Abstract
Resistance to apoptosis is one of the hallmarks of cancer and members of the B-cell lymphoma 2 (BCL-2) family of proteins are central regulators of apoptosis. Many cancers become resistant to chemotherapy and apoptosis by up-regulating BCL-2 and other family members, making these proteins attractive targets for cancer therapy. Venetoclax is an orally administered, small-molecule apoptosis stimulant that targets BCL-2 proteins by acting as a BCL-2 homology domain 3 (BH3) mimetic. The drug is approved in the USA and EU as a monotherapy for the for the treatment of certain patients with chronic lymphocytic leukemia (CLL) and is in phase III clinical development for multiple myeloma (MM), and in phase II or I/II clinical trials for acute myeloid leukemia, and several B-cell malignancies, including diffuse large B-cell lymphoma, Waldenstrom's macroglobulinaemia, follicular lymphoma, and mantle-cell lymphoma.
Similar content being viewed by others
Avoid common mistakes on your manuscript.

1 The Role of the BCL-2 Pathway in Hematologic Malignancies
Resistance to apoptosis is one of the hallmarks of cancer cell biology and contributes to chemotherapy resistance. The relevance of B-cell lymphoma 2 (BCL-2) proteins in cell death and survival has been well described and includes both external and internally initiated pathways of cell death. In fact, the BCL-2 protein, encoded on chromosome 18, was the first anti-apoptotic protein described and was discovered as a chromosomal fusion product with the immunoglobulin heavy chain machinery, t(14;18) in follicular lymphoma (FL) in 1985 [1]. Since then, our understanding of the BCL-2 gene family has evolved and more than 20 proteins that impact the balance between cell survival and death have been described.
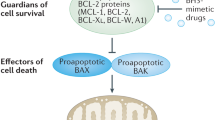
While the extrinsic pathway of apoptosis is "switched on" with the binding of ligands to cell-surface death receptors, the intrinsic pathway of apoptosis is initiated by various different stimuli, including DNA damage and oxidative stress. The BCL-2 family proteins help facilitate the intrinsic pathway of apoptosis by causing mitochondrial depolarization and ultimately caspase-mediated cell death. BCL-2 family proteins are divided into three categories, based on both structure and function (Fig. 1). The anti-apoptotic proteins BCL-2, BCL-XL, myeloid cell leukemia 1 (MCL-1), BCL-W, and A1 contain four conserved BCL-2 homology (BH) domains and are antagonistic to pro-apoptotic BCL-2 family proteins. The latter share a BH3 structural homology, and are therefore referred to as BH3-only proteins, which include BID, BIM, BAD, PUMA, and NOXA. The cell death mediators, BCL-2 antagonist killer (BAK) and BCL-2-associated X protein (BAX), are inhibited by the binding of anti-apoptotic BCL-2 family proteins and can be directly activated or sensitized by the interaction of other BCL-2 family members.
The BCL-2 protein family [2]. a Pro-survival or anti-apoptotic proteins have 4 BCL-2 homology (BH) domains. The apoptosis sensitizers are BH3-only proteins. b Apoptosis sensitizers bind to the hydrophobic groove of pro-survival proteins and are sequestered. When BH3 mimetics, such as venetoclax bind to BCL-2, BIM is displaced and can then interact with the mitochondrial membrane, activating caspase release and cell death.
While the t(14;18) is a hallmark of FL, it is also found in a proportion of diffuse large B-cell lymphoma (DLBCL) cases. Both the activated B-cell subtype (ABC) and germinal center (GC) subtype DLBCL can show BCL-2 overexpression, though the mechanism by which this occurs differs in each. The t(14;18) only occurs in the GC subtype and often this is the cause of BCL-2 overexpression, whereas in the ABC subtype, BCL-2 overexpression may be the result of transcriptional activation, including NFκB effects, or copy number gains. Through either overexpression or dysregulation of BCL-2, there is a net increase in its anti-apoptotic functions, resulting in resistance to apoptosis. The role of BCL-2-related chemotherapy resistance has been described across the spectrum of hematologic malignancies including MM, myelodysplastic syndrome (MDS), acute myeloid leukemia (AML), acute lymphoid leukemia (ALL), DLBCL, mantle cell lymphoma (MCL), FL, and notably chronic lymphoid leukemia (CLL), which has demonstrated remarkable sensitivity to BCL-2 antagonists. Despite the high rate of BCL-2 overexpression in FL, there has not been a proportionate efficacy with single-agent BCL-2 inhibitors.
Herein, we review the development of BCL-2 inhibitors in hematologic malignancies, with an emphasis in the successes achieved in CLL and B-cell lymphomas.
2 BCL-2 Inhibition in CLL
CLL cells effectively evade apoptosis by overproduction of BCL-2. In CLL cells, pro-apoptotic BCL-2 family proteins such as BIM are sequestered by binding to BCL-2 [3]. Due to the high expression of BIM, CLL cells are thought to be “primed” for apoptosis by BCL-2 inhibitor proteins. Small molecule inhibitors of BCL-2 can displace BIM from the BH3-binding pocket of BCL-2, allowing BIM to activate BAX and thereby induce mitochondrial membrane permeability and cell death.
Functionally, BCL-2 inhibitors are BH3 mimetics. Several small molecule inhibitors of BCL-2 have been developed and although they demonstrated activity in CLL cell lines, there were significant limitations preventing clinical utility of the early agents. ABT-737, the first anti-BCL-2 agent that was developed by Abbott, was found to inhibit BCL-2, BCL-XL, and BCL-W [4]. Cancer cell lines and xenograft models of lymphoma demonstrated regression and death when exposed to ABT-737 [5]. ABT-737 is not an orally bioavailable compound and its further development was limited by unfavorable pharmacologic properties. Subsequently, ABT-263 or navitoclax, which is orally bioavailable, demonstrated significant activity in early phase clinical trials; however, off-target binding to BCL-XL, which is highly expressed in platelet precursors, was the putative cause of thrombocytopenia, a significant dose-limiting toxicity [6, 7].
Obatoclax was a pan-BCL-2 inhibitor in development by Teva. There was no significant single-agent activity in hematologic malignancies and combined with a toxicity profile that included dizziness, somnolence, and ataxia, the development of the non-specific BCL-2 agent was halted [8].
Oblimersen is an anti-sense RNA that targets the start codon of BCL-2 mRNA. This was a promising therapy for B-cell malignancies and melanoma, but due to the lack of robust efficacy in either disease, FDA approval was not obtained, and drug development has stagnated.
The third compound in Abbott’s series of BCL-2 inhibitors, venetoclax (Venclexta™, formerly ABT-199, GDC-0199) is orally bioavailable and selectively binds BCL-2 with a more than 100–fold higher affinity compared to other BCL-2 family members, such as BCL-XL, thereby resulting in an improved toxicity profile. Venetoclax is the first BCL-2 inhibitor to be FDA-approved and impressive responses have been seen in some hematologic malignancies thus far, prompting further evaluations with combination strategies.
Venetoclax is approved by the FDA for CLL patients that harbor a del(17p) and have received at least one prior therapy. The European approval is for the treatment of CLL in the presence of del(17p) or TP53 mutation in adult patients who are unsuitable for or have failed a B-cell receptor pathway inhibitor, and for the treatment of CLL in the absence of del(17p) or TP53 mutation patients who have failed both chemoimmunotherapy and a B-cell receptor pathway inhibitor.
The loss of functional p53, which is harbored on the short arm of chromosome 17, results in chemo-refractory CLL, with poor prognosis and shortened response durations to novel agents such as ibrutinib or idelalisib. The finding of del(17p) or TP53 loss of function mutations, precludes use of chemotherapy and in the relapsed setting, represents a high unmet need in CLL. The FDA-approved indications for venetoclax are expected to eventually include all relapsed CLL patients. The current National Comprehensive Cancer Network (NCCN) guidelines for CLL recommend venetoclax use for treatment of all CLL patients with relapsed/refractory (RR) disease, regardless of 17p status and with or without rituximab [9]. Therefore, the agent is being used in clinical practice, beyond the scope of the narrower FDA-supported label. Currently, single-agent venetoclax is offered as an indefinite therapeutic to RR CLL patients; however, combinations with targeted therapies and immunotherapies have resulted in higher rates of minimal residual disease (MRD) clearance and offer the possibility of finite therapy. Thus far, only the combination of rituximab and venetoclax has been reported in a phase III evaluation, the MURANO trial, supporting its use in the RR setting, as a truncated treatment strategy. The main clinical concerns with venetoclax administration include tumor lysis syndrome (TLS) risk and hematologic toxicities.
Herein, we review the results of single-agent venetoclax trials and novel combination strategies with venetoclax.
2.1 Venetoclax in CLL Monotherapy
Chemo-immunotherapy had been the mainstay of CLL treatment for decades. Recently, the introduction of several small molecule inhibitors has resulted in a paradigm shift in the treatment of many CLL patients. Chemo-immunotherapy is still considered to be the optimal approach for younger fit patients, who do not harbor del(17p), and who have no other negative prognostic markers that would portend short response durations, such as seen in IgVH unmutated CLL patients, who should not receive fludarabine, cyclophosphamide, and rituximab (FCR). With the introduction of B-cell receptor (BCR) kinase inhibitors, ibrutinib and idelalisib, the treatment landscape for patients with RR CLL, as well as for first-line treatment of patients with del(17p) has been transformed. Nevertheless, resistance as well as intolerance to the side effects of these therapies is proving to be a rising challenge. There is a growing need for alternative agents with non-redundant mechanisms of action.
BCL-2 is overexpressed in CLL as a result of hypomethylation of the BCL-2 gene. Furthermore, negative regulators of BCL-2 expression, miRNA-15 and miRNA-16, which are encoded on 13q14, are deleted in a majority of CLL [10].
The initial venetoclax studies in CLL were conducted in patients with RR disease and there were some instances of rapid debulking and resultant TLS, causing the death of some patients. Due to these unforeseen events, the dosing schedule of the drug was changed, significantly mitigating the risk of clinical TLS. The phase I study of 56 patients with RR CLL and SLL was a dose escalation study followed by an expansion cohort of 60 patients that demonstrated impressive response rates in patients with chemo-refractory disease, regardless of the presence of del(17p) [11]. In the dose-escalation phase, there were 10/56 patients with TLS and 3/56 patients that developed clinical TLS, with 2 requiring dialysis for renal failure and 1 resultant death. Protocol modifications were made, incorporating a slower dose ramp-up to the goal dose of 400 mg. This prevented clinical TLS events in the expansion cohort. However, due to the risk of TLS, the package insert for venetoclax includes a risk stratification schema for TLS and management suggestions, based on the presence of a relatively high circulating lymphocyte count (>25,000) or the presence of bulky nodal disease (>5 cm). The maximum tolerated dose (MTD) was not reached in this study and the 15-month progression-free survival (PFS) estimate was 69% with an objective response rate (ORR) of 79% (92/116), including 20% complete responses (CRs). Of these, eight patients (5%) had no detectable MRD. The median PFS in patients with del(17p) was 16 months. Of the 41 patients who progressed while on treatment, there were 14 patients who had a Richter transformation (RT). The most common grade 3-4 adverse events (AEs) included neutropenia (41%), anemia (12%), and thrombocytopenia (12%).
Another phase II evaluation of 107 CLL patients with RR disease and del(17p) demonstrated a similarly impressive ORR of 85% at a median follow-up of 12 months with 8 patients (8%) achieving a CR [12]. The median PFS was not reached at the 12-months median follow-up time. TP53 mutations were detected in 60/107 patients (72%). The dose ramp-up to 400 mg was conducted over 4–5 weeks and no clinical TLS occurred. The most common grade 3-4 AEs reported included neutropenia (40%), anemia (18%), thrombocytopenia (15%), and infection (20%). Autoimmune hemolytic anemia was seen in 7% of patients and the mechanism of this toxicity is not well understood. Laboratory TLS occurred in five patients. Of the 107 patients treated, 37 discontinued therapy, with 22 patients having progression of disease, including 11 RT. There were a total of 14 deaths as a result of disease progression and 4 were non-treatment-related. These results, published by Stilgenbauer et al., led to the accelerated approval of venetoclax for patients with RR CLL and harboring del(17p). The presence of del(17p) is relatively uncommon, varying from 7% to as high as 30–50% in patients with multiple relapsed disease [13, 14].
With the recent introduction of several novel therapies in the CLL armamentarium, the question of how to best sequence these therapies arises. Jones et al. [15] presented their results of venetoclax therapy in patients with CLL who relapsed or were refractory to treatment with either ibrutinib or idelalisib. There were 39 patients refractory to ibrutinib who were treated with venetoclax for a median of 13 months and showed an impressive ORR of 70% in this small cohort. There were 21 patients with prior idelalisib therapy treated for a median duration of 9 months, and these patients had an ORR of 48%, as assessed by an independent review committee (IRC). While there were very few CRs seen, there were also very few progressions. This trial suggests that the sequencing of targeted therapies is safe and treatment with venetoclax after progression on other small molecule inhibitors is a feasible and effective option.
A notable outcome in the results seen in venetoclax trials is the finding of MRD negativity in a proportion of patients who also achieve a CR. The utility of MRD negativity to predict long-term outcome following chemo-immunotherapy has been well-described [16]. The eradication of all detectable clones with the use of small molecule inhibitors is uncommon. Currently, most small molecule inhibitors are dosed indefinitely, as long as responses continue to be seen and toxicities are not prohibitive, with re-emergence of disease off therapy. The depth of response achieved with venetoclax and the durability of the response with combination therapies (see below) raises the possibility that truncated therapy may be feasible in some patients and the duration of PFS prolonged. Consensus definitions of MRD are lacking. Methodologies (PCR vs. flow cytometry), thresholds of detection, and even assignment of MRD to patients who have less than a CR make interpretation across studies challenging.
2.2 Venetoclax in CLL Combinations
The addition of rituximab to venetoclax showed synergy in preclinical models and led to the evaluation of the combination in early phase clinical studies, with the goal of deepening the responses seen with single-agent venetoclax. The first published results of a combination study of venetoclax were those of a phase Ib trial with rituximab in 49 patients with a median follow-up of 28 months [17]. Rituximab was given monthly for six cycles and venetoclax was administered as a ramp-up over 4 weeks and then given daily. The MTD of venetoclax was not reached and the phase 2 dose was determined as 400 mg. The ORR was 86 % (42/49) with an impressive CR rate achieved in 51% (25/49) of patients. There was a negative bone marrow MRD in 80% of those who achieved a CR (20/25). Clinical TLS occurred in two patients, resulting in one patient death. With protocol amendments, slower dose ramp-up of venetoclax, and enhancing TLS monitoring and prophylaxic measures, there were no further clinical TLS events. The AE profile of the combination was similar to that seen with single-agent venetoclax and overall was deemed to be safe. There were 11 patients who had progression while on therapy and 5 of these represented an RT. PET/CT scans were not performed as a part of mandatory evaluation for the trial and all of the RT patients progressed within 9 months on study. The deep responses seen with the combination supported ongoing studies.
There have been a number of combination studies with immunotherapy and chemo-immunotherapies with early results presented at national meetings (Table 1). The CLL14 study is a phase III, German-led trial comparing venetoclax/obinutuzumab with venetoclax/chlorambucil in previously untreated CLL patients with a coexisting medical conditions score (CIRS) score ≥6.[24] . Obinutuzumab was administered for 6 cycles and venetoclax was given for 12 cycles. The ORR at 3 months after therapy completion was 100% (11/11) with CRs having been achieved in 78% (7/12) of patients. At final staging, five of seven available bone marrow aspirates showed clearance of MRD. There were two laboratory TLS events and no clinical TLS. The combination was found to be well-tolerated. This phase III study has completed accrual, and the highly anticipated full results are pending.
Stilgenbauer et al. reported their interim results of a phase Ib combination of bendamustine/rituximab or bendamustine/obinutuzumab with venetoclax in untreated as well as RR CLL patients [22]. Fifty-five patients were treated and no DLT or TLS were reported in this study. At early time points, the vast majority of patients had demonstrated responses and the safely profiles of the chemo-immunotherapy arms were comparable. After 6 months of combination therapy, RR patients may continue single-agent venetoclax until unacceptable toxicity or disease progression, and treatment-naïve patients can have one year of venetoclax in total.
The combination of venetoclax and obinutuzumab in 32 treatment-naïve patients was also presented at American Society of Hematology (ASH) 2017 [25]. Patients received a 6-month treatment course with the combination, followed by 6 months of single-agent venetoclax. There were two dosing schemas, with venetoclax preceding obinutuzumab in one schema and in the second, obinutuzumab was introduced before venetoclax. Continued therapy with venetoclax was offered to patients who achieved a PR or had detectable MRD. The median time on study was 11.3 (10–23) mos. All patients cleared MRD from the peripheral blood and 14/32 cleared MRD from the bone marrow (62.5%). The MRD negativity rate is impressive and, at a minimum, appears to be non-inferior to chemotherapy-containing regimens. A phase III study is planned based on these results.
More recently, at the 2017 ASH meeting in Atlanta, the much-anticipated results of the phase III MURANO trial were presented [18]. This was a randomized trial comparing the combination of bendamustine with rituximab (BR) to venetoclax and rituximab (VR), and represents the first results of a head-to-head comparison of a standard chemotherapy regimen with a regimen containing targeted agents in CLL. A total of 398 patients who had been treated with one to three lines of prior therapies were enrolled and randomized 1:1 to either VR or BR (194 VR and 195 BR). The VR regimen included rituximab given at 375 mg/m2 for the first dose and then 500 mg/m2 monthly for a total of 6 cycles, and venetoclax, ramped up over either 4 or 5 weeks, to a goal of 400 mg daily and continued for 2 years for responders. The BR regimen included bendamustine at 70 mg/m2 given on days 1 and 2 and with rituximab, as described with VR. Importantly, patients were stratified according to del(17p) status and responsiveness to prior therapy. The primary endpoint was investigator-assessed PFS, which was found to be superior for VR vs. BR (HR 0.17, 95% CI 0.11–0.25, P < 0.0001; median not reached vs. 17.0 mo). CRs were achieved in a larger proportion of patients treated with VR versus BR as assessed by investigators (26.8 versus 8.2%, P < 0.0001). Key toxicities included a low frequency of TLS events, especially in patients treated with VR. There was one clinical TLS event seen in each of the two arms. There were higher rates of grade 3-4 neutropenia in the VR arm, though no increased rates of grade 3-4 infection. The MURANO trial demonstrated impressive responses in RR CLL, including MRD negativity, echoing results previously seen in phase I and II studies of single-agent venetoclax. The finding of p53 derangements would be another predictor of inferior responses to chemo-immunotherapies and, despite this, a significant proportion of patients (48 and 51 for VR and BR, respectively) harbored this poor prognostic feature and were treated with BR. Nevertheless, the significant degree of MRD clearance with the VR regimen was impressive and the results support the combination of venetoclax with rituximab as a therapeutic option for some patients with highly refractory CLL. It is noteworthy that the investigator assessment of CRs (negative CT and negative bone marrow) vastly differed from the independent review assessments of CR, with the IRC finding much fewer CRs achieved due to differences in CT scan interpretation. After the initial 6 months of treatment, the PFS curves for the 2 regimens began to separate greatly and the PFS of VR-treated patients at 24 months remains over 80%. Truncated therapy with venetoclax is not a standard for R/R CLL patients, though the combination with rituximab may be very effective for selected patients. Once patients stopped venetoclax therapy, there was a sustained benefit reflected in the majority of patients who remained on study, with only a slight decrement from the responses achieved while on treatment. Because this was an abstract presentation, some very important details regarding CR/MRD were not presented, but will be highly anticipated in a full manuscript. The time to MRD negativity in the experimental arm and the ability of MRD to predict sustained control will be highly relevant for understanding which patients may have a planned treatment-free interval and which will require ongoing daily venetoclax treatment. In addition to p53 dysfunction, key disease features, such as complex karyotype and molecular alternations in NOTCH 1 and SF3B, amongst others, may be very important predictors of success with abbreviated therapy. In current practice, ibrutinib, an oral BTK inhibitor, is used most frequently by US practitioners to treat R/R CLL, with venetoclax often considered after ibrutinib failure. The sequencing of therapy may shift towards earlier VR usage, with the potential to offer truncated therapy, with FDA approval of venetoclax for all RR CLL patients. The results thus far support the use of VR for RR CLL patients regardless of 17p deletion.
A dual targeted therapy combination of ibrutinib and venetoclax has shown promising results in early evaluations. The CLARITY Study was designed as a feasibility study to determine the safety and efficacy of the combination of ibrutinib and venetoclax in RR CLL [19]. Higher-risk patients were considered for enrollment and included patients who relapsed within 3 years of treatment with FCR or BR, 20% had del(17p), 25% had del(11q), and 74% had unmutated VH genes. Fifty patients were enrolled in the study. The median age at enrolment was 64 years. Bulky disease (lymph nodes ≥ 5 cm) was reported in 8% of patients. After an 8-week lead-in of ibrutinib monotherapy (420 mg/day), venetoclax dosing was ramped up, from a starting dose of 10 mg/day, with weekly escalations to a final dose of 400 mg/day. The primary endpoint of the study was MRD clearance. Venetoclax and ibrutinib were stopped at 14 months, if bone marrow biopsy at 8 months was MRD-negative, and at 26 months if MRD negativity was achieved by month 14 of treatment. Ibrutinib monotherapy then continued if there was MRD positivity at 26 months. A single case of TLS, managed by delaying venetoclax, was seen as increasing phosphate and creatinine at a venetoclax dose of 200 mg. The venetoclax dose was rapidly re-escalated with no further event. Thirty-eight patients reached month 8 of therapy and all showed a response (100% ORR), with 39% (15/38) achieving a CR and 8% (3/38) achieving a complete remission with incomplete bone marrow recovery (CRi). Of patients receiving prior FCR or BR, all patients showed a response (100% ORR), with 53% (9/17) achieving a CR and 12% (2/17) achieving a CRi. Thirty-eight patients had MRD determinations at 8 months, having received venetoclax and ibrutinib for 6 months: 84% (32/38) of patients showed no morphological evidence of CLL in marrow biopsy; 37% (16/38) and 32% (12/38) of patients achieved MRD negativity in peripheral blood and the bone marrow, respectively. Based on these data, the UK phase III FLAIR trial has been modified to include the combination of ibrutinib and venetoclax in front-line CLL. Other arms include ibrutinib alone and FCR in patients with previously untreated CLL.
Another evaluation of the combination of ibrutinib and venetoclax in both treatment-naïve (cohort 1) and RR (cohort 2) patients showed similarly promising results [20]. The primary endpoint was achievement of CR. Treatment-naïve patients were required to have one negative prognostic feature, including del(17p), mutated TP53, del(11q), unmutated IGHV, or ≥65 yrs. Ibrutinib was given for 3 months, followed by the addition of venetoclax for a 2-year interval. Ibrutinib could then be continued indefinitely. The median follow-up time at reporting was 7.5 (0.6–12.1) months. Of 16 patients who received at least 3 months of combination therapy, there were 9 CR/CRi and 7 PRs. The most common reasons for dose reductions were neutropenia and 24% of patients required a dose reduction in ibrutinib and 18% in venetoclax dosage.
Interim results of the combination of ibrutinib and venetoclax, with the monoclonal antibody obinutuzumab, were presented [28]. Venetoclax was administered in a 3 + 3 dose escalation and there were no DLTs encountered; therefore, 400 mg of venetoclax was concluded to be the appropriate dose in this combination. While this was a small study, there was one patient who had a CR that also had negative MRD, an encouraging outcome for two small molecule inhibitors that have demonstrated synergy in preclinical models and clinical evaluations thus far [29, 30].
The schema for an innovative trial incorporating a maintenance stratification based on MRD after induction was recently presented [21]. In this ongoing phase Ib/II study, patients with high risk by fluorescence in situ hybridization (FISH) are treated with 6 months of an induction strategy with ibrutinib, rituximab, and prednisone. With the finding of MRD negatively after induction, patients can go on to receive ibrutinib maintenance and those with a detectable CLL clone will be treated with ibrutinib and venetoclax.
Overall, combination strategies had similar toxicity profiles as compared with single-agent venetoclax, with higher rates of MRD negativity reported, supporting continued efforts at combining therapies with a goal of finite-duration treatment.
3 Venetoclax in Non-Hodgkin Lymphoma
While venetoclax has demonstrated exceptional efficacy in CLL, there has been variable activity across other subtypes of non-Hodgkin lymphoma (NHL, Table 2). As previously discussed, the majority (85%) of FL harbor the t(14;18), which results in overexpression of BCL-2. Neither protein expression nor the presence of the BCL-2 translocation has been shown to be a biomarker of sensitivity to venetoclax. This speaks to the complex interplay of other BH3 family members, including MCL1, which may be a dominant anti-apoptotic protein in some hematologic malignancies.
The M12-175 phase I study evaluated 106 patients with a range of NHLs, including FL, DLBCL, MCL, and RT [31]. The overall response rate was 44%, with significant variability in sensitivities by subtype, as follows: MCL, 75%; FL, 38%; DLBCL, 18%, and estimated median PFS in months, by subtype: MCL 14; FL 11; DLBCL 1. The PFS for all patients (N = 106) in the study was estimated to be 6 months (95% CI, 4 to 10 mos). The majority of patients were deemed “high expressers” of BCL-2, which was defined as >50% expression of immunohistochemistry (IHC) 2+ or 3+. The level of BCL-2 expression by IHC was not predictive of response or TLS risk, again demonstrating that the balance between pro-apoptotic and anti-apoptotic factors is complex and not simply reflected in the amount of BCL-2 detected across histologies. The responses seen in MCL patients were among the highest and parallel the high responses seen with the first-in-class BTK inhibitor, ibrutinib, in MCL [34]. Venetoclax administration was felt to be safe, with few laboratory TLS events and no clinical TLS seen. Of five DLBCL patients with sufficient tissue specimens for molecular analysis, four patients had GC and one had the ABC subtype.
The CAVALLI study is a phase I evaluation of venetoclax/chemo-immunotherapy combinations, including venetoclax + R-CHOP and venetoclax + G-CHOP [33]. Patients with ≤1 prior therapies across subtypes of NHL were included. While R-CHOP or G-CHOP were given for six cycles, venetoclax was administered discontinuously over eight cycles. The recommended phase 2 dose (RP2D) for venetoclax + R-CHOP was reported as 800 mg on days 4–10 of cycle 1 and days 1–10 of cycles 2 through 8. Based on the results of the trial, a phase 2 evaluation in frontline DLBCL is ongoing. For the combination of venetoclax + G-CHOP, dose finding was ongoing due to thrombocytopenia. ”Double expressers” are defined by co-expression of MYC and BCL-2 or BCL-6 proteins by IHC. Of the 8 DLBCL patients that were double expressers, the ORR was 7/8 (87.5%) and progression occurred in 1/8 (12.5%). The median follow-up for patients who achieved at least a CR or PR at the end of treatment was 11 months.
“Double-hit” and “triple-hit” lymphomas are characterized by the presence of a myc translocation in combination with either a bcl2 or bcl6 translocation and define a more aggressive DLBCL subtype with high rates of relapse. These subtypes are described in the 2016 World Health Organization (WHO) document as a new classification of “high grade B-cell lymphoma with translocations involving myc and BCL-2 or BCL-6” [35]. Cases of DLBCL with high expression of MYC and BCL-2 define another subtype, “double expresser”, which bears an intermediate prognosis between “double hit” and DLBCL. There are ongoing evaluations of venetoclax with chemoimmunotherapy including R-CHOP and R-EPOCH for patients with DLBCL, who are double hit and double expressers, including an ongoing phase I ALLIANCE study with dose-adjusted R-EPOCH and venetoclax dosed at 800 mg daily. Additionally, the combination of venetoclax with dose-adjusted R-EPOCH is being evaluated in patients with Richter syndrome, which represents a highly chemo-refractory DLBCL that has transformed from CLL.
BR is considered to be a standard chemo-immunotherapy backbone for patients with indolent lymphomas, including patients with FL. Patients often relapse after chemo-immunotherapy regimens and those patients who relapse within 2 years have a particularly poor overall survival [36]. Given the overexpression of BCL-2 in FL, and activity of the agent in this disease subtype, there is a rationale to combine a BCL-2 inhibitor with chemo-immunotherapy strategies. Interim results of the CONTRALTO study, a randomized study comparing a chemoimmunotherapy combination arm with a chemotherapy-free arm in patients with relapsed/refractory FL, were presented at ASH 2016 [32]. Patients in the chemotherapy-containing arm were randomized to BR versus BR plus venetoclax. There were a total of 164 patients enrolled and the primary endpoint was CR by PET/CT scan. There were 53 patients in the chemotherapy-free arm of venetoclax plus rituximab and 111 patients treated with a chemotherapy-containing regimen including 51 in the venetoclax-plus-BR arm and 51 with BR alone. There were nine patients enrolled in a run-in phase. Reponses in the combination venetoclax-with-chemotherapy arm were slightly better (ORR 68%, CR 50%) as compared with BR alone (ORR 64%, CR 41%), and far exceeded VR alone (ORR 33%, CR 14%), albeit at the cost of greater toxicity. There were five deaths in the study, with four occurring in a venetoclax-containing arm (colitis, pulmonary hemorrhage, pneumonia, and PD) and one death due to PD in the BR arm.
Given the improved responses seen with a combination of a bendamustine-containing backbone with venetoclax, the Eastern Cooperative Oncology Group (ECOG) Lymphoma Working Group is conducting a phase II study across 10 academic centers evaluating the combination of venetoclax with bendamustine and obinutuzumab in patients with untreated FL. Following a 6-month induction with V+B+O, patients will be stratified to one of two maintenance arms depending on their response. Those who achieve a CR will have a 2-year maintenance with O planned and those who have a PR or SD will have dual-therapy maintenance with V+O.
MCL represents 6% of all NHL histologies and has a highly variable clinical course, with some younger patients benefiting from high-dose chemotherapy and transplant and other MCL patients managed with low-dose strategies, with no impact on survival, similar to an indolent lymphoma. There has been impressive single-agent activity seen in RR MCL patients, as previously outlined, and evaluation of combination strategies suggests similarly high response rates. Synergy between 2 targeted agents was seen in a phase 2 combination of venetoclax + ibrutinib in 23 RR MCL cases, with 560 mg of ibrutinib introduced for 4 weeks of therapy, followed by ramp-up of venetoclax to the daily dose of 400 mg [37]. One third of the patients had failed prior autologous stem cell transplant. At 16 weeks, the ORR was 71%, with 63% having achieved a CR. The combination was well-tolerated and the most common adverse events were fatigue, diarrhea, and nausea. This is a combination that will likely be evaluated in phase III studies.
4 Venetoclax in Myeloid Malignancies
A third of acute myeloid leukemia (AML) patients over the age of 75 receive palliative strategies due to co-morbidities that would prohibit intensive strategies in the setting of highly resistant disease after relapse [38]. The development and introduction of novel therapies with improved toxicity profiles in this patient population represents a high unmet need. With the successful development of targeted therapies in the treatment of lymphoid malignancies, there has been cross-pollination into therapeutic strategies for myeloid diseases, for which clinical trials offer the best strategy in the relapsed setting. The administration of single-agent venetoclax in relapsed AML and MDS has resulted in clinical responses in some patients. In a single-arm phase II study, single-agent venetoclax was administered to 32 patients with RR AML, and the ORR was 19% [39]. A biomarker for response to therapy, a BCL-2 sensitivity index was calculated retrospectively, defined as the ratio of BCL-2-to-BCL-XL and patients with a higher ratio had more durable responses to therapy as compared with those who had lower sensitivity scores.
The combination of venetoclax with either hypomethylating agents (HMAs) or low-dose cytarabine was evaluated in 43 RR AML patients [40]. There were objective responses observed in 9 (21%) patients and 2 had CRs and 3 CRis, with a median survival of 3 months. An open-label phase IB evaluation of venetoclax with decitabine or azacitadine in previously untreated patients with AML, over the age of 65, showed impressive responses [41]. Thirty-five of 67 (61%) patients achieved a CR or CRi and the recommended phase 2 venetoclax dose of 400 mg or 800 mg, interrupted, is being evaluated in phase II studies, with both hypomethylating agents. Given the early efficacy signals in AML, the FDA has granted venetoclax a break-through designation, for use in combination with hypomethylating agents in patients deemed ineligible for more intensive treatment strategies.
5 Venetoclax in Multiple Myeloma
MM is characterized by a relapsing course that necessitates introduction of novel therapies with alternative mechanisms of action. Venetoclax has demonstrated activity in early-phase studies and appears to have efficacy in MM that harbors t(11;14), thought to be due to the relatively higher expression of BCL-2, compared with BCL-XL or MCL-1 [42, 43]. Kumar et al. evaluated venetoclax up to doses of 1200 mg in previously treated MM patients, who had received a median of 5 prior therapies, and reported on the safety and tolerability of the relatively higher dose [43]. The observation that higher MCL-1 expression leads to treatment resistance and correlates with reduced efficacy of venetoclax prompted combination studies with bortezomib, which has been shown to reduce MCL-1 levels in xenograft models of MM [44]. In a phase I study of the combination of bortezomib with venetoclax and dexamethasone, in 66 patients treated with a median of 3 prior therapies, the ORR was 44/66 (67%), with 42% having achieved a very good partial response, or better (≥VGPR) [45]. In patients who were not refractory to bortezomib, the ORR was 97% and 73% ≥VGPR. There was a correlation between bcl2 gene expression and efficacy of the combination, with an ORR of 94% and 59% in high expressers and low expressers, respectively. These impressive results have led to a phase III trial of the triplet regimen in MM. Evaluation of combination strategies in MM are ongoing and with the recognition of biomarkers predicting response to the BCL-2 inhibitor, it may be possible to select MM patients who are likely to benefit from these strategies.
6 Next-Generation BCL-2 inhibitors
With BH3 mimetic profiling of hematologic malignancies it has been increasingly apparent that resistance to specific BCL-2 inhibitors may be due to the dominant effects of other BH3 protein members. Given the marked success of venetoclax in some hematologic subtypes, there has been a strong impetus to develop BCL-2 inhibitors with greater activity and agents that target more than one contributor to apoptosis resistance. The agents outlined in Table 3 highlight some of the compounds in development in hematologic and solid malignancies.
7 Conclusions
Venetoclax has been the first highly successful BCL-2 inhibitor to be used as a cancer therapeutic and has paved the way for other inhibitors of BCL-2 family proteins, as well as combination strategies with both novel agents and traditional chemotherapy. Thus far, impressive activity has been demonstrated in CLL, MCL, and MM, with less robust single-agent activity seen in FL and DLBCL. The reliance on BCL-2 for survival has been demonstrated across hematologic malignancies, including highly treatment-refractory diseases such as AML. The variability in responses to venetoclax across malignancies underscores the relevance of biomarkers for sensitivity to BCL-2 inhibition, and investigation of the complex interplay of BCL-2 proteins in evasion of cell death. “Dynamic BH3 profiling” (DBP) is one potential method of interrogation of apoptotic pathways in living patients’ cells, and may yield valuable insight into the mechanisms by which malignant cells are resistant to specific inhibitors of BCL-2, despite overexpression of the BCL-2 protein [46]. Very well tolerated overall, venetoclax has some important safety concerns; however, with appropriate risk stratification and management, TLS risk can be reduced. Demonstration of MRD negativity is one of the most promising aspects of therapy with the BCL-2 inhibitor in CLL and raises expectations for highly effective, truncated strategies, heralding a shift away from indefinite treatment with targeted agents in some patients.
References
Tsujimoto Y, Cossman J, Jaffe E, et al. Involvement of the bcl-2 gene in human follicular lymphoma. Science. 1985;228:1440–3.
Merino D, Lok SW, Visvader JE, et al. Targeting BCL-2 to enhance vulnerability to therapy in estrogen receptor-positive breast cancer. Oncogene. 2016;35:1877–87.
Del Gaizo MV, Brown JR, Certo M, et al. Chronic lymphocytic leukemia requires BCL2 to sequester prodeath BIM, explaining sensitivity to BCL2 antagonist ABT-737. J Clin Invest. 2007;117:112–21.
Oltersdorf T, Elmore SW, Shoemaker AR, et al. An inhibitor of Bcl-2 family proteins induces regression of solid tumours. Nature. 2005;435:677–81.
Hauck P, Chao BH, Litz J, et al. Alterations in the Noxa/Mcl-1 axis determine sensitivity of small cell lung cancer to the BH3 mimetic ABT-737. Mol Cancer Ther. 2009;8:883–92.
Kaefer A, Yang J, Noertersheuser P, et al. Mechanism-based pharmacokinetic/pharmacodynamic meta-analysis of navitoclax (ABT-263) induced thrombocytopenia. Cancer Chemother Pharmacol. 2014;74:593–602.
Rudin CM, Hann CL, Garon EB, et al. Phase II study of single-agent navitoclax (ABT-263) and biomarker correlates in patients with relapsed small cell lung cancer. Clin Cancer Res. 2012;18:3163–9.
Goard CA, Schimmer AD. An evidence-based review of obatoclax mesylate in the treatment of hematological malignancies. Core Evid. 2013;8:15–26.
Wierda WG, Zelenetz AD, Gordon LI, et al. NCCN Guidelines Insights: Chronic Lymphocytic Leukemia/Small Lymphocytic Leukemia, Version 1.2017. J Natl Compr Canc Netw. 2017;15:293–311.
Hanada M, Delia D. Aiello A, et al: bcl-2 gene hypomethylation and high-level expression in B-cell chronic lymphocytic leukemia. Blood. 1993;82:1820–8.
Roberts AW, Davids MS, Pagel JM, et al. Targeting BCL2 with Venetoclax in Relapsed Chronic Lymphocytic Leukemia. N Engl J Med. 2016;374:311–22.
Stilgenbauer S, Eichhorst B, Schetelig J, et al. Venetoclax in relapsed or refractory chronic lymphocytic leukaemia with 17p deletion: a multicentre, open-label, phase 2 study. Lancet Oncol. 2016;17:768–78.
Lozanski G, Heerema NA, Flinn IW, et al. Alemtuzumab is an effective therapy for chronic lymphocytic leukemia with p53 mutations and deletions. Blood. 2004;103:3278–81.
Stilgenbauer S, Zenz T, Winkler D, et al. Subcutaneous Alemtuzumab in Fludarabine-Refractory Chronic Lymphocytic Leukemia: Clinical Results and Prognostic Marker Analyses From the CLL2H Study of the German Chronic Lymphocytic Leukemia Study Group. J Clin Oncol. 2009;27:3994–4001.
Jones J, Choi MY, Mato AR, et al. Venetoclax (VEN) Monotherapy for Patients with Chronic Lymphocytic Leukemia (CLL) Who Relapsed after or Were Refractory to Ibrutinib or Idelalisib. Blood. 2016;128:637.
Kovacs G, Robrecht S, Fink AM, et al. Minimal Residual Disease Assessment Improves Prediction of Outcome in Patients With Chronic Lymphocytic Leukemia (CLL) Who Achieve Partial Response: Comprehensive Analysis of Two Phase III Studies of the German CLL Study Group. J Clin Oncol. 2016;34(31):3758–65.
Seymour JF, Ma S, Brander DM, et al. Venetoclax plus rituximab in relapsed or refractory chronic lymphocytic leukaemia: a phase 1b study. Lancet Oncol. 2017;18:230–40.
Seymour JF, Kipps TJ, Eichhorst BF, et al. Venetoclax Plus Rituximab Is Superior to Bendamustine Plus Rituximab in Patients with Relapsed/ Refractory Chronic Lymphocytic Leukemia - Results from Pre-Planned Interim Analysis of the Randomized Phase 3 Murano Study. Blood. 2017;130:LBA-2.
Hillmen P, Munir T, Rawstron A, et al. Initial Results of Ibrutinib Plus Venetoclax in Relapsed, Refractory CLL (Bloodwise TAP CLARITY Study): High Rates of Overall Response, Complete Remission and MRD Eradication after 6 Months of Combination Therapy. Blood. 2017;130:428.
Jain N, Thompson PA, Ferrajoli A, et al. Combined Venetoclax and Ibrutinib for Patients with Previously Untreated High-Risk CLL, and Relapsed/Refractory CLL: A Phase II Trial. Blood. 2017;130:429.
Park S, Davis L, Hsu P, et al. Phase II/1b Trial of Ibrutinib Plus Prednisone and Rituximab Induction Followed By Venetoclax Plus Ibrutinib Maintenance in Newly Diagnosed High-Risk Chronic Lymphocytic Leukemia. Blood. 2017;130:5351.
Stilgenbauer S, Morschhauser F, Wendtner C-M, et al. Phase Ib Study (GO28440) of Venetoclax with Bendamustine/Rituximab or Bendamustine/Obinutuzumab in Patients with Relapsed/Refractory or Previously Untreated Chronic Lymphocytic Leukemia. Blood. 2016;128:4393.
Salles GA, Boyd TE, Morschhauser F, et al. Updated Safety and Preliminary Efficacy Data from a Phase 1b Study Combining Venetoclax (GDC-0199, ABT-199) with Bendamustine/Rituximab in Patients with Relapsed/Refractory or Previously Untreated Chronic Lymphocytic Leukemia. Blood. 2015;126:4.
Fischer K, Al-Sawaf O, Fink AM, et al. Venetoclax and obinutuzumab in chronic lymphocytic leukemia. Blood. 2017;129:2702–5.
Flinn IW, Gribben JG, Dyer MJS, et al. Safety, Efficacy and MRD Negativity of a Combination of Venetoclax and Obinutuzumab in Patients with Previously Untreated Chronic Lymphocytic Leukemia - Results from a Phase 1b Study (GP28331). Blood. 2017;130:430.
Flinn IW, Brunvand M, Choi MY, et al. Safety and Efficacy of a Combination of Venetoclax (GDC-0199/ABT-199) and Obinutuzumab in Patients with Relapsed/Refractory or Previously Untreated Chronic Lymphocytic Leukemia - Results from a Phase 1b Study (GP28331). Blood. 2015;126:494.
Rogers KA, Huang Y, Stark A, et al. Initial Results of the Phase 2 Treatment Naive Cohort in a Phase 1b/2 Study of Obinutuzumab, Ibrutinib, and Venetoclax in Chronic Lymphocytic Leukemia. Blood. 2017;130:431.
Jones JA, Woyach J, Awan FT, et al. Phase 1b Results of a Phase 1b/2 Study of Obinutuzmab, Ibrutinib, and Venetoclax in Relapsed/Refractory Chronic Lymphocytic Leukemia (CLL). Blood. 2016;128:639.
Deng J, Isik E, Fernandes SM, et al. Ibrutinib Therapy Increases BCL-2 Dependence and Enhances Sensitivity to Venetoclax in CLL. Blood. 2015;126:490.
Jayappa KD, Portell CA, Gordon V, et al. Ligands That Mimic the Tissue Microenvironment of Replicating Chronic Lymphocytic Leukemia (CLL) and Mantle Cell Lymphoma (MCL) Protect Ex Vivo Patient Cell Samples from the Cytotoxicity of Combined Treatment with Ibrutinib and Venetoclax (ABT-1 99). Blood. 2015;126:448.
Davids MS, Roberts AW, Seymour JF, et al. Phase I First-in-Human Study of Venetoclax in Patients with Relapsed or Refractory Non-Hodgkin Lymphoma. J Clin Oncol. 2017;35:826–33.
Zinzani PL, Topp MS, Yuen SL, et al. Phase 2 Study of Venetoclax Plus Rituximab or Randomized Ven Plus Bendamustine+Rituximab (BR) Versus BR in Patients with Relapsed/Refractory Follicular Lymphoma: Interim Data. Blood. 2016;128:617.
Zelenetz AD, Salles GA, Mason KD, et al. Results of a Phase Ib Study of Venetoclax Plus R- or G-CHOP in Patients with B-Cell Non-Hodgkin Lymphoma. Blood. 2016;128:–3032.
Advani RH, Buggy JJ, Sharman JP, et al. Bruton tyrosine kinase inhibitor ibrutinib (PCI-32765) has significant activity in patients with relapsed/refractory B-cell malignancies. J Clin Oncol. 2013;31:88–94.
Swerdlow SH, Campo E, Pileri SA, et al. The 2016 revision of the World Health Organization classification of lymphoid neoplasms. Blood. 2016;127:2375–90.
Casulo C, Byrtek M, Dawson KL, et al. Early Relapse of Follicular Lymphoma After Rituximab Plus Cyclophosphamide, Doxorubicin, Vincristine, and Prednisone Defines Patients at High Risk for Death: An Analysis From the National LymphoCare Study. J Clin Oncol. 2015;33:2516–22.
Tam CSL, Roberts AW, Anderson MA, et al. Combination ibrutinib (Ibr) and venetoclax (Ven) for the treatment of mantle cell lymphoma (MCL): Primary endpoint assessment of the phase 2 AIM study. J Clin Oncol. 2017;35:7520.
Medeiros BC, Satram-Hoang S, Hurst D, et al. Big data analysis of treatment patterns and outcomes among elderly acute myeloid leukemia patients in the United States. Ann Hematol. 2015;94:1127–38.
Konopleva M, Pollyea DA, Potluri J, et al. Efficacy and Biological Correlates of Response in a Phase II Study of Venetoclax Monotherapy in Patients with Acute Myelogenous Leukemia. Cancer Discovery. 2016;6:1106–17.
DiNardo CD, Rausch CR, Benton C, et al. Clinical experience with the BCL2-inhibitor venetoclax in combination therapy for relapsed and refractory acute myeloid leukemia and related myeloid malignancies. Am J Hematol. 2018;93(3):401–7.
DiNardo CD, Pratz KW, Letai A, et al. Safety and preliminary efficacy of venetoclax with decitabine or azacitidine in elderly patients with previously untreated acute myeloid leukaemia: a non-randomised, open-label, phase 1b study. Lancet Oncol. 2018;19(2):216–28.
Punnoose EA, Leverson JD, Peale F, et al. Expression Profile of BCL-2, BCL-XL, and MCL-1 Predicts Pharmacological Response to the BCL-2 Selective Antagonist Venetoclax in Multiple Myeloma Models. Mol Cancer Ther. 2016;15:1132–44.
Kumar S, Kaufman JL, Gasparetto C, et al. Efficacy of venetoclax as targeted therapy for relapsed/refractory t(11;14) multiple myeloma. Blood. 2017;130:2401–9.
Edwards SK, Han Y, Liu Y, et al. Signaling mechanisms of bortezomib in TRAF3-deficient mouse B lymphoma and human multiple myeloma cells. Leuk Res. 2016;41:85–95.
Moreau P, Chanan-Khan A, Roberts AW, et al. Promising efficacy and acceptable safety of venetoclax plus bortezomib and dexamethasone in relapsed/refractory MM. Blood. 2017;130:2392–400.
Montero J, Sarosiek KA, DeAngelo JD, et al. Drug-induced death signaling strategy rapidly predicts cancer response to chemotherapy. Cell. 2015;160:977–89.
Funding
No specific funding for the preparation of this manuscript was received.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Kahl has consulted for Abbvie and Pharamcyclics. Dr. Khan has consulted for Gilead and Abbvie.
Rights and permissions
About this article
Cite this article
Khan, N., Kahl, B. Targeting BCL-2 in Hematologic Malignancies. Targ Oncol 13, 257–267 (2018). https://doi.org/10.1007/s11523-018-0560-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11523-018-0560-7