Abstract
Purpose
The aim of the study was to evaluate the prevalence of collateral findings detected in computed tomography coronary angiography (CTCA) in a multi-center registry.
Materials and methods
We performed a retrospective review of 4303 patients (2719 males, mean age 60.3 ± 10.2 years) undergoing 64-slice CTCA for suspected or known coronary artery disease (CAD) at various academic institutions between 01/2006 and 09/2010. Collateral findings were recorded and scored as: non-significant (no signs of relevant pathology, not necessary to be reported), significant (clear signs of pathology, mandatory to be reported), or major (remarkable pathology, mandatory to be reported and further investigated).
Results
We detected 6886 non-cardiac findings (1.6 non cardiac finding per patient). Considering all centers, only 865/4303 (20.1 %) patients were completely without any additional finding. Overall, 2095 (30.4 %) non-significant, 4486 (65.2 %) significant, and 305 (4.4 %) major findings were detected. Among major findings, primary lung cancer was reported in 21 cases. In every center, most prevalent significant findings were mediastinal lymph nodes >1 cm. In 256 patients, collateral findings were clinically more relevant than coexisting CAD and justified the symptoms of patients.
Conclusions
The prevalence of significant and major collateral findings in CTCA is high. Radiologists should carefully evaluate the entire scan volume in each patient.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Non-invasive imaging of the coronary arteries represents an important clinical application since CT Coronary Angiography (CTCA) has proven to be an accurate imaging method alternative to conventional coronary angiography [1–3]. CTCA may be employed in patients with low-to-intermediate pre-test probability of coronary artery disease (CAD) and negative or equivocal findings on exercise stress testing [4–10].
The increasing demand of non-invasive imaging of the coronary arteries has determined the emerging issue of non-cardiac collateral findings in CTCA [11–16]. In most of the cases such findings are incidental and without any significance, but in other cases they are significant or even responsible of major pathology to be further investigated. Previous papers have addressed this issue but only on a single center level with a limited number of patients [11–16].
The aim of our study was to assess the prevalence of non-cardiac collateral findings at CTCA in a multi-center registry.
Materials and methods
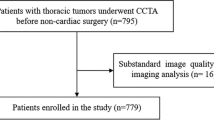
Patient population
This is a retrospective review of CTCA examinations performed for clinical reasons at various academic institutions applying comparable scan and image analysis protocols (Table 1).
All examinations were performed with 64-slice CT scanners (Sensation 64 Cardiac, Siemens, Forcheim, Germany in centers 1 and 2; VCT, GEHC, Milwaukee, USA in center 1; Brilliance 64, Philips, Best, The Netherlands in centers 3 and 4). Institutional review board approval was not required since retrospective data of standard cardiac CT examinations were used.
Inclusion and exclusion criteria
All centers applied the same inclusion and exclusion criteria. Inclusion criteria for 64-slice CTCA were: stable and low heart rate <65 bpm; breath-hold for at least 12–15 s during the acquisition. Exclusion criteria were: prior adverse reactions to iodinated contrast material, pregnancy, impaired respiratory and renal function, unstable clinical conditions, or severe heart failure. In case of high (>65 bpm) or irregular heart rate, patients received orally or intravenously β blocker therapy before scanning. Patients were scanned in the supine position during breath hold from carina to diaphragm. In case of expected cardiac surgery (i.e., aortic valve replacement) or coronary artery by-pass graft (CABG) follow-up study, the examinations were extended cranially to the origin of epiaortic vessels.
CTCA protocol
The scan and reconstruction parameters are summarized in Table 1. A retrospective ECG-gated technique was used for image reconstruction. Eighty to 100 ml of non-ionic iodinated contrast material (Iomeprol 400 mgl/ml, Iomeron, Bracco, Milan, Italy; Iodixanol 320 mgI/ml, Visipaque, GEHC, USA) were intravenously administered at a flow rate of 5 ml/s, followed by 40 ml of saline solution at the same rate. Contrast material was administered in all centers with a dual-syringe automatic injector (Stellant, MedRad, Pittsburgh, USA) connected to an 18G cannula placed in a right arm antecubital vein. The synchronization of the scan with the passage of contrast material was performed with the bolus-tracking technique.
The image datasets were reconstructed during the mid-to-end diastolic phase, with reconstruction windows set at 60–80 % of the R–R interval. In case of insufficient image quality, additional reconstructions during the end-systolic phase (25–45 % of the R–R interval) were performed. When mildly irregular heart rates were encountered, such as bundle branch blocks or premature beats, the temporal variability in the reconstruction phase was compensated manually with ECG editing. The reconstructed slice thickness was 0.6–0.75 mm with an increment of 0.4–0.5 mm. All the datasets were filtered with medium-smooth and sharp convolution kernels. In all centers an image dataset with a large field of view (including the entire thorax) was always reconstructed in each patient with the following parameters: slice thickness 1 mm, increment 0.6 mm, convolution filters medium-soft and sharp.
Image evaluation and follow-up of findings
The radiologists of every center participating to the study had a consensus meeting before the start-up of the review and decided the classification of findings.
All scans were reviewed in each center by two radiologists unaware of CT official report and with at least 6 year of training in cardiac and chest CT. Datasets were reviewed with standard mediastinal (350 W/50C), lung (1400 W/600C), and bone window settings (2000 W/800C) (Fig. 1). Additional multiplanar reconstructions with different slice thicknesses were performed to assess non-cardiac findings.
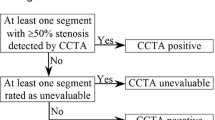
Radiologists set the classification after acknowledgement of the existing literature [12–15] and arrangement of a specific scoring method aiming at clinical relevance of findings. Furthermore, any finding not initially defined was discussed and classified in consensus at the end of the reviewing process of CTCA examinations. Therefore, all incidental non-cardiac collateral findings were recorded. The findings were scored as non-significant (no signs of clinically relevant pathology, not necessary to be reported; i.e., liver cysts), significant (clear signs of pathology, mandatory to be reported; i.e. pulmonary emphysema), and major (remarkable pathology, mandatory to be reported, and further investigated; i.e., lung cancer) (Figs. 2, 3, 4). In case of significant or major findings medical records of patients were reviewed in every center to check clinical follow-up, subsequent examinations (i.e., laboratory tests or imaging studies such as chest or column X-ray, CT of the neck, thorax or abdomen, and abdominal US) or surgical procedures in the 12 months after CTCA.
Collateral findings: liver cyst (arrow) as an example of non-significant finding (a); liver haemangioma (thin arrow) as an example of major finding, and hiatal hernia (thick arrow) as an example of significant finding in the same patient (b); vertebral haemangioma (arrow) as an example of significant finding (c)
Statistical analysis
Findings are expressed in terms of absolute values and percentages. Analysis was performed using the statistical options included in the package Microsoft Excel 2007. The Chi-square test was used to analyze the statistical difference between centers with reference to non-cardiac collateral findings and their classification. A value of p < 0.05 was considered significant.
Results
We retrospectively reviewed 4303 consecutive patients (2719 males and 1584 females, mean age 60.3 ± 10.2 years) undergoing CTCA for suspected or known CAD between 01/2006 and 09/2010. The first center included 2673 patients, the second 670 patients, the third 550, and the fourth 410 patients.
The patients selected for the study had clinical indications to CTCA, in particular: patients with atypical chest pain and inconclusive or equivocal or disagreeing stress test, or inability to undergo the stress test examination (n = 2279, 53 %); patients with stable angina (n = 682, 16 %); asymptomatic patients with multiple risk factors (i.e., smoking, family history, hypertension, high cholesterol, obesity, and diabetes) (n = 553, 13 %); follow-up of patients revascularized with coronary stents (n = 344, 8 %); follow-up of patients revascularized with CABG (n = 260, 6 %); patients referred to cardiac surgery (i.e., aortic valve replacement) (n = 185, 4 %). Patients’ characteristics are summarized in Table 2.
Overall, 3438 patients had non-cardiac findings: 2111 (79.3 %) in center 1, 545 (81.3 %) in center 2, 445 (80.9 %) in center 3, and 337 (82.2 %) in center 4 (p > 0.05). Only 865 (20.1 %) patients were completely without any additional finding.
Moreover, 3657 patients (85 %) revealed obstructive or not-obstructive CAD. In 256 of them (7 %), the collateral finding was more relevant than coexisting CAD and justified the clinical symptoms. Major collateral findings included pulmonary embolism (n = 35) and aortic dissection (n = 17).
Overall, 6886 non-cardiac findings (1.6 per patient) were identified: 2095 (30.4 %) non-significant, 4486 (65.2 %) significant, and 305 (4.4 %) major findings were detected (Fig. 2). In particular, 2279 (33 %) findings were detected in the lung parenchyma (Fig. 3), 1729 (25.1 %) lesions were detected in the mediastinum, and 1682 of these (97.2 %) were mediastinal lymphnodes larger than 1 cm in diameter.
On a per-center analysis, 4304 non-cardiac findings (1.6 per patient) were found in center 1, 1234 (1.8 per patient) in center 2, 781 (1.4 per patient) in center 3, and 567(1.4 per patient) in center 4. Table 3 summarizes the percentages of collateral findings per center.
The percentages of non-significant findings were 30.5 % (n = 1312) in center 1, 26.9 % (n = 332) in center 2, 40 % (n = 313) in center 3, and 24.3 % (n = 138) in center 4. The percentages of significant findings were 66.5 % (n = 2861) in center 1, 66.5 % (n = 821) in center 2, 56.5 % (n = 441) in center 3, and 64 % (n = 363) in center 4. The percentages of major findings were 3 % (n = 131) in center 1, 6.6 % (n = 81) in center 2, 3.5 % (n = 27) in center 3, and 11.7 % (n = 66) in center 4. The prevalence of non-cardiac collateral findings scored as non-significant, significant, and major differs between centers (p < 0.05).
Most prevalent not-significant findings were as follows: aortic calcifications in 37.4 % (n = 490) in center 1, in 38.9 % (n = 129) in center 2, and in 30.5 % (n = 42) in center 4, and vertebral arthrosis in 60.4 % (n = 189) in center 3. Most prevalent significant findings were mediastinal lymphnodes >1 cm in every center: 25.7 % (n = 735) in center 1, 60.1 % (n = 493) in center 2, 73.5 % (n = 324) in center 3, and 35.8 % (n = 130) in center 4. Most prevalent major findings were as follows: pulmonary nodules >1 cm in 35.1 % (n = 46 cases) in center 1 and in 18.5 % (n = 15) in center 2, lung infections in 37 % (n = 10) in center 3, and hepatic haemangioma in 24.2 % (n = 16) in center 4. Primary lung cancer was reported in 21 cases.
Discussion
With the widespread use of CTCA, the issue of incidental findings is receiving increasing attention. Previous studies have already discussed this topic with single center series [11–16]. In 2001 Hunold et al. [11] reviewed the electron beam CT examinations of 1812 consecutive patients using only the mediastinal windows and considering also cardiac extracoronary findings. They reported 38 % of non-coronary findings as located in the heart or pericardium. Moreover, they included a large number of minor, relatively insignificant abnormalities, such as scars, granulomata, atelectasis, degenerative arthritis, and rib fractures. Only 2 % of collateral findings in the lungs, mediastinum or upper abdomen were considered significant and underwent further analyses. Also in our multicenter study most of the findings were located in the lungs (33 %) and in the mediastinum (25.1 %). In 670 patients undergoing CTCA Cademartiri et al. [12] reported that only 138 patients (20.6 %) were without any additional finding. Law et al. reported that 19 % of their patients required follow-up of findings [13]. The papers of Onuma [14] and MacHaalany [15] showed similar results to our study. Onuma et al. reported a high prevalence of 58.1 % of non-cardiac findings, 35.4 % of them being non-significant. The higher prevalence of findings was mainly due to a systematic and accurate analysis of each finding which can be present in the chest; only 211 (41.9 %) patients in their series were completely free of any additional finding. In our multi-center registry, the overall prevalence of findings was even higher (79.9 %). In our series, the prevalence of non-significant collateral finding resulted 30.4 %, similar to that reported by Onuma et al. However, the prevalence of non-significant collateral findings was quite variable between centers, ranging from 24.3 % of center 4 to 40 % of center 3. The variability can be explained by the different individual attention of the radiologists to common abnormalities of chest. In MacHaalany paper out of 966 consecutive patients, 401 patients (41.5 %) had non-cardiac findings. A total of 12 (1.2 %) patients had clinically significant findings, and 68 (7 %) patients had indeterminate findings [15].
Although the number of collateral non-cardiac findings is high in all the reported experiences, including our study, the most intriguing data emerging from our study is the number of major findings (4.4 %). The result deriving from a multi-center registry amplifies the need of a thorough review of image datasets by radiologists. Our study demonstrated the potential presence of several major pathologies among different organs in the chest and upper abdomen. Furthermore, non-cardiac findings, such as pulmonary embolism and aortic dissection, may be incidentally displayed in the clinical setting of non-cardiac chest pain [8, 17]. The first center had the lowest prevalence of major findings (3 %), although the population was the largest; this aspect accounts for the high variability of findings in different populations and may reflect the different attention of radiologists to deal with non-cardiac findings in CTCA. On the other side, significant findings were more frequent with a heterogeneous distribution across centers ranging from 56.5 to 66.5 %.
The mainly involved organ in all centers was the lung parenchyma. All lung cancers detected were asymptomatic and totally incidental. For this reason, CTCA examinations deserve a careful analysis and reporting by radiologists, who should have both cardiac and thoracic CT expertise. A recent metanalysis found that extracardiac malignancies occur in 0.7 percent of patients who underwent cardiac CT, and more than 70 % of previously unknown malignancies were lung cancers [18]. In this setting, it is still controversial if a large FOV should be reconstructed. Large FOV images may display a high number of significant or major findings, but on the other side a restricted FOV can be also acceptable if a dedicated cardiac CT study is performed similarly to other districts of the body (i.e. spine, orbits, inner ear, and sinuses) [19, 20]. At our institutions large FOV images were reconstructed, however they do not include the entire lungs because the upper regions were often excluded from dedicated cardiac CT examinations.
Several limitations occur in our study. A bias may be identified because of the retrospective design of the study. The radiologists may have different individual attention to describe specific non-cardiac findings despite the definition of initial criteria. A prospective study could facilitate the description of collateral findings because of the association with the reporting process. We considered a follow-up of 1-year to check pathology in our records (Fig. 4). In some diseases such as small lung nodules, the follow-up can be too short. However, other published studies on incidental findings have incomplete or absent follow-up [16]. Our study included patients who underwent cardiac CT at different centers with the same scanner technology, namely 64-slice CT. Sixty-four-slice CT equipment fulfills current standards to perform cardiac examinations [8], despite available more recent CT generations may effectively reduce the radiation dose to patients [7–9].
Conclusions
In conclusion, a considerable number of non-cardiac findings are reported in CTCA examinations across different centers. Some of them could be missed if a comprehensive assessment of the scanned volume is not performed. Radiologists should carefully take into account and describe significant and major non-cardiac findings in CTCA reports.
References
Mowatt G, Cook JA, Hillis GS et al (2008) 64-Slice computed tomography angiography in the diagnosis and assessment of coronary artery disease: systematic review and meta-analysis. Heart 94:1386–1393. doi:10.1136/hrt.2008.145292
Francone M, Napoli A, Carbone I et al (2007) Noninvasive imaging of the coronary arteries using a 64-row multidetector CT scanner: initial clinical experience and radiation dose concerns. Radiol Med. 112:31–46. doi:10.1007/s11547-007-0118-8
Pugliese F, Mollet NR, Hunink MG et al (2008) Diagnostic performance of coronary CT angiography by using different generations of multisection scanners: single-center experience. Radiology 246:384–393. doi:10.1148/radiol.2462070113
Cademartiri F, La Grutta L, Palumbo A et al (2009) Computed tomography coronary angiography vs. stress ECG in patients with stable angina. Radiol Med. 114:513–523. doi:10.1007/s11547-009-0388-4
Malagò R, Pezzato A, Barbiani C et al (2012) Role of coronary angiography MDCT in the clinical setting: changes in diagnostic workup in the real world. Radiol Med. 117:939–952. doi:10.1007/s11547-012-0842-6
La Grutta L, La Grutta S, Galia M et al (2014) Acceptance of noninvasive computed tomography coronary angiography: for a patient-friendly medicine. Radiol Med. 119:128–134. doi:10.1007/s11547-013-0319-2
Di Cesare E, Gennarelli A, Di Sibio A et al (2014) Assessment of dose exposure and image quality in coronary angiography performed by 640-slice CT: a comparison between adaptive iterative and filtered back-projection algorithm by propensity analysis. Radiol Med. 119:642–649. doi:10.1007/s11547-014-0382-3
Di Cesare E, Carbone I, Carriero A (2012) Clinical indications for cardiac computed tomography. From the Working Group of the Cardiac Radiology Section of the Italian Society of Medical Radiology (SIRM). Radiol Med. 117:901–938. doi:10.1007/s11547-012-0814-x
Maffei E, Martini C, De Crescenzo S et al (2010) Low dose CT of the heart: a quantum leap into a new era of cardiovascular imaging. Radiol Med. 115:1179–1207. doi:10.1007/s11547-010-0566-4
La Grutta L, Runza G, Gentile G et al (2011) Prognostic outcome of routine clinical noninvasive multidetector-row computed tomography coronary angiography in patients with suspected coronary artery disease: a 2-year follow-up study. Radiol Med. 116:521–531. doi:10.1007/s11547-011-0655-z
Hunold P, Schmermund A, Seibel RM, Gronemeyer DH, Erbel R (2001) Prevalence and clinical significance of accidental findings in electron-beam tomographic scans for coronary artery calcification. Eur Heart J 22:1748–1758. doi:10.1053/euhj.2000.2586
Cademartiri F, Malago R, Belgrano M et al (2007) Spectrum of collateral findings in multislice CT coronary angiography. Radiol Med. 112:937–948. doi:10.1007/s11547-007-0194-9
Law YM, Huang J, Chen K, Cheah FK, Chua T (2008) Prevalence of significant extracoronary findings on multislice CT coronary angiography examinations and coronary artery calcium scoring examinations. J Med Imaging Radiat Oncol 52:49–56. doi:10.1111/j.1440-1673.2007.01911.x
Onuma Y, Tanabe K, Nakazawa G et al (2006) Noncardiac findings in cardiac imaging with multidetector computed tomography. J Am Coll Cardiol 48:402–406. doi:10.1016/j.jacc.2006.04.071
Machaalany J, Yam Y, Ruddy TD et al (2009) Potential clinical and economic consequences of noncardiac incidental findings on cardiac computed tomography. J Am Coll Cardiol 54:1533–1541. doi:10.1016/j.jacc.2009.06.026
Horton KM, Post WS, Blumenthal RS, Fishman EK (2002) Prevalence of significant noncardiac findings on electron-beam computed tomography coronary artery calcium screening examinations. Circulation 106:532–534. doi:10.1161/01.CIR.0000027136.56615.DE
Runza G, La Grutta L, Alaimo V et al (2007) Comprehensive cardiovascular ECG-gated MDCT as a standard diagnostic tool in patients with acute chest pain. Eur J Radiol 64:41–47. doi:10.1016/j.ejrad.2007.06.020
Flor N, Di Leo G, Squarza SA et al (2013) Malignant incidental extracardiac findings on cardiac CT: systematic review and meta-analysis. AJR Am J Roentgenol 201:555–564. doi:10.2214/AJR
Earls JP (2011) The pros and cons of searching for extracardiac findings at cardiac CT: studies should be reconstructed in the maximum field of view and adequately reviewed to detect pathologic findings. Radiology 261:342–346. doi:10.1148/radiol.11111099
White CS (2011) The pros and cons of searching for extracardiac findings at cardiac CT: use of a restricted field of view is acceptable. Radiology 261:338–341. doi:10.1148/radiol.11111131
Conflict of interest
None of the Authors have potential conflict of interests or financial disclosures concerning the material of this study.
Ethical standards
This article contains a retrospective study; for this type of study formal consent is not required. This article does not contain any studies with animals performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
La Grutta, L., Malagò, R., Maffei, E. et al. Collateral non cardiac findings in clinical routine CT coronary angiography: results from a multi-center registry. Radiol med 120, 1122–1129 (2015). https://doi.org/10.1007/s11547-015-0551-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-015-0551-z