Abstract
Aim
Evaluating clinical and technical factors affecting thermal ablation of B-Mode/CEUS inconspicuous HCC nodules, relying only on fusion imaging (FI) performed under conscious sedation and using previously acquired CT or MR.
Materials and methods
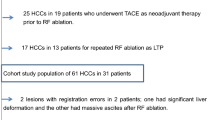
Among 367 HCC nodules treated in the study period, data of 37 B-mode/CEUS undetectable HCC nodules treated with FI-guided ablation were extracted from our prospectively collected institutional database. Analyzed variables included patients’ sex, age, cirrhosis etiology, Child–Pugh status, size of the lesion, liver segment, subcapsular or central liver site, type of imaging used for fusion (MR/CT), and the presence of surrounding anatomical landmarks (SAL) < 3 cm from the index lesion.
Results
The primary efficacy was 59.4% (22/37 nodules); nine lesions (24.3%) were partially ablated (PA), six lesions (16.7%) were mistargeted (MA). Eight nodules were retreated with a CA obtained in all cases (100% CA, secondary efficacy in 30/37—81.1%). LTP was observed in 2/30 cases (6.7%). Two minor complications were registered (Clavien–Dindo, Grade1, CIRSE Classification Grade 2). SAL were related to a better ablation outcome (37.5% vs 84.6% p = 0.01). No differences were observed between CA group and PA–MA group in terms of lesion size (15.4 mm vs 14.9 mm p = 0.63), liver segment (p = 0.58), subcapsular or central liver site (8/22 36% vs 4/15 26.7% p = 0.84), and imaging (MR vs CT, p = 0.72).
Conclusion
Even in the presence of potentially critical conditions (completely B-Mode/CEUS inconspicuous nodules, spontaneous breathing, and previously acquired CT or MRI), FI-only guidance is safe and allows having good primary, secondary efficacy and LTP rates. The outcome of the procedure is heavily affected by the presence of SAL.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Image-guided percutaneous thermal ablation is a well-established curative treatment for the very early and early stage of hepatocellular carcinoma (HCC) [1, 2] that remains the sixth most common cancer worldwide and the third leading cause of cancer-related deaths in the world [3].
Nowadays, ultrasound (US) guidance, especially in Europe and eastern countries, remains the most used guiding modality because of its several advantages, such as real-time control, accessibility, relatively low cost without ionizing radiation exposure [1, 4].
Nevertheless, due to the great recent developments in the CT and MRI fields, interventional radiologists are asked to reach and treat percutaneously smaller nodules, not clearly detectable on conventional ultrasound imaging [5, 6]. Indeed, according to the literature data, approximately 14.6–33.1% of the HCC nodules are inconspicuous on conventional B-mode evaluation and ablation could not be performed under the sole US guidance [4, 7,8,9].
Contrast-enhanced US (CEUS) has been reported as a valuable aid in these cases to target properly the nodules. However, because of poor conspicuity, location or low arterial phase wash-in, there are some cases (up to 45% in the literature series) in which even CEUS fails to clearly detect the nodule [10].
In recent years, fusion imaging (FI) has been proposed as a solution to overcome these limitations of US guidance, enabling a real-time display of MR or CT images on the same screen during ablation [11,12,13,14,15].
Despite the presence in the literature of several reports on this topic, factors affecting FI guidance during ablation of US inconspicuous HCC nodules have never been fully investigated, especially if performed under conscious sedation, when patients can breathe spontaneously, potentially affecting the synchronization process of FI.
The aim of our study is to evaluate, in this specific setting, the most relevant factors affecting the outcome of thermal ablation of completely inconspicuous HCC nodules with FI guidance.
Materials and methods
Study design
This study was approved by the institutional ethics review board. Written informed consent was obtained from each patient. The prospectively compiled interventional radiology liver ablation registry of our institution was retrospectively evaluated and updated by review of the electronic medical records to identify consecutive patients who underwent percutaneous liver ablation for the treatment of HCC nodules from January 2016 through May 2018.
Patient selection, ablation eligibility criteria and technique
Patients were considered for percutaneous ablation in case of no more than three HCC nodules, measuring ≤ 3 cm each. HCC diagnosis was performed with cross-sectional imaging (CT or MRI) according to EASL criteria.
Indication for ablation was discussed at the institution’s multidisciplinary HCC tumor board. Patients underwent percutaneous image-guided ablation according to BCLC indications. Exclusion criteria were platelets count < 50,000, INR > 1.5, and the presence of massive ascites.
Among 367 HCC nodules treated in 272 patients in the study period, 58 nodules in 42 patients were considered as undetectable with conventional B-mode ultrasound only. Among these, 21 nodules were visible with good conspicuity at CEUS examination by injecting 2.4 ml of SonoVue (Bracco, Milan, Italy); 37 nodules in 26 patients were completely undetectable at B-mode or CEUS examination and FI guidance was performed. Variables extracted from the database or updated by review of electronic medical records for each patient and procedure included sex, age, cirrhosis etiology, Child–Pugh status, size of the lesion, liver segment, subcapsular or central liver site, type of imaging used for fusion (MRI sequences or CT phases), and the presence of surrounding anatomical landmarks (SAL); SAL were defined as any anatomical structure (such as vessels larger than 3 mm, cysts or ligaments) no more distant than 3 cm on axial CT or MR images from the index lesion.
Ablations were done under conscious sedation by interventional radiologists using a 17-gauge RFA electrode multi-tined needle (Med-Italia, Medolla, Italy) with a radiofrequency generator (RF3000, 200 W capacity, Radiofrequency Ablation System, Boston Scientific). No virtual needle assistance was used. Procedures were performed under conscious sedation and spontaneous breathing. Before the needle insertion, 10 ml of 2% lidocaine hydrochloride was injected at the puncture site.
Fusion imaging process
Before fusion imaging, the pre-acquired dynamic CT or MRI DICOM volume data were loaded into the ultrasound unit (Esaote My Lab Twice, Genova, ITA). The patient was always positioned in the supine position as for the CT and MRI scan. With the plane registration, the physician found the same plane on real-time US and uploaded CT or MR images (any plane can be used but, for simplicity, the umbilicus axial plane was considered the first choice) [16]. After plane registration, point registration was performed to improve the matching. This was usually performed by using an internal point near the target lesion. Other available functions, such as “rotate” or “drag,” were useful to optimize the real-time US-CECT/CEMRI matching [17].
Assessment of tumor ablation results
Standardized terminology and reporting criteria for tumor ablation were utilized to determine ablation endpoints [18]. Accordingly, primary efficacy rate was defined as the percentage of target tumors successfully eradicated following the initial procedure. Residual unablated tumor (partial ablation PA) was defined as the presence of peripheral or nodular enhancement within 1 cm of the ablated area at the first imaging follow-up (triple-phase contrast-enhanced computed tomography [CT] or magnetic resonance [MR]). We defined missed ablation (MA) as the condition of complete mistargeting of the nodule at the first ablation attempt, when the distance between ablated volume center and ideal target point preoperatively established was greater than 5 mm [19]. The secondary efficacy rate is defined as including tumors that have undergone successful repeat ablation. Local tumor progression (LTP) was defined as the appearance of tumor foci at the edge of the ablation zone or within 1 cm after at least one cross-sectional imaging had demonstrated complete ablation.
Statistical analysis
The normality of distribution for continuous numeric data was assessed with Saphiro–Wilk test. Thus, according to the defined groups, data were reported as mean, standard deviation (SD), and ranges for normally distributed variables, while median, ranges, and interquartile ranges were used for not normally distributed variables. Non-continuous non-normally distributed variables were analyzed using Chi-Squared test or Fisher’s test in case of small numbers. In case of small data (such as segment location), pooled analysis was performed. Mann–Whitney test was used to compare continuous non-normally distributed variables. p values below 0.05 were considered statistically significant. Statistical analysis was performed using GraphPad Stats Software (2018).
Results
From January 2016 to May 2018, a total of 37 HCC nodules in 26 patients (see Table 1 for nodule and patient characteristics) underwent image-guided ablation relying only on FI guidance in consideration of their undetectability at conventional B-mode or CEUS imaging. (See Table 1 for patients’ characteristics.)
According to Clavien–Dindo classification, only two minor complications requiring standard medical therapy (grade I) were observed after two ablation sessions. According to CIRSE classification of complications, only two non-severe complications occurred (grade II).
Complete ablation (primary efficacy) was obtained in 22/37 nodules (59.4%); nine lesions (24.3%) were partially ablated (PA), whereas six lesions (16.7%) were mistargeted (MA). Eight nodules were retreated with a CA obtained in all cases (100% CA, overall secondary efficacy in 30/37—81.1%). Among the seven remaining nodules, in four cases (two patients), intrahepatic progression was observed and TACE was performed; in two cases, patients underwent liver transplantation, and in one case, patient was lost to follow-up. On the whole, LTP was observed in 2/30 cases (6.7%). Mean time F.U was 12.4 months.
The presence of surrounding anatomical landmarks was statistically related to a better ablation outcome (37.5% vs 84.6% p = 0.01). No differences were observed between CA group and PA–MA group in terms of patients’ age (58.3 vs 63.8 years p = 0.23), Child–Pugh class (6.2 vs 5.6 for both groups, median 6, p = 0.6), cirrhosis etiology (HCV-related in 10/22 in CA group vs 8/15 in PA–MA group, p = 0.82), lesion size (15.4 mm vs 14.9 mm p = 0.63), liver segment (9/22 vs 9/15 p = 0.58), subcapsular or central liver site (8/22 36% vs 4/15 26.7% p = 0.84), and type of imaging used for fusion imaging (MRI sequences, 19/22, 86% vs 12/15, 80% p = 0.45) (see Table 2).
Discussion
Our study investigated the role of fusion imaging guidance in treating HCC nodules completely undetectable at conventional B-mode US or CEUS evaluation.
The main findings of our study were:
-
The primary efficacy of FI-guided treatments is 59.4%; the secondary efficacy reaches the 81.1% with a LTP rates at 1 year F.U. of 6.7%;
-
The outcome of the procedure is affected by the presence of anatomical landmark (CA in the absence of AL 37.5% vs CA in the presence of SAL 84.6% p = 0.01);
-
The lesion site (segment, subglissonian or central parenchymal lesion) does not significantly affect the ablation outcome (p > 0.05).
On the whole, primary efficacy of FI-guided ablation presented in our series may appear below the literature-reported results for US conspicuous HCC nodules [2, 20].
In recent years, several retrospectives [13, 20,21,22,23,24,25], and one prospective studies [26] evaluated FI technique and compared it with the conventional ultrasound guidance (see Table 2). The reported technical success rate of these procedures was around 90% (89.2–92%).
However, these series often included nodules with poor conspicuity [22] or CEUS positivity [25]. In a more recent series, Mauri et al. [19] analyzed a series of FI-guided ablation of completely inconspicuous liver metastases and they demonstrated a similar primary success rate (56.7% 17/30 patients, in the PET-CT group). In our series, however, even in case of missed ablation at the first ablation, the ablation scar was used as reliable internal anatomical landmark to repeat the FI targeting and to perform ablation. Indeed, we reached a 100% CA as a second attempt with an overall LTP rate (6.7%) in line with the other literature reports about poorly visible or visible nodules [13, 22, 26].
As for the anatomical landmarks, they are well known among FI operators for their role in the second part of the plane and point registration [17]. Our study suggests for them a role of paramount importance in case of ablation of completely inconspicuous nodules in procedures performed in critical technical conditions, such as under conscious sedation, spontaneous breathing and with a pre-acquired CT. Indeed, once co-registration is performed, a surrounding anatomical landmark in proximity of the target may help the operator to continually visualize the area of interest, even during respiratory movements (see Fig. 1). The presence of SAL < 3 cm permitted to achieve a better local result (37.5% vs 84.6%, p = 0.01).
Despite its relevance, the breathing status during FI registration and during the procedure is rarely described in the literature reports. However, many studies with primary efficacy rates above 90% (such as the one of Mauri et al. [21]) are performed with patients under general anesthesia. In fact, with endotracheal general anesthesia, the breath of the patient can be well controlled using a breathing machine for as long as 2 min, greatly facilitating co-registration and subsequent ablation.
Furthermore, our series was characterized by the usage of pre-acquired cross-sectional imaging (CT or MR). In other series, the availability of CT in the operatory room allowed for acquisition of real-time CT images with the patient already under general anesthesia and in the desired decubitus, so the correspondence between CT and US images is increased [27].
However, these facilities are rarely available in most of the IR services worldwide and physicians are usually asked to merge with real-time US a pre-acquired CT or MRI in supine position. Furthermore, costs and risks of general anesthesia should be carefully evaluated. Therefore, we believe our study gives pertinent information on the relevance of anatomical landmarks in a specific but widespread clinical setting of fusion imaging.
As for other possible predicting factors that may affect the outcome of the ablation, our study did not find any significant statistical correlation. Relevantly, despite a prevalence of HCC nodules located in segment 7 and 8 (19/37, 51%), this did not affect the outcome of the FI-guided ablation if compared with other segment site (p = 0.58). Even the subglissonian or central parenchyma site of the lesion seems not to affect the ablation outcome. As for clinical- and patient-related factors potentially affecting the ablation outcomes, as well as in the other literature series [21, 28], we did not find any significant correlation (p > 0.05).
The major limitation of our study is its retrospective nature and a relatively limited sample size; for the same reason, we could not stratify results based on minimal margin size given the need for a much larger sample size; however, these problems are common with other published papers on similar series [19, 22, 25].
In conclusion, our study demonstrates the feasibility of FI-guided ablation under conscious sedation of inconspicuous HCC nodules with acceptable primary, excellent secondary efficacy, and LTP rates. The presence of anatomical landmarks in proximity of the inconspicuous HCC target is a relevant predictive factor of effective ablation outcome that can overcome the challenges of respiratory movements during FI-guided ablation.
References
Choi D et al (2007) Percutaneous radiofrequency ablation for early-stage hepatocellular carcinoma as a first-line treatment: long-term results and prognostic factors in a large single-institution series. Eur Radiol 17(3):684–692
Livraghi T et al (2007) Sustained complete response and complications rates after radiofrequency ablation of very early hepatocellular carcinoma in cirrhosis: Is resection still the treatment of choice? Hepatology 47(1):82–89
Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D (2011) Global cancer statistics. CA Cancer J Clin 61(2):69–90
Rhim H, Lee MH, Kim Y, Choi D, Lee WJ, Lim HK (2008) Planning sonography to assess the feasibility of percutaneous radiofrequency ablation of hepatocellular carcinomas. Am J Roentgenol 190(5):1324–1330
Samanci C et al (2016) Magnetic resonance imaging in diagnosis and monitoring of hepatocellular carcinoma in liver transplantation: a comprehensive review. Ann Transplant 21:68–76
Park HJ, Lee JM, Park SB, Lee JB, Jeong YK, Yoon JH (2016) Comparison of knowledge-based iterative model reconstruction and hybrid reconstruction techniques for liver CT evaluation of hypervascular hepatocellular carcinoma. J Comput Assist Tomogr 40(6):863–871
Kim PN et al (2012) Planning ultrasound for percutaneous radiofrequency ablation to treat small (≤ 3 cm) hepatocellular carcinomas detected on computed tomography or magnetic resonance imaging: a multicenter prospective study to assess factors affecting ultrasound visibility. J Vasc Interv Radiol 23(5):627–634
Lee MW et al (2010) Targeted sonography for small hepatocellular carcinoma discovered by CT or MRI: factors affecting sonographic detection. Am J Roentgenol 194(5):W396–W400
Kim J-E et al (2011) Outcomes of patients with hepatocellular carcinoma referred for percutaneous radiofrequency ablation at a tertiary center: analysis focused on the feasibility with the use of ultrasonography guidance. Eur J Radiol 79(2):e80–e84
Jo PC, Jang H-J, Burns PN, Burak KW, Kim TK, Wilson SR (2017) Integration of contrast-enhanced US into a multimodality approach to imaging of nodules in a cirrhotic liver: How I do it. Radiology 282(2):317–331
Lee MW (2014) Fusion imaging of real-time ultrasonography with CT or MRI for hepatic intervention. Ultrasonography 33(4):227–239
Abi-Jaoudeh N et al (2012) Multimodality image fusion guided procedures: technique, accuracy, and applications. Cardiovasc Intervent Radiol 35(5):986–998
Lee MW et al (2012) Percutaneous radiofrequency ablation of hepatocellular carcinoma: fusion imaging guidance for management of lesions with poor conspicuity at conventional sonography. Am J Roentgenol 198(6):1438–1444
Ewertsen C, Săftoiu A, Gruionu LG, Karstrup S, Nielsen MB (2013) Real-time image fusion involving diagnostic ultrasound. Am J Roentgenol 200(3):W249–W255
Dong Y, Wang W-P, Mao F, Ji Z-B, Huang B-J (2016) Application of imaging fusion combining contrast-enhanced ultrasound and magnetic resonance imaging in detection of hepatic cellular carcinomas undetectable by conventional ultrasound: hepatocellular carcinoma imaging fusion. J Gastroenterol Hepatol 31(4):822–828
Ewertsen C, Săftoiu A, Gruionu LG, Karstrup S, Nielsen MB (2013) Real-time image fusion involving diagnostic ultrasound. Am J Roentgenol 200(3):W249–W255
Lee MW (2014) Fusion imaging of real-time ultrasonography with CT or MRI for hepatic intervention. Ultrasonography 33(4):227–239
Ahmed M et al (2014) Image-guided tumor ablation: standardization of terminology and reporting criteria—a 10-year update. Radiology 273(1):241–260
Mauri G et al (2018) Real-time US-18FDG-PET/CT image fusion for guidance of thermal ablation of 18FDG-PET-positive liver metastases: the added value of contrast enhancement. Cardiovasc Intervent Radiol 42:60–68
Veltri A, Sacchetto P, Tosetti I, Pagano E, Fava C, Gandini G (2008) Radiofrequency ablation of colorectal liver metastases: small size favorably predicts technique effectiveness and survival. Cardiovasc Intervent Radiol 31(5):948–956
Mauri G et al (2015) Real-time US-CT/MRI image fusion for guidance of thermal ablation of liver tumors undetectable with US: results in 295 cases. Cardiovasc Intervent Radiol 38(1):143–151
Makino Y et al (2013) Ultrasonography fusion imaging system increases the chance of radiofrequency ablation for hepatocellular carcinoma with poor conspicuity on conventional ultrasonography. Oncology 84(s1):44–50
Min JH et al (2014) Radiofrequency ablation of very-early-stage hepatocellular carcinoma inconspicuous on fusion imaging with B-mode US: value of fusion imaging with contrast-enhanced US. Clin Mol Hepatol 20(1):61
Song KD, Lee MW, Rhim H, Cha DI, Chong Y, Lim HK (2013) Fusion imaging—guided radiofrequency ablation for hepatocellular carcinomas not visible on conventional ultrasound. Am J Roentgenol 201(5):1141–1147
Minami T et al (2014) Combination guidance of contrast-enhanced US and fusion imaging in radiofrequency ablation for hepatocellular carcinoma with poor conspicuity on contrast-enhanced US/fusion imaging. Oncology 87(s1):55–62
Ahn SJ et al (2017) Real-time US-CT/MR fusion imaging for percutaneous radiofrequency ablation of hepatocellular carcinoma. J Hepatol 66(2):347–354
Hakime A, Yevich S, Tselikas L, Deschamps F, Petrover D, De Baere T (2017) Percutaneous thermal ablation with ultrasound guidance. Fusion imaging guidance to improve conspicuity of liver metastasis. Cardiovasc Intervent Radiol 40(5):721–727
Brunello F et al (2008) Radiofrequency ablation versus ethanol injection for early hepatocellular carcinoma: a randomized controlled trial. Scand J Gastroenterol 43(6):727–735
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standards
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation and with the Helsinki Declaration of 1975.
Informed consent
Informed consent was obtained from all patients included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Calandri, M., Ruggeri, V., Carucci, P. et al. Thermal ablation with fusion imaging guidance of hepatocellular carcinoma without conspicuity on conventional or contrast-enhanced US: surrounding anatomical landmarks matter. Radiol med 124, 1043–1048 (2019). https://doi.org/10.1007/s11547-019-01057-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-019-01057-1