Abstract
Background
Population shifts among surgeons and the general populous will contribute to a predicted general surgeon shortage by 2020. The Public Policy and Advocacy Committee of the Society for Surgery of the Alimentary Tract designed and conducted a survey to assess perceptions and possible solutions from important stakeholders: practicing surgeons of the society, general surgery residents, and medical students.
Results
Responses from 1,208 participants: 658 practicing surgeons, 183 general surgery residents, and 367 medical students, were analyzed. There was a strong perception of a current and future surgeon shortage. The majority of surgeons (59.3 %) and residents (64.5 %) perceived a current general surgeon shortage, while 28.6 % of medical students responded the same. When asked of a perceived general surgery shortage in 20 years, 82.4, 81.4, and 51 % said “yes”, respectively. There were generational differences in responses to contributors and solutions for the impending shortage. Surgeons placed a high value on improving reimbursement, tort reform, and surgeon burnout, while residents held a strong interest in a national loan forgiveness program and improving lifestyle barriers.
Conclusion
Our survey offers insight into possible solutions to ward off a surgeon shortage that should be addressed with programmatic changes in residency training and by reform of the national health care system.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Scholars who investigate the future of the surgical workforce predict a significant surgeon shortage as soon as 20201 , 2 in the USA. These predictions influence medical student and resident career choices, surgeon professional expectations, and public policy decisions. Failure to understand what providers perceive limits our ability to control practice patterns within general surgery. Without data, surgeons are at the mercy of political whims and cannot properly advocate for rational health care resource allocation and decision-making.
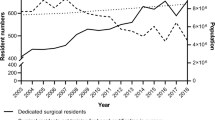
A major contributor to surgeon shortage is the aging of the general surgery workforce; approximately 32 % of general surgeons are 55 years old or older. In 2000, there were 39,000 practicing general surgeons and it is estimated that the number will drop to 30,800 by 2020. It is projected that the USA will need 52,200 practicing general surgeons in 2020.3 These numbers predict a shortage of 21,400 general surgeons. This unmet need is in the context of an aging population, which comprises an increasing percentage of the general populous.
Many theories are put forth to explain this surgeon shortage. Authors cite declining reimbursement, increasing malpractice expenses, lifestyle barriers for a younger generation, increasing early sub-specialization that bypasses general surgery training, and rising medical student debt as contributing factors for the anticipated surgeon shortage.4 The Public Policy and Advocacy Committee (PPAC) of the Society for Surgery of the Alimentary Tract (SSAT) designed and conducted a survey to assess the perceptions and possible solutions from important stakeholders: practicing surgeons who are members of the surgical society, general surgery residents, and medical students. The goal is to use the gathered data to rationally direct society activities to help combat this anticipated shortage.
Material and Methods
Questionnaire Development
The survey questions were designed by the membership of the 2011–2012 PPACFootnote 1 with guidance from the Mayo Clinic Survey Research Center. This SSAT committee is made up of surgeons in academic and community practices from across the nation. Using the current literature as a guide, this expert panel drafted surveys, in consultation with the late Doctor George Sheldon, an expert in this field, for members of the SSAT who are practicing surgeons, residents, and medical students. An Institutional Review Board at Mayo Clinic in Rochester, MN, approved this minimal risk survey.
The Mayo Clinic Survey Research Center assisted in the survey design, formatting, administration, tracking, creating reports, and analyzing the resultant data. Survey questions were completed in March of 2011. The survey was given over three time periods and utilized two modalities: web via email (March 2012 and September 2012) and paper copy by mail (December 2012). Data acquired from the survey was stored on an in-house server at Mayo Clinic in Rochester, MN, to eliminate security risk.5 The survey was closed to web and mail participants in February 2013. The initial data based on the first web survey was presented at the SSAT meeting during Digestive Disease Week in May of 2012 in San Diego, CA, and the final survey results were presented during the SSAT annual meeting during Digestive Disease Week in May of 2013 in Orlando, FL.
All groups were queried about their perceptions regarding the predicted general surgery shortage and opinions of public policy interventions that could help mitigate that shortage along with demographic questions. Practicing surgeons, residents, and medical students were all surveyed in March and April of 2012.
Subjects/Selection Criteria
Practicing Surgeons
Practicing surgeons who were active members of the SSAT and resided in the USA were invited to participate in the survey via an emailed link. The first web survey was sent to 1,796 surgeons (undeliverable, n = 72), the second to 1,234 for an overall response rate of 52.1 % (15.3 %—first web survey, 10.2 %—second web survey, and 26.6 %—third paper mailing). Surgeons who answered the first survey were excluded from subsequent email or paper mail survey requests.
Residents
An initial emailed question to the Association of Program Directors in Surgery email list to ask if they would be willing to forward this survey to their residents. Nineteen were undeliverable by email and 36 of 237 agreed to forward the survey to their residents. A letter of introduction and the resident survey was then sent via an email link to the Association of Program Directors in Surgery email list, and program directors (PDs) were asked to forward the survey to their residents followed by two reminders.
Medical Students
The Association of American Medical Colleges (AAMC) does not provide email contact information for medical students; as such, members of the PPAC submitted an IRB proposal to their own institutions: Mayo Clinic College of Medicine, the Feinberg School of Medicine, Northwestern University, the School of Medicine at the University of Virginia, David Geffen School of Medicine at University of California Los Angeles, Harvard Medical School, Uniformed Services University of Health Sciences, the College of Human Medicine at Michigan State University, Perelman School of Medicine at the University of Pennsylvania, students affiliated with the Advocate Illinois Masonic Medical Center, University of Illinois Medical School at Chicago, Chicago Medical School, New York Medical, St. Vincent’s Hospital, and New York University. A total of 367 medical students responded to the surveys.
Statistical Analysis
Categorical responses were summarized with frequencies and percentages. In order to determine the appropriateness of combining practicing surgeon responses across the two survey modes (mail and web), selected demographics (age, gender, race/ethnicity, relationship status, have children, and participation in medical volunteerism) were compared with chi-square tests. P values less than 0.05 were considered statistically significant. All analyses were performed using SAS® version 9.1 (SAS Institute, Inc., Cary, NC).
Practicing surgeons were asked to provide the zip code where they do the majority of their work; residents were asked to provide the zip code of their primary teaching hospital; and medical student were asked to provide the zip code of their medical school. Based on the zip codes provided, respondents were grouped into census regions as designated by the US Census bureau. Response percentages were calculated for each item on the survey. These percentages were used to locate the mode for each response on the medical student, resident, and attending physician surveys. Regions of the USA were based on the four groups as based on the US Census bureau and calculated from the zip code information provided. The following are included in each region: Region 1 (Northeast)—Maine, New Hampshire, Vermont, Massachusetts, Rhode Island, Connecticut, New York, Pennsylvania, New Jersey; Region 2 (Midwest)—Wisconsin, Michigan, Illinois, Indiana, Ohio, Missouri, North Dakota, South Dakota, Nebraska, Kansas, Minnesota, Iowa; Region 3 (South)—Delaware, Maryland, District of Columbia, Virginia, West Virginia, North Carolina, South Carolina, Georgia, Florida, Kentucky, Tennessee, Mississippi, Alabama, Oklahoma, Texas, Arkansas, Louisiana; and Region 4 (West)—Idaho, Montana, Wyoming, Nevada, Utah, Colorado, Arizona, New Mexico, Alaska, Washington, Oregon, California, and Hawaii.
A Wilcoxon rank sum test was run on the Likert scale topic inclusion question to compare the responses of students, residents, and attending physicians’ opinions about effective public policy initiatives.
Results
Demographics
The response rate from practicing surgeons was 51.2 % (n = 658: 126 from the first web survey, 266 from the second web survey, and 266 from mailed surveys). There was no difference in age, sex, race, or response between survey methods (P > 0.05). We were not able to calculate a response rate for residents and medical students because emails were forwarded to these participants; however, we have data from 367 medical students and 167 residents for a total of 1,208 participants of the survey.
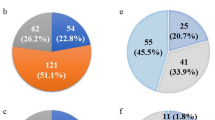
Among practicing surgeons, the most frequent responders were over the age of 61 (n = 134, 20.6 %). There were higher racial diversity and gender differences among medical students when compared to residents and practicing surgeons; however, males represented a large percentage of responders among all groups, 75.4 % of the total group. Rates of marriage were found to be higher than the general population among resident and practicing surgeon groups. Marriage status was not captured for medical students. Regional distributions (Table 1, Fig. 1a–c) were equally distributed among the Midwest, Northeast, South, and West among practicing surgeons (Fig. 1a), but for residents (Fig. 1b) and medical students (Fig. 1c) there was less representation for the western states, 8.1 and 4.3 %, respectively.
Perception of General Shortage (Practicing Surgeons and Residents)
When practicing surgeons, residents, and medical students were asked if they perceived that there was a current general surgeon shortage, they answered “yes” 59.3, 64.5, and 28.6 %, respectively. The majority of medical students were “unsure” if there was a current surgeon shortage, 35.7 %, while the majority of residents even more so that the practicing surgeons felt that there was a current shortage (Table 2). When survey responders were asked if they perceived that there would be a general surgery shortage in 20 years, 82.4, 81.4, and 51 % practicing surgeons, residents, and medical students said “yes,” respectively (Table 3). The uncertainty among medical students remained with 30 % indicating they were “unsure.”
Perceived Contributors of Surgeon Shortage (Practicing Surgeons and Residents)
Practicing surgeons felt that decreasing insurance reimbursement (30.4 %), increasing early sub-specialization (15.4 %), and lifestyle barriers for younger generation (14.1 %) were top contributors of surgeon shortage, Fig. 2a. Residents felt that decreasing insurance reimbursement (25.7 %), lifestyle barriers for younger generation (22.4 %), and increasing early specialization (12.0 %) were the top contributors, Fig. 2b. When asked what single factor contributed the most, the response was decreasing insurance reimbursement among both practicing surgeons and residents, 30.4 and 25.6 %, respectively. Early retirement and increasing frequency of emergency call contributed very little <1 % as viewed by participants, Fig. 3.
Possible Solutions to Surgeon Shortage (Practicing Surgeons and Residents)
The survey offered a range of possible solutions and participants were asked to declare agreement from strongly agree to strongly disagree on those solutions. Practicing surgeons and residents selected strongly agree for increasing insurance reimbursement (87.5 and 93.5 %), tort reform (73.3 and 82.5 %), addressing lifestyle barriers (66.0 and 79.2 %), increased hospitalists (66.0 and 79.3 %), increased surgical mentoring at medical school level (64.7 and 68.9 %), expanding residency slots (56.4 and 65.0 %), and increasing utilization of physician extenders (54.0 and 60.7 %), respectively, for issues that can help solve surgeon shortage (Fig. 4a, b). Residents and practicing surgeons felt more strongly that a national loan forgiveness program would help recruit surgeons into the field (82.5 vs. 79.2 %) but did not feel recruiting and matching at a medical school level would have an important impact (18.1 and 13.1 %). They felt the largest impact would be in the area of improved reimbursements 78.7 % among practicing surgeons and 72.1 % among residents.
Medical Student Responses
The majority of medical school responders were in the third year (47.1 %) of medical education. Of the 237 students who have completed a surgery clerkship, 41.8 % rated it an “excellent” rotation, and they stated that choice of specialty is heavily influenced by the following factors: fit with personality, 79.3 %; work life balance, 48.8 %; and mentor/role model, 47.4 %. When asked if they would consider a general surgery career, 47.1 % said “yes” and 39.5 % said “no.” The “no” responders were asked a series of questions to see what would have to improve to consider general surgery as a career. They indicated they would reconsider if there were less work hours, 69.7 %; shorter length of training, 40.7 %; less emergency call, 35.9 %; more paternity/maternity time off, 34.5 %; increased salary, 26.9 %; or loan forgiveness, 20.7 %. In concert with the answer given by the practicing surgeons and residents, 82.1 % would not consider an early “match” into surgery during medical school.
Discussion
Our survey assessed perceptions and possible solutions to an impending general surgeon shortage. The survey revealed a strong perception of a current shortage and even a stronger perception for a surgeon shortage in the future. There are generational differences in the responses for possible solutions to address this shortage. Practicing surgeons placed a high value on improved reimbursement and tort reform, and expressed concerns about increasing practice expenses and burnout. Residents echoed the same sentiments regarding need for improved reimbursement but placed more interest in a national loan forgiveness program in concert with addressing lifestyle barriers. Likewise, medical students, from the millennial generation, who initially said that they would not consider surgery as a career choice overwhelmingly said they would if lifestyle barriers (70 %) were addressed over other options such as higher income (32.4 %) or loan forgiveness programs (20.7 %). We cannot underscore enough the generational differences in the survey response. The solutions discussed below may therefore meet the needs of a segment of the workforce while not meeting the needs of another segment of a different generation and so addresses the important aspects that the survey results elucidated.
Our survey while having a very good response rate for practicing surgeons, 56 %, we were not able to sample the entire pipeline (residents and medical students) due to policies protecting trainees from direct access for the purposes of a survey and as such had to rely on forwarding of surveys by participating program directors. This is a major limitation of the study.
Contributing Factors Seen as Problems
Fiscal Considerations
Known fiscal challenges to the profession such as declining reimbursements, increasing practice expenses, and rising malpractice costs were seen as major contributors to the overall decline over the last quarter century in the area of general surgery. Contemporary politics have placed health care at the top of the list of national and local politics as the economics related to the delivery of care has become exorbitant. Health care costs now represents approximately 18 % of the gross domestic product (GDP) according to a 2011 report by the World Bank6 in the USA, behind the top two rated countries, Liberia and Sierra Leone, who notably are third world countries. In fact, the situation of health care costs is so dire that the White House released a formal statement regarding the need for economic reform in health care stating that “slowing the growth rate of health care costs will prevent disastrous increases in the Federal budget deficit.”7 The drivers of cost in health care are numerous and complex, yet the prime area and one of the easiest to tackle is physician reimbursement as a way to curtail costs. Physician reimbursement has become the driver for many recent bills, Table 4; in Congress for example, the Medicare’s sustainable growth rate (SGR) bill that passed in 1997 to help balance the budget and the subsequent bills presented to Congress to repeal the bill as it states that in 2014 there will be a 20 % cut in physician reimbursement.8
Aging Population of Patients and Surgeons
The aging of the population to include surgeons will drive a need for increased surgeons especially in the area of GI surgery. We are expected to lose over 25 % of our surgical workforce due to attrition from retired surgeons, leaving a gap for care especially in the area of oncology.3 This will be at a time when an increasingly older patient population is likely to suffer from malignancies requiring the need of qualified providers.
Lifestyle Barriers
Practicing surgeons listed increasing frequency of emergency call as a major contributor to surgeon shortage. Many individuals including the uninsured rely on emergency room visits to help manage medical conditions.9,10 Therefore, a robust call system is required to address not only emergent surgical issues but non-urgent and urgent issues as well. While the new model of acute care surgery has helped to meet this need in larger hospitals, smaller hospitals and rural areas with a single practitioner do not necessarily have access to this model. Newer models of health insurance along with changing economic schemes of coverage have also led to a decline of the private practitioner leaving the solo practitioners to fend for themselves with too much emergency room call.
The surgical culture of long work hours lead to continuity of care and early mastery; however, the millennial generation, who is now entering the workforce, finds the lifestyle to be less palatable as they place greater value on achieving balance between work and home. As such, many find the surgical lifestyle uncontrollable, unpredictable, and unattractive. Younger surgeons also are less willing to participate in general surgery emergency call, and in the era of increased patient utilization due to population shifts and potentially increased access to health care, this is of certain concern. While workforce shortage is not a new topic,11 we have not as a profession addressed problem adequately. Interestingly, our survey participants however did not cite frequent emergency room call as the area that required the most immediate focus.
Education
There were three areas that the survey highlighted as areas for concern and as major contributors to the impeding shortage: (1) increase specialization, (2) inadequate number of trainees, and (3) rising medical school debts. In the commentary section of the survey, many surgeons felt that the creation of numerous fellowships and early sub-specialization have allowed for increasing numbers of trainees to bypass traditional general surgery training.12 However, a number of these specialties fall under general surgery, and as such, these specialists continue to perform general surgery in their practice.5 The issues of sub-specialization will not likely result in a reversal in specialization as over 70 % of trainees elect to continue with fellowship training. New modes of training currently in pilot mode such as the Flexibility in Surgical Training (FIST) pilot study that will evaluate the impact of enacting the American Board of Surgery’s (ABS) new guidelines will likely help to address the issue of sub-specialization and years in training while continuing to train highly skilled general surgeons.
Second, in order to increase the denominator of surgeons, medical schools and schools of osteopathic medicine (D.O.) have realized the need for an increase in the number of physicians in the USA. Medical schools have planned an increase in medical school graduates from 16, 444 graduates in 2008–2009 to a goal of 21,647 by 2018.13 Osteopathic schools have increased the number of graduates by 4,000 graduates per year.14 A survey by Charles et al.15 that evaluated the possibility for an expansion of residency slots revealed that 123/246 programs could expand on average 1.9 residents/year (33 expansion). This expansion would address the surgeon shortage within a period of 5 years. However, the Graduate Medical Education (GME) has not increased the number and funding for more training slots in more than several decades. There are currently 246 accredited training programs in the USA that graduate 1,137 trainees in general surgery, of which roughly 909 are certified by the ABS in general surgery.5
The rising medical school debt now at an average of $120,000–160,000 upon medical school graduation and that increases to $150,000–250,000 after 3 years of residency16 puts pressure on trainees to seek specialties that have loan replacement opportunities or to join the military to help manage debt. There is currently no national loan forgiveness in general surgery. According to the National Health Service Corp, the only State that has an option for general surgery graduates to apply to work in a “state-designated shortage area” for a 3-year obligation with a maximum of $40,000 per year loan repayment is Nebraska. However, the program is not solely funded by federal funds, but it instead matched 50 % with state funds.17
Possible Solutions
Short-Term Solutions
The short-term solutions to a shortage are relatively limited. An immediate solution is to increase employment of foreign medical graduates (FMG) and engaging more graduates from schools of osteopathic medicine. As discussed, the number of graduates from American Association of Colleges of Osteopathic Medicine (AACOM) approved schools is limited as there are only 4,000 graduates annually. This is a 25 % increase over the last 10 years but not enough to sustain demand.
A more reasonable short-term strategy is the employment of foreign medical graduates to fill positions especially in areas with critical shortage, i.e., rural and certain urban areas. Currently, 14.5 % of all surgeons practicing in the US hold an international medical degree: 22.7 % in the area of general surgery, 20.3 % in colorectal surgery, and 21.9 % in thoracic surgery.18
Long-Term Solutions
GME Slot Modification
The majority of long-term solutions require policy or programmatic changes. The most obvious choice is to increase the number of GME slots in general surgery. This proposition, however, is unrealistic, as the number of GME slots in the USA in the field of general surgery has not changed since 1982. This is despite the recommendation by the Council on Graduate Medical Education (CoGME) in 1992 stating that the US population will increase a demand for surgical services, and that the number of physicians in general surgery are not adequate to provide the need for trauma care surgical services and for surgical care in rural areas.19 Perhaps the solutions should not be so broadly applied to all residencies and should instead focus on increasing general surgery spots for programs that train for practice in rural areas as this would address the dire need in these select areas.
Another focus should be the increase of underrepresented minorities in medical school with the goal to attract them to the field of surgery. Many studies have shown that this methodology may be useful to serve urban areas where the physicians from those communities can lead to a bigger impact in alleviating health care disparities.20–22
Tort Reform
Tort reform was listed as a target for eliminating surgeon shortage in our survey. The reality of its effectiveness and feasibility has not bourne out well in the past due to an inability to gain national consensus. While there is no national tort reform policy, Texas in 2003 enacted tort reform legislature that has led to an increased number of complaints but decreased rewards as reported by the Texas Medical Board. Instead of issues of negligent complaints proceeding to the courts, they are now managed by the medical board.23 However, a report from a Texas academic medical center revealed a much larger reduction of malpractice cost, measured by prevalence and cost, after tort reform was enacted in Texas, leading to a decrease in the number of malpractice lawsuits in that center.24
Early Outreach
Surgical societies can begin outreach programs as they have a national membership that could engage premedical and medical students early and expose them to the virtues of surgery as a practice. These programs could align with established programs such as the Student National Medical Association and National Medical Association to encourage the pipeline to consider the field of surgery as a career choice and more importantly obtain mentorship to help them navigate that goal. These working groups can also be established with federal and local programs to help with regional directed solutions.
Surgeons can be more engaged in medical student education during their early and non-clinical years with longitudinal patient care experiences, lectures, and summer research experiences. In fact in many medical schools across the country, these experiences are already in place for non-surgical specialties and therefore can be easily transitioned to include surgical specialties.
An obvious area where surgeons may be able to have early exposure to students and thereby attract medical students is in skill-based simulation. A survey of medical students showed that medical students were eager to learn on simulators and with simulation in the skills lab.25 The American College of Surgeons and Association for Surgical Education have developed a comprehensive skills-based simulation curriculum for medical schools years 1–3,26 while the modules can be taught in different venues, the surgeon educator is ideally suited to teach procedural skills and therefore has an opportunity to impact students early in their career choice.
Addressing Lifestyle Barriers
Based on the responses from the survey policies as a group, it is imperative that we address lifestyle barriers without modifying the integrity of training programs. One area that needs a critical focus is the area on maternity and paternity time off. This is extremely relevant as increasingly more women entering the field of general surgery. According to the ABS, women constitute 30 % of the workforce. With medical schools graduating, on average, 50 % female graduates coupled with the evolving social expectations of a husband in the home with regards to engagement in household chores, we need to find a balance between training expectations and providing adequate time off for childbearing and especially at critical times during child rearing for women and men. Flexibility in the training program is also critical to allow people time off for, family, personal interests, such as medical missions or medical volunteerism which is increasingly important to practitioners, without penalties.
Other lifestyle barriers such as the frequency of call are being addressed by the Acute Care Surgery model, surgical hospitalist, and consideration of utilizing physician extenders such as physician assistants to address this issue. Regional solutions that fit not only the culture but the available workforce are required.
Technology has potential to improve quality of practice. Smartphones and iPads® (Apple, Cupertino, CA), for example, allow videoconferencing. As this technology is integrated into practice, the surgeon will be able to assess patients without driving in at all hours of the night to see a patient. Barriers to tele-medicine vary from state to state but adaptation should be embraced. Coupled with the now federally mandated electronic medical record, tele-medicine can help meet the needs of non-emergent or urgent emergency room visits.
Teleconferencing might also help meet needs of rural consults and improve access to care. There are increasing examples of telemedicine successful capability to assist with the care of critically ill patients27–29 or the follow-up of patients with complicated comorbidities.30
Loan Forgiveness
Loan forgiveness for surgeons seems a very viable option especially to address surgical needs in the rural areas that are most vulnerable to general surgery shortages. A loan forgiveness program by the federal government would allow for an exchange of committed time for improved access to surgical care. Loan forgiveness may be the easiest and most effective first step to reallocate workforce.
Conclusion
Our survey results indicate that there is a strong perception of current and future general surgeon shortage among practicing surgeons of the SSAT and among general surgery residents. The results also highlight that the issue is a complex problem with numerous perceived probable causes and possible solutions. Identifying and accepting that the problem does and will exist is critical as this will lead to leadership responses on many levels and hopefully action led by policy changes. This requires an engaged surgical workforce and increased advocacy activities. If we ignore this compelling warning of a future workforce shortage, there may not be a general surgeon when we need one.31
Notes
SSAT Public Policy Committee, 2011–2012: Daniel B. Jones, M.D., M.S. Chair; KMarie Reid Lombardo, M.D., M.S, Co-Chair; David Bentrem, M.D.; Ross F. Goldberg, M.D.; Peter T. Hallowell, M.D.; Johnathan R. Hiatt, M.D.; Tara S. Kent, M.D., M.S.; Stuart G. Marcus, M.D.; Fabrizio Michelassi, M.D., ex-officio; Marek Rudnicki, M.D.; Shean Satgunam, M.D.; Thomas Schnelldorfer, M.D.; Richard Smith, M.D.
References
Williams, T.E., Jr. and E.C. Ellison, Population analysis predicts a future critical shortage of general surgeons. Surgery, 2008. 144(4): p. 548–54; discussion 554–6.
Williams, T.E., Jr., B. Satiani, and E.C. Ellison, A comparison of future recruitment needs in urban and rural hospitals: the rural imperative. Surgery, 2011. 150(4): p. 617–25.
Health Resources and Services Administration, Physician Supply and Demand: Projections to 2020. 2006.
Fischer, J., The impending disappearance of the general surgeon. JAMA, 2007. 298(18): p. 2191–2193.
Sheldon, G.F., Access to care and the surgeon shortage: American Surgical Association forum. Annals of Surgery, 2010. 252(4): p. 582–90.
The World Bank. Health expenditure, total (% of GDP) 2014 [cited 2014]; Available from: http://data.worldbank.org/indicator/SH.XPD.TOTL.ZS. Accessed 25 Mar 2014
Executive Office of the President of the United States, The Economic Case for Health Care Reform, Executive Office of the President Council of Economic Advisers, Editor 2009: Washington D.C.
United States Senate and House of Representatives. 105th Congress. H.R. 2015; Pages: 111, STAT. 251, Public Law 105-33: An Act to provide for reconciliation pursuant to subsections (b)(1) and (c) of section 105 of the concurrent resolution on the budget for fiscal year 1998. Short title: The Balanced Budget Act of 1997. Washington: Government Printing Office, 1997. http://www.gpo.gov/fdsys/pkg/PLAW-105publ33/html/PLAW-105publ33.htm. Accessed 24 Apr 2014
Program for uninsured cuts ED visits, admissions. Hospital Case Management, 2012. 20(10): p. 154–5.
DeHaven, M., et al., The effects of a community-based partnership, Project Access Dallas (PAD), on emergency department utilization and costs among the uninsured. Journal of Public Health, 2012. 34(4): p. 577–83.
Henningsen, J.A., Why the numbers are dropping in general surgery: the answer no one wants to hear–lifestyle! Archives of Surgery, 2002. 137(3): p. 255–6.
Borman, K.R., et al., Changing demographics of residents choosing fellowships: longterm data from the American Board of Surgery. Journal of the American College of Surgeons, 2008. 206(5): p. 782–8; discussion 788–9.
American Medical Association. AMA Physician Masterfile. 2009 [cited 2012 10/29/2012]; Available from: http://www.ama-assn.org/ama/pub/about-ama/physician-data-resources/physician-masterfile.page. Accessed 25 Mar 2014
American Association of Colleges of Osteopathic Medicine, 2011–2012 Osteopathic Medical College Total Enrollment, by State of Legal Residence, American Association of Colleges of Osteopathic Medicine, Editor 2012: Chevy Chase, MD.
Charles, A.G., et al., Increasing the number of trainees in general surgery residencies: is there capacity? Academic Medicine, 2011. 86(5): p. 599–604.
Youngclaus, J. and J. Fresne, Physician Education Debt and the Cost to Attend Medical School, 2013, Association of American Medical Colleges.
Work, S.C.S.f.S. National Health Service Corporation—State Loan Repayment Program. 2014.
Akl, E.A., et al., The United States physician workforce and international medical graduates: trends and characteristics. Journal of General Internal Medicine, 2007. 22(2): p. 264–8.
Council on Graduate Medical Education, Summary of Third Report: Improving Access to Health Care Through Physician Workforce Reform: Directions for the 21st Century Council on Graduate Medical Education 1992, U.S. Department of Health and Human Services: Washington DC
Mitchell, D. and S. Lassiter, Addressing health care disparities and increasing workforce diversity: the next step for dental, medical, and public health professions. American Journal of Public Health, 2006. 96(12): p. 2093–2097.
Armstrong, K., et al., Prior experiences of racial discrimination and racial differences in health care system distrust. Med Care, 2013. 51(2): p. 144–150.
Norris, K., et al., Historically black medical schools: addressing the minority health professional pipeline and the public mission of care for vulnerable populations. Journal of the National Medical Association, 2009. 101(9): p. 864–872.
Stewart, R.M., et al., Tort reform is associated with more medical board complaints and disciplinary actions. Journal of the American College of Surgeons, 2012. 214(4): p. 567–71; discussion 572–3.
Stewart, R.M., et al., Malpractice Risk and Cost Are Significantly Reduced after Tort Reform. Journal of the American College of Surgeons, 2011. 212(4): p. 463–467.e42.
Glass, C., et al., American College of Surgeons/Association for Surgical Education medical student simulation-based surgical skills curriculum needs assessment. American Journal of Surgery, 2014. 207(2): p. 165–169.
American College of Surgeons and Association for Surgical Education. ACS/ASE Medical Student Simulation-Based Surgical Skills Curriculum. 2013 [cited 2013]; Available from: http://www.facs.org/education/medicalstudents-MODULES.html. Accessed 25 Mar 2014
Deslich, S. and A. Coustasse, Expanding technology in the ICU: the case for the utilization of telemedicine. Telemed J E Health, 2014. 20(5): p. 485–92
Reynolds, E., et al., Utilization of robotic “remote presence” technology within North American intensive care units. Telemed J E Health, 2012. 18(7): p. 507–515.
Marcin, J., et al., Use of telemedicine to provide pediatric critical care inpatient consultations to underserved rural Northern California. J Pediatr, 2004. 144(3): p. 375–380.
Davis, L., et al., Teleneurology: Successful delivery of chronic neurologic care to 354 patients living remotely in a rural state. Telemed J E Health, 2014. 20(5): p.473–7.
Goldberg, R., et al., Will there be a good general surgeon when you need one? J Gastrointest Surg, 2013. 18(5): p. 1032–9.
Pub. L. 74-271; Pages: The Social Security Act of 1935. Short title: The Social Security Act of 1935. Washington: Government Printing Office, 1935. http://www.ssa.gov/OP_Home/ssact/title18/1848.htm. Accessed 24 Apr 2014
United States Senate and House of Representatives. 109th Congress. H.R.6111 Pages: 120, STAT. 2922, Public Law 120-432: An Act to amend the Internal Revenue Code of 1986 to extend expiring provisions, and for other purposes. Short title: Tax Relief and Health Care Act of 2006. Washington: Government Printing Office, 2006. http://www.gpo.gov/fdsys/pkg/PLAW-109publ432/html/PLAW-109publ432.htm. Accessed 24 Apr 2014
United States Senate and House of Representatives. 110th Congress. S. 2499; Pages: 121, STAT. 2942, Public Law 110-173: An act to amend titles XVIII, XIX, and XXI of the Social Security Act to extend provisions under the Medicare, Medicaid, and SCHIP programs, and for other purposes. Short title: Medicare, Medicaid, and SCHIP Extension Act of 2007. Washington: Government Printing Office, 2007. http://www.gpo.gov/fdsys/pkg/PLAW-110publ173/html/PLAW-110publ173.htm. Accessed 24 Apr 2014
United States Senate and House of Representatives. 110th Congress. H.R. 6331; Pages: 122, STAT. 2494, Public Law 110-275: An Act to amend titles XVIII and XIX of the Social Security Act to extend expiring provisions under the Medicare Program, to improve beneficiary access to preventive and mental health services, to enhance low-income benefit programs, and to maintain access to care in rural areas, including pharmacy access, and for other purposes. Short title: Medicare Improvements for Patients and Providers Act of 2008. Washington: Government Printing Office, 2008. http://www.gpo.gov/fdsys/pkg/PLAW-110publ275/pdf/PLAW-110publ275.pdf. Accessed 24 Apr 2014
United States Senate and House of Representatives. 111th Congress. H.R. 4691; Pages: 124, STAT. 42, Public Law 111-144: An Act to provide a temporary extension of certain programs, and for other purposes. Short title: Public Law 111-144: An Act to provide a temporary extension of certain programs, and for other purposes. Washington: Government Printing Office, 2010. http://www.copyright.gov/legislation/pl111-144.pdf. Accessed 24 Apr 2014
United States Senate and House of Representatives. 111th Congress, 2D Session. H.R. 4851 Amendment; Pages: 124, STAT. 1116, Public Law 111-157: An Act to suspend the Rules and Pass the Bill, H.R. 4851 “To provide a temporary extension of certain programs, and for other purposes”, with An Amendment. Short title: Continuing Extensions Act of 2010. Washington: Government Printing Office, 2010. http://npl.ly.gov.tw/pdf/7208.pdf. Accessed 24 Apr 2014
United States Senate and House of Representatives. 111th Congress. H.R. 3962; Pages: 124, STAT. 1280, Public Law 111-192: An act to provide a physician payment update, to provide pension funding relief, and for other purposes. Short title: Preservation of Access to Care for Medicare Beneficiaries and Pension Relief Act of 2010. Washington: Government Printing Office, 2010. http://www.gpo.gov/fdsys/pkg/PLAW-111publ192/html/PLAW-111publ192.htm. Accessed 24 Apr 2014
United States Senate and House of Representatives. 111th Congress, 2D Session. H.R. 4994; Pages: Public Law 111-309: An Act to amend the Internal Revenue Code of 1986 to reduce taxpayer burdens and enhance taxpayer protections, and for other purposes. Short title: Medicare and Medicaid Extenders Act of 2010. Washington: Government Printing Office, 2010. http://www.gpo.gov/fdsys/pkg/BILLS-111hr4994eas/html/BILLS-111hr4994eas.htm. Accessed 24 Apr 2014
United States Senate and House of Representatives. 112th Congress. H.R. 3630; Pages: 126, STAT. 156, Public Law 112-96: An Act to provide incentives for the creation of jobs, and for other purposes. Short title: Middle Class Tax Relief and Job Creation Act of 2012. Washington: Government Printing Office, 2012. http://www.gpo.gov/fdsys/pkg/PLAW-112publ96/pdf/PLAW-112publ96.pdf. Accessed 24 Apr 2014
United States Senate and House of Representatives. 112th Congress. H.R. 8; Pages: 126, STAT. 2313, Public Law 112-240: An Act to extend certain tax relief provisions enacted in 2001 and 2003, and to provide for expedited consideration of a bill providing for comprehensive tax reform, and for other purposes. Short title: American Taxpayer Relief Act of 2012. Washington: Government Printing Office, 2013. http://www.gpo.gov/fdsys/pkg/BILLS-112hr8eas/pdf/BILLS-112hr8eas.pdf. Accessed 24 Apr 2014
United States Senate and House of Representatives. 113th Congress. H.R. 4302; Pages: Public Law 113-93: An Act to amend the Social Security Act to extend Medicare payments to physicians and other provisions of the Medicare and Medicaid programs, and for other purposes. Short title: Protecting Access to Medicare Act of 2014. Washington: Government Printing Office, 2014. http://beta.congress.gov//bill/113th-congress/house-bill/4302/text. Accessed 24 Apr 2014
United States Senate and House of Representatives. 113th Congress, 2D Session. Pages: An Act to amend title XVIII of the Social Security Act to repeal the Medicare sustainable growth rate and improve Medicare payments for physicians and other professionals, and for other purposes. Short title: SGR Repeal and Medicare Provider Payment Modernization Act of 2014. Washington: Government Printing Office, 2014. http://energycommerce.house.gov/sites/republicans.energycommerce.house.gov/files/BILLS-113hr4015ih.pdf. Accessed 24 Apr 2014
Acknowledgments
Many thanks to the late George Sheldon, MD, FACS, for his assistance in reviewing questions and for making recommendations during the development phase of the surgeon shortage survey. This study was funded by the Society for Surgery of the Alimentary Tract.
Conflict of Interest
No financial disclosures or conflicts of interest for any of the authors.
Author information
Authors and Affiliations
Consortia
Corresponding author
Rights and permissions
About this article
Cite this article
Reid-Lombardo, K., Glass, C.C., Marcus, S.G. et al. Workforce Shortage for General Surgeons: Results from the Society for Surgery of the Alimentary Track (SSAT) Surgeon Shortage Survey. J Gastrointest Surg 18, 2061–2073 (2014). https://doi.org/10.1007/s11605-014-2636-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-014-2636-8