Abstract
Undifferentiated embryonal sarcoma is the third most common malignant tumor of the liver in children, accounting for 13% of hepatic malignancies in this age group. It has been considered an aggressive neoplasm with very poor prognosis until the late 1980s, when long-term survivors were reported after multiagent chemotherapy followed by resection. We, herein, report two pediatric cases of undifferentiated embryonal sarcoma treated successfully with surgical resection after neoadjuvant chemotherapy based on therapy used in childhood soft tissue sarcomas and in childhood hepatic malignancies. The first patient also had a concurrent cerebellar tumor (pilocytic astrocytoma), for which he first underwent craniotomy and resection, delaying the liver tumor resection by 10 weeks. They are alive and tumor free at 48 months (case no. 1) and 18 months (case no. 2) following neoadjuvant chemotherapy and liver resection.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Undifferentiated embryonal sarcoma (UES), first described by Stocker and Ishak in 1978, is the third most common malignant tumor of the liver in children, accounting for about 13% of hepatic malignancies1,2. It is most commonly seen in children between 6 and 10 years of age, and about 88% occur in children less than 15 years of age. The tumor is located in the right lobe of the liver in the majority of the patients, and it rarely involves both lobes. The main presenting symptoms are typically an abdominal mass and right upper quadrant or epigastric pain of few weeks or months duration. Complaints such as nausea, anorexia, intermittent fever or headache may also be present. Children have usually been otherwise healthy before diagnosis.
This tumor was considered an aggressive neoplasm with very poor prognosis3 until the late 1980s, when long-term survivors were reported following multiagent chemotherapy before liver resection4,5. Complete surgical resection with neoadjuvant chemotherapy offers the best long-term results and possibility of cure3,6–8.
We herein report two pediatric cases of UES successfully treated with surgical resection and neoadjuvant chemotherapy, including a unique case of UES of the liver associated with pilocytic astrocytoma of the cerebellum.
Case 1
This 13-year-old previously healthy Caucasian male developed intermittent headache, high fever, sore throat, cough and rhinorrhea 3 months before presentation. A large epigastric nontender mass was found on physical examination. An extensive oncologic work-up revealed a large mass (20 × 14 cm) occupying the majority of the right lobe of the liver, with mild displacement of the inferior vena cava and the right kidney. A 2.9-cm tumor was also noted in the posterior cranial fossa at the level of the fourth ventricle. Resection of the cerebellar mass demonstrated pilocytic astrocytoma, but was complicated by intraventricular hemorrhage and subsequent hydrocephalus, treated with frontal ventriculostomy. His postoperative course was complicated by deep coma and respirator dependency for several weeks. After 10 weeks of slow postoperative improvement, he underwent a successful right hepatic trisegmentectomy. A histopathologic examination demonstrated a large undifferentiated embryonal sarcoma of the liver (3 kg, 25 cm in diameter), with tumor-free surgical margins. He received a total of six cycles of chemotherapy, all postoperatively, alternating a combination of cisplatin and adriamycin with vincristine, ifosfamide, and etoposide (VIE). Computed tomography (CT) scans of the abdomen and pelvis, 3 and 6 months after surgical resection, showed no evidence of recurrent liver tumor and showed almost complete regeneration of the right lobe of the liver. The child continues his neurologic rehabilitation, but is currently tumor-free, 48 months after surgical resection and neoadjuvant chemotherapy.
Case 2
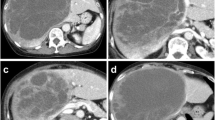
This 11-year old boy developed fatigue, decreased appetite, and weight loss. His work-up revealed anemia and a large liver mass (12 × 8 cm) localized in the anterior segment of the right lobe (segments 5 and 8) and the medial segment of the left lobe of the liver (segment 4B). He underwent a needle biopsy of the tumor, which showed features typical of undifferentiated embryonal sarcoma. His metastatic work-up was negative. He underwent four courses of neoadjuvant chemotherapy, alternating cycles of cyclophosphamide, mesna, vincristine, and actinomycin, with cycles of ifosfamide and VP-16. He responded very well, and his liver mass decreased in size by approximately 40%. Two weeks after chemotherapy, he underwent extended right lobectomy without complications. The surgical specimen revealed minimal residual viable tumor (less than 1%) with significant tumor necrosis and tumor-free surgical margins. He received two additional courses of chemotherapy after liver resection without complications. He is tumor free and doing well 18 months after surgical resection and neoadjuvant chemotherapy.
Discussion
UES is the third most common malignant tumor of the liver in children, after hepatoblastoma and hepatocellular carcinoma. It most commonly occurs between 6 and 10 years of age, in contrast to hepatoblastoma, which is most commonly seen in children under 5 years of age, and hepatocellular carcinoma which is more frequent in patients more than 10 years old. UES is rare in adults and is slightly more frequent in boys9. The tumor usually presents as a large abdominal mass, with or without pain or fever, as in our cases. The majority of the reported cases have not had liver function abnormalities despite massive tumor size.
Useful imaging studies include initial ultrasonography with Doppler examination, followed by CT or magnetic resonance imaging (MRI) to better characterize the tumor and assist in surgical planning. Tumor markers are typically not present in the serum of these patients. In one adult case, CA-125 was found elevated in the tumor itself10.
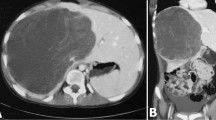
These tumors are typically large and difficult to resect (Fig. 1), but distant metastasis is rare. The tumor rarely involves both lobes, but this was not the case in our experience. The characteristic gross appearance is that of a large intraparenchymal heterogeneous mass with solid and cystic areas, the latter often containing necrotic material and hemorrhage (Fig. 2). The tumor has a variable but distinctively sarcomatous appearance under the microscope, with the tumor cells showing variable morphology, but typically spindle-shaped or pleomorphic (Fig. 3), and often with relatively frequent tumor giant cells. Immunohistochemistry typically shows divergent staining, including variable expression of histiocytic, muscle and epithelial markers, suggesting origin from primitive stem cells.
Microscopic appearance typical of undifferentiated embryonal sarcoma, with nondescript malignant spindled stromal cells and occasional intermixed large pleomorphic tumor giant cells. The tumor lacks any evidence of more specific differentiation as seen in the other more common malignant tumors of the pediatric liver, namely, muscle differentiation typical of biliary rhabdomyosarcoma or immature hepatocytes typical of hepatoblastoma. (hematoxylin–eosin stain, case no. 1).
One of our cases appears to be unique by virtue of its association with a low-grade cerebellar pilocytic astrocytoma. It raises the question as to whether this patient may have had some type of unrecognized underlying genetic disorder, which might have predisposed the development of these tumors. However, clinically, there was no recognized genetic or syndromic abnormality.
The prognosis of UES has been very poor until recently when aggressive chemotherapy similar to that used for rhabdomyosarcoma has come into use preoperatively, which more often permits complete tumor resection of initially unresectable tumors. Bisogno et al. reported 12 of 17 patients who were alive after a 20-year follow-up11. The use of a similar combination chemotherapy in our patients allowed us to achieve complete resection and tumor-free survival to date. Radiotherapy has not been considered helpful in patients with UES so far.
In conclusion, we report two pediatric cases of UES treated with neoadjuvant chemotherapy and liver resection that are tumor-free at 48 months (case no. 1) and 18 months (case no. 2) following resection. We also describe a unique case of UES associated with a low-grade pilocytic astrocytoma of the cerebellum.
References
Weinberg AG, Finegold MJ. Primary hepatic tumors of childhood. Hum Pathol 1983;14(6):512.
Stocker JT, Ishak KG. Undifferentiated (embryonal) sarcoma of the liver: report of 31 cases. Cancer 1978;42(1):336.
Horowitz ME, Etcubanas E, Webber BL, et al. Hepatic undifferentiated (embryonal) sarcoma and rhabdomyosarcoma in children. Results of therapy. Cancer 1987;59(3):396.
Babin-Boilletot A, Flamant F, Terrier-Lacombe MJ, et al. Primitive malignant nonepithelial hepatic tumors in children. Med Pediatr Oncol 1993;21(9):634.
Kadomatsu K, Nakagawara A, Zaizen Y, et al. Undifferentiated (embryonal) sarcoma of the liver: report of three cases. Surg Today 1992;22(5):451.
Urban CE, Mache CJ, Schwinger W, et al. Undifferentiated (embryonal) sarcoma of the liver in childhood. Successful combined-modality therapy in four patients. Cancer 1993;72(8):2511.
Smithson WA, Telander RL, Carney JA. Mesenchymoma of the liver in childhood: five-year survival after combined-modality treatment. J Pediatr Surg 1982;17(1):70.
Ware R, Friedman HS, Filston HC, et al. Childhood hepatic mesenchymoma: successful treatment with surgery and multiple-agent chemotherapy. Med Pediatr Oncol 1988;16(1):62.
Leuschner I, Schmidt D, Harms D. Undifferentiated sarcoma of the liver in childhood: morphology, flow cytometry, and literature review. Hum Pathol 1990;21(1):68.
Houry S, Gharbi L, Huguier M, Callard P, Andre T. Undifferentiated embryonal sarcoma in the liver of adults. Presse Méd 1998;27(11):518.
Bisogno G, Pilz T, Perilongo G, et al. Undifferentiated sarcoma of the liver in childhood: a curable disease. Cancer 2002;94(1):252.
Acknowledgement
This work was supported by a grant from the Loma Linda Transplantation Institute, Loma Linda, CA.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Baron, P.W., Majlessipour, F., Bedros, A.A. et al. Undifferentiated Embryonal Sarcoma of the Liver Successfully Treated With Chemotherapy and Liver Resection. J Gastrointest Surg 11, 73–75 (2007). https://doi.org/10.1007/s11605-006-0044-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-006-0044-4