Abstract
Background
The purpose of this study was to evaluate long-term outcomes of first metacarpal extension osteotomy for early trapeziometacarpal arthritis.
Methods
We retrospectively reviewed 13 patients who underwent first metacarpal extension osteotomy at our institution between 1996 and 2005 and obtained subjective and objective outcome data.
Results
Mean follow-up was 9.9 years (range 6 to 14 years). Ten of the 13 patients (77 %) were either satisfied or very satisfied with their results. Mean pain level was 2.00 on a scale of 1 (nonexistent) to 7 (unbearable). Mean QuickDASH score was 24.17, with a median score of 9.09. Mean pinch strength was 13.1 lbs compared to 12.8 lbs in the nonoperative extremity. Mean radial abduction of the thumb was 45.5° which was equal to the nonoperative extremity. Of the eight patients who agreed to repeat radiographs, five had no progression of degenerative changes compared to pre-op radiographs.
Conclusions
Based on subjective and objective follow-up data, first metacarpal extension osteotomy can provide good long-term results in terms of patient satisfaction, pain relief, and upper extremity function. It is a reasonable alternative to ligament reconstruction in patients with early-stage trapeziometacarpal arthritis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Thumb carpometacarpal (CMC) arthritis is the second most common form of primary osteoarthritis in the hand, after distal interphalangeal (DIP) joint arthritis [19]. In early anatomic studies, Eaton and Littler identified the anterior oblique “beak” ligament as a primary stabilizer of the trapeziometacarpal (TM) joint [3]. The beak ligament, originating from the palmar aspect of the trapezium and attaching to the palmar beak of the thumb metacarpal, serves as a restraint against dorsal translation of the metacarpal on the trapezium. Pellegrini and colleagues’ studies in the early 1990s demonstrated that degeneration of the beak ligament, also known as the palmar oblique ligament (POL), can lead to pathologic laxity, subluxation of the first metacarpal on the trapezium, abnormal joint loading, and eventually degenerative arthritis, typically starting in the palmar region of the joint [12–14, 16]. Because of the central role of the POL in TM joint stability, reconstruction of the POL has been a traditional recommendation for all stages of TM arthritis, including early-stage disease [2, 4, 19].
First metacarpal extension osteotomy, described by Wilson [20], is another option for patients with less advanced disease and has the advantage of preserving options for future joint reconstruction in case of disease progression. Pellegrini’s biomechanical analysis of thumb metacarpal osteotomy demonstrated a dorsal load transfer during pinch [15]. He showed that a 30° closing wedge extension osteotomy can unload the palmar aspect of the TM joint, which is typically the region first affected by degenerative changes. Forces are thus shifted to the intact dorsal articular cartilage, which has the theoretical advantage of decreasing arthritic pain and slowing progression of arthritis. Short-term follow-up studies have shown promising results [5, 10, 18, 20, 21]. Two published studies have reported long-term follow-up, also with promising results [6, 11]. Due to the dearth of long-term results reported in the literature for this relatively uncommon procedure, we reviewed the long-term results of this procedure performed at our institution, which would be the largest series with follow-up beyond 5 years. Our hypothesis is that even 5–10 years postoperative, first metacarpal extension osteotomy provides good relief of pain and patient satisfaction, while preserving range of motion and pinch strength compared to the contralateral extremity.
Materials and Methods
Approval of the institutional review board was obtained prior to conducting the study. We retrospectively reviewed a consecutive series of 20 individuals who underwent first metacarpal extension osteotomy for Eaton stage I or II [3] CMC arthritis at our institution between 1996 and 2005. In all cases, the indication for surgery was persistent pain following a period of nonoperative treatment including oral nonsteroidal anti-inflammatory drugs, splinting, and corticosteroid injections. In the procedure, the dorsal aspect of the first metacarpal was exposed subperiosteally. Approximately 1 cm from the base of the first metacarpal, a microsagittal saw was used to make a 30° closing wedge osteotomy. A 22-gauge wire was passed through transverse holes on either side of the osteotomy. After manual compression of the osteotomy site, the tightened wire was supplemented with 0.045-in K-wire across the osteotomy site. The K-wire was removed 6 weeks postoperative. Postoperative X-rays are shown in Figs. 1, 2, and 3.
A questionnaire was sent to each individual with basic questions about satisfaction with the procedure (e.g., What was your satisfaction level in the few months after surgery compared to your satisfaction level now? Given the choice now, would you have the procedure done again? Have you had any additional treatment for the hand since surgery?). The questionnaire also included a visual analog scale (Table 1) [9] and a QuickDASH questionnaire [1, 7]. Each individual was also invited to return for a follow-up examination and X-rays to objectively evaluate the status of his or her hand.
Subjective outcome data from the questionnaires was collected for the enrolled patients and organized in an Excel spreadsheet (Microsoft, Redmond, WA). The results were summarized as percentages or as means with standard deviations and ranges.
For the patients who agreed to return for clinical examination, objective data collected included range of motion (radial abduction, palmar abduction, and opposition), pinch strength, and grip strength using a standard handheld dynamometer (Jamar, Sammons Preston Rolyan, Bolingbrook, IL). Measurements were compared to the contralateral, nonoperative extremity. New hand radiographs were compared to preoperative radiographs for progression of degenerative changes.
Results
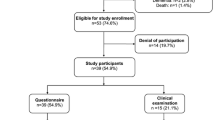
Of the 20 individuals who underwent the procedure between 1996 and 2005, 1 was deceased. One individual was contacted but refused to participate in the study. Five individuals had moved or were otherwise not able to be contacted. The remaining 13 individuals completed and returned their questionnaires and were enrolled in the study. There were 12 women and 1 man with an average age of 53 years (range 40 to 69). Ten patients were classified as Eaton stage I, and three were classified as Eaton stage II preoperatively. The surgery was performed by one of three hand surgeons at our institution. Surgery was performed on ten right thumbs and three left; in ten cases, it was the dominant hand. Of the 13 patients who completed questionnaires, 10 agreed to return for clinical evaluation. Of those ten, eight agreed to repeat radiographs of the hand.
The average postoperative follow-up period was 9.9 years (range 68 to 170 months). Ten patients (77 %) reported being either satisfied or very satisfied during the few months after surgery. One was neither satisfied nor dissatisfied, and two were dissatisfied. The same ten patients remained satisfied or very satisfied at the current time, with two neither satisfied nor dissatisfied and one very dissatisfied currently. Nine patients (69 %) answered that given the choice now, they would have the procedure done again. Three patients stated that they would not have the surgery again, and one was not sure. Of those patients, one was dissatisfied due to residual numbness around the incision, although she had complete resolution of her arthritic pain. One patient reported being very satisfied with the results of the operation but indicated on her questionnaire that she would not have the procedure done again, with no specified reason. One patient had a genuinely poor result with persistent severe pain and a QuickDASH score of 79.6. The patient who indicated that she was not sure if she would have the procedure done again had a traditional ligament reconstruction tendon interposition (LRTI) on the contralateral side and was happier with the final result of that operation.
To date, none of the patients have required further operative intervention on the involved thumb, although one patient subsequently received a corticosteroid injection. Two patients subsequently underwent conventional LRTI procedures on the contralateral thumb for a more advanced stage of CMC arthritis.
Results of the visual analog scale are summarized in Table 2. The mean value for pain level, on a scale of 1 (nonexistent) to 7 (unbearable), was 2.0. Mean value for fine hand use, on a scale of 1 (skillful) to 7 (clumsy), was 3.0. Mean value for hand use with day-to-day activities, on a scale of 1 (no problem) to 7 (useless), was 2.1.
Scores for the QuickDASH questionnaire were calculated. QuickDASH scores are based on a scale of 1 to 100, with higher scores signifying greater disability [1, 7]. The mean QuickDASH score was 23.3, with a median of 9.1 and a range of 0 to 79.6. Eight (62 %) of the 13 patients had a QuickDASH score below 10, representing minimal disability.
Objective data was obtained for 10 of the 13 enrolled patients, as 3 patients refused returning for a follow-up appointment. Results are detailed in Table 3. Range of motion was preserved compared to the contralateral, nonoperative extremity. Mean radial abduction was 45.5° in both operative and nonoperative extremities. Palmar abduction was 48.5° compared to 47° in the nonoperative extremity. Opposition, measured as the point to which the tip of the thumb could be opposed, was equal to the contralateral side in nine of the ten patients and decreased for one patient (metacarpophalangeal (MCP) flexion crease of ring finger compared to MCP flexion crease of small finger). Pinch strength was also preserved, with a mean of 13.1 lbs compared to 12.8 lbs in the contralateral extremity.
Eight of the 10 patients who returned for follow-up consented to follow-up radiographs. All eight had healed their osteotomies (in our chart review, there was no mention of nonunion at the osteotomy site). Five (63 %) had no progression in Eaton stage. The remaining three (37 %) progressed from an Eaton stage I to an Eaton stage II. Of these three, one remained very satisfied, with symmetric pinch strength and range of motion. One was satisfied, with symmetric pinch strength and range of motion. The last was neither satisfied nor dissatisfied, with symmetric pinch strength but slightly decreased radial and palmar abduction compared to the contralateral side at follow-up. She reported improvement in pain after surgery, although she stated that it was “not perfect.”
Discussion
Thirty-degree extension osteotomy of the first metacarpal as described by Wilson has been used as an alternative to reconstruction of the POL for treatment of early-stage CMC arthritis [20]. Pellegrini and associates’ biomechanical studies demonstrated that a 30° closing wedge extension osteotomy unloads the volar aspect of the TM joint, typically the area affected earliest by degenerative changes. During pinch, force is thereby transferred to the dorsal articular surface, which is typically uninvolved in early disease [15]. By off-loading the arthritic volar aspect of the TM joint, progression of arthritis should theoretically be slowed, and arthritic pain should be reduced, providing a rationale for the procedure. Additionally, biomechanical studies by Shrivastava and Koff et al. demonstrated that metacarpal extension osteotomy in cadaveric specimens reduces CMC joint laxity in the position of lateral pinch, to a degree similar to that of standard ligament reconstruction [8, 17]. Thus, in addition to physically off-loading the arthritic volar aspect of the TM joint, metacarpal extension osteotomy may reduce the joint laxity that initially contributed to the early joint degeneration. These studies provide two possible biomechanical explanations for the clinical improvement and slowing of degenerative changes that can be seen following metacarpal extension osteotomy.
Several studies have reported short- to medium-term follow-up following metacarpal extension osteotomy. These studies have reported subjective measures such as pain relief and patient satisfaction, as well as objective measures such as strength and radiographic progression of arthritis. In terms of pain relief, three studies (8 cases, 23 cases, and 17 cases) reported pain relief in all patients who underwent the procedure [10, 20, 21]. One study reported 80 % good or excellent pain relief [6]. Regarding subjective patient satisfaction, studies have reported 6 of 8 (75 %) satisfied, 8 of 10 (80 %) satisfied, and up to 11 of 12 (92 %) satisfied [5, 11, 18].
In terms of objective measures, more recent studies have reported improvements in grip and pinch strengths. One study reported a mean increase of 8.5 kg in grip strength and 3 kg in pinch strength compared to preoperative [18]. Another study compared strength to the contralateral side, as we did in our study; grip strength averaged 108 % contralateral, and pinch strength averaged 103 % contralateral [11]. Two studies evaluated radiographic progression of arthritis; one reported progression in three of the eight at a mean follow-up of 9 years, while the other reported no progression in Eaton stage, although the mean follow-up was only 4 years [5, 11].
The results of our study are similar to the previously published results in terms of pain relief (mean value 2 on the scale of 1–7), patient satisfaction (77 % satisfied or very satisfied), pinch strength (13.1 lbs compared to 12.8 lbs contralateral), and radiographic progression (5 of 8 with no radiographic progression). Our study included additional outcome measures such as a QuickDASH score and range of motion (radial/palmar abduction and opposition), which remained similar to the contralateral extremity. Most importantly, though, despite our considerable loss to follow-up, our study is the largest series reporting results of long-term follow-up beyond 5 years. We could only find two other studies that reported any long-term data, with mean follow-up periods of 9 and 6.8 years, compared to 9.9 years in our study [6, 11].
Two of our study patients subsequently had a traditional LRTI procedure performed on the contralateral side for a more advanced stage of CMC arthritis. In one of these patients (patient 2, Table 3), final radial abduction, palmar abduction, and grip strength were all higher than the contralateral thumb that underwent LRTI. Pinch strength was slightly decreased (5 vs 6 lbs). In the other patient (patient 5, Table 3), radial abduction, palmar abduction, pinch strength, and grip strength were all higher on the osteotomy side compared to the LRTI side. Although one patient reported a better subjective result from the LRTI side, our results show that within our small study group, range of motion and strength are still overall better preserved with the osteotomy procedure, although the severity of the preoperative arthritis was less.
Most of the weaknesses of our study are due to its retrospective nature and our lack of preoperative data. Loss to follow-up was considerable. All efforts were made to contact the potential subjects, but some were not able to be contacted, and some refused participation. Our sample size was small, but it is comparable to other reported study groups for this relatively uncommon procedure. We did not have preoperative values for the visual analog scale or the QuickDASH, which limits the interpretation of those results. We also did not have adequate preoperative data for range of motion and grip/pinch strength, so comparisons were made to the contralateral side, which is potentially flawed because of the possibility of concomitant disease in the contralateral extremity. Finally, our patients were treated by three different surgeons, so the surgical technique among our study group may have differed slightly.
Still, we report long-term follow-up data (average 9.9 years) on a group of patients who underwent first metacarpal extension osteotomy for early CMC arthritis. These results are comparable to results for metacarpal osteotomy reported to date in the literature, with longer term follow-up. Even 5–10 years postoperative, first metacarpal extension osteotomy provides good relief of pain and patient satisfaction, while preserving range of motion and pinch strength compared to the contralateral extremity. It is a reasonable and durable alternative to traditional ligament reconstruction in patients with early-stage CMC arthritis.
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008. Informed consent was obtained from all patients for being included in the study.
References
Beaton DE, Wright JG, Katz JN, Upper Extremity Collaborative Group. Development of the QuickDASH: comparison of three item-reduction approaches. J Bone Joint Surg Am. 2005;87(5):1038–46.
Eaton RG, Lane LB, Littler JW, Keyser JJ. Ligament reconstruction for the painful thumb carpometacarpal joint: a long-term assessment. J Hand Surg [Am]. 1984;9(5):692–9.
Eaton RG, Littler JW. Ligament reconstruction for the painful thumb carpometacarpal joint. J Bone Joint Surg Am. 1973;55(8):1655–66.
Freedman DM, Eaton RG, Glickel SZ. Long-term results of volar ligament reconstruction for symptomatic basal joint laxity. J Hand Surg [Am]. 2000;25(2):297–304.
Futami T, Nakamura K, Shimajiri I. Osteotomy for trapeziometacarpal arthrosis. 4(1-6) year follow-up of 12 cases. Acta Orthop Scand. 1992;63(4):462–4.
Hobby JL, Lyall HA, Meggitt BF. First metacarpal osteotomy for trapeziometacarpal osteoarthritis. J Bone Joint Surg (Br). 1998;80(3):508–12.
Hudak PL, Amadio PC, Bombardier C. Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder and hand) [corrected]. The Upper Extremity Collaborative Group (UECG). Am J Ind Med. 1996;29(6):602–8.
Koff MF, Shrivastava N, Gardner TR, Rosenwasser MP, Mow VC, Strauch RJ. An in vitro analysis of ligament reconstruction or extension osteotomy on trapeziometacarpal joint stability and contact area. J Hand Surg [Am]. 2006;31(3):429–39.
Macey AC, Burke FD, Abbott K, Barton NJ, Bradbury E, Bradley A, et al. Outcomes of hand surgery. British Society for Surgery of the Hand. J Hand Surg (Br). 1995;20(6):841–55.
Molitor PJ, Emery RJ, Meggitt BF. First metacarpal osteotomy for carpometacarpal osteoarthritis. J Hand Surg (Br). 1991;16(4):424–7.
Parker WL, Linscheid RL, Amadio PC. Long-term outcomes of first metacarpal extension osteotomy in the treatment of carpal-metacarpal osteoarthritis. J Hand Surg [Am]. 2008;33(10):1737–43.
Pellegrini Jr VD. Osteoarthritis of the trapeziometacarpal joint: the pathophysiology of articular cartilage degeneration. I. Anatomy and pathology of the aging joint. J Hand Surg [Am]. 1991;16(6):967–74.
Pellegrini Jr VD. Osteoarthritis of the trapeziometacarpal joint: the pathophysiology of articular cartilage degeneration. II. Articular wear patterns in the osteoarthritic joint. J Hand Surg [Am]. 1991;16(6):975–82.
Pellegrini Jr VD, Olcott CW, Hollenberg G. Contact patterns in the trapeziometacarpal joint: the role of the palmar beak ligament. J Hand Surg [Am]. 1993;18(2):238–44.
Pellegrini Jr VD, Parentis M, Judkins A, Olmstead J, Olcott C. Extension metacarpal osteotomy in the treatment of trapeziometacarpal osteoarthritis: a biomechanical study. J Hand Surg [Am]. 1996;21(1):16–23.
Pellegrini Jr VD, Smith RL, Ku CW. Pathobiology of articular cartilage in trapeziometacarpal osteoarthritis. I. Regional biochemical analysis. J Hand Surg [Am]. 1994;19(1):70–8.
Shrivastava N, Koff MF, Abbot AE, Mow VC, Rosenwasser MP, Strauch RJ. Simulated extension osteotomy of the thumb metacarpal reduces carpometacarpal joint laxity in lateral pinch. J Hand Surg [Am]. 2003;28(5):733–8.
Tomaino MM. Treatment of Eaton stage I trapeziometacarpal disease with thumb metacarpal extension osteotomy. J Hand Surg [Am]. 2000;25(6):1100–6.
Tomaino MM, King J, Leit M. Thumb basal joint arthritis. In: Green DP, Hotchkiss RN, Pederson WC, Wolfe SW, editors. Green’s operative hand surgery. 5th ed. Philadelphia, PA: Elsevier; 2005. p. 461.
Wilson JN. Basal osteotomy of the first metacarpal in the treatment of arthritis of the carpometacarpal joint of the thumb. Br J Surg. 1973;60(11):854–8.
Wilson JN, Bossley CJ. Osteotomy in the treatment of osteoarthritis of the first carpometacarpal joint. J Bone Joint Surg (Br). 1983;65(2):179–81.
Conflict of Interest
Franklin H. Chou declares that he has no conflict of interest.
James J. Irrgang declares that he has no conflict of interest.
Robert J. Goitz declares that he has no conflict of interest.
No identifiable patient information was included in this submission, so no additional informed consent was obtained beyond the written informed consent to participate in the study.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Chou, F.H., Irrgang, J.J. & Goitz, R.J. Long-term follow-up of first metacarpal extension osteotomy for early CMC arthritis. HAND 9, 478–483 (2014). https://doi.org/10.1007/s11552-014-9632-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11552-014-9632-z