Abstract
Objective
To evaluate the significance of tumor locations in patients with resected gallbladder carcinoma (GBC) and to supply the indication of extra-hepatic bile duct resection (EHBDR) according to tumor locations.
Methods
Patients with resected GBC from 2010 to 2020 in our hospital were retrospectively analyzed. Comparative analyses and a meta-analysis were performed according to different tumor locations (body/fundus/neck/cystic duct).
Results
Article: A total of 259 patients were identified (neck: 71; cystic: 29; body: 51; fundus: 108). Patients with proximal tumors (neck/cystic duct) were often in a more advanced stage and had more aggressive tumor biological features as well as a worse prognosis compared with those with distal tumors (fundus/body). Moreover, the observation was even more obvious between cystic duct and non-cystic duct tumors. Cystic duct tumor was an independent prognostic factor for overall survival (P = 0.01). EHBDR provided no survival advantage even in those with cystic duct tumor. Meta-analysis: With our own cohort incorporated, five studies with 204 patients with proximal tumors and 5167 patients with distal tumors were identified. Pooled results revealed that proximal tumors indicated worse tumor biological features and prognosis versus distal tumors.
Conclusion
Proximal GBC had more aggressive tumor biological features, and a worse prognosis versus distal GBC and cystic duct tumor can be regarded as an independent prognostic factor. EHBDR had no obvious survival advantage even in those with cystic duct tumor and was even harmful in those with distal tumors. Upcoming more powerful well-designed studies are required for further validation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gallbladder carcinoma (GBC) is a biliary epithelium-derived rare but deadly malignancy with a reported 5-year survival rate less than 5%.1 Curative surgery provides the only chance of curing the disease, and a significantly prolonged survival could be observed in those who received radical resection.2 According to its tumor locations, such rare entity can be furtherly classified into five major categories, including lesions located in the fundus, body, neck, cystic duct, and disease with diffused spread type. Tumor location has been introduced as a vital prognostic factor, sharing similar prognostic value as lymph node status, surgical margin, tumor differentiation status, and tumor stages.3,4,5 Based on the tumor locations, Kuruhara et al. firstly classified GBC as two major subtypes: the proximal type (n = 40) and the distal type (n = 40).6 The former mainly indicated those with tumor mass located in the neck or the cystic duct, and the latter mainly indicated those with tumor mass located in the fundus or the body.6 Their results indicated that the proximal tumors were associated with more aggressive tumor biological features compared with those with distal tumors.6 Similar results were also reported by Leigh N et al. that neck tumors (n = 15) had a significantly shorter survival even with a higher R0 rate after curative resection.7 More specifically, Yu TN et al. focused on the prognostic significance of cystic duct GBC (n = 36).8 A significantly worse prognosis in patients with cystic duct tumor versus those with non-cystic duct tumor and therefore these authors recommended that cystic duct cancer should be deemed as extra-hepatic cholangiocarcinoma rather than GBC.8 Obviously, although previous studies have revealed the clinical significance of tumor locations in patients with GBC, especially lesions located in neck and cystic duct, their small sample size has continued undermining the validity of their findings. Therefore, our study was performed to have a comprehensive evaluation on the significance of tumor locations in patients with GBC, especially in those with neck and cystic tumors. Moreover, with our own single-center experience incorporated, a meta-analysis was also performed for further validation.
Besides, in our previous series, although the role of combined extra-hepatic bile duct resection (EHBDR) in the surgical management of patients with GBC has been systematically evaluated,9,10 its prognostic value with regard to different tumor locations has been rarely explored. Only Kuruhara et al. indicated that patients with proximal tumors might benefit from combined EHBDR compared with those with distal tumors with a small sample size.6 Consequently, we also explored the significance of EHBDR in patients with GBC according to different tumor locations at the same time, which might provide clinical indication of EHBDR in the curative resection of patients with GBC.
Materials and Methods
Patient Selection and Identification
Patients who received curative-intent surgery between September 2010 and September 2020 were reviewed and analyzed. Patients who have lost the follow-up as well as those without adequate clinical date would be excluded. In line with the classification criteria of the study by Kurahara et al., we identified patients with characteristic anatomical features and divided them into two major subgroups, the proximal tumor group (neck, cystic duct) and the distal tumor group (body, fundus).6 This study was approved by institutional ethics review board of West China Hospital.
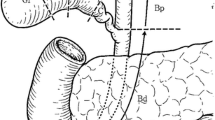
Surgical Procedures
All patients have received the standard radical cholecystectomy. Basic surgical procedures included gallbladder resection, partial hepatectomy, and a regional or more extended lymph node dissection. The extent of liver resection and lymphadenectomy was mainly driven by surgeons depending on preoperative imaging details, gross intraoperative findings as well as the information provided by intraoperative frozen biopsy. The extent of liver resection can be roughly divided into two categories: minor resection (wedge, SIVB + V) and major resection (right hemi-hepatectomy, extended right hemi-hepatectomy or tri-segmentectomy). Lymph node dissection included a regional (lymph nodes along with the cystic duct, hilum of the liver and hepatoduodenal ligament) or a more extended dissection. Lymph node status (N0, positive lymph node = 0; N1, positive lymph nodes ≤ 3; N2, positive lymph nodes > 3) was evaluated based on the latest 8th AJCC criteria. When there were no enlarged lymph nodes detected pre- or intra-operatively, the surrounding fibro-fatty tissue would be dissected and sent for pathological evaluation. EHBDR was performed when an obvious bile duct or hepatoduodenal ligament invasion was detected or there is an intraoperative pathologically-confirmed positive cystic duct margin. When the tumor directly infiltrated adjacent organs or structures, combined multi-visceral resections would be performed in order to achieve a clear surgical margin. R0 resection indicates a completely clear margin with no microresidual tumor. R1 resection indicates a relatively clear margin with no grossly tumor or the tumor is closely adjacent to the margin. R2 resection indicates macroscopic residual tumor.
Statistical Analysis
Article
IBM SPSS version 22.0 (IBM SPSS, Chicago, IL, USA) and Graph-Pad Prism 7 were used for statistical analysis. Categorical data are recorded as numbers (percentages). Categorical variables were evaluated via Chi-squared and Fisher’s exact tests. Overall survival (OS) was defined as the living period from the date of receiving radical surgery to the date of death or last follow-up. Disease-free survival (DFS) was defined as the living period from the date of receiving surgery to the date of recurrence or progression. Kaplan–Meier curves were used for evaluating survival differences. Cox-proportional hazards model was used to create multivariate model for independent prognostic factors for survival, which were presented with Hazard ratio (HR) with its 95% confidence interval (CI). P values lower than 0.05 indicated the existence of statistical significance.
Meta-Analysis
Comparative studies regarding different tumor locations were searched in PubMed, EMBASE, and the Cochrane Library. Searching key terms were restricted to gallbladder, tumor location, and cystic duct. Only published English comparative studies providing tumor location-related clinic-pathological features or survival outcome would be included. The inclusion and exclusion criteria were listed as follows: (1) published English literature; (2) comparative studies regarding different tumor locations; (3) studies with adequate clinical-pathological data or survival data for further analysis; (4) abstracts, letters, reviews, and meeting conference would be excluded; and (5) studies with data duplication would be excluded. Quality scores for included studies were analyzed according to the Newcastle–Ottawa Scale (NOS) score.11 RevMan5.3 software was used for statistical analysis. The HR with its 95% CI was applied in the survival analysis, and Tierney’s method would be used for a rough estimate of HR when not directly provided.12 The odds ratio (OR) was applied in dichotomous variables. A random-effects model would be used if the heterogeneity was > 50%; otherwise, a fixed-effects model would be used.
Results
Baseline Characteristics
A total of 259 patients with pathologically-confirmed GBC were identified, including 100 patients with proximal tumors (neck tumor: 71, cystic duct tumor: 29) and 159 patients with distal tumor (body tumor: 51; fundus tumors: 108). All patients received a standard radical cholecystectomy. Based on the 8th AJCC criteria, the number of patients with T1a, T1b, T2, T3, and T4 disease were 8, 23, 53, 105, and 70, respectively. Hepatectomy and lymphadenectomy were performed in all cases. Thirty-two (12.8%) patients received major hepatectomies. Sixty-two (23.9%) patients received bile duct resections. Thirty-six (13.9%) patients received combined multi-visceral resections. Four patients (1.5%) died within 90 days after surgery. The median survival time of the entire cohort was 29 months, ranging from 4 to 124 months. The 1-, 3-, and 5-year survival rates were 80.8%, 32.9%, and 12.2%, respectively.
Comparisons of Clinic-Pathological Features and Long-Term Survival Between Patients with Proximal and Distal Tumors
As is presented in Table 1, patients with proximal tumors and those with distal tumors are comparable in terms of age (≥ 60 vs < 60 years) and sex (male vs female). However, patients with proximal tumors had a significantly higher incidence of preoperative CA199 ≥ 37 U/ml (P = 0.021). The incidences of preoperative obstructive jaundice (P < 0.0001) and bile duct resection (P < 0.0001) were significantly higher in patients with proximal tumors. Major vascular reconstructions (portal vein or hepatic artery) (P = 0.005) were also more frequently performed in proximal tumors. The resected tumor size was significantly smaller in patients with proximal tumors that the incidence of resected tumor size lower than 3 cm was significantly higher in proximal group (P < 0.0001). The overall R0 rate was significantly lower in patients with proximal tumors (82.0% vs 95.6%, P < 0.0001). Regarding postoperative pathological findings, the incidence of peri-neural invasion (44.0% vs 11.3%, P < 0.0001) as well as lymph-vascular invasion (21.0% vs 10.1%, P = 0.012) was significantly higher in patients with proximal tumors. Patients with proximal tumors were more frequently in an advanced stage that the proportion of patients with stage III to IV disease (76.0% vs 66.0%, P = 0.001) or T3 to T4 disease (76.0% vs 62.3%, P = 0.015) disease was significantly higher in proximal group. The overall recurrence rate as well as the recurrence rate within 6 months after surgery was also significantly higher in proximal group (P < 0.05). Comparable incidences of direct liver invasion (P = 0.522), lymph node metastasis (P = 0.234), pathological subtypes (P = 0.196), tumor differentiation status (P = 0.266), postoperative morbidities (P = 0.180), and mortalities (P = 0.501) were acquired between two groups. Moreover, the incidences of receiving postoperative adjuvant chemotherapy (P = 0.545) were also comparable between two groups. Regarding survival outcomes, as is presented in Fig. 1, patients with proximal tumors share a significantly worse OS (median survival time: 19 vs 33 months, P < 0.0001) (Fig. 1A) or DFS (median recurrence-free time: 16 vs 30 months, P = 0.0002) (Fig. 1B) than those with distal tumors. We also performed subgroup analyses to evaluate the major source which might be the leading cause of the great survival difference between proximal and distal tumors. Patients with neck tumor shared comparable OS (median survival time: 33 vs 25 months, P = 0.0839) (Fig. 1C) and DFS (median recurrence-free time: 30 vs 19 months, P = 0.1079) (Fig. 1D) than those with distal tumors. However, patients with cystic duct tumor shared significantly worse OS (median survival time: 9 vs 33 months, P < 0.0001) (Fig. 1E) and DFS (median recurrence-free time: 5 vs 30 months, P < 0.0001) (Fig. 1F) than those with distal tumors. Moreover, patients with cystic duct tumor shared significantly worse OS (median survival time: 9 vs 25 months, P < 0.0001) (Fig. 1G) and DFS (median recurrence-free time: 5 vs 19 months, P < 0.0001) (Fig. 1H) than those with neck tumor. Obviously, cystic duct tumor was the leading cause of the great survival difference between proximal and distal tumors.
Kaplan–Meier curves reflecting the survival differences based on tumor locations. A OS between proximal and distal tumors; B DFS between proximal and distal tumors; C OS between neck and distal tumors; D DFS neck and distal tumors; E OS between cystic duct and distal tumors; F DFS between cystic duct and distal tumors; G OS between neck and cystic duct tumors; H DFS between neck and cystic duct tumors
Comparisons of Clinic-Pathological Features and Long-Term Survival Between Patients with Cystic Duct and Those with Non-Cystic Duct Tumors
As is presented in Table 1, similar to previous findings between the proximal and distal tumors, patients with cystic duct tumor had a significantly higher incidence of preoperative CA199 ≥ 37 U/ml than those with non-cystic duct tumor (P < 0.0001). The incidence of preoperative jaundice (P < 0.0001) as well as combined EHBDR (P < 0.0001) was also significantly higher in patients with cystic duct tumor. Moreover, major vascular reconstruction (P = 0.008), major hepatectomies (P = 0.018), and combined multi-visceral resections (P = 0.031) were also more frequently performed in patients with cystic duct tumor. The overall R0 rate was significantly lower in cystic duct tumor than those with non-cystic duct tumor (65.5% vs 93.5%, P < 0.0001). The tumor size (> 3 cm vs ≤ 3 cm) was comparable between two groups (P = 0.176). The incidence of lymph node metastasis (55.2% vs 40.0%, P = 0.087), liver invasion (69% vs 43.9%, P = 0.009), peri-neural invasion (58.6% vs 19.6%, P < 0.0001), lymph-vascular invasion (24.1% vs 13%, P = 0.097), and poorly to moderate differentiation status (93.1% vs 81.3%, P = 0.086) was significantly higher in patients with cystic duct tumor (Table 1). The proportion of patients with offstage III to IV disease or T3 to T4 disease was significantly higher in patients with cystic duct tumor (P < 0.0001). The overall recurrence rate as well as the recurrence rate within 6 months after surgery was also significantly higher in cystic duct tumor group (P < 0.05). However, the incidences of postoperative morbidities, mortalities, and postoperative adjuvant chemotherapy were comparable between two groups. Regarding survival outcomes, as is presented in Fig. 2, patients with cystic duct tumor share a significantly worse OS (median survival time: 9 vs 32 months, P < 0.0001) (Fig. 2A) or DFS (median recurrence-free time: 5 vs 28 months, P = 0.0002) (Fig. 2B) than those with non-cystic duct tumor.
Univariate and Multivariate Analysis on Prognostic Factors for OS of the Entire Cohort
As is recorded in Table 2, univariate analyses indicated that preoperative CA199 (≥ 37 U/ml vs < 37 U/ml, P < 0.0001), surgical margin (positive vs negative) (P < 0.0001), tumor location (proximal vs distal)(P < 0.0001), tumor location (cystic duct vs non-cystic duct) (P < 0.0001), lymph node metastasis (P < 0.0001), peri-neural invasion (P < 0.0001), lymph-vascular invasion (P = 0.001), liver invasion (P < 0.0001), tumor differentiation status (poor to moderate vs high) (P < 0.0001), T stage (T1-2 vs T3-4, P < 0.0001), pathological subtype (adenocarcinoma vs others, P < 0.0001), and postoperative adjuvant chemotherapy (P = 0.001) were all prognostic factors for OS of the entire cohort. Multivariate analyses indicated that surgical margin (positive vs negative) (P = 0.038), tumor location (cystic duct vs non-cystic duct) (P = 0.010), lymph node metastasis (P = 0.002), T stage (T1-2 vs T3-4, P < 0.0001) (P < 0.0001), and postoperative chemotherapy (P < 0.0001) were independent prognostic factors for OS of the entire cohort.
Further evaluation on the impact of EHBDR according to tumor locations
As summarized in Table 3, patients in the bile duct-resected group are generally in a more advanced tumor stage and received more extended radical cholecystectomies versus those in the non-resected group regardless of tumor locations. As presented in Fig. 3, EHBDR fails to improve the overall prognosis of patients with GBC that a comparable or even worse postsurgical survival was acquired in patients who received RHBDR.
Kaplan–Meier curves reflecting survival differences between those who received bile duct resection versus those without it. A OS in patients with proximal disease; B DFS in patients with proximal disease; C OS in patients with distal disease; D DFS in patients with distal disease; E OS in patients with cystic disease; F DFS in patients with cystic disease; G OS in patients with non-cystic disease; H DFS in patients with non-cystic disease
Additional Meta-Analysis Based on Different Tumor Locations
A systematic literature researching was performed in PubMed, EMBASE, and the Cochrane library, and according to the inclusion and exclusion criteria, only four relevant studies6,7,8,13 were included. With our own cohort incorporated, a total of 204 patients with proximal tumors and 5167 patients with distal tumors were finally identified (Table S1). As is summarized in Table S2 and Fig. S1, patients with proximal tumors share a significantly higher incidence of preoperative jaundice (P < 0.00001), a significantly higher preoperative CA199 level (P = 0.008), and a significantly higher incidence combined EHBDR (P < 0.00001). Moreover, lymph node metastasis (44.0% vs 36.7%, P = 0.08) and peri-neural invasion (50.0% vs 21.1%, P < 0.00001) were more frequently detected in patients with proximal tumors. Patients with proximal tumors were generally in a more advanced tumor stage than those with distal tumors (P = 0.006). The incidence of lymph-vascular invasion was comparable between two groups (P = 0.5). Patients with proximal tumors shared a significantly worse OS (P = 0.0002) or DFS (P = 0.0005) than those with distal tumors.
Discussion
The role of anatomical tumor locations in patients with GBC has always been a debating issue. Numerous studies have explored the consistencies and inconsistencies regarding biological features and long-term survival between abdominalT2 GBC and hepatic side T2 GBC. Their findings consistently indicated that T2 tumor located in the liver side shared more aggressive tumor biological features and worse prognosis than those with T2 tumor located in the abdominal side.14,15,16,17 Additionally, the latest 8th AJCC staging criteria creatively classified T2 GBC into two completely different subtypes, T2a (peritoneal side) and T2b (hepatic side).18,19 Apart from the exploration of tumor location in patients with T2 disease, others have also explored the biological features and long-term survival of tumors located in different anatomical sites within the whole gallbladder. These studies consistently indicated that tumors located in the neck or the cystic duct generally shared more aggressive tumor biological features and worse prognosis and often required a more extended range of resection.6,7,8,13 When the tumor of GBC was located in the neck or the cystic duct of the gallbladder, owing to its anatomical features that the tumor mass was extremely adjacent to extra-hepatic bile duct, a direct bile duct invasion or biliary metastasis would be more frequently detected, which would finally lead to a more advanced tumor stage and worse prognosis.20,21,22 This phenomenon was even more obvious when focused on cystic duct tumor.8
Nakata T et al. firstly analyzed the impact of tumor located in the cystic duct.13 In their study, thirteen patients with cystic duct tumor were compared with twenty-nine patients with non-cystic duct tumor, and significantly higher frequencies of lymph node metastasis and peri-neural invasion in patients with cystic duct tumor were detected.13 Similar results were also reported by Kurahara H et al. that relatively higher incidence of lymph node metastasis (15% vs 10%, P = 0.335) and peri-neural invasion (22% vs 10%, P = 0.012) was detected in patients with neck or cystic duct tumor.6 More powerful evidence from a multi-center study has also been reported that neck tumor was generally smaller than body/fundus tumor but shared more aggressive tumor biological features and worse prognosis.7 Additionally, Sakata J et al. analyzed 41 patients with primary cystic duct cancer and revealed that primary GBC patients with cystic duct tumor spread were characterized by locally advanced tumor stage and aggressive histopathological features at surgery, requiring a more extended range of resection.23 Moreover, based on the population-based data, Yu TN et al. found that it is the T staging criteria of peri-hilar cholangiocarcinoma, rather than the staging criteria of GBC, better predicated the overall prognosis of GBC with cystic duct spread.8 These observations consistently suggested that more adjacent tumor spread to the extra-hepatic bile duct, more invasive tumor biological features, and worse prognosis would be observed. In consistent with previous series, our study also proved that proximal tumors were associated with more aggressive tumor biological features and worse prognosis than those with distal tumors with a much larger sample size and a much higher level of evidence. Tumors located in the neck or cystic duct were generally smaller (P < 0.0001) but have often infiltrated more organs and structures and therefore required a wider range of resections, specially combined major vascular reconstructions (P = 0.005). Moreover, the incidences of node metastasis (P = 0.012) and peri-neural invasion (P < 0.0001) were significantly higher in patients with proximal tumors, which furtherly validated previous findings.6,13 Finally, with our own cohort incorporated, a meta-analysis was performed, which greatly validated our findings. The most important is that we also comparatively analyzed the similarities and differences between cystic duct tumor and non-cystic duct tumor. Our final results revealed that cystic duct tumor was associated with a higher incidence of combined multi-visceral resections (P = 0.031), a significantly lower R0 rate (P < 0.0001), and more aggressive tumor biological features (liver invasion, lymph node metastasis, neural invasion, and lymph-vascular invasion). Tumor located in the cystic duct can be regarded as an independent prognostic factor for OS among patients with resected GBC, which was in line with findings reported by Sakata J et al.23 and Yu TN et al.,8 suggesting the unique features of cystic duct tumor versus other non-cystic duct tumor. Therefore, some researchers even hold the view that cystic duct GBC should be classified as a subtype of extra-hepatic cholangiocarcinoma rather than GBC.8 However, for patients with cystic duct tumor in our cohort, the median survival time was only 9 months, and the median recurrence-free time was only 5 months, which seemed to be much worse than the postoperative survival information reported by others. We subjectively accounted this for the following reasons. Firstly, the sample size of cystic duct tumor was limited and was less sufficient to draw a powerful conclusion. Moreover, the proportion of patients with moderate to poor differentiation disease was significantly higher in patients with cystic duct tumor in our cohort (27/29, 93.1%), while only 65.5% (19/29) patients with cystic duct tumor have achieved negative margins. Almost all patients with cystic duct tumor were in advanced stages (III–IV) (28/29, 96.6%). Consequently, whether cystic duct cancer should be deemed as GBC or another subtype of extra-hepatic cholangiocarcinoma remains to be explored, and more powerful well-designed studies are required for further exploration.
Owing to the anatomical features of cystic duct tumor or neck tumor that the tumor mass is adjacent to the extra-hepatic bile duct, the direct extra-hepatic bile duct invasion was more frequently detected, which would furtherly lead to more advanced tumor stage and worse prognosis.20,21,22 Combined EHBDR has been routinely performed in cases with an obvious bile duct invasion. Our previous meta-analysis has evaluated the significance of EHBDR in patients with GBC, and subgroup analyses have been performed according to different tumor stages and pathological status.9 However, to our knowledge, little evidence has been provided on the indication of EHBDR according to different tumor locations.6 Therefore, we also evaluated the significance of EHBDR in patients with GBC based on different tumor locations (proximal, distal, cystic duct, and non-cystic duct). Unfortunately, consistent with our previous findings,9 combined EHBDR has no significant survival advantage, and patients who received bile duct resections were generally in a more advanced tumor stage. Moreover, EHBDR was even harmful in cases with distal tumors. However, the DFS for patients who received combined EHBDR was comparable versus those who did not receive EHBDR among patients with proximal tumors (median recurrence-free time: 13 months vs 18.5 months, P = 0.1411) or cystic duct tumor (median recurrence-free time: 5 months vs 5 months, P = 0.1317), which partially reflected the potential contribution in tumor clearance of EHBDR.
Although our study provided an in-depth analysis on the significance of tumor locations and supplied the indication of EHBDR according to different tumor locations, our study should still be interpreted with various limitations. For example, current study was based on a 10-year cohort, and the evolvement in the peri-operative management would influence the long-term survival to some extent. Moreover, the survival impact due to different pathological subtypes and chemotherapy regimens, as well as inconsistent overall preoperative health status, might also introduce bias to some extent. However, the insufficient original data hindered us from further exploration. Additionally, in the section of meta-analysis, a rough estimate of HR via Tierney’s method might also introduce bias.
Conclusion
Anatomical tumor locations of GBC had a significant impact on clinical manifestations and prognosis. Proximal tumors generally shared more aggressive tumor biological features and shared worse prognosis than those with distal tumors. Cystic duct tumor could be regarded as an independent prognostic factor for OS among patients with resected GBC. EHBDR had no survival advantage for patients with GBC and was even harmful in those with distal tumors. Upcoming more powerful and well-designed studies are warranted for further validation.
Data Availability
All data generated or analyzed during this study is included in the published article.
Abbreviations
- GBC:
-
Gallbladder carcinoma
- EHBDR:
-
Extra-hepatic bile duct resection
- HR:
-
Hazard ratio
- CI:
-
Confidence interval
- OR:
-
Odds ratio
References
Rakić M, Patrlj L, Kopljar M, Kliček R, Kolovrat M, Loncar B et al. Gallbladder cancer. Hepatobiliary surgery and nutrition. 2014;3(5):221-6. https://doi.org/10.3978/j.issn.2304-3881.2014.09.03.
Fong Y, Jarnagin W, Blumgart L. Gallbladder cancer: comparison of patients presenting initially for definitive operation with those presenting after prior noncurative intervention. Annals of surgery. 2000;232(4):557-69. https://doi.org/10.1097/00000658-200010000-00011.
Chang J, Jang JY, Lee KB, Kang MJ, Jung W, Shin YC et al. Improvement of clinical outcomes in the patients with gallbladder cancer: lessons from periodic comparison in a tertiary referral center. J Hepatobiliary Pancreat Sci. 2016;23(4):234-41. https://doi.org/10.1002/jhbp.330.
Chen C, Geng Z, Shen H, Song H, Zhao Y, Zhang G et al. Long-Term Outcomes and Prognostic Factors in Advanced Gallbladder Cancer: Focus on the Advanced T Stage. PLoS One. 2016;11(11):e0166361. https://doi.org/10.1371/journal.pone.0166361.
Yang XW, Yang J, Li L, Man XB, Zhang BH, Shen F et al. Analysis of the relationships between clinicopathologic factors and survival in gallbladder cancer following surgical resection with curative intent. PLoS One. 2012;7(12):e51513. https://doi.org/10.1371/journal.pone.0051513.
Kurahara H, Maemura K, Mataki Y, Sakoda M, Iino S, Kawasaki Y et al. Indication of extrahepatic bile duct resection for gallbladder cancer. Langenbecks Arch Surg. 2018;403(1):45-51. https://doi.org/10.1007/s00423-017-1620-7.
Leigh N, Pletcher E, Solomon D, Sarpel U, Labow DM, Magge DR et al. The significance of anatomic tumor location in gallbladder cancer. J Surg Oncol. 2021;123(4):932-8. https://doi.org/10.1002/jso.26345.
Yu TN, Mao YY, Wei FQ, Liu H. Cystic duct cancer: Should it be deemed as a type of gallbladder cancer? World journal of gastroenterology. 2019;25(44):6541-50. https://doi.org/10.3748/wjg.v25.i44.6541.
Lv T, Liu F, Hu H, Regmi P, Ma W, Yang Q et al. The role of extra-hepatic bile duct resection in the surgical management of gallbladder carcinoma. A first meta-analysis. Eur J Surg Oncol. 2022;48(3):482–491. https://doi.org/10.1016/j.ejso.2021.11.131.
Wang JK, Ma WJ, Wu ZR, Yang Q, Hu HJ, Liu F et al. Is combined extra-hepatic bile-duct resection justified for advanced gallbladder carcinoma? Gastroenterol Rep (Oxf). 2019;7(6):426-33. https://doi.org/10.1093/gastro/goz018.
Stang A. Stang A (2010) Critical evaluation of the Newcastle–Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;259(9):603–5. https://doi.org/10.1007/s10654-010-9491-z.
Tierney JF, Stewart LA, Ghersi D, Burdett S, Sydes MR. Practical methods for incorporating summary time-to-event data into meta-analysis. Trials. 2007;8:16. https://doi.org/10.1186/1745-6215-8-16.
Nakata T, Kobayashi A, Miwa S, Soeda J, Miyagawa S. Impact of tumor spread to the cystic duct on the prognosis of patients with gallbladder carcinoma. World journal of surgery. 2007;31(1):155-61; discussion 62-3. https://doi.org/10.1007/s00268-006-0118-1.
Jung W, Jang JY, Kang MJ, Chang YR, Shin YC, Chang J et al. Effects of Surgical Methods and Tumor Location on Survival and Recurrence Patterns after Curative Resection in Patients with T2 Gallbladder Cancer. Gut and liver. 2016;10(1):140-6. https://doi.org/10.5009/gnl15080.
Lee W, Jeong CY, Jang JY, Kim YH, Roh YH, Kim KW et al. Do hepatic-sided tumors require more extensive resection than peritoneal-sided tumors in patients with T2 gallbladder cancer? Results of a retrospective multicenter study. Surgery. 2017;162(3):515-24. https://doi.org/10.1016/j.surg.2017.05.004.
Shindoh J, de Aretxabala X, Aloia TA, Roa JC, Roa I, Zimmitti G et al. Tumor location is a strong predictor of tumor progression and survival in T2 gallbladder cancer: an international multicenter study. Ann Surg. 2015;261(4):733-9. https://doi.org/10.1097/sla.0000000000000728.
de Aretxabala X, Roa I, Hepp J, Maluenda F, Mordojovich G, Leon J et al. Early gallbladder cancer: is further treatment necessary? J Surg Oncol. 2009;100(7):589-93. https://doi.org/10.1002/jso.21389.
Aloia T, Járufe N, Javle M, Maithel S, Roa J, Adsay V et al. Gallbladder cancer: expert consensus statement. HPB : the official journal of the International Hepato Pancreato Biliary Association. 2015;17(8):681-90. https://doi.org/10.1111/hpb.12444.
Chun Y, Pawlik T, Vauthey J. 8th Edition of the AJCC Cancer Staging Manual: Pancreas and Hepatobiliary Cancers. Annals of surgical oncology. 2018;25(4):845-7. https://doi.org/10.1245/s10434-017-6025-x.
Lee H, Choi DW, Park JY, Youn S, Kwon W, Heo JS et al. Surgical Strategy for T2 Gallbladder Cancer According to Tumor Location. Annals of surgical oncology. 2015;22(8):2779-86. https://doi.org/10.1245/s10434-014-4300-7.
Nishio H, Ebata T, Yokoyama Y, Igami T, Sugawara G, Nagino M. Gallbladder cancer involving the extrahepatic bile duct is worthy of resection. Ann Surg. 2011;253(5):953-60. https://doi.org/10.1097/SLA.0b013e318216f5f3.
D'Angelica M, Dalal KM, DeMatteo RP, Fong Y, Blumgart LH, Jarnagin WR. Analysis of the extent of resection for adenocarcinoma of the gallbladder. Ann Surg Oncol. 2009;16(4):806-16. https://doi.org/10.1245/s10434-008-0189-3.
Sakata J, Hirose Y, Prasoon P, Kitami C, Minagawa M, Nomura T et al. Clinicopathological Characteristics and Surgical Outcomes of Primary Cystic Duct Carcinoma: A Multi-institutional Study. World J Surg. 2020;44(11):3875-83. https://doi.org/10.1007/s00268-020-05656-2.
Funding
This study was Supported by 1.3.5 project for disciplines of excellence, West China Hospital, Sichuan University (ZYJC21046); 1.3.5 project for disciplines of excellence-Clinical Research Incubation Project, West China Hospital, Sichuan University (2021HXFH001); Natural Science Foundation of Sichuan Province (2022NSFSC0806); National Natural Science Foundation of China for Young Scientists Fund (82203650, 82203782), Sichuan Science and Technology Program (2021YJ0132, 2021YFS0100); the Fellowship of China Postdoctoral Science Foundation (2021M692277); Sichuan University-Zigong School-local Cooperation project (2021CDZG-23); Science and Technology Project of the Health Planning Committee of Sichuan (21PJ046); and Post-Doctor Research Project, West China Hospital, Sichuan University (2020HXBH127).
Author information
Authors and Affiliations
Contributions
Tian-Run Lv and Jun-Ke Wang contributed equally to the study. Tian-Run Lv contributed to data acquisition and drafted the manuscript. Jun-Ke Wang contributed to the literature review, manuscript editing, and subsequent minor revision. Hai-Jie Huand Wen-Jie Ma were involved in editing the manuscript. Fu-Yu Li contributed to the study design and revision of the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lv, TR., Wang, JK., Hu, HJ. et al. The Significance of Tumor Locations in Patients with Gallbladder Carcinoma After Curative-Intent Resection. J Gastrointest Surg 27, 1387–1399 (2023). https://doi.org/10.1007/s11605-023-05665-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-023-05665-1