Abstract
Objective
To assess the resectability and the long-term survival in patients of gallbladder cancer with duodenal involvement.
Background
Duodenal infiltration in patients of carcinoma gallbladder is generally regarded as a sign of advanced disease and an indicator of unresectable disease.
Methods
A total of 252 patients of gallbladder cancer (GBC) who underwent surgery over a 5-year period were studied for duodenal involvement. Patients with duodenal infiltration on per-operative assessment were analyzed for resectability, postoperative morbidity, mortality and disease free survival.
Results
Forty-three patients were detected to have duodenal infiltration on per-operative assessment out of which 17 had unresectable disease (39.54%), whereas the remaining 26 patients underwent R0 resection (61.9%). Of these, nine underwent distal gastrectomy with resection of the first part of the duodenum (34.62%), 16 underwent duodenal sleeve resection (61.54%), and in one patient pancreatoduodenectomy (HPD) (3.85%) was performed. With regard to the extent of liver resection, two underwent extended right hepatectomy, whereas the remaining 24 underwent segment IVB and V resection. Bile duct and adjacent viscera were resected when involved. Of the resected patients, eight underwent bile duct excision, seven had colonic resection, and three had vascular resection and reconstruction. The postoperative morbidity and mortality was 15 (34.9%) and three (6.97%), respectively, in the resected group of patients. The overall actual survival in the resected group was a mean of 15.87 months, median of 14 months (range 3 to 56 months).
Conclusion
Duodenal infiltration is neither an indicator of unresectability nor an indication to perform Hepato-pancreatoduodenectomy (HPD). In most of these patients, an oncologically adequate R0 resection can be performed with either a duodenal sleeve resection or distal gastrectomy with resection of the first part of the duodenum.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Gallbladder cancer (GBC) has long been known to have a poor outcome.1,2 It is generally believed that only early stage tumors limited to the mucosa or muscle layer can have a satisfactory outcome with simple cholecystectomy or extended cholecystectomy with lymph node clearance.3,4 Despite great advancement in diagnostic techniques, majority of gall bladder malignancies are diagnosed at advanced stages, when radical surgery is either not feasible or when feasible is noncurative with only a limited increase in survival.5–7 A significant number of these advanced cases include tumors that infiltrate the duodenum. Duodenal infiltration in patients of gall bladder cancer has been regarded as a sign of advanced disease and an indicator of unresectability.8,9 Most of these studies have documented unresectability in these groups of patients and those in whom it has been resectable, the long-term survival has been very poor. However, recently some authors, especially from Japan, have shown improved survival with aggressive resection. These studies from Japan and some also from the west have reported that gall bladder cancer with duodenal infiltration merits an associated pancreatoduodenectomy (PD) to accomplish R0 resection and allow good long-term survival.10–14
We have analyzed our prospectively collected data of gall bladder cancer to assess the resectability in patients with duodenal involvement, the necessity of hepatopancreatoduodenectomy (HPD) in these patients and the long-term survival.
Materials and Methods
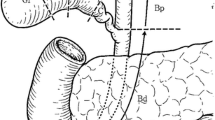
The prospectively collected data of patients undergoing surgery for carcinoma of the gall bladder between January 2000 and December 2004 in the Department of Gastrointestinal Surgery, Gobind Ballabh Pant Hospital, New Delhi, a tertiary care referral and teaching hospital of Northern India, was analyzed. The standard preoperative workup included abdomen ultrasound with Doppler for the assessment of portal vein and hepatic artery involvement and contrast-enhanced computed tomography (CT) of the abdomen. Magnetic Resonance Imaging with Magnetic Resonance Cholangio-pancreatography (MRCP) was obtained in selected patients, particularly those with associated bile duct involvement. All the patients underwent an upper gastrointestinal tract endoscopy (UGIE) to look for any gastroduodenal involvement. UGIE evidence of involvement was defined as external compression, obvious infiltration of tumor into the lumen, or gastric outlet obstruction. Assessment of involvement on UGIE was further categorized into two types: “A” when there was only external compression but no evidence of gastric outlet obstruction (GOO); and “B” when there was obvious infiltration of the tumor into the lumen or gastric outlet obstruction. Endosonography for evaluation of the tumors was not performed in our study. Patients who appeared to be resectable on preoperative imaging underwent surgery with a curative intent, whereas some of the patients considered to have unresectable disease underwent palliative procedure. Those patients with distant metastasis, who otherwise did not require palliation, were not operated upon. Informed consent was taken of all patients in accordance with ethical standards of our institution (ethical standards of the Helsinki Declaration of 1975). Routine staging laparoscopy was introduced in the later part of the study (from September 2002) during which all subsequent patients underwent staging laparoscopy before definitive surgery under the same anesthesia to detect occult distant metastasis. Doubtful lesions were biopsied and sent for frozen section. Laparoscopic ultrasound and extensive mobilization was not included. Patients who were subsequently considered to be resectable or required palliation underwent laparotomy. Patients who proceeded to laparotomy underwent routine sampling of the inter-aortocaval lymph node for frozen section analysis. Wide kocherization of the duodenum and division of the gastrocolic omentum was performed and involvement of the pyloroduodenal area and head of the pancreas was assessed. In patients with a small area of duodenal infiltration where it was expected that there would be no luminal compromise after sleeve resection of the duodenum, we would perform the same. In the presence of more significant duodenal infiltration but no evidence of pancreatic involvement, where luminal compromise was expected after a simple sleeve resection, we would perform a distal gastrectomy with resection of the first part of the duodenum (D1). Bowel continuity in such case would be restored by a gastro-jejunostomy (GJ). We would perform pancreatoduodenectomy (PD) only if there was extensive peripancreatic lymph nodes, which could not be otherwise cleared, or direct involvement of the head of pancreas.
Resected specimens were analyzed histopathologically. Pathological staging was done according to the 6th edition of the AJCC TNM staging handbook14 and the long-term survival of the patients who underwent R0 resection was analyzed. Resectabilty of the tumors with regards to the preoperative imaging was analyzed.
Statistical analysis has been carried out with the help of statistical software SPSS 10.0, copyright© SPSS, Inc, USA, 1989–1999. Survival was calculated by Kaplan–Meier method and statistical significance by Log rank test and Fisher’s exact test.
Results
The total number of patients of GBC operated during this period was 252. The male-to-female ratio was 1:3. The mean age of our patients was 49.8 years (20 to 80 years). On preoperative workup, 65 patients (25.79%) were suspected to have duodenal infiltration on cross-sectional imaging (CECT and/or MRI). Out of these 19 patients were found to have gastroduodenal involvement on endoscopy (Type B) in the form of gastric outlet obstruction or obvious infiltration (7.54%, 19 of 252; 29.23%, 19 of 65). Only external compression on endoscopy (Type A) was seen in 21 (8.33%, 21 of 252; 32.3%, 21 of 65) of our patients.
On per-operative assessment, 43 out of the 252 (17.06%) were found to have duodenal involvement. Out of the 65 patients with duodenal involvement on CT or MR, 35 actually had duodenal involvement out of which 18 were resectable (51.42%). All (100%) of the 19 patients who had type B involvement on endoscopy had actual involvement, and out of these only two (10.53%) were resectable. Out of the 21 patients with type A involvement, six had actual involvement of the duodenum, whereas 15 did not. Of these six patients, four were resectable, whereas two were unresectable. There were eight patients who had duodenal involvement, which was neither detected on imaging nor on endoscopy, and all eight of them were resectable (Table 1).
The sensitivity and specificity of CT and MRI for detecting duodenal involvement was 81.4% and 85.64%, whereas for UGIE it was 75.76% and 93.15% (Table 2).
The mean age in this group of patients with duodenal involvement (n = 43) was 50.16 years (range 22–70 years). The male-to-female ratio was 1:3. Out of the 43 patients, 17 (39.54%) were unresectable on account of locally unresectable disease in 10 patients, positive inter-aortocaval lymph node in three, noncontiguous liver metastasis in two, and peritoneal metastasis in two patients. Out of these 17 patients, five were considered to have unresectable disease on preoperative imaging and hence were taken up for surgery with palliative intent. The rest 26 (61.9%) patients were resectable and underwent R0 resection. Among the patients who underwent resection, segment IVB and V resection was performed in 24, whereas two patients underwent extended right hepatectomy. All 26 patients underwent standard lymph node dissection. Common bile duct excision was performed in 15 patients, in eight on account of bile duct involvement by the tumor, in five for adequate lymph node clearance, in one for positive cystic duct margin, and in one on account of associated choledochal cyst. Reconstruction was done in the form of roux-en-Y hepaticojejunostomy. Segmental colonic resection was performed in seven and vascular resection and reconstruction in three patients. With regard to the duodenal resection in 26 patients, 16 underwent sleeve resection of the duodenum, nine underwent distal gastrectomy and excision of the first part of the duodenum (DG & D1), whereas only one patient underwent PD (Table 3). Four patients underwent completion radical cholecystectomy for incidental GBC, two of which underwent duodenal sleeve resection, whereas the other two underwent DG & D1 resection.
Among the unresectable group, only gastrojejunostomy(GJ) was performed in 10, gastrojejunostomy with segment III bypass in six, and feeding jejunostomy (FJ) in one. Overall, 18 out of 43 patients (41.86%) had postoperative complications. In the resected Group, 15 out of 26 patients had complications (57.69%), whereas in the palliative group, three out of 17 (17.65%) had complications. The details of the morbidity are given in Table 4 Overall mortality was 6.97% (three out of 43 patients). All the deaths were in the resected group—three out of 26patients (11.54%). The cause of death was anastomotic leak and sepsis in two patients (one from RYHJ site and the other from the duodenal stump) and postoperative bleed in one. The mean hospital stay of our patients was 14.38 days, median of 12 days, and range of 9 to 97 days.
Twenty-four patients resected had evidence of histopathologic involvement of the duodenum with varying depths of invasion. Involvement of only the serosa was seen in 10 (one patient of incidental GBC had few atypical cells in the serosa), infiltration up to the muscularis in seven, up to the submucosa in three, and up to the mucosa in four. Whereas, the remaining two patients did not have any evidence of tumor in the specimen (both these patients had incidental GBC). Stagewise distribution of the disease of the 26 resected patients showed four patients in stage IIA, three in stage IIB, 18 in III, and one in IV. Of the 23 patients who were discharged, we have a complete follow up available of 17 patients.
The overall actual survival in the 23 patients was a mean of 15.87 months, median of 14 months, range of 3 to 56 months and a 1- and 3-year actual survival of 60.87% and 13.04%, respectively. The 1, 2, and 3 years overall actuarial survival in our patients was 76.64%, 76.64%, and 51.09%, respectively.
Survival calculated from the Kaplan–Meier survival curves for all the patients (n = 23) (Figs. 1 and 2) was a mean of 40 months (95% Confidence Interval [CI] of 29 and 52). The same for stage IIA disease was a mean of 31 months (95% CI of 24 and 38) and median of 36 months (95% CI of 2 and 70). By log-rank test survival when compared with different stages of disease survival was statistically significant (p value 0.0364).
Discussion
Duodenal involvement was seen in 17.06% (n = 43) of GBC patients who underwent surgery at our institution. Duodenal infiltration was detected in 35 out of the 43 patients (81.4%) on preoperative imaging, whereas in eight patients it was neither detected on imaging nor on endoscopy. All these eight patients, were found to be resectable. On the other hand, out of the 65 patients who had suspected involvement on imaging, only 35 (53.85%) had actual involvement. Out of these 35 patients, 18 (51.42%) were resectable. In comparison, out of the 19 patients who had type B involvement on endoscopy, all 19 had actual involvement, two of which (10.53%) were resectable. On the contrary, patients with type A involvement on UGIE had a lower incidence of actual infiltration (28.57%) and a higher resectability (66.67%). These data would imply patients who were incidentally detected to have duodenal infiltration had higher probability of having a resectable disease. Patients with limited involvement on endoscopy (external compression alone) were more likely to have resectable diseases compared to patients with more extensive involvement in form of mucosal involvement or complete duodenal obstruction.
It is apparent that although these investigations help in preoperative detection of duodenal infiltration and to some extent the resectability, the overall management does not change.
Imaging is more sensitive, whereas endoscopy has high specificity and a high positive predictive value. With regard to the type of involvement on UGIE, type B is more sensitive and specific and has greater positive predictive value, whereas type A has greater negative predictive value. Simple external compression is a poor positive predictor of duodenal involvement (28.57%). This would imply that in several patients, because of the anatomical proximity, a large mass in the gall bladder could create an impression on the duodenum without actual tumor infiltration. To this end, endosonography may be more reliable. However, although there are studies that have dealt with endosonography in the assessment of the T-stage of GBC, but none has assessed duodenal infiltration with this modality.16,17
All the patients in our series underwent a R0 resection. The majority of our resections were segment IVB & V wedge resection, only two underwent extended right hepatectomy. With regard to the resection performed on the duodenum most underwent either duodenal sleeve resection or distal gastrectomy and D1 resection, only one patient underwent pancreatodudenectomy.
The stage-wise distribution of our patients has shown that most of our patients were in stage III (Table 5). The best survival was seen in patients with stage IIA disease. Stage of disease was a significant factor in predicting survival (p value 0.0364).
Some of the older studies that have dealt with this entity have essentially concluded that gastric outlet obstruction in gall bladder cancer is an advanced disease and can only be palliated.18,19 These studies have not specifically analyzed the spectrum of duodenal infiltration, which can occur without gastric outlet obstruction being present. Our study reveals that in the absence of symptomatic duodenal infiltration the resectability is high and that although patients with gastric outlet obstruction have a high chance of unresectability, it should not be used as the sole criteria for unresectability. Most studies do not analyze the involvement of the duodenum in gall bladder cancer. Most Japanese literature recommends performing HPD for involvement of the duodenum, pancreas, and lymph node clearance. Majority of these studies have not clearly defined the incidence of duodenal infiltration and comparisons with our study cannot be made.13–15,20,21 Kondo et al., have shown that radical surgery in GBC patients with duodenal involvement had a postoperative mortality of 28%, which was higher than those without duodenal infiltration but was not statistically significant. This higher mortality rate as compared to our study (11.54%) could be caused by the fact they had performed extended right hepatectomy, HPD with or without portal vein resection in a significant number of their patients. Among their patients with duodenal involvement, the 3-year survival was 14%, which is similar to the 13.04% in our study.10 Nakamura et al, in their patients of advanced GBC infiltrating the duodenum and pancreas (seven patients) who had undergone HPD, reported that the 1- and 2-year survival rates were 57% and 28.6%, respectively, with a median survival time of 12 months.22 Nimura et al. in their 14 patients of advanced GBC, who underwent HPD, reported a median survival of 12.4 months and a 2-year survival rate of 20.8%.23 Nagakawa et al., in a collective review of Japanese literature of HPD being performed in 355 GBC patients with surrounding organ infiltration over a period of 10 years, reported a 5-year survival of more than 10%.24
The long-term survival advantage of this policy has been debated. In fact, some studies have shown that the overall long-term survival is limited, with only very limited survival advantage seen in patients with positive lymph nodes but no obvious hepatoduodenal infiltration (21). There are, however, other studies that have shown that resection of such advanced GBC leads to significant increase in survival and a better quality of life (20). Thus, in view of the current literature and our results, we believe that minor duodenal infiltration with no luminal compromise can be resected with sleeve resection, whereas advanced involvement of a significant portion of the circumference with the possibility of luminal compromise requires distal gastrectomy and excision of the first part of the duodenum, and pancreatoduodenectomy is only reserved for more extensive involvement. We do not perform HPD unless there are extensive peripancreatic lymph nodes, which cannot be otherwise cleared, tumor extension into the head of pancreas or advanced duodenal infiltration where pancreas preserving duodenectomy is not possible.
Conclusion
Duodenal infiltration in gall bladder cancer does not preclude resection. It should not be taken as sole indicator of performing HPD. R0 resection can be achieved with limited surgical procedure without resorting to HPD in most cases, and survival depends on the overall stage of the disease.
References
Chattopadhyay TK, Kumar A, Kapoor VK, Sharma LK, Kapur MM, Kapur BM, Dhawan IK. Carcinoma of the gall bladder—can we do anything? Postgrad Med J 1988;64(754):593–595.
Hawkins WG, DeMatteo RP, Jarnagin WR, Ben-Porat L, Blumgart LH, Fong Y. Jaundice predicts advanced disease and early mortality in patients with gallbladder cancer. Ann Surg Oncol 2004 Mar;11(3):310–315.
Ouchi K, Suzuki M, Tominaga T, Saijo S, Matsuno S. Survival after surgery for cancer of the gallbladder. Br J Surg 1994 Nov;81(11):1655–1657.
Frezza EE, Mezghebe H. Galbladder carcinoma: a 28-year experience. Int Surg 1997;82:295–300.
Okamoto A, Tsuruta K, Ishiwata J, Isawa T, Kamisawa T, Tanaka Y. Treatment of T3 and T4 carcinomas of the gallbladder. Int Surg 1996;81(2):130–135.
Ruckert JC, Ruckert RI, Gellert K, Hecker K, Muller JM. Surgery for carcinoma of the gallbladder. Hepatogastroenterology;43(9):527–533.
Benoist S, Panis Y, Fagniez PL. Long-term results after curative resection for carcinoma of the gallbladder. French University Association for Surgical Research. Am J Surg 1998;175(2):118–122.
Cubertafond P, Gainant A, Cucchiaro G. Surgical treatment of 724 carcinomas of the gallbladder. Results of the French Surgical Association Survey. Ann Surg 1994;219(3):275–280.
Wilkinson DS. Carcinoma of the gall-bladder: An experience and review of the literature. Aust N Z J Surg 1995;65(10):724–727. Review.
Kondo S, Nimura Y, Kamiya J, Nagino M, Kanai M, Uesaka K, Yuasa N, Sano T, Hayakawa N. Factors influencing postoperative hospital mortality and long-term survival after radical resection for stage IV gallbladder carcinoma. World J Surg 2003;27(3):272–277. Epub 2003 Feb 27.
Dixon E, Vollmer CM Jr, Sahajpal A, Cattral M, Grant D, Doig C, Hemming A, Taylor B, Langer B, Greig P, Gallinger S. An aggressive surgical approach leads to improved survival in patients with gallbladder cancer: a 12-year study at a North American Center. Ann Surg 2005;241(3):385–394.
Greene FL. TNM staging for malignancies of the digestive tract: 2003 changes and beyond. Semin Surg Oncol 2003;21(1):23–29. Review.
Miyazaki M, Itoh H, Ambiru S, Shimizu H, Togawa A, Gohchi E, Nakajima N, Suwa T. Radical surgery for advanced gallbladder carcinoma. Br J Surg 1996;83(4):478–481.
Todoroki T, Takahashi H, Koike N, Kawamoto T, Kondo T, Yoshida S, Kashiwagi H, Otsuka M, Fukao K, Saida Y. Outcomes of aggressive treatment of stage IV gallbladder cancer and predictors of survival. Hepatogastroenterology 1999;46(28):2114–2121.
Nakamura S, Suzuki S, Konno H, Baba S, Baba S. Outcome of extensive surgery for TNM stage IV carcinoma of the gallbladder. Hepatogastroenterology 1999;46(28):2138–2143.
Fujita N, Noda Y, Kobayashi G, Kimura K, Yago A. Diagnosis of the depth of invasion of gallbladder carcinoma by EUS. Gastrointest Endosc 1999;50(5):659–663.
Inui K, Nakazawa S. Diagnosis of depth of invasion of gallbladder carcinoma with endosonography. Nippon Geka Gakkai Zasshi 1998;99(10):696–699.
Chaudhary A, Dhar P, Sachdev A, Agarwal A. Gastric outlet obstruction in carcinoma gall bladder. Indian J Gastroenterol 1999;18(3):101–103.
Singh B, Kapoor VK, Sikora SS, Kalawat TC, Das BK, Kaushik SP. Malignant gastroparesis and outlet obstruction in carcinoma gall bladder. Trop Gastroenterol 1998;19(1):37–39.
Nakamura S, Nishiyama R, Yokoi Y, Serizawa A, Nishiwaki Y, Konno H, Baba S, Muro H. Hepatopancreatoduodenectomy for advanced gallbladder carcinoma. Arch Surg 1994;129(6):625–629.
Yoshikawa T, Ohta T, Araida T, Azuma T, Takasaki K. Indications for and operative outcome of hepato-pancreatoduodenectomy in the treatment of carcinoma of the gallbladder. Nippon Geka Gakkai Zasshi 1998;99(10):717–721.
Nakamura S, Nishiyama R, Yokoi Y, Serizawa A, Nishiwaki Y, Konno H, Baba S, Muro H. Hepatopancreatoduodenectomy for advanced gallbladder carcinoma. Arch Surg 1994;129(6):625–629.
Nimura Y, Hayakawa N, Kamiya J, Maeda S, Kondo S, Yasui A, Shionoya S. Hepatopancreatoduodenectomy for advanced carcinoma of the biliary tract. Hepatogastroenterology 1991;38(2):170–175.
Nagakawa T, Kayahara M. Indication for and problems of hepatopancreatoduodenectomy for carcinoma of the biliary tract based on the statistical registry in Japan. Nippon Geka Gakkai Zasshi 2001;102(2):199–202.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Agarwal, A.K., Mandal, S., Singh, S. et al. Gallbladder Cancer with Duodenal Infiltration: Is it still resectable?. J Gastrointest Surg 11, 1722–1727 (2007). https://doi.org/10.1007/s11605-007-0320-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-007-0320-y