Abstract
One of the most effective multiple sclerosis (MS) treatment is natalizumab. Nevertheless, it has been associated with an increased risk of progressive multifocal leukoencephalopathy (PML) caused by the JC virus (JCV). Our main objective was to assess the utility of testing JCV-DNA, apart from anti-JCV antibodies, to determine which natalizumab-treated MS patients has been previously in contact with the virus. For this purpose, 138 MS natalizumab/non-natalizumab treated patients participated in several studies. Cross-sectional study (CS): association of several epidemiological variables with anti-JCV antibodies and JCV-DNA levels in PBMC/serum/urine. First longitudinal study (A): evaluation of JCV-DNA prevalence in urine throughout the treatment. Second longitudinal study (B): simultaneous assessment of antibodies and viral DNA levels in PBMC/serum/urine at two time points. CS: The seropositivity rate for anti-JCV antibodies (62.3 %) and JCV prevalence in urine (59.4 %) were similar; although 26 % of our population was positive only using one of the two techniques. A: The viral prevalence in urine seemed to increase between the baseline visit and the others (Baseline-Visit/V18months, p = 0.006). B: Our rate of positive antibody seroconversion was 36 %. Nearly all patients with detectable JCV-DNA levels in PBMC excreted the virus intermittently in urine; while our PML case, positive in PBMC and serum samples 2 month before the PML, excreted JCV permanently. In conclusion, the determination of JCV DNA levels in urine could be complementary to anti-JCV antibodies for identifying MS patients who has been infected by the JCV. Further research would be necessary to understand the different JCV excretion profiles in urine.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Natalizumab (Tysabri, Biogen Idec) is a humanized monoclonal antibody directed against the α4-subunit of α4β1 and α4β7 integrins for the treatment of highly active relapsing-remitting multiple sclerosis (RRMS). It is characterized for its high efficacy for the MS treatment, but it has been associated with an increased risk of progressive multifocal leukoencephalopathy (PML), a devastating demyelinating disease caused by the human polyomavirus JC (Major 2010).
A prerequisite for the development of this pathology is a previous contact with the JC virus (JCV), and one of the methods for detecting this virus is by assessing the anti-JCV antibodies through immunoassays. The incidence of these antibodies varied between 35 % (Knowles et al. 2003) and 91 % (Matos et al. 2010) among some of the published works. However, recent studies used a new two-step immunoassay (two-step ELISA) that allowed the stratification of patients according to the higher or lower risk of developing PML (Gorelik et al. 2010). This original two-step ELISA has been improved with the second generation two-step ELISA, although the results obtained with both techniques are comparable due to the high agreement between them (Lee et al. 2013). Another methodology would be the viral DNA detection using qPCR in blood, serum, plasma and/or urine; whose clinical relevance has been suggested by certain authors (Chen et al. 2009) but not by others (Rudick et al. 2010; Sadiq et al. 2010; Jilek et al. 2010).
Thus, apart from positive status with respect to anti-JCV antibodies, the risk of PML in MS patients has been quantified according to the presence of other two risk factors: the prior use of immunosuppressants and the increasing duration of natalizumab treatment. Thus, the estimated incidence in the highest risk of PML group (patients positive for anti-JCV antibodies, had taken immunosuppressants before the initiation of natalizumab therapy, and had received 25 to 48 months of natalizumab) was 11.1 cases per 1,000 patients versus the 0.09 cases or less per 1,000 patients of the lowest risk (patients negative for antibodies) (Bloomgren et al. 2012). Another important issue concerning the risk of PML is the different immunological responses associated with JCV control depending on the patient. For example, MS patients with natalizumab-associated PML were distinguished from healthy donors and other natalizumab-treated MS patients in that they either had no detectable JCV-specific T cell response or had JCV-specific CD4 T cell responses uniquely dominated by IL-10 production (Perkins et al. 2012).
Our main purpose was to assess the utility of testing JCV-DNA with qPCR, apart from anti-JCV antibodies using two-ELISA, for the determination of MS patients with previous or recent contact with the JCV. Additionally, we studied the influence of different epidemiological variables (including gender, age, immunosuppressive pretreatment, and duration of natalizumab treatment) in these antibodies and DNA levels in a previously unexamined Spanish MS cohort.
Materials and methods
Patients
A total number of 149 patients diagnosed according to McDonalds’ criteria with MS at the MS reference center of the Hospital Clínico San Carlos of Madrid were included in this study, which was conducted from July 2010 to June 2012. All patients in our center with anti-JCV antibodies status (two-step ELISA), who were or were going to be treated with natalizumab, participated in our study. Eleven patients were excluded because the JCV DNA levels could not be measured at the same time as that of the anti-JCV-antibodies (Fig. 1). All of them signed informed consent to participate in this study, which was previously approved by the Ethical Committee of Clinical Investigation of the Hospital Clínico San Carlos.
Flow diagram of subjects participating in the cross-sectional study and the longitudinal studies (A: JCV DNA levels in urine throughout the natalizumab-treatment, and B: simultaneous evaluation of the anti-JCV antibody presence and the JCV DNA levels in PBMC/serum/urine at two different time points). Abbrevations: MS multiple sclerosis; NTZ natalizumab treated patients, non-NTZ non-natalizumab treated patients, * patients excluded because the JCV DNA levels could not be measured at the same time as the anti-JCV-antibodies; ** patients excluded because they did not have samples for participating in any longitudinal studies; ***patients excluded because they only had samples to participate in one of the longitudinal studies
Patient treatment and design of studies
Cross-sectional study
This retrospective observational study included 82 RRMS patients treated with natalizumab (59.4 %) and other 56 patients with interferon beta, glatiramer acetate, or no treatment; in this second group, all patients were RRMS except for two secondary progressive MS patients, SPMS (3.6 %). Patients received natalizumab at a dose of 300 mg by intravenous infusion every 4 weeks. Clinical characteristics of this population are available in Table 1.
Blood samples from these patients were sent to a reference laboratory (Unilabs, Denmark) in order to perform the STRATIFY JCVtm Test (two-step ELISA), as previously described by Gorelik et al. (2010), or the STRATIFY JCV™ DxSelect™ (2nd-generation two-step ELISA) for detecting JCV-specific antibodies (the anti-JCV antibody levels in the two-step ELISA were given in nOD450 and in the 2nd-generation two-step ELISA in index value). The 2nd-generation two-step ELISA was employed only with 17 non-natalizumab patients. Using qPCR, JCV DNA was assessed in peripheral blood mononuclear cells (PBMC), serum and urine samples extracted the same day as the blood for testing antibodies.
Longitudinal studies
-
Study A
JCV DNA levels in urine throughout the natalizumab-treatment
Sixty-five patients out of the 138 previous patients were included in this longitudinal retrospective study. We obtained their urine samples from the baseline visit (BV, without treatment) and the follow-up visits made every 3 months until the blood samples were sent to detect JCV-specific antibodies. Afterward, we detected the JCV DNA through qPCR.
-
Study B
simultaneous evaluation of anti-JCV antibodies presence and JCV DNA levels in PBMC/serum/urine at two different time points
Twenty-three out of 82 natalizumab-treated patients and 10 out of 56 non-treated patients from the cross-sectional study, had a second measurement of anti-JCV antibodies using Enhanced ELISA (STRATIFY JCV™ DxSelect™; “2nd-generation assay”) from Unilabs, after 11.8 ± 0.6 (11, 13) and 10.8 ± 1.4 (8, 12) months respectively from the first sample
swe sent to the laboratory. These patients had a second measurement of the antibodies because they were negative in the first one. All patients were treated with natalizumab during the second sample extraction, included the ten non-natalizumab-treated patients in the first one. The JCV DNA level was assessed in PBMC, serum and urine simultaneously to the detection of the anti-JCV antibodies.
PML case
One of these natalizumab-treated patients developed PML at month 46 of the treatment. The JCV DNA levels in PBMC, serum, and urine samples were tested quarterly throughout the natalizumab treatment and in the CSF (cerebrospinal fluid) at the moment of the PML diagnosis.
Samples and viral DNA detection
When necessary, the samples were stored frozen at −80 °C until analyzed. The isolation of the total DNA from PBMC, serum and urine samples was performed using the QIAamp DNA Blood Mini Kit, QIAamp Viral RNA Mini Kit and the QIAamp Ultrasense Virus Kit (QIAGEN, Hilden, Germany) respectively, according to the manufacturer’s protocol. The serum was previously ultracentrifuged at 350,000 × g for 15 min at 8 °C.
This DNA was analyzed in order to detect the late mRNA gene of JCV genome by a qPCR assay, as previously described (Watzinger et al. 2004), using a Corbett Research RotorGen 3000. The lower limit of detection was 4 copies/μg in PBMC, 17 copies/ml in serum and 14 copies/ml in urine. If only one of the duplicates of a sample was positive, we repeated the qPCR, considering as a positive result if at least one of these repeated duplicates was positive again. The final viral load values were the mean of the viral load values of the duplicates.
Statistics
Continuous variables were expressed as mean and standard deviation (minimum, maximum) or medians (25th and 75th percentile) and categorical variables as percentages. Categorical variables were compared using the χ 2 test, the values of the continuous ones between groups using the Mann–Whitney U test. The agreement between two categorical variables was assessed using Kappa index. McNemar test was used to study the relationship between two related paired categorical variables in the longitudinal study (viral prevalence between BV and the rest). We assessed if there was a difference among the values of a continuous variable throughout a longitudinal study using the Friedman test and between two of these values using Wilcoxon test; considering that after the logarithmic transformation of the non-parametric variables (viral load) they continued to be non-parametric. The non-parametric Spearman coefficient was applied in order to evaluate the correlation between two continuous variables. Subjects with missing data were omitted from the corresponding analyses. P-values <0.05 were referred to as statistically significant in the text. All analyses were performed using SPSS for Windows (Ver. 15.0) software (SPSS Inc.).
Results
Cross-sectional study
The rate of seropositivity measured with ELISA was 62.3 % (86/138) in the total population. The seroprevalence in women and men was similar and the frequency of anti-JCV antibodies did not change depending on the age of the patients or the period of time from MS diagnosis (Table 2). There was no correlation between the anti-JCV antibodies levels (nOD450) and age at the sample extraction (Spearman’s correlation test, r = 0.147, p = 0.114).
The JCV DNA in urine was detected in 59.4 % (76/128) of the whole population and was similar in both sexes. The JCV DNA in urine was not found with different frequency depending on the range of age, but we observed a low positive correlation between JC viral load and age (Spearman’s correlation test, r = 0.280, p = 0.001). The viral prevalence was similar in patient groups displaying different durations of MS; likewise the viral load did not change with longer periods of time from the MS diagnosis (Spearman’s correlation test, r = 0.377, p = 0.84). In 4 out of 6 MS patients previously treated with immunosuppressor (mitoxantrone or azathioprine) anti-JCV-antibodies were detected; however, the viral DNA was identified in only one out of those four patients.
The kappa index rate (0–1, from no to perfect agreement) used for comparing the agreement between the two techniques, ELISA and qPCR, was 0.41 (p = 4.1E*10-6). Likewise, this comparison allowed us to divide our population into 4 groups as shown in Fig. 2, where 26 % of patients had a different result depending on the technique used (12 % positive only with qPCR, plus 14 % positive only with two-step ELISA).
Besides, these results were grouped by the ELISA test employed (STRATIFY JCVtm Test: two-step ELISA, used in 87.8 % of our cross-sectional population; or the STRATIFY JCV™ DxSelect™: 2nd-generation two-step ELISA, used in the other 12.2 % of the population) (Table 3).
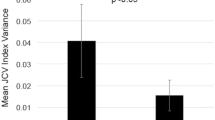
In the 114 patients analyzed with the two-step ELISA, we detected a correlation between anti-JCV antibody levels (nOD450,) and the JCV levels in urine (viral load) (Spearman’s correlation test, r = 0.705, p = 1.96*E-18). Similarly, in the 17 patients analyzed with the second generation two-step ELISA, the correlation between the anti-JCV antibodies levels (the index value) and the viral load in urine was nearly significant (Spearman’s correlation test, r = 0.533, p = 0.074). The viral load in urine of the 15 (12 %) patients who only tested positive with qPCR [2.6 (1.5, 3.5) log10 copies/ml] was significantly lower (Mann–Whitney U test, p = 0.0002) than the viral load of those 61 patients with the same positive result using both techniques [5 (3.2, 6.6) log10 copies/ml]. Similarly, the anti-JCV antibody levels of the 17 patients who only tested positive with the original two-step ELISA [0.22 (0.15, 0.35)] were significantly lower than the levels of those patients with the same positive result with qPCR and original two-step ELISA [0.7 (0.38, 0.97)] (Mann–Whitney U test, p = 8.96*E-5) (Fig. 3).
Comparison of the JC viral loads in urine (a) and the anti-JCV antibody levels (b) in patients with concordant or discordant DNA–antibody status. a Concordant, positive qPCR and two-step ELISA results (n = 61): 5 (3.2, 6.6) log10 copies/ml, and discordant, positive qPCR but negative two-step ELISA results (n = 15): 2.6 (1.5, 3.5) log10 copies/ml (Mann–Whitney U test, p = 0.0002). b Concordant, (n = 53): 0.7 (0.38, 0.97), and discordant, negative qPCR but positive original two-step ELISA (n = 17): 0.22 (0.15, 0.35) (Mann–Whitney U test, p = 8.96*E-5) (cross-sectional study)
There was no significant difference between the anti-JCV antibodies presence in natalizumab and non-natalizumab treated patients, nor between the JCV DNA prevalence in urine between these two groups (Fig. 4). The percentage of positive anti-JCV antibody patients among the non-natalizumab treated group were not different between patients analyzed with the second generation two-step ELISA, 12/17 (70.6 %), and the previous one, 19/39 (48.7 %) (χ2 test, p = 0.13).
Anti-JCV antibody presence and viral prevalence in urine in natalizumab and non-natalizumab treated patients did not vary as a function of the sex, age or duration of the illness (data not showed). There was no difference in natalizumab-treatment duration (months) between positive anti-JCV antibody patients and negative antibody patients, or between JCV prevalence in urine-positive and negative patients. The rate of positive anti-JCV antibody patients and the viral prevalence in urine was similar, regardless of whether patients had been treated with natalizumab (Table 2).
The anti-JCV antibody levels and the JCV DNA levels in urine, in PBMC and serum, were measured at the same time. There were 4 patients with detectable levels of viral DNA in PBMC, who had been treated with natalizumab for 3, 21, 33 and 36 months respectively at the moment of the sample collection; all of them were positive for anti-JCV antibodies at these moments of the treatment. We also detected JCV DNA in PBMC of 3 non-natalizumab treated patients, but only detected the anti-JCV antibodies in two of them at same point in time. None of these PBMC positive patients were treated previously with immunosuppressors and all of them were positive for JCV in the urine sample at the same point time that the PBMC sample was analyzed. JCV was not detected in serum samples of any of 138 patients who participated in this cross-sectional study.
Longitudinal studies
In the longitudinal study A the JCV DNA in urine was detected throughout the treatment - permanently (included BV) in 32.3 % (21/65) of the patients, never in 15.4 % (10/65) (neither in BV), and intermittently in 52.3 % (34/65). The viral load mean in the group with permanent viral excretion in urine (6.4 (5.5, 7) log 10 copies/ml) was significantly higher than this value in the intermittent group (2.3 (2, 2.8) log10 copies/ml) (Mann–Whitney U test, p = 2.5E*10-9).
We observed a significant increase of viral prevalence in urine between BV and the others starting at V12 (visit at month 12 of natalizumab treatment) until V30, except between BV and V21/V24 (e.g. McNemar test, p = 0.006 between BV prevalence, 52.3 %, and V18 prevalence, 68.1 %) (Table 4). We found a significant variation of viral load measured throughout the treatment, at the different time points (Friedman test, p = 0.00005). Similarly, we detected a significant difference when we compared the viral load at BV with the others, starting at V12, except between BV and V24.
On the other hand, approximately 1 year after the first evaluation in the cross-sectional study, the patients who were negative for the ELISA test, were re-evaluated for the JCV antibody presence. Thus, simultaneous evaluation of the anti-JCV antibodies presence and the JCV DNA levels in PBMC/serum/urine at two different time points was performed in 33 out of 138 total patients (study B). The rate of positive seroconversion was 36.4 % (12/33). Among the patients who seroconverted, 25 % (5/12) were positive by qPCR in the first measurement. The percentage of positive seroconversion in natalizumab-treated patients, 39.1 % (9/23), was not different from that of non-natalizumab treated patients, 30 % (3/10) (χ2 test, p = 0.616). Regarding the results of the qPCR at these two different time points of the study, the positive conversion rate in urine was 27.3 % (9/33) and the negative rate was 12.1 % (4/33). We did not find any difference between these rates in the natalizumab and the non-natalizumab patients at the first sample (positive rate: 27.3 % (6/22) vs 33.3 % (3/9), negative rate: 13.6 % (3/22) vs 11.1 % (1/9) p = 0.939). Among these 33 patients (study B), in the second measurement, one patient was positive in PBMC after 42 months with natalizumab, and two in serum after 42 and 8 months of treatment. These patients with detectable JCV DNA levels in serum samples also tested positive in their urine at this time of the treatment, but only one of them had detectable levels of anti-JCV antibody levels. The positive one in PBMC had detectable levels of anti-JCV antibody but he was not positive in urine.
Thus, we determined the JCV DNA levels in urine throughout the natalizumab-treatment (study A), and the presence of anti-JCV antibodies beside the JCV DNA levels in PBMC/serum/urine, at two different time points (study B) in 23 patients of our cohort. As we can see in Table 5, comparing the results of the two techniques in the two visits for antibodies (study B), we obtained the same results in 52.2 % (12/23) of the cases (10/23 patients remained negative with two-step ELISA and qPCR in both time points, more 2/23 patients who got positive with both techniques in the second measurement). Among the ten negative patients using the two techniques in both visits, only in one of them we detected viral DNA in urine in an intermittent way, and in the rest of them we could not detect it. All patients with different results in the longitudinal study B depending on the used technique exhibited detectable JCV DNA levels in urine intermittently since BV.
The JCV DNA levels in urine throughout the natalizumab-treatment were measured in five patients with detectable levels of JCV in PBMC; in four of these patients the virus was detected intermittently in the urine and in the other one permanently. One of the patients with detectable JCV levels in serum excreted this virus in urine intermittently, while in other patient the virus excretion could not be evaluated.
PML case
One of the patients developed PML after 46 months with natalizumab. He was a 54-year old man, diagnosed with RRMS 9 years ago and treated for 4 years with IFN beta 1-a and glatiramer acetate before starting with natalizumab. The JCV was detected in serum and PBMC using qPCR 2 months before the PML diagnosis, permanently in urine throughout the natalizumab treatment, and in CSF in the PML diagnosis. He was positive for anti-JCV antibodies at V30.
Discussion
Several factors have been proposed in order to stratify the risk of suffering from PML among the natalizumab-treated MS patients (e.g. duration of the treatment and the previous use of immunosuppressors). We assessed the utility of performing qPCR for the detection of JCV DNA in PBMC, serum and urine apart from testing for the anti-JCV antibodies in these patients. In addition, we studied the influence of different epidemiologic factors in these two parameters: anti-JCV antibodies and viral DNA levels in a Spanish cohort not previously studied.
In our cohort the rate of seropositivity for anti-JCV antibodies and viral prevalence in urine were similar, 62.3 % and 59.4 %, respectively. These levels did not seem to be different when we divided our population in natalizumab and non-natalizumab treated patients. When we compared our results with other previously published ones, we observed that our rate of seropositivity was similar to that of the natalizumab-treated patients cohort from Italy (52 %) (Laroni et al. 2012) and Germany (58.8 %) (Trampe et al. 2012), and it seemed be greater than those from other continents (Gorelik et al. 2010). Our viral prevalence in urine was greater than other previously published in healthy population (19 %) (Egli et al. 2009) or natalizumab treated patients (around 26 %) (Rudick et al. 2010); probably because our detection limit used through all the study was considerably lower than the other ones.
Both, males and females, had similar anti-JCV antibodies and JCV DNA levels, in contrast to other results for antibodies (Trampe et al. 2012) and for viral prevalence in urine of healthy people (Rossi et al. 2007), where these percentages seemed to be greater in males. We did not find significantly different levels of antibodies and DNA in relation to the age and to the number of years after diagnosing the illness, only a slight positive association between age and viral load. However, most previous published studies, even in healthy people, described an increase of the antibody seroprevalence and the viral prevalence in urine with age, what justified the follow-up of these parameters during the treatment (Gorelik et al. 2010; Rossi et al. 2007; Trampe et al. 2012; Ling et al. 2003; Kitamura et al. 1990; Agostini et al. 1996). The previous treatment with immunosuppressor and longer period of treatment did not seem to be related with higher rate of antibodies presence, probably because the increase of the risk of PML with these parameters was not directly related to de novo JCV infection, as previously suggested (Trampe et al. 2012).
In our cohort the rate of agreement between the two techniques was moderate; 26 % of our population would have been exposed to the JCV or not, depending on the technique used, they had different values in qPCR and two-step ELISA. This percentage was similar to other publications, such as that of Laroni et al. (20.5 %) (Laroni et al. 2012), and higher than other ones (Gorelik et al. 2010). It is likely that the difference was due to the higher sensitivity of our qPCR. The detection limit of our qPCR in urine was 14 copies/ml instead of the 50 copies/ml used by Gorelik et al. (2010). At the same time, this fact could explain that we described a high correlation between the anti-JCV antibody levels and the JCV DNA levels, but not these other authors.
We found a viral reactivation in PBMC samples in natalizumab treated patients, but also in non-treated patients. Consequently, we could not consider this reactivation as a risk factor for the PML. However, an association has been observed between the asymptomatic appearance of JCV DNA in the blood of natalizumab treated MS patients, and the differentiation of naïve CD8+ T lymphocytes into memory populations and the elicitation of a CD8+ T lymphocyte-mediated immune effector response (Mancuso et al. 2012). It would be interesting to evaluate the presence of these differences in our PML patient (positive for viral DNA in PBMC and serum 1 month before the PML diagnosis), and in patients with detectable DNA levels in serum. Likewise, the study of the different viral variants of these patients could help us to know if there are different kinds of reactivation.
The viral prevalence in urine seemed to increase between BV and the other ones from month 12, except for V21 and V24. This increase of the viral prevalence in urine, found in one study (Chen et al. 2009) but not in others (Rinaldi et al. 2010; Jilek et al. 2010), did not have clinical relevance. The neurotropic JCV variant did not seem to come from the urine; previous studies have not found this variant in urine (Reid et al. 2011).
Our rate of seroconvertion, 36 %, was higher than other previously published (Gorelik et al. 2010; Trampe et al. 2012). The use of the second generation two-step ELISA to analyze the second blood samples, instead of the original two-step ELISA (used with the first samples) would not alter the seroconvertion data, because the agreement between the original and the second generation two-step ELISA is very high (Lee et al. 2013). We only selected negative patients in the first measurement for a second analysis of the antibodies, so we could not detect negative seroconvertion as in other previous published studies (Trampe et al. 2012); although we detected this negative seroconvertion in the case of the prevalence in urine.
We stratified our population according to the viral presence in urine in three groups: with none, intermittent and permanent excretion of the virus in urine. All patients with detectable JCV DNA levels in PBMC except one were in the intermittent excretion group. Our case of PML, positive simultaneously for JCV DNA in serum and PBMC, presented the virus in urine permanently during the natalizumab-treatment; other previously described PML case had also this kind of JCV excretion in urine (Laroni et al. 2012). Most of the patients with divergent results regarding the conversion from positive to negative, or vice versa depending on the technique used (qPCR or two-step ELISA), belonged to the group with intermittent viral presence in urine, that had lower viral load than the patient group that exhibited permanent viral excretion. At the same time, we have demonstrated a correlation between the anti-JCV antibodies and the viral load levels. So it could be interesting to study whether these patterns are the same for the anti-JCV antibody levels and whether this fact is associated with different immunological way of control the JCV infection. To test this hypothesis we should increase the cohort and the number of visits in the longitudinal study of the anti-JCV antibodies, and to study the immunological response against the JCV in every pattern.
In summary, our results point out that assessing the JCV DNA levels in urine could be complementary to determine the anti-JCV antibodies for identifying MS patients who has been infected by the JCV. Nevertheless, the detection of viral DNA in urine but not the anti-JCV antibodies does not necessarily imply the same risk of PML than positive anti-JCV antibodies. Further research would be necessary to know if the different excretion pattern of the virus in urine, besides the detection of the virus in PBMC and/or serum, and the anti-JCV antibody levels, could have any relationship with immunological response against the JCV in MS patients treated with natalizumab.
References
Agostini HT, Ryschkewitsch CF, Stoner GL (1996) Genotype profile of human polyomavirus JC excreted in urine of immunocompetent individuals. J Clin Microbiol 34:159–164
Bloomgren G, Richman S, Hotermans C, Subramanyam M, Goelz S, Natarajan A, Lee S, Plavina T, Scanlon JV, Sandrock A, Bozic C (2012) Risk of natalizumab-associated progressive multifocal leukoencephalopathy. N Engl J Med 366:1870–1880
Chen Y, Bord E, Tompkins T, Miller J, Tan CS, Kinkel RP, Stein MC, Viscidi RP, Ngo LH, Koralnik IJ (2009) Asymptomatic reactivation of JC virus in patients treated with natalizumab. N Engl J Med 361:1067–1074
Egli A, Infanti L, Dumoulin A, Buser A, Samaridis J, Stebler C, Gosert R, Hirsch HH (2009) Prevalence of polyomavirus BK and JC infection and replication in 400 healthy blood donors. J Infect Dis 199:837–846
Gorelik L, Lerner M, Bixler S, Crossman M, Schlain B, Simon K, Pace A, Cheung A, Chen LL, Berman M, Zein F, Wilson E, Yednock T, Sandrock A, Goelz SE, Subramanyam M (2010) Anti-JC virus antibodies: implications for PML risk stratification. Ann Neurol 68:295–303
Jilek S, Jaquiery E, Hirsch HH, Lysandropoulos A, Canales M, Guignard L, Schluep M, Pantaleo G, Du Pasquier RA (2010) Immune responses to JC virus in patients with multiple sclerosis treated with natalizumab: a cross-sectional and longitudinal study. Lancet Neurol 9:264–272
Kitamura T, Aso Y, Kuniyoshi N, Hara K, Yogo Y (1990) High incidence of urinary JC virus excretion in nonimmunosuppressed older patients. J Infect Dis 161:1128–1133
Knowles WA, Pipkin P, Andrews N, Vyse A, Minor P, Brown DW, Miller E (2003) Population-based study of antibody to the human polyomaviruses BKV and JCV and the simian polyomavirus SV40. J Med Virol 71:115–123
Laroni A, Giacomazzi CG, Grimaldi L, Gallo P, Sormani MP, Bertolotto A, McDermott JL, Gandoglia I, Martini I, Vitello G, Rinaldi F, Barzon L, Militello V, Pizzorno M, Bandini F, Capello E, Palu G, Uccelli A, Mancardi GL, Varnier OE (2012) Urinary JCV-DNA testing during natalizumab treatment may increase accuracy of PML risk stratification. J Neuroimmune Pharmacol 7:665–672
Lee P, Plavina T, Castro A, Berman M, Jaiswal D, Rivas S, Schlain B, Subramanyam M (2013) A second-generation ELISA (STRATIFY JCV DxSelect) for detection of JC virus antibodies in human serum and plasma to support progressive multifocal leukoencephalopathy risk stratification. J Clin Virol 57:141–146
Ling PD, Lednicky JA, Keitel WA, Poston DG, White ZS, Peng R, Liu Z, Mehta SK, Pierson DL, Rooney CM, Vilchez RA, Smith EO, Butel JS (2003) The dynamics of herpesvirus and polyomavirus reactivation and shedding in healthy adults: a 14-month longitudinal study. J Infect Dis 187:1571–1580
Major EO (2010) Progressive multifocal leukoencephalopathy in patients on immunomodulatory therapies. Annu Rev Med 61:35–47
Mancuso R, Saresella M, Hernis A, Marventano I, Ricci C, Agostini S, Rovaris M, Caputo D, Clerici M (2012) JC virus detection and JC virus-specific immunity in natalizumab-treated multiple sclerosis patients. J Transl Med 10:248
Matos A, Duque V, Beato S, da Silva JP, Major E, Melico-Silvestre A (2010) Characterization of JC human polyomavirus infection in a Portuguese population. J Med Virol 82:494–504
Perkins MR, Ryschkewitsch C, Liebner JC, Monaco MC, Himelfarb D, Ireland S, Roque A, Edward HL, Jensen PN, Remington G, Abraham T, Abraham J, Greenberg B, Kaufman C, Laganke C, Monson NL, Xu X, Frohman E, Major EO, Douek DC (2012) Changes in JC virus-specific T cell responses during natalizumab treatment and in natalizumab-associated progressive multifocal leukoencephalopathy. PLoS Pathog 8:e1003014
Reid CE, Li H, Sur G, Carmillo P, Bushnell S, Tizard R, McAuliffe M, Tonkin C, Simon K, Goelz S, Cinque P, Gorelik L, Carulli JP (2011) Sequencing and analysis of JC virus DNA from natalizumab-treated PML patients. J Infect Dis 204:237–244
Rinaldi L, Rinaldi F, Perini P, Calabrese M, Seppi D, Grossi P, Mattisi I, Barzon L, Mengoli C, Sanzari M, Palu G, Gallo P (2010) No evidence of JC virus reactivation in natalizumab treated multiple sclerosis patients: an 18 month follow-up study. J Neurol Neurosurg Psychiatry 81:1345–1350
Rossi A, Delbue S, Mazziotti R, Valli M, Borghi E, Mancuso R, Calvo MG, Ferrante P (2007) Presence, quantitation and characterization of JC virus in the urine of Italian immunocompetent subjects. J Med Virol 79:408–412
Rudick RA, O’Connor PW, Polman CH, Goodman AD, Ray SS, Griffith NM, Jurgensen SA, Gorelik L, Forrestal F, Sandrock AW, Goelz E (2010) Assessment of JC virus DNA in blood and urine from natalizumab-treated patients. Ann Neurol 68:304–310
Sadiq SA, Puccio LM, Brydon EW (2010) JCV detection in multiple sclerosis patients treated with natalizumab. J Neurol 257:954–958
Trampe AK, Hemmelmann C, Stroet A, Haghikia A, Hellwig K, Wiendl H, Goelz S, Ziegler A, Gold R, Chan A (2012) Anti-JC virus antibodies in a large German natalizumab-treated multiple sclerosis cohort. Neurology 78:1736–1742
Watzinger F, Suda M, Preuner S, Baumgartinger R, Ebner K, Baskova L, Niesters HG, Lawitschka A, Lion T (2004) Real-time quantitative PCR assays for detection and monitoring of pathogenic human viruses in immunosuppressed pediatric patients. J Clin Microbiol 42:5189–5198
Acknowledgments
We are indebted to Cristina Fernández-Pérez, from the Department of Preventive Medicine, who participated in the statistical analysis. In addition, we are particularly thankful to María Concepción Ramírez and María Jesús Díez who collected the specimens.
Competing interests
All authors declared do not have any competing interests.
Funding
This work was supported by grants from the Instituto de Salud Carlos III-Fondo Europeo de Desarrollo Regional (Feder) [FIS Nº 09/02074]; Fundación Mutua Madrileña; Fundación LAIR; the Instituto de Salud Carlos III-Fondo Europeo de Desarrollo Regional (Feder) [CP07/00273] to [RAL] and REEM: Red Española de Esclerosis Múltiple” [RETICS-REEM RD07/0060] to [AGM].
Author information
Authors and Affiliations
Corresponding author
Additional information
Rafael Arroyo and Roberto Alvarez-Lafuente contributed equally to this work.
Rights and permissions
About this article
Cite this article
Dominguez-Mozo, M.I., Garcia-Montojo, M., De Las Heras, V. et al. Anti-JCV Antibodies Detection and JCV DNA Levels in PBMC, Serum and Urine in a Cohort of Spanish Multiple Sclerosis Patients Treated with Natalizumab. J Neuroimmune Pharmacol 8, 1277–1286 (2013). https://doi.org/10.1007/s11481-013-9496-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11481-013-9496-y