Abstract
Purpose
Long-term results after laparoscopic ileal pouch anal anastomosis (IPAA) have not been thoroughly evaluated. Our study prospectively compares short- and long-term outcomes of laparoscopic and open IPAA.
Methods
Between October 2002 and November 2007, 73 laparoscopic and 106 open IPAA patients were enrolled. Patient- and disease-specific characteristics and short- and long-term outcomes were prospectively collected.
Results
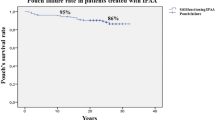
There were no differences in demographics, treatment, indication, duration of surgery, and diversion between groups. Laparoscopic patients had faster return of flatus (p = 0.008), faster assumption of a liquid diet (p < 0.001), and less blood loss (p = 0.026). While complications were similar, the incidence of incisional hernias was lower in the laparoscopic group (p = 0.011). Mean follow-up was 24.8 months. Average number of bowel movements was 6.8 ± 2.8/day for laparoscopy and 6.3 ± 1.7 for open (p = 0.058). Overall, 68.4% of patients were fully continent at 1 year, up to 83.7% long term without differences between groups. Other indicators of defecatory function and quality of life remain similar overtime.
Conclusions
Laparoscopic IPAA confers excellent functional results. Most patients are fully continent and have an average of six bowel movements/day. When present, minor incontinence improves over time. Laparoscopy mirrors the results of open IPAA and is a valuable alternative to open surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Despite significant advances in the medical treatment of ulcerative colitis (UC),1,2 surgery still remains the definitive option for UC patients who fail medical management or are diagnosed with neoplastic degeneration. Restoration of intestinal continuity with an ileal pouch anal anastomosis (IPAA) is uniformly considered the gold standard of modern management of UC patients in need of surgical treatment. A laparoscopic approach to IPAA has been proposed not only in the adult3,4 but also in the pediatric population.5 While long-term function after conventional open IPAA has been extensively analyzed,6,7 the results of laparoscopic IPAA have been reported only as single institution series8 with short follow-up9 or in small prospective randomized trials.10,11
From the limited data available, it is clear, however, that laparoscopic IPAA offers significant advantages over the open conventional procedure in terms of body image and cosmesis.11,12 Although these findings may have been expected, cosmesis and body image are important factors in the acceptance of surgery in this young patient population. The results of postoperative return of bowel function and analgesic requirements after laparoscopic IPAA have been less concordant. Although several authors have reported faster return of bowel function after laparoscopy, often associated with decreased use of narcotic pain medications,9 these findings did not always translate into a shorter hospital stay.10
On the other side of the argument, concerns have been raised regarding the longer duration of surgery often reported even by very experienced laparoscopic colon and rectal surgeons.9,10 Although this finding may in part reflect the learning curve of the surgical team, in studies comparing costs, longer duration of surgery often resulted in higher expenses.10
Though feasibility and safety remain the main issues when proposing a new procedure, especially for a benign condition in a young patient population, efficacy and functional results ought to be analyzed as well. Data on long-term sequelae after laparoscopic IPAA, such as the incidence on incisional hernias and bowel obstruction, have not to our knowledge been published. The same applies to pouch function and quality of life with very few studies reporting adequate follow-up.8,9,11,12
The number and quality of studies available does not allow us to draw any definitive conclusions on this topic to date. Clearly this is a procedure that requires a dedicated surgical team with highly sophisticated skills and expertise. To justify the additional training and expenses, long-term results of this procedure and the tangible benefits for our patients need to be further characterized. Since 2002 when laparoscopic IPAA was first introduced in our practice, we have been prospectively collecting data to answer some of these questions. In light of the need for long-term functional data on this topic, our current study was designed to prospectively analyze short- and long-term outcomes after laparoscopic IPAA in comparison with contemporary open IPAA from the same tertiary practice.
Materials and Methods
Patients and Operative Technique
Consecutive UC patients that were referred for surgery between August 2002 and November 2007 were evaluated for inclusion in this study. The decision to offer a laparoscopic approach was left to the surgeon’s assessment. No formal inclusion or exclusion criteria were defined for this study; the decision to offer laparoscopy was left to the surgeon’s judgment and experience. Although obesity and previous abdominal operations often make laparoscopic colorectal procedures difficult to complete, they were not considered absolute contraindications to laparoscopy in our study. As experience with the laparoscopic approach increased, laparoscopic-assisted IPAA has become the procedure of choice in our practice.
The indications for a stapled versus hand-sewn IPAA in our practice have been previously described13 and were applied to both the open and the laparoscopic group. Briefly, hand-sewn IPAA with a transanal mucosectomy starting at the dentate line was recommended to patients whose colonoscopic biopsy showed evidence of dysplasia, irrespective of location and severity. Stapled IPAA was recommended only after the presence of dysplasia had been ruled out by multiple endoscopic biopsies.13
Although a hand-assisted approach is a valuable alternative to laparoscopic-assisted surgery, it has not been offered to any of our patients in this series.
All the patients underwent the procedure under elective circumstances. For our laparoscopic operations we used a five, 5-mm trocar approach (Fig. 1). In case of a previous abdominal colectomy, we would start the operation by taking down the ileostomy and gaining access to the peritoneal cavity through the ileostomy site where a 12-mm trocar would be placed. All the proctectomies were performed laparoscopically with intracorporeal vessel ligation after having identified the left ureter. The specimen was exteriorized through a suprapubic Pfannenstiel incision (Fig. 1). The pouch was constructed according to the technique previously described.14 The rectal transection, pouch construction, and anastomosis were performed under direct vision through the Pfannenstiel incision. Since an incision was needed to extract the specimen, we elected to place it in the suprapubic area as a classic Pfannenstiel incision to decrease the incidence of incisional hernia and to allow the transection of the specimen and the anastomosis to be performed under direct vision. We consistently used an open stapling device, as an endoscopic stapler often requires multiple applications to divide the rectum and thus leaves overlapping staple lines. The decision to construct a diverting ileostomy was left to the surgeon’s intraoperative assessment in both groups, with ileostomy being performed when there was judged to be moderate or severe tension on the anastomosis. Conversions were defined as any diversion from the surgical plan involving early placement of an incision, irrespective of the size of the incision, or any completion of the mobilization of the specimen through the extraction site.15
Trocars placement. Specimen extraction site. Five, 5-mm trocars are used for our laparoscopic approach. The specimen is exteriorized through a suprapubic incision. The vascular division is performed intracorporeally. The rectal transection, pouch construction, and the anastomosis are performed under direct vision through the Pfannenstiel incision.
Postoperative management did not follow a formal care path, but patients from both groups were treated similarly. Diet was advanced as bowel function resumed, with clears given upon passage of flatus and solids given after patients had a bowel movement. Pain was controlled with parenteral narcotics through patient-controlled analgesia, which was weaned as patient pain could be controlled with oral medications. Early postoperative mobilization was implemented equally for both groups, and patients were discharged once they were tolerating solid food, having bowel movements, and not requiring intravenous narcotics.
Patients’ demographics, disease-specific characteristics, intraoperative variables, short-term perioperative results, and long-term postoperative outcomes were analyzed. The study was approved by the Institutional Review Board of the Division of Biologic Sciences of the University of Chicago.
Questionnaires and Data Analysis
Patients completed a previously validated two-part questionnaire at 3, 6, 9, 12, 18, and 24 months after the procedure and yearly thereafter.7 Part I evaluated bowel habits and functional parameters as well as quality of life and adjustment to the new lifestyle following the operation. Part II consisted of a week-long diary of daily frequency, timing, and consistency of bowel movements, in addition to the timing and severity of any fecal incontinence episodes.
These surveys were followed by clinic visits in which the answers were evaluated, and diet and medications reviewed. Suggestions were made to improve functional results, but the surveys were not changed. The diary results for each patient were averaged over the 7-day period and expressed as mean number of daily bowel movements, daytime and nighttime bowel movements, and percentage of bowel movements that were solid, pasty, or liquid. Additional follow-up data, including long-term complications and need for additional surgery, were collected at the clinic visits.
The results were initially analyzed comparing the open and the laparoscopic groups, along with subgroup analyses when indicated, based on body mass index (BMI) and anastomotic technique (hand-sewn versus stapled) within and between the two groups.
Statistical Analysis
Statistical analysis was performed using SPSS 14.0 (SPSS Inc., Chicago, IL, USA). Continuous variables were analyzed using independent samples t tests, and categorical variables were analyzed with the Pearson χ 2 test. The Fisher Exact Test was used for categorical variables when there were fewer than five observations in a particular group. For questionnaire measures with more than two categories, the responses were dichotomized prior to analysis. A p value of less than 0.05 was considered to indicate statistical significance.
Results
Demographics
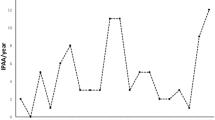
Of the 179 ulcerative colitis patients who underwent IPAA during the study period, 106 (59.2%) received an open IPAA and 73 (40.8%) a laparoscopic procedure. The percentage of patients undergoing a laparoscopic procedure has increased throughout the study period (Fig. 2). One laparoscopic patient required conversion to an open procedure for adhesions leaving a conversion rate of 1.4%. He was included in the laparoscopic group for intent to treat analysis (Table 1).
There were no significant differences in age, gender distribution, BMI, indication for surgery, percentage of patients that had undergone previous abdominal colectomy, and the use of a temporary diverting ileostomy between the groups. More patients in the laparoscopic group received a stapled IPAA (79.5% versus 56.9%, p = 0.002). The mean follow-up was 24.8 months (range = 3–60 months) and there was no difference in the length of follow-up between the two groups.
Perioperative Results
The duration of surgery was not different between groups, and blood loss was significantly less in the laparoscopic group (p = 0.026). While the overall length of stay did not vary between groups, laparoscopic IPAA patients reported passage of flatus and tolerated a liquid diet approximately 1 day earlier than the open patients (p = 0.008 and <0.001, respectively). The amount and duration of administration of parenteral narcotic pain medications were notably lower in the laparoscopic group but did not reach statistical significance (Table 2).
Postoperative Complications
There was a postoperative mortality in the laparoscopic group. The incidence of delayed return of bowel function, small bowel obstruction before or after closure of the ileostomy, and the need for surgical intervention to relieve bowel obstruction did not differ between groups. Also, the incidence of septic anastomotic complications or anastomotic strictures requiring mechanical dilatation did not differ between groups. While no patients in the laparoscopic group developed an incisional hernia, nine open IPAA patients (8.8%) were diagnosed with a hernia (p = 0.011) and eight (7.8%) required surgical repair during the study period (p = 0.022). Of these patients, 88.9% had a BMI >25. Pouch failure requiring excision was needed only in four open IPAA patients (3.9%), all for septic anastomotic complications. Three were suspicious for Crohn’s disease and were converted to a permanent end ileostomy and one had her pouch reconstructed. This difference was not statistically significant (Table 3).
Frequency and Consistency of Bowel Movements
The overall average number of daily bowel movements for the two groups was not significantly different, nor was the average number of daytime or nighttime bowel movements. In the laparoscopic group, the fraction of bowel movements that were pasty in consistency was higher than the open group (p = 0.026), while in the open group the fraction of bowel movements that were liquid in consistency was higher (p = 0.016). To eliminate the potential bias of having a higher percentage of hand-sewn anastomosis patients in the open group, we performed a subgroup analysis of the hand-sewn and the stapled IPAA patients separately. Laparoscopic hand-sewn IPAA patients had more pasty bowel movements than the open group (70% versus 48%, p = 0.003). The fraction of liquid bowel movements was not statistically different. Laparoscopic stapled IPAA patients had fewer liquid bowel movements than the open group (15.3% versus 22.9%, p = 0.008), but the difference in pasty bowel movements was not statistically significant (Table 4).
Continence
No significant differences in fecal continence were noted between the two groups. During the entire study period, only 20.8% of the laparoscopic patients and 21.9% of the open patients experienced some degree of incontinence. Similar were the fraction of patients with minor leakage (18.5% in the laparoscopic group and 20.2% in the open) and the fraction with major loss of stool (6.9% in the laparoscopic and 7.1% in the open). In line with our previous data, an improvement of continence function was evident over time in both groups.7 There were no differences in continence results within the hand-sewn and the stapled IPAA groups or within the overweight group (Table 5).
Defecatory Function
Protective pad usage mirrored the consistency of bowel movements data, with fewer laparoscopic IPAA patients wearing pads during the daytime (p < 0.001) and nighttime (p < 0.001), likely as a consequence of their lower fraction of liquid bowel movements. There was also a significantly lower fraction of patients reporting frequent perianal rash in the laparoscopic IPAA patients (p = 0.021). No significant differences were noted between the two groups for the other indicators of defecatory function. In the subgroup analysis, more overweight open IPAA patients wore protective pads at night than overweight laparoscopic patients (35% versus 16.3%, p = 0.024) and more patients in the stapled open IPAA group wore protective pads at night than in the stapled laparoscopic (20% versus 10%, p = 0.041; Table 6).
Quality of Life
In both groups, the large majority of patients similarly rated their quality of life as “better” or “much better” compared to before their IPAA or to before the ileostomy closure. There were no significant differences between groups in the percentage of patients who reported “excellent” or “good” satisfaction with the operation or in the fraction whose adjustment to the new lifestyle imposed by the operation was rated as “excellent” or “good”. In both groups, the large majority of patients would recommend the procedure to others. There were no differences in quality of life or satisfaction results within the hand-sewn and the stapled IPAA groups or within the overweight patients group (Table 7).
Discussion
We have very meticulously collected data on pouch function and outcomes in our UC patients for over two decades,7,14,16–19 for a better understanding of the correct indications for this life-changing operation and to better educate our patients. When laparoscopic IPAA was introduced in our practice in 2002, we designed this study to expand our knowledge and analysis to this new surgical approach. At the beginning of our experience, very limited data on laparoscopic IPAA were available and relatively little has been written on this topic since then.3,4,8–12,20,21
Our study offers a detailed analysis of the results of the last 5 years of laparoscopic pouch surgery for UC in a tertiary referral practice compared with the results of the contemporary open pouch surgery group. Overall, the two groups had very similar patient characteristics despite the lack of randomization. Even though the laparoscopic group includes the early phases of our learning curve, perioperative results are quite comparable between the two groups. The longer duration of laparoscopic surgery noted by many authors9,21 was not present in our series, despite similar BMI and incidence of previous colectomy between groups. The higher number of hand-sewn anastomoses in the open group may appear to have affected this result, but even when hand-sewn patients are eliminated from both groups for analysis, the operative times remain similar.
In the perioperative period, we observed a faster return of bowel function, represented by passage of flatus and assumption of a liquid diet, in the laparoscopic group, as has been previously described.4,9 However, these findings did not translate into a shorter hospital stay despite similar percentages of patients with a diverting stoma and similar incidence of postoperative complications between the two groups. Other authors have found the same discrepancy10 between return of bowel function and hospital stay.
The incidence of incisional hernia after laparotomy has been reported to be as high as 20% after a 10-year period.22 More recent studies have reported an incidence after colorectal surgery of between 12.9% and 14.7% with a follow-up up to approximately 5 years.23,24 Both studies have also reported a significant lower incidence of incisional hernias after laparoscopic colorectal resections.23,24 Based on anecdotal experience, we believe the incidence of incisional hernias to be significantly higher than reported after open surgery in the inflammatory bowel disease population with increased risk associated with malnutrition, long-term steroid use, chronic illness, and obesity that is not an uncommon finding even in inflammatory bowel disease patients. In our study, we found 8.8% of the open group with incisional hernias, with a follow-up of 24.8 months. We are expecting the incidence of incisional hernias in these patients to increase with the length of follow-up. With these concerns in mind, we have planned our laparoscopic approach to include a Pfannenstiel incision for both the extraction site and for pouch construction and anastomosis. A classic Pfannenstiel incision is a true muscle sparing incision that causes minimal weakening of the abdominal wall, thus in part explaining the fact that we have not seen any incisional hernias in the laparoscopic IPAA patients, even in those that have required an ileostomy closure. We will continue to follow these patients.
Another advantage of the Pfannenstiel incision is the ability to transect the rectum under direct vision using an open stapling device, thus avoiding multiple applications often needed with an endoscopic stapler with the resulting overlapping staple lines. Furthermore, through the Pfannenstiel, we are able to truly construct the pouch in the same way as we have described for the open approach14 and to complete the anastomosis under direct vision. By keeping the pouch construction and anastomosis consistent between the two groups, we have been able to duplicate the results previously published in our large open series.7 The difference noted in consistency of bowel movements and pad usage in favor of our laparoscopic IPAA group is difficult to explain and we will continue to investigate it during further follow-up.
One of the major limitations of the study is the lack of randomization. Additionally, as we have become increasingly comfortable with laparoscopic IPAA since adopting it in 2002, we have offered this approach to more patients, so we were not able to maintain formal inclusion or exclusion criteria for laparoscopy over the course of this study. These methodological drawbacks, however, did not result in significant differences between the characteristics of the two groups, so we believe the results we obtained are valid and valuable. Although some patients in our study did have as much as 5 years of follow-up, the average follow-up for all patients was only slightly over 2 years. While we will continue to follow these patients, we have reason to believe from our previous study7 that functional results after a 12- to 18-month adjustment period generally remain stable over the years to come, so the results from this study are likely to reflect the outcomes that would be found over an even more extended follow-up period.
Conclusions
Our study, like others currently available in the literature, supports the use of laparoscopy in UC patients in need of an IPAA. Laparoscopic IPAA provides comparable results to the traditional open approach, offers some short-term and very promising long-term benefits, and confers excellent functional outcomes.
References
Jarnerot G, Hertervig E, Friis-Liby I, et al. Infliximab as rescue therapy in severe to moderately severe ulcerative colitis: a randomized, placebo-controlled study. Gastroenterology 2005;128(7):1805–1811. doi:10.1053/j.gastro.2005.03.003.
Rutgeerts P, Sandborn WJ, Feagan BG, et al. Infliximab for induction and maintenance therapy for ulcerative colitis. N Engl J Med 2005;353(23):2462–2476. doi:10.1056/NEJMoa050516.
Larson DW, Dozois EJ, Piotrowicz K, Cima RR, Wolff BG, Young-Fadok TM. Laparoscopic-assisted vs. open ileal pouch-anal anastomosis: functional outcome in a case-matched series. Dis Colon Rectum 2005;48(10):1845–1850. doi:10.1007/s10350-005-0143-4.
Marcello PW, Milsom JW, Wong SK, et al. Laparoscopic restorative proctocolectomy: case-matched comparative study with open restorative proctocolectomy. Dis Colon Rectum 2000;43(5):604–608. doi:10.1007/BF02235570.
Meier AH, Roth L, Cilley RE, Dillon PW. Completely minimally invasive approach to restorative total proctocolectomy with j-pouch construction in children. Surg Laparosc Endosc Percutan Tech 2007;17(5):418–421.
Fazio VW, Ziv Y, Church JM, et al. Ileal pouch-anal anastomoses complications and function in 1005 patients. Ann Surg 1995;222(2):120–127. doi:10.1097/00000658-199508000-00003.
Michelassi F, Lee J, Rubin M, et al. Long-term functional results after ileal pouch anal restorative proctocolectomy for ulcerative colitis: a prospective observational study. Ann Surg 2003;238(3):433–441, discussion 42–45.
Larson DW, Davies MM, Dozois EJ, et al. Sexual function, body image, and quality of life after laparoscopic and open ileal pouch-anal anastomosis. Dis Colon Rectum 2008;51(4):392–396. doi:10.1007/s10350-007-9180-5.
Larson DW, Cima RR, Dozois EJ, et al. Safety, feasibility, and short-term outcomes of laparoscopic ileal-pouch-anal anastomosis: a single institutional case-matched experience. Ann Surg 2006;243(5):667–670, discussion 70–72. doi:10.1097/01.sla.0000216762.83407.d2.
Maartense S, Dunker MS, Slors JF, et al. Hand-assisted laparoscopic versus open restorative proctocolectomy with ileal pouch anal anastomosis: a randomized trial. Ann Surg 2004;240(6):984–991, discussion 91–92. doi:10.1097/01.sla.0000145923.03130.1c.
Polle SW, Dunker MS, Slors JF, et al. Body image, cosmesis, quality of life, and functional outcome of hand-assisted laparoscopic versus open restorative proctocolectomy: long-term results of a randomized trial. Surg Endosc 2007;21(8):1301–1307. doi:10.1007/s00464-007-9294-9.
Dunker MS, Bemelman WA, Slors JF, van Duijvendijk P, Gouma DJ. Functional outcome, quality of life, body image, and cosmesis in patients after laparoscopic-assisted and conventional restorative proctocolectomy: a comparative study. Dis Colon Rectum 2001;44(12):1800–1807. doi:10.1007/BF02234458.
Fichera A, Ragauskaite L, Silvestri MT, et al. Preservation of the anal transition zone in ulcerative colitis. Long-term effects on defecatory function. J Gastrointest Surg 2007;11(12):1647–1652, discussion 52–53. doi:10.1007/s11605-007-0321-x.
Michelassi F, Block GE. A simplified technique for ileal J-pouch construction. Surg Gynecol Obstet 1993;176(3):290–294.
Fichera A, Peng SL, Elisseou NM, Rubin MA, Hurst RD. Laparoscopy or conventional open surgery for patients with ileocolonic Crohn’s disease? A prospective study. Surgery 2007;142(4):566–571, discussion 71 e1.
Hurst RD, Chung TP, Rubin M, Michelassi F. The implications of acute pouchitis on the long-term functional results after restorative proctocolectomy. Inflamm Bowel Dis 1998;4(4):280–284. doi:10.1002/ibd.3780040405.
Hurst RD, Finco C, Rubin M, Michelassi F. Prospective analysis of perioperative morbidity in one hundred consecutive colectomies for ulcerative colitis. Surgery 1995;118(4):748–754. doi:10.1016/S0039-6060(05)80045-5.
Hurst RD, Molinari M, Chung TP, Rubin M, Michelassi F. Prospective study of the incidence, timing and treatment of pouchitis in 104 consecutive patients after restorative proctocolectomy. Arch Surg 1996;131(5):497–500.
Michelassi F, Hurst R. Restorative proctocolectomy with J-pouch ileoanal anastomosis. Arch Surg 2000;135(3):347–353. doi:10.1001/archsurg.135.3.347.
Ky AJ, Sonoda T, Milsom JW. One-stage laparoscopic restorative proctocolectomy: an alternative to the conventional approach. Dis Colon Rectum 2002;45(2):207–210, discussion 10–11. doi:10.1007/s10350-004-6149-5.
Zhang H, Hu S, Zhang G, et al. Laparoscopic versus open proctocolectomy with ileal pouch-anal anastomosis. Minim Invasive Ther Allied Technol 2007;16(3):187–191. doi:10.1080/13645700701384090.
Akman PC. A study of five hundred incisional hernias. J Int Coll Surg 1962;37:125–142.
Andersen LP, Klein M, Gögenur I, Rosenberg J. Incisional hernia after open versus laparoscopic sigmoid resection. Surg Endosc 2008;22(9):2026–2029.
Duepree HJ, Senagore AJ, Delaney CP, Fazio VW. Does means of access affect the incidence of small bowel obstruction and ventral hernia after bowel resection? Laparoscopy versus laparotomy. J Am Coll Surg 2003;197(2):177–181. doi:10.1016/S1072-7515(03)00232-1.
Author information
Authors and Affiliations
Corresponding author
Additional information
This study was funded in part by the University of Chicago Cancer Research Foundation (UCCRF) Auxiliary Board Research Support Grant (A.F.).
Rights and permissions
About this article
Cite this article
Fichera, A., Silvestri, M.T., Hurst, R.D. et al. Laparoscopic Restorative Proctocolectomy with Ileal Pouch Anal Anastomosis: A Comparative Observational Study on Long-term Functional Results. J Gastrointest Surg 13, 526–532 (2009). https://doi.org/10.1007/s11605-008-0755-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-008-0755-9