Abstract
Background and Aims
While colonic resection is standard practice in complicated colonic diverticular disease (DD), treatment of uncomplicated diverticulitis is, as yet, unclear. The aim of the present study was to evaluate the long-term clinical outcome and quality of life in DD patients undergoing colonic resection compared to those receiving medical treatment only.
Patients and Methods
Seventy-one consecutive patients who were admitted to our surgical department with left iliac pain and endoscopical or radiological diagnosis of DD were enrolled in this trial. Disease severity was assessed with Hinchey scale. Twenty-five of the patients underwent colonic resection, while 46 were treated with medical therapy alone. After a median follow-up of 47 (3–102) months from the time of their first hospital admission, the patients responded to the questions of the Cleveland Global Quality of Life (CGQL) questionnaire and to a symptoms questionnaire during a telephone interview. Admittance and surgical procedures for DD were also investigated, and surgery- and symptoms-free survival rates were calculated. Nonparametric tests and survival analysis were used.
Results
The CGQL total scores and symptom frequency rate were found to be similar in the two groups (resection vs nonresection). Only current quality of health item was significantly worse in patients who had undergone colonic resection (p = 0.05). No difference was found in the rate and in the timing of surgical procedures and hospital admitting for DD in the two groups. In particular, the nine patients classified as Hinchey 1 who underwent surgery reported the same quality of life, symptoms frequency, operation, and hospital admitting rate as those who had been admitted with the same disease class but who received medical treatment only.
Conclusions
Our results indicate that there does not seem to be any long-term advantage to colonic resection which should be considered only in patients presenting complicated DD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Diverticular disease (DD) of the colon is common in the Western world, accounting for more than 200,000 hospitalizations annually, health care costs of more than $300 million, and with a prevalence of approximately 33% in patients over 60 years of age.1,2 Perforation associated with diverticular disease has concurrently increased in prevalence from 2.4 cases per 100,000 in 1986 to 3.8 cases per 100,000 in 2000.3
Colonic resection is standard practice when there is perforation and peritonitis. Primary anastomosis with defunctioning stoma seems to be the optimal surgical strategy for fit patients with diverticular peritonitis as it seems to be a good compromise between postoperative complications, long-term quality of life, and risk of requiring permanent stoma. Hartmann’s procedure is, instead, recommended in high-risk patients.4
Treatment of acute diverticulitis without perforation and peritonitis is yet unclear. In these cases, nonoperative management is usually successful,1,5 but up to 25% of these patients may end to require an urgent operation,6 and more than half of these procedures involve a colostomy.7–9 Elective colectomy is, thus, often recommended to avoid the risks and high mortality rate connected to emergency surgery usually associated with recurrent diverticulitis. The timing of elective surgery is, nevertheless, controversial, with most advisory bodies recommending surgery after the second episode.1,10 Many surgeons, however, advise prophylactic colon resection after a single hospitalization in younger patients because the disease is considered more virulent in these subjects.10–13 Advances in laparoscopic colonic surgery have widened the spectrum of indications, and a large multicentric study has recently reported that 87% of the patients undergoing this procedure are affected with an uncomplicated DD.14
The aim of the present study was to evaluate the impact of colonic resection for DD on the natural history and on the long-term quality of life of these patients. The study was particularly focused on the long-term clinical outcome of noncomplicated diverticulitis.
Patients and Methods
Patients
The hospital records as well as the clinical and surgical follow-up files of 149 consecutive patients who had been admitted to the Department of Surgical and Gastroenterological Sciences of the University of Padova from 1998 to 2005 with a diagnosis of DD were reviewed. Attempt was made to contact all of these, and the 71 who agreed to submit to a telephone interview were enrolled in our cross-sectional study. Healthy, normal subjects were also enrolled as controls.
The diagnosis of diverticular disease was based on a report of a barium enema, a colonoscopy, or both. At admission, all patients with left iliac fossa pain underwent plain abdomen X-ray and ultrasound (US) or computed tomography (CT) scan, and Hinchey 4-stage classification was usedto assess severity of DD.15 Hinchey stage 1 indicates acute phlegmonous diverticulitis without complications; Hinchey stage 2 diverticulitis with paracolic abscess without perforation; Hinchey stage 3 diffuse purulent peritonitis; and Hinchey stage 4 diffuse fecal peritonitis. Patients with no sign of perforation were conventionally classified as Hinchey 0.
Patients with Hinchey stage 2, 3, or 4 DD were treated with antibiotics, laparotomy, colonic resection, and if necessary, diverting stoma; the minimally invasive approach with percutaneous CT or US-guided drainage was always attempted to manage Hinchey stage 2 patients; subjects with nonperforated DD and Hinchey stage 1 DD were treated with antibiotic therapy, while colonic resection was considered whenever the patient reported more than two previous episodes of acute DD or in case of inflammatory stenosis.
Quality of life was also assessed in 69 healthy subjects [39 males and 30 females with a mean age of 43 (22–85) years] without gastroenteric symptoms enlisted from among hospital employees and their relatives
Study Design
Patients were enrolled in the study provided that they were admitted for abdominal pain, obstruction, or rectal bleeding and a confirmed diagnosis of diverticular disease. They were included in the medical group if they were treated with medical therapy and in the surgical group if they hada colonic resection. Patients also presenting other bowel diseases associated to Crohn’s disease such as colon cancer were excluded. The study was conducted in accordance with the principles to Helsinki Declaration contacted by phone, all of the patients were provided information about the methods and the study’s purposes, and those agreeing to give informed consent and to submit to a telephone interview were enlisted.
The long-term outcome of DD patients who underwent colonic resection or who were treated with medical therapy was compared. The outcome measures analyzed were: readmission to the hospital and/or further surgery for DD, current health status (fever, abdominal pain, constipation, diarrhea, rectal bleeding, and bloating), and quality of life. Each of these parameters was analyzed according to possible predictors such as gender, age at admission, symptoms at admission (fever, abdominal pain, constipation, diarrhea, rectal bleeding, and bloating), Hinchey disease severity class, indication for surgery, laparoscopy/laparotomy approach, the need of a diverting stoma, postoperative surgical and intestinal complications, co-morbidity, and medical therapy.
Italian Cleveland Global Quality of Life Questionnaire
The Cleveland Global Quality of Life (CGQL) score consists in three items (current quality of life, current quality of health, and current energy level), each on a scale of 0 to 10 (0, worst; 10, best). The scores were added, and the final CGQL utility was obtained by dividing this result by 30.16 The CGQL was created to assess health-related quality of life (HRQL) in patients affected by ulcerative colitis after restorative proctocolectomy and then was used in HRQL analysis of patients with Crohn’s disease.17,18 Given its short framework, the Italian translation, recently validated in one of our previous studies,19 was considered a suitable instrument for telephone interviews.
Surgical Technique
In open colonic resection, the exploration of the abdomen, the mobilization of the colon, the identification of the critical structures, the section of the vascular pedicle, the resection of the diseased colon, and the anastomosis were performed through a xifo-pubic midline incision. The extension of the resection was decided intraoperatively depending on the involved tract: it could be a simple sigmoidectomy or a proper left hemicolectomy with full mobilization of the splenic flessure. In any case, the resection was carried down to the level of the rectum at or just below the peritoneal reflection. A colon–rectal anastomosis was performed with a circular stapler (typically a CEEA 31) using end-to-end technique. The decision to open a diverting stoma was made intraoperatively, depending on the disease severity (Hinchey stage 3 or stage 4) and on the technical difficulty in creating the anastomosis.
In the laparoscopy-assisted colonic resection, open laparoscopy through a paraumbilical incision was used to obtain pneumoperitoneum. Typically, a 10-mm port was placed on the right midclavicular line in the higher abdominal quadrant, a 10-mm port was placed slightly more medially on the supra-pubic line in the lower abdominal quadrant, and a 5-mm port was always placed in the left iliac fossa in order to provide adequate traction when mobilizing the left colonic flexure and the sigmoid colon. Just as in the open procedure, the resection was carried down to the level of the rectum at or just below the peritoneal reflection. The mobilized bowel was then exteriorized through a small median peri-umbilical or Pfannestiel incision, typically smaller than 6 cm, and a standard open technique was used for the resection and the anastomosis of the colon.
Conservative Therapy
Medical therapy protocol in case of DD included fasting and parenteral nutrition while abdominal pain persisted associated to antibiotic therapy for 10 days (ciprofloxacin 500 mg twice daily and metronidazole 500 mg three times daily). US- or CT-guided percutaneous drainage was attempted in case of isolated abdominal abscess, and endoscopic hemostasis was carried out when there was rectal bleeding. All patients were discharged with a diet enriched with fibers, 1.5 l of liquid per day, and paramomicin cycle (one spoon tris in die for a week per month).
Statistical Analysis
Data are presented as median and range or number of patients affected (%). Alpha (the probability of committing a type I error) was set at 0.05 (two-tailed), beta (the probability of committing a type II error) at 0.20, and E/SD (standardized effect size, expected effect size divided by standard deviation) at 0.50; the sample size of the study and control groups was calculated to be at least of 63 patients for two-tailed t test. Continuous data were compared with Kruskal–Wallis analysis of variance (ANOVA), in case of multiple comparisons, or with Mann–Whitney U rank test when appropriate. Fisher exact test was used to compare dichotomous variables. Correlations between Italian CGQL and possible HRQL predictors were explored with the Spearman correlation rank test. All the variables that resulted to be significant at the univariate analysis were included in a multiple regression model in order to identify the independent predictor of long-term HRQL.
Admission-free and reoperation-free survival were calculated using the Kaplan–Meier method with follow-up time (time at risk) beginning at initial discharge from hospital and ending at the hospital admission for DD, at reoperation for DD, or at last available follow-up, whichever came first. Data were considered complete when hospital admission for DD or reoperation for DD, respectively, occurred. Cumulative recurrence rates were compared using the log rank test according to dichotomous or dichotomized variables. All the variables that resulted to be significant at the univariate analysis were included in a multiple variable Cox proportional hazards model. A level of p < 0.05 was considered significant.
Results
One hundred forty-nine patients were admitted to our surgical department with a diagnosis of DD from January 1998 to December 2005. After a median follow-up of 47 (3–102) months from hospital admission, 71 of them could be contacted, accepted to have an interview, and thus, were eligible for the study. The characteristics of the patients enrolled in the study are shown in Table 1.
The 78 patients who did not participate to the study were 38 men and 40 women, their median age was 67 (35–93) years, and 25 of them had surgery for DD. Twenty-five patients were admitted for Hinchey stage 0 DD, 30 for Hinchey stage 1 DD, 14 for Hinchey stage 2 DD, six for Hinchey stage 3 DD, and three for Hinchey stage 4 DD. The patients who did not participate were not significantly different from those who were actually enrolled in the study.
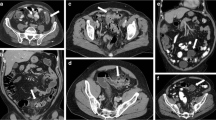
In the study group, a colonic resection was performed in 25 patients (10 left hemicolectomy and 15 sigmoidectomy), while the remaining 46 were treated with medical therapy (fasting, parenteral nutrition, and antibiotic therapy). Therapy adopted in the two groups is shown in Table 2. The disease severity was different in the two groups: Hinchey stage 3 and 4 patients were all operated on, while patients with no signs of diverticular perforation (Hinchey stage 0) were all treated with medical therapy. Three patients with Hinchey stage 2 DD were treated conservatively with percutaneous drainage of the abdominal abscess and antibiotic therapy, while 13 of them underwent colonic resection. The Hinchey stage 1 class was equally distributed in the two groups: nine patients had colonic resection, and 17 were treated with medical therapy. Therapeutical choice according to DD severity is shown in Fig. 1.
As shown in Figs. 2 and 3, no significant difference was evidenced in the rate and in the timing of readmission and surgical procedures for DD in the two groups (p = 0.957 and p = 0.372, respectively) as well as in the total number of re-admission for DD [0 (0–3) vs 0 (0–2), p = 0.576]. There was no significant difference, likewise, in hospital admission rate as well as in the total number of re-admission for DD [0 (0–2) vs 0 (0–1), p = 0.235] in the 26 patients with Hinchey stage 1 DD between those who had been operated on and those who had been treated conservatively (p = 0.609). Among all the possible predictors, only the extension of surgery was associated to readmission for DD: patients who had a simple sigmoidectomy had a cumulative readmission-free survival rate higher than those who had left hemicolectomy (after 5 years follow-up, 93% vs 54%, p = 0.047). None of the other possible predictors seemed to be associated to reoperation.
As shown in Table 3, no significant difference was observed in terms of symptoms rate at follow-up between the patients treated with colonic resection and those who had medical therapy.
Quality of life analysis is outlined in Table 4. CGQL total score as well as the two items current quality of life and current energy level responses were similar in the two groups of patients and in the group of healthy subjects. Only the scoring on the current quality of health was significantly worse in patients who had undergone colonic resection (p = 0.02). Similarly, in the Hinchey 1 sub-group, no significant difference in CGQL score (p = 0.948), current quality of health (p = 0.383), current quality of life (p = 0.583) and current energy level (p = 0.897) was observed in patients who had been operated on and those who had been treated conservatively. Patients’ characteristics and long-term outcome of Hinchey I patients are summarized in Table 5.
Constipation at admission (R = −0.35, p = 0.004), Hinchey severity class (R = −0.24, p = 0.050), and antibiotic therapy (R = 0.25, p = 0.047) were significantly correlated with the CGQL score at univariate analysis, although none of these were confirmed independent predictors of quality of life at the multiple regression analysis.
Discussion
DD of the colon affects approximately one third of the population over 60 years of age in the Western world with a consequent impact on public health organization and costs,1,2 and perforation associated with diverticular disease is the main complication.3 In these cases, colonic resection is standard practice, but the management of episodes of uncomplicated diverticulitis is still unclear. Medical therapy is usually successful,1,5 but the risk of emergency surgery,6 often involving colostomy, must be considered.7–9 Elective colectomy is often recommended instead of conservative management to minimize these risks. Furthermore, the enthusiasm of surgeons for laparoscopic colonic surgery and its lighter impact perceived by the patients expanded the indications. Consequently, most of patients who have a laparoscopic colonic resection for diverticular disease have uncomplicated diverticulitis.14 The biggest controversy today remains the management of recurrent and symptomatic chronic diverticular disease.20 Therefore, the aim of the present study was to evaluate the impact of colonic resection for DD on the natural history and on the long-term quality of life of these patients.
Some authors reported that after one episode of DD treated conservatively, up to a third of patients develop recurrent symptoms, while recurrence rates after colonic resection for DD were between 1% and 10%.21,22 On the contrary, in the present series, the rate and timing and total number of re-admissions for DD of the patients treated with conservative therapy and those who had a colonic resection was similar. This similarity in ratings was also observed in the group of patients with Hinchey stage 1 DD. This could be due, in part, to the lack of uniformity of definitions of episodes of diverticulitis in the different series.20 In fact, many studies have reported that these patients are often affected with concomitant irritable bowel syndrome or that their recurrent symptoms in the immediate postoperative period may be related to anastomotic complications.23 In the present study, episodes of diverticulitis were defined as left iliac fossa pain associated to fever or rise of serum inflammatory markers (white blood cell count, C-reactive protein or erythrocyte sedimentation rate).
Although two of our patients treated with medical therapy later required surgery, none undergoing colonic resection needed any further resection, and the rate and timing of surgical procedures was not significantly different in the two groups. Even if this result could be due to the small sample size of the groups studied, it nonetheless reflects the seemingly low risk of surgery in these patients. Paradoxically, patients with a simple sigmoidectomy had a lower cumulative re-admission rate than those who had left hemicolectomy, suggesting that resection is probably efficacious because the sigmoid high pressure zone is ablated and not because the large bowel affected by the DD has been removed.
Quality of life scores obtained in the two groups of patients and in healthy subjects were similar as were the responses to the current quality of life and current energy level. There was, likewise, no significant difference in the Hinchey stage 1 patients with regards to the CGQL total score or response to the single questions. These data seem to reflect the similarity of symptom rates at follow-up between the patients treated with colonic resection and those who received medical therapy. In fact, at follow-up, the frequency of abdominal pain, constipation, diarrhea, rectal bleeding, and bloating were similar in the two groups. Nevertheless, quality of life of these patients was not different from that of healthy subjects, and it is known that DD negatively affects quality of life,24 so an improvement of sorts might be hypothesized. It has also been reported that cyclic treatment with antibiotics or anti-inflammatory drugs relieves symptoms and improves HRQL in patients with DD.24 The effect of surgery on quality of life could indeed be equivalent, and the low discriminative ability of generic quality of life questionnaires in general and the CGQL in particular may have influenced the results being reported.19 This questionnaire was chosen for this study because it is easy to use during a telephone interview that could be more affordable for elderly patients than coming to the clinic for a face-to-face interview or self administration of a mailed questionnaire.
Post-operative complications are, in any case, an important consideration, and in effect, current quality of health was significantly worse in the patients who had undergone colonic resection. Constantides et al. had already reported that there is a significant impact on the physical health of elderly subjects and postoperative complications following this procedure.25 The risks related to colostomy should in any case be considered carefully as patients who have undergone this procedure for benign processes have found it difficult to adapt to their new body situation and have reported a worse quality of life.26
The main limit of this observational study is the low number of patients who had surgery for DD at the Hinchey stage 1, and the small sample size of this crucial group might make our findings less conclusive. Therefore, further larger studies with a longer follow-up and more detailed quality of life questionnaires are advisable to investigate the actual impact of surgery on quality of life of these patients.
In conclusion, our results indicate that there are no long-term advantages to colonic resection for DD, and these data seemed to be supported by the analysis of the small group of Hinchey stage 1 patients. Thus, in our opinion, surgical resection should be reserved for patients who present with a complicated DD and not for patients who present a mere abdominal discomfort attributed to DD.
References
Wong WD, Wexner SD, Lowry A et al. Practice parameters for the treatment of sigmoid diverticulitis-supporting documentation: the Standards Task Force. The American Society of Colon and Rectal Surgeons. Dis Colon Rectum 2000;43:290–297. doi:10.1007/BF02258291.
Delvaux M. Diverticular disease of the colon in Europe: epidemiology, impact on citizen health and prevention. Aliment Pharmacol Ther 2003;18(Suppl 3):71–74. doi:10.1046/j.0953-0673.2003.01720.x.
Makela J, Kiviniemi H, Laitinen S. Prevalence of perforated sigmoid diverticulitis is increasing. Dis Colon Rectum 2002;45:955–961. doi:10.1007/s10350-004-6335-5.
Constantinides VA, Heriot A, Remzi F, Darzi A, Senapati A, Fazio VW et al. Operative strategies for diverticular peritonitis: a decision analysis between primary resection and anastomosis versus Hartmann’s procedures. Ann Surg 2007;245(1):94–103. doi:10.1097/01.sla.0000225357.82218.ce.
Brandimarte G, Tursi A. Rifaximin plus mesalazine followed by mesalazine alone is highly effective in obtaining remission of symptomatic uncomplicated diverticular disease. Med Sci Monit 2004;10(5):PI70–PI73.
Parks TG. Natural history of diverticular disease of the colon. A review of 521 cases. BMJ 1969;4:639–642.
Tudor RG, Farmakis N, Keighley MR. National audit of complicated diverticular disease: analysis of index cases. Br J Surg 1994;81:730–732. doi:10.1002/bjs.1800810537.
Elliott TB, Yego S, Irvin TT. Five-year audit of the acute complications of diverticular disease. Br J Surg 1997;84:535–539. doi:10.1002/bjs.1800840428.
Lambert ME, Knox RA, Schofield PF, Hancock BD. Management of the septic complications of diverticular disease. Br J Surg 1986;73:576–579. doi:10.1002/bjs.1800730721.
Kohler L, Sauerland S, Neugebauer E. Diagnosis and treatment of diverticular disease: results of a consensus. Surg Endosc 1999;13:430–436. doi:10.1007/s004649901007.
Freischlag J, Bennion RS, Thompson JE Jr. Complications of diverticular disease of the colon in young people. Dis Colon Rectum 1986;29:639–643. doi:10.1007/BF02560326.
Ambrosetti P, Robert JH, Witzig JA et al. Acute left colonic diverticulitis in young patients. J Am Coll Surg 1994;179:156–160.
Konvolinka CW. Acute diverticulitis under age forty. Am J Surg 1994;167:562–565. doi:10.1016/0002-9610(94)90098-1.
Scheidbach H, Schneider C, Rose J, Konradt J, Gross E, Bärlehner E et al. Laparoscopic approach to treatment of sigmoid diverticulitis: changes in the spectrum of indications and results of a prospective, multicenter study on 1,545 patients. Dis Colon Rectum 2004;47(11):1883–1888. doi:10.1007/s10350-004-0715-8.
Hinchey EJ, Schaal PG, Richards GK. Treatment of perforated diverticular disease of the colon. Adv Surg 1978;12:85–109.
Fazio VW, O’Riordain MG, Lavery IC et al. Long term functional outcome and quality of life after stapled restorative proctocolectomy. Ann Surg 1999;1230:575–586. doi:10.1097/00000658-199910000-00013.
Kiran RP, Delaney CP, Senagore AJ et al. Prospective assessment of Cleveland Global Quality of Life and disease activity in Crohn’s disease. Am J Gastroenterol 2003;98:1783–1789. doi:10.1111/j.1572-0241.2003.07592.x.
Scarpa M, Ruffolo C, D’Incà R et al. Health related quality of life after ileo-colonic resection for Crohn’s disease: long-term results. Inflamm Bowel Dis 2007;13(4):462–469. doi:10.1002/ibd.20080.
Scarpa M, Ruffolo C, Polese L, Martin A, D’Incà R, Sturniolo GC et al. Quality of life after restorative proctocolectomy for ulcerative colitis: different questionnaires lead to different interpretations. Arch Surg 2007;142(2):158–165. doi:10.1001/archsurg.142.2.158.
Frattini J, Longo WE. Diagnosis and treatment of chronic and recurrent diverticulitis. J Clin Gastroenterol 2006;40:S145–S149. doi:10.1097/01.mcg.0000225507.52300.b9.
Janes SS, Meagher A, Frizelle FA. Elective surgery after acute diverticulitis. Br J Surg 2005;92:133–142. doi:10.1002/bjs.4873.
Wolff BG, Frizelle FA. Recurrent diverticulitis following resection. In Welch JP, ed. Diverticular Disease. Management of the difficult case. Baltimore, MD: Williams & Wilkins, 1999, pp 343–351.
Bell AM, Wolff BG. Progression and Recurrence after resection for diverticulitis. Semin Colon Rectal Surg 1990;1:99–102.
Comparato G, Fanigliulo L, Aragona G, Cavestro GM, Cavallaro LG, Leandro G et al. Quality of life in uncomplicated symptomatic diverticular disease: is it another good reason for treatment. Dig Dis 2007;25:252–259. doi:10.1159/000103896.
Constantinides VA, Aydin HN, Tekkis PP, Fazio VW, Heriot AG, Remzi FH. Long-term, health-related, quality of life comparison in patients undergoing single stage vs staged resection for complicated diverticular disease. Colorectal Dis 2006;8:663–671. doi:10.1111/j.1463-1318.2006.00961.x.
Krouse R, Grant M, Ferrell B, Dean G, Nelson R, Chu D. Quality of life outcomes in 599 cancer and non-cancer patients with colostomies. J Surg Res 2007;138:79–87. doi:10.1016/j.jss.2006.04.033.
Acknowledgments
The authors are very grateful to Mrs Linda Moretti for her assistance in preparing the final version of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
Presented as a poster at the Digestive Disease Week, San Diego CA, USA May 19-24, 2008.
Rights and permissions
About this article
Cite this article
Scarpa, M., Pagano, D., Ruffolo, C. et al. Health-Related Quality of Life after Colonic Resection for Diverticular Disease: Long-term Results. J Gastrointest Surg 13, 105–112 (2009). https://doi.org/10.1007/s11605-008-0667-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-008-0667-8