC, Dombrowski J, Dimick JB. Video-Based Surgical Coaching: An Emerging Approach to Performance Improvement. JAMA Surg. 2016;151(3):282–3.
Xiao Y, Schimpff S, Mackenzie C, Merrell R, Entin E, Voigt R, et al. Video Technology to Advance Safety in the Operating Room and Perioperative Environment. Surg Innov. 2007;14(1):52–61.
Guerlain S, Adams RB, Turrentine FB, Shin T, Guo H, Collins SR, et al. Assessing team performance in the operating room: Development and use of a “black-box” recorder and other tools for the intraoperative environment. J Am Coll Surgeons. 2005;200(1):29–37.
Keller DS, Winslow ER, Goldberg JE, Ahuja V. Video-Based Coaching: Current Status and Role in Surgical Practice (Part 1) From the Society for Surgery of the Alimentary Tract, Health Care Quality and Outcomes Committee. J Gastrointest Surg. 2021;25(9):2439–2446.
Petrosoniak A, Welsher A, Hicks C. Tubes, lines, and videotape: a new era for quality and safety in trauma resuscitation. Can J Emerg Med Care. 2022;24(4):351–352.
Undre S, Sevdalis N, Healey AN, Darzi A, Vincent CA. Observational Teamwork Assessment for Surgery (OTAS): Refinement and Application in Urological Surgery. World J Surg. 2007;31(7):1373–1381.
Non-Technical Skills for Surgeons (NOTSS) | RCSEd [Internet]. [cited 2022 Aug 22]. https://www.rcsed.ac.uk/professional-support-developm35ent-resources/learning-resources/non-technical-skills-for-surgeons-notss
Steinemann S, Berg B, DiTullio A, Skinner A, Terada K, Anzelon K, et al. Assessing teamwork in the trauma bay: introduction of a modified “NOTECHS” scale for trauma. Am J Surg. 2012;203(1):69–75.
Hull L, Arora S, Kassab E, Kneebone R, Sevdalis N. Observational Teamwork Assessment for Surgery: Content Validation and Tool Refinement. J Am Coll Surg. 2011;212(2):234-243.e5.
Georgiou A, Lockey DJ. The performance and assessment of hospital trauma teams. Scand J Trauma Resusc Emerg Medicine. 2010;18(1):66.
Maarseveen OEC van, Ham WHW, Cruchten S van, Duhoky R, Leenen LPH. Evaluation of validity and reliability of video analysis and live observations to assess trauma team performance. Eur J Trauma Emerg S. 2022;1–7.
Maarseveen OEC van, Ham WHW, Huijsmans RLN, Dolmans RGF, Leenen LPH. Reliability of the assessment of non-technical skills by using video-recorded trauma resuscitations. Eur J Trauma Emerg S. 2022;48(1):441–447.
Williams KS, Pace C, Milia D, Juern J, Rubin J. Development of a Video Recording and Review Process for Trauma Resuscitation Quality and Education. West J Emerg Med. 2019 Mar;20(2):228-231.
Vassiliou MC, Feldman LS, Andrew CG, Bergman S, Leffondré K, Stanbridge D, et al. A global assessment tool for evaluation of intraoperative laparoscopic skills. Am J Surg. 2005;190(1):107–113.
Goh AC, Goldfarb DW, Sander JC, Miles BJ, Dunkin BJ. Global Evaluative Assessment of Robotic Skills: Validation of a Clinical Assessment Tool to Measure Robotic Surgical Skills. J Urology. 2012;187(1):247–252.
Gordon L, Reed C, Sorensen JL, Schulthess P, Strandbygaard J, Mcloone M, et al. Perceptions of safety culture and recording in the operating room: understanding barriers to video data capture. Surg Endosc. 2022;36(6):3789–3797.
Patel SJ, Guddati AK. Visibility Versus Privacy of Physicians in the Age of Social Media. Interact J Méd Res 2021; 10: e21640.
Henken KR, Jansen FW, Klein J, Stassen LPS, Dankelman J, Dobbelsteen JJ van den. Implications of the law on video recording in clinical practice. Surg Endosc. 2012;26(10):2909–2916.
Edemekong PF, Annamaraju P, Haydel MJ. Health Insurance Portability and Accountability Act. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022.
Prigoff JG, Sherwin M, Divino CM. Ethical Recommendations for Video Recording in the Operating Room. Ann Surg. 2016;264(1):34–35.
SURGICAL SAFETY TECHNOLOGIES [Internet]. [cited 2022 Sep 1]. Available from: https://www.surgicalsafety.com/index.php
Pradarelli JC, Yule S, Panda N, Craig M, Lowery KW, Ashley SW, et al. Optimizing the Implementation of Surgical Coaching Through Feedback from Practicing Surgeons. Jama Surg. 2021;156(1):42–49.
Jones DB, Stefanidis D, Korndorffer JR, Dimick JB, Jacob BP, Schultz L, et al. SAGES University MASTERS Program: a structured curriculum for deliberate, lifelong learning. Surg Endosc. 2017;31(8):3061–3071.
Pradarelli JC, Hu YY, Dimick JB, Greenberg CC. The Value of Surgical Coaching Beyond Training. Adv Surg. 2020 Sep; 54:31-47.
Jackson HT, Young MT, Rodriguez HA, Wright AS. SAGES Foregut Surgery Masters Program: a surgeon’s social media resource for collaboration, education, and professional development. Surg Endosc. 2018;32(6):2800–2807.
A Video Storage and Learning Community Built for Surgeons | C-SATS [Internet]. [cited 2022 Aug 22]. Available from: https://www.csats.com/?utm_source=bing&;utm_medium=cpc&utm_campaign=csats-2022-surgery_resources%3Bs%3Bmd%3Bbr%3Bsur%3Bhcp%3Btre&utm_content=Surgery+Resources&utm_term=surgery+coaching&gclid=efb65c41b10d105b79283e7fb28e1492&gclsrc=3p.ds&
The Academy for Surgical Coaching [Internet]. [cited 2023 May 10]. Available from: https://surgicalcoaching.org/
van Dalen ASHM, Legemaate J, Schlack WS, Legemate DA, Schijven MP. Legal perspectives on black box recording devices in the operating environment. Br J Surg. 2019 Oct;106(11):1433-1441.
Orlando MS, Greenberg CC, Pavuluri Quamme SR, Yee A, Faerber AE, King CR. Surgical coaching in obstetrics and gynecology: an evidence-based strategy to elevate surgical education and promote lifelong learning. Am J Obstet Gynecol. 2022 Jul;227(1):51-56.
Acknowledgements
The authors acknowledge the SSAT Health Care Quality and Outcomes Committee members Dmitry Oleynikov, Brett Sheppard, and Cherif Boutros for their assistance with the critical revision.
Author information
Authors and Affiliations
Contributions
Deborah S Keller, MS MD Drafting, revising, final approval.
Vamsi V Alli, MD Drafting, revising, final approval.
Emily R Winslow, MD Drafting, final approval.
Joel E Goldberg MD Drafting, final approval.
Ayaka Tsutsumi MD: critical revision of the manuscript, provision of resources, final approval.
Vanita Ahuja MD MPH EMBA Drafting, revising, final approval.
Corresponding author
Ethics declarations
All authors have read and approved the final version of the manuscript.
Ethical Approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Disclosure
Deborah S Keller, MS MD: None Declared.
Vamsi V Alli, MD: None Declared
Emily R Winslow, MD: None Declared.
Joel E Goldberg MD: None Declared.
Ayaka Tsutsumi MD: None Declared.
Vanita Ahuja MD MPH MBA: The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the United States government.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Keller, D.S., Alli, V.V., Winslow, E.R. et al. Video-based Coaching: Current Status and Role in Surgical Practice, Part II- Practical Implementation and Risk Mitigation from the Society for Surgery of the Alimentary Tract, Health Care Quality and Outcomes Committee. J Gastrointest Surg 27, 2876–2884 (2023). https://doi.org/10.1007/s11605-023-05866-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-023-05866-8