Abstract
The aim of this national, multicenter, cross-sectional study was to assess the prevalence of hepatitis B (HBV), hepatitis C (HCV), and human immunodeficiency viruses (HIV) among prisoners, and to identify related risk behaviors including injection drug use. Overall, 4,894 inmates from 20 prisons were enrolled. To have a comparison group, prison staff were also asked to take part. Altogether, 1,553 of the 4,894 inmates from seven prisons completed a questionnaire on risk behaviors. According to the survey, 1.5%, 4.9%, and 0.04% of the prisoners were tested positive for HBsAg, anti-HCV and anti-HIV, respectively. These prevalence data are among the lowest reported from prisons worldwide, although comparable to the Central European data. The prevalence of HBV, HCV, and HIV in the Hungarian prison staff was low (0.38%, 0.47%, and 0%, respectively). The rate of HCV infection was significantly higher among inmates who have ever injected drugs (22.5%) than among inmates who reported they had never injected drugs (1.1%). This first prevalence study of illegal drug injection-related viral infections among Hungarian prisoners points out that ever injecting drugs is the main reason for HCV infection among inmates. The opportunity to reach drug users infected with HCV for treatment underlines the importance of screening programs for blood-borne viruses in prisons.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Throughout the world, hepatitis B virus (HBV), hepatitis C virus (HCV), and human immunodeficiency virus (HIV) infections are considered a major healthcare problem. People carrying blood-borne hepatitis viruses are at risk of developing liver cirrhosis and liver cancer.1 , 2 HBV, HCV, and HIV are transmitted most efficiently by percutaneous exposure to infectious blood. Since donated blood is tested for these viruses, high proportion of the new infections are associated with injecting drug use or other risk behaviors, such as tattooing, unprotected sexual contact (especially men having sex with men), piercing, and malpractice in the healthcare system.3 – 7 The number of active injection drug users in the European Union (EU) was estimated to be about 750,000–1 million (0.26%) in 2008.8 This estimate must be regarded with caution as it is based upon data available from only 12 of the 27 EU Member States and Norway, with the exclusion of Estonia. The number of those who have ever injected drugs must be higher,9 but data are not available for most of the countries.8 We know very little about the number of the active injection drug users in Hungary. The number of active opiate users is estimated to be around 3,500 people (0.05% of the Hungarian population aged 18–64).10 Estimated number of injection drug users is around 6,000 people (0.08% of the Hungarian population aged 18–64).11 The prevalence of HIV among at-risk populations is low in most of the Central European countries.11 , 12 The anti-HCV prevalence was reported around 35% in the Czech Republic, 46% in Croatia, and 76% in Warsaw, Poland among injecting drug users (IDUs).12 – 14 HBsAg prevalence was reported 0.8% in Croatia and 12% in Warsaw, Poland among IDUs.12 , 14 In Hungary, the seroprevalence of HCV in IDUs is high (22.6%), while seroprevalence of HIV (0%) and HBV(0.5%) is not higher than in the general population.15
Among high-risk environments, prisons are well-known settings for the spread of blood-borne viruses. Those who use illicit drugs or engage in sex work are often incarcerated. In addition, during imprisonment, prisoners often engage in unprotected sex, syringe/needle sharing, or sharing of other paraphernalia (spoon, water) because of the limited access to condoms and injecting equipment, etc.16 , 17 Tattooing and scarification are also common.18 Investigations carried out in correctional facilities around the world have shown a high prevalence of blood-borne hepatitis viruses and HIV.16 , 19 – 26 Only few studies were found that assessed the prevalence of these infections in prisons of Central Europe.27 – 29
Therefore, the aim of this study was to determine the prevalence of selected drug use-related viral infections among Hungarian inmates and prison staff, to examine related risk behaviors in order to identify the risk factors, and to offer the possibility of treatment according to national treatment protocols.
Methods
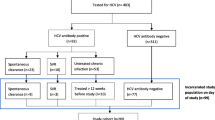
A national, multicenter, cross-sectional study was conducted between June 2007 and June 2009 in 20 Hungarian prisons, which geographically covered the entire country. The target groups of the study received a short explanation on the purpose of the study before the enrollment. Participation was voluntary. Out of a total of 14,331 inmates in the prison system at that time, 4,894 (34.2%) participated in this study of whom 9.2% were women. The percentage of female inmates in the total prison population was 6.7%. In order to have a comparison group, prison staff was also asked to take part in the survey voluntarily. A total of 1,066 (13.4% of the total prison staff) staff members were enrolled, of whom 52.2% were women. The age of the participants (inmates and prison staff) ranged between 21 and 60 years.
Venous blood samples were collected from each participant and centrifuged, and sera were kept at −20°C until analysis. Commercially available enzyme-linked immunosorbent assay (ELISA) kits were used in accordance with the manufacturers’ instructions. For the detection of HBsAg, Hepanostika HBsAg Ultra and Confirmatory tests (Biomerieux) were used. For the detection of antibodies to hepatitis C virus, HCV Ab (Dia.Pro) was used. Results were confirmed by HCV Ab or HCV Inno-LIA (Innogenetics). The presence of HCV RNA in the samples was determined by using a nested polymerase chain reaction (PCR) method.30 Sera were screened for the presence of anti-HIV antibodies in addition to the HIV antigen p24 using the Vironostika HIV Uni-Form II Ag/Ab microelisa system (Biomerieux). Repeatedly reactive specimens were further assayed by Genscreen HIV 1/2 version 2 ELISA (BIO-RAD), Murex HIV Ag/Ab Combination test (Murex Biotech Limited), INNO-LIA HIV I/II Score line immunoassay (Innogenetics N.V.) and indirect immunofluorescence assay.
Risk Behavior-Related Questionnaires
After informed consent was obtained, anonymous questionnaires on risk behaviors relating to the transmission of HIV and hepatitis infections were filled in voluntarily by 1,553 participating inmates between June 2008 and June 2009 in seven prisons. The questionnaire was developed, based upon the recommendations of the European Monitoring Centre for Drugs and Drug Addiction,31 and it was recorded by using the self-administration technique. Each serological test result was linked to the participant’s corresponding questionnaire by an anonymous unique identification code. Detailed analysis was carried out on hepatitis C and hepatitis B infections and related associations. Contingency tables to describe breakdowns and chi-square test or Fisher’s exact test with corresponding p values were used to determine significant associations with HCV or HBV infections. The dependent variable was the laboratory confirmed HCV/HBV infection. In statistical analysis, a p value of <0.05 was considered significant.
Results
Results of Serologic Assays and PCR
Two inmates of the 4,894 prisoners were HIV-1 positive (0.04%) and no HIV infection was detected among the staff. The difference between the prisoners and staff was not significant. A total of 72 and 241 of the 4,894 prisoners were HBsAg and HCV antibody positive, resulting in an overall seroprevalence of 1.5% and 4.9%, respectively; and 74% of the anti-HCV positive persons were carrying HCV detected by PCR. Among the staff, the seroprevalence of HBsAg and anti-HCV was 0.4% and 0.5%, respectively. The difference between the prisoners and staff was significant for HBV (p = 0.005) and HCV (p < 0.001). Prevalence of HCV and HBsAg was varied by prison. The highest anti-HCV prevalence was found in the capital, Budapest, 10.8% (N = 777), and the lowest was 0% (N = 170) in a prison in the eastern part of Hungary. The highest and lowest HBsAg prevalence were measured in prisons in the countryside, 2.5% (N = 277) and 0% (N = 58), respectively.
Results of the Analysis of Risk Behavior-Related Questionnaires
Altogether, 1,553 inmates completed a questionnaire on risk behaviors. The mean age of the subsample of the prison population was 35.5 years (SD = 9.6; median, 34; range, 39), the mean period of current imprisonment were 2.7 years (SD = 2.2; median, 2; range, 26) and 85.8% of them were male. Overall, 49.6% had received tattoos prior to imprisonment and 14.3% had their last tattoos done while in prison. Out of the 1,553 participants, 35.6% (N = 553) reported using illicit drugs in some form at least once; and 37.8% (N = 209) of this group of 553 reported injecting drugs at least once in their lives. Altogether, 44% of the IDUs injected within 1 month, 18.7% injected within 1 year, 28.3% injected more than 1 year before imprisonment, and 8.6% reported injecting drugs in prison for the last time.
In this subsample (N = 1,553), no HIV cases were detected and 1.2% and 4.0% of the inmates tested positive for HBsAg and anti-HCV antibodies, respectively. In a univariate analysis, drug use, especially drug injecting but not non-injecting drug use, was significantly associated with testing positive for HCV. Unsafe sexual behavior, any tattooing, and tattooing during imprisonment did not show significant association with HCV infection. No association was found between the mean duration of present imprisonment and HCV infection. None of the aforementioned risk behaviors were associated significantly with HBV carrier state (Table 1). Univariate analysis among a subsample of those inmates that ever reported injecting drugs showed an association between HCV infection and ever syringe/needle sharing and injecting equipment sharing (Table 2).
Discussion
This is the first large-scale study of selected drug use-related infections in Hungarian prisons. We have found that the prevalence of anti-HCV (4.9%), HBsAg (1.5%), and HIV (0.04%) is higher among prisoners compared to prison staff, although significant difference was found only for HCV and HBV. Only one study was found from Central Europe that assessed the prevalence of all three viruses in prisons.27 The authors found that 12.5%, 1.3%, and 0.16% of the adult prisoners were positive for HCV, HBsAg, and HIV, respectively. Other studies also described low number of HIV positive inmates in Slovakia and Poland.28 , 29 Our results show lower HCV and HIV prevalence among the Hungarian inmates than reported for Croatian inmates,27 and are among the lowest prevalence data for HCV, HBsAg, and HIV ever reported from prisons in the world.22 – 27 , 32 – 38
As a supplemental analysis to better understand the results, we compared the prevalence data of the prison staff to the general population (unpublished data) as well. The staff did not differ significantly from the general population after the data were adjusted to age regarding HIV, HCV, and HBV infections, which suggests low occupation-related virus transmission in Hungary. Few publications reported prevalence data of prison staff, but most of them described higher prevalence of HIV, HCV, and HBV among prison officers than among the general population, indicative of occupation-related virus transmission.36 , 39 , 40
None of those who completed the questionnaire on risk behaviors tested positive for HIV in this study. Hungary as well as most of the Central European countries have a relatively low HIV prevalence.11 In Hungary, since 1985, only 22 HIV infections were detected in ever-injecting drug users (with no yearly increase of the rate); only 5 of these cases had not been acquired abroad (Dudás M. personal communication). There are several HIV prevention projects (governmental and nongovernmental) and the prevention has been working well so far. Regarding hepatitis B virus carrier state and risk behaviors, we found higher prevalence data among prisoners who had any tattooing (and slightly higher among inmates who reported unprotected sex or ever-injection drug use), but none of them were statistically significant. However, the low HBsAg prevalence and the small sample size may have masked possible differences. HBV vaccination program started at the age of 14 in 1995 in Hungary.41 Prevention of HBV infection through active immunization should be recommended for unvaccinated inmates.
Our results suggest that ever injecting drugs is the main reason for the elevated anti-HCV prevalence in Hungarian prisons, since HCV infection was the highest among prisoners, who had ever injected drugs (48 times higher compared to staff). Further, there was no significant difference between staff and inmates who had never used drugs; and staff and prisoners admitted non-injecting drug use ever. Although 13.5% of the prisoners self-admitted injection drug use ever, the rate of injecting drugs in prisons was low (estimated to be about 9% of ever IDUs) on the basis of the present study and other national surveys carried out recently.15 We also found a lack of association between years of present imprisonment and HCV infection. These observations underline our suggestion that the entrants to prisons are already infected, similarly to other publications that reported high prevalence of blood-borne viruses even among entrants to prisons.19 , 42 It is not surprising that the highest HCV positivity was found among inmates in Budapest, since HCV infection rates in IDUs are four times higher in Budapest than outside of Budapest.15
We also examined two drug injection-related risk behaviors, such as ever sharing syringes/needles or injecting equipment, and found that both were significantly associated with testing positive for HCV. Fortunately, injection drug use is not common in Hungarian prisons. However, prison could be a suitable setting for conducting education programs on drug-related issues, client-centered prevention counseling, and tailored discussion of risk behaviors.
Although we had a great number of participants, we must note the following limitations. Since drug use is illegal, it is possible that some drug users chose to hide their history of drug use despite the clear explanation before enrollment that answers would be anonymous. This possibility may cause an underestimation of the number of drug users and may influence the prevalence data of the infectious diseases. Questionnaire data collection started a year later and only in selected prisons. We did not find significant difference between the whole examined inmate population and the subsample regarding HCV prevalence, which suggests no important selection bias. Questionnaires were filled out by using the self-administration technique which may result in incorrect answers by misunderstanding some questions.
After our screening, measures were initiated for the provision of care and treatment for the infected prisoners if their status met the criteria for antiviral therapy. Antiviral therapy was started in 60.1% of the HCV PCR-positive prisoners. As the analysis indicated, most of the HCV-infected inmates were IDUs. IDUs outside the prison system are not likely to undergo antiviral treatment due to various reasons (lack of necessary abstinence, lack of health insurance, lack of knowledge about the diseases, and other barriers). Abstinence from illicit drug use is mandatory to undergo treatment in Hungary. Prisons are closed settings, where IDUs are less likely to use drugs. Thus, prisons provide an effective environment to treat HCV-infected individuals. These persons could hardly be otherwise reached and referred to treatment to prevent the transmission of HCV to others. The current law in Hungary provides health care for those who are incarcerated; thus, there is no such obstacle to treatment as in certain other countries.42 , 43 Identification of undiagnosed infected persons and commencement of antiviral treatment should be part of the screening process when an inmate is admitted to a prison.
References
Beasley RP, Hwang LY, Lin CC, Chien CS. Hepatocellular carcinoma and hepatitis B virus. A prospective study of 22,707 men in Taiwan. Lancet. 1981;2:1129-1133.
Castello G, Scala S, Palmieri G, Curley SA, Izzo F. HCV-related hepatocellular carcinoma: from chronic inflammation to cancer. Clin Immunol. 2010;134:237-250.
Lauer GM, Walker BD. Hepatitis C virus infection. N Engl J Med. 2001;345:41-52.
MacDonald M, Crofts N, Kaldor J. Transmission of hepatitis C virus: rates, routes, and cofactors. Epidemiol Rev. 1996;18:137-148.
Holmberg SD. Molecular epidemiology of health care-associated transmission of hepatitis B and C viruses. Clin Liver Dis. 2010;14:37-48.
Rauch A, Rickenbach M, Weber R, et al. Unsafe sex and increased incidence of hepatitis C virus infection among HIV-infected men who have sex with men: the Swiss HIV Cohort Study. Clin Infect Dis. 2005;41:395-402.
Dencs A, Farkas A, Gyugos M, et al. Phylogenetic analysis of a nosocomial transmission of hepatitis B virus at a paediatric haematology ward. Acta Microbiol Immunol Hung. 2011;58:23-29.
EMCDDA (2010) Annual report on the state of the drugs problem in Europe. EMCDDA, Lisbon, November 2010. http://www.emcdda.europa.eu/publications/annual-report/2010. Accessed 3 May 2011.
Sweeting M, De Angelis D, Ades A, Hickman M. Estimating the prevalence of ex-injecting drug use in the population. Stat Methods Med Res. 2009;18:381-395.
Bozsonyi K, Csesztregi T, Dudás M, et al. National Report to the EMCDDA by the Reitox National Focal Point. 2010. http://www.drogfokuszpont.hu/dfp_docs/?id=nr_10_en.pdf. Accessed 3 May 2011.
EuroHIV. HIV/AIDS Surveillance in Europe: Mid-year report 2007. Saint-Maurice, France: Institut de Veille Sanitaire; 2007. No. 76. http://www.ecdc.europa.eu/en/activities/surveillance/hiv/Documents/report_eurohiv_midyear_2007.pdf. Accessed 5 May 2011.
Kolari B, Stajduhar D, Gajnik D, Rukavina T, Wiessing L. Seroprevalence of blood-borne infections and population sizes estimates in a population of injecting drug users in Croatia. Cent Eur J Public Health. 2010;18:104-109.
Zabransky T, Mravcik V, Korcisova B, Rehak V. Hepatitis C virus infection among injecting drug users in the Czech Republic—prevalence and associated factors. Eur Addict Res. 2006;12:151-160.
Laskus T, Radkowski M, Lupa E, et al. Prevalence of markers of hepatotropic viruses among drug addicts in Warsaw, Poland. J Hepatol. 1992;15:114-117.
Cserszegi T, Csohán Á, Elekes Zs, et al. National Report to the EMCDDA by the Reitox National Focal Point. 2009. http://www.drogfokuszpont.hu/dfp_docs/?id=nr_09_en.pdf. Accessed 5 May 2011.
Allwright S, Bradley F, Long J, Barry J, Thornton L, Parry JV. Prevalence of antibodies to hepatitis B, hepatitis C, and HIV and risk factors in Irish prisoners: results of a national cross-sectional survey. BMJ. 2000;321:78-82.
Stark K, Bienzle U, Vonk R, Guggenmoos-Holzmann I. History of syringe sharing in prison and risk of hepatitis B virus, hepatitis C virus, and human immunodeficiency virus infection among injecting drug users in Berlin. Int J Epidemiol. 1997;26:1359-1366.
Hellard ME, Aitken CK, Hocking JS. Tattooing in prisons—not such a pretty picture. Am J Infect Control. 2007;35:477-480.
Long J, Allwright S, Barry J, et al. Prevalence of antibodies to hepatitis B, hepatitis C, and HIV and risk factors in entrants to Irish prisons: a national cross-sectional survey. BMJ. 2001;323:1209-1213.
Horne JA, Clements AJ, Drennan P, Stein K, Cramp ME. Screening for hepatitis C virus in the Dartmoor prison population: an observational study. J Public Health (Oxf). 2004;26:372-375.
Hennessey KA, Kim AA, Griffin V, Collins NT, Weinbaum CM, Sabin K. Prevalence of infection with hepatitis B and C viruses and co-infection with HIV in three jails: a case for viral hepatitis prevention in jails in the United States. J Urban Health. 2009;86:93-105.
Massad E, Rozman M, Azevedo RS, et al. Seroprevalence of HIV, HCV and syphilis in Brazilian prisoners: preponderance of parenteral transmission. Eur J Epidemiol. 1999;15:439-445.
Weild AR, Gill ON, Bennett D, Livingstone SJ, Parry JV, Curran L. Prevalence of HIV, hepatitis B, and hepatitis C antibodies in prisoners in England and Wales: a national survey. Commun Dis Public Health. 2000;3:121-126.
Babudieri S, Longo B, Sarmati L, et al. Correlates of HIV, HBV, and HCV infections in a prison inmate population: results from a multicentre study in Italy. J Med Virol. 2005;76:311-317.
Meyer MF, Wedemeyer H, Monazahian M, Dreesman J, Manns MP, Lehmann M. Prevalence of hepatitis C in a German prison for young men in relation to country of birth. Epidemiol Infect. 2007;135:274-280.
Mahfoud Z, Kassak K, Kreidieh K, Shamra S, Ramia S. Prevalence of antibodies to human immunodeficiency virus (HIV), hepatitis B and hepatitis C and risk factors in prisoners in Lebanon. J Infect Dev Ctries. 2010;4:144-149.
Burek V, Horvat J, Butorac K, Mikulic R. Viral hepatitis B, C and HIV infection in Croatian prisons. Epidemiol Infect. 2010;138:1610-1620.
Staneková D, Ondrejka D, Habeková M, Wimmerová S, Kucerková S. Pilot study of risk behaviour, voluntary HIV counselling and HIV antibody testing from saliva among inmates of prisons in Slovakia. Cent Eur J Public Health. 2001;9:87-90.
Caban J, Dolezal M, Błach A, Wiśniowski Z. Detection of HIV antibodies among prisoners from penitentiary units within the district penal institutions in Cracow. Przegl Epidemiol. 1990;44:155-159.
Khan N, Aswad S, Shidban H, et al. Improved detection of HCV Infection in hemodialysis patients using a new HCV RNA qualitative assay: experience of a transplant center. J Clin Virol. 2004;30:175-182.
Wiessing L, Klempova D, Taylor C et al (2006) Protocol for the implementation of the EMCDDA key indicator: drug-related infectious diseases (DRID), draft version 6 October 2006, Project CT.04.P1.337 EMCDDA, Lisbon. http://www.emcdda.europa.eu/html.cfm/index65537EN.html. Accessed 5 March 2010.
Macalino GE, Vlahov D, Sanford-Colby S, et al. Prevalence and incidence of HIV, hepatitis B virus, and hepatitis C virus infections among males in Rhode Island prisons [Erratum in: Am J Public Health. 2004;94:1847]. Am J Public Health. 2004;94:1218-1223.
Kazi AM, Shah SA, Jenkins CA, Shepherd BE, Vermund SH. Risk factors and prevalence of tuberculosis, human immunodeficiency virus, syphilis, hepatitis B virus, and hepatitis C virus among prisoners in Pakistan. Int J Infect Dis. 2010;14:e60-e66.
Hammett TM, Harmon MP, Rhodes W. The burden of infectious disease among inmates of and releasees from US correctional facilities, 1997. Am J Public Health. 2002;92:1789-1794.
Christensen PB, Krarup HB, Niesters HG, Norder H, Georgsen J. Prevalence and incidence of bloodborne viral infections among Danish prisoners. Eur J Epidemiol. 2000;16:1043-1049.
Adjei AA, Armah HB, Gbagbo F, et al. Correlates of HIV, HBV, HCV and syphilis infections among prison inmates and officers in Ghana: a national multicenter study. BMC Infect Dis. 2008;8:33.
Saiz de la Hoya P, Bedia M, Murcia J, Cebria J, Sanchez-Paya J, Portilla J. Predictive markers of HIV and HCV infection and co-infection among inmates in a Spanish prison. Enferm Infecc Microbiol Clin. 2005;23:53-57.
Hammett TM. HIV/AIDS and other infectious diseases among correctional inmates: transmission, burden, and an appropriate response. Am J Public Health. 2006;96:974-978.
Adjei AA, Armah HB, Gbagbo F, et al. Prevalence of human immunodeficiency virus, hepatitis B virus, hepatitis C virus and syphilis among prison inmates and officers at Nsawam and Accra, Ghana. J Med Microbiol. 2006;55:593-597.
Chiaramonte M, Trivello R, Renzulli G, et al. Hepatitis B virus infection in prisons. A seroepidemiological survey in prisoners and attending staff. J Hyg (Lond). 1982;89:53-58.
Szomor KN, Dencs A, Garai E, Rusvai E, Berencsi G, Takacs M. Mutation spectra of the surface-protein-coding region of the HBV genome in HBV-vaccinated and non-vaccinated individuals in Hungary. Arch Virol. 2008;153:1885-1892.
Solomon L, Flynn C, Muck K, Vertefeuille J. Prevalence of HIV, syphilis, hepatitis B, and hepatitis C among entrants to Maryland correctional facilities. J Urban Health. 2004;81:25-37.
Kheirandish P, SeyedAlinaghi S, Jahani M, et al. Prevalence and correlates of hepatitis C infection among male injection drug users in detention, Tehran, Iran. J Urban Health. 2009;86:902-908.
Acknowledgments
This work was supported by Schering-Plough Hungary Ltd. (anti-HCV), the Hungarian Prison Service HQ, the Office of the Chief Medical Officer, and the National Center for Epidemiology (HBsAg and anti-HIV). The authors thank the staff of the Department of Hepatitis Viruses and Molecular Virology for the excellent technical assistance. We are grateful to Prof. Eva Gonczol and Carolyn Otterness for critical reading of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tresó, B., Barcsay, E., Tarján, A. et al. Prevalence and Correlates of HCV, HVB, and HIV Infection among Prison Inmates and Staff, Hungary. J Urban Health 89, 108–116 (2012). https://doi.org/10.1007/s11524-011-9626-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11524-011-9626-x