Abstract
Background
Trapeziometacarpal arthrodesis (TMA) has been complicated by nonunion and hardware failure.
Questions/Purposes
We hypothesized that modification of the TMA technique with a locking cage plate construct would afford reliable bony union while producing greater hand function than trapeziectomy with ligament reconstruction and tendon interposition (LRTI) at early follow-up.
Methods
We enrolled 36 consecutive patients with trapeziometacapal osteoarthritis (14 TMA patients (15 thumbs), 22 LRTI patients (22 thumbs)). The study was powered to detect a minimal clinically important difference on the QuickDASH questionnaire between groups. Secondary outcomes included Michigan Hand Questionnaire (MHQ), VAS-pain, and EQ-5D-3L scores. Patients were examined to evaluate thumb motion and strength. TMA patients were evaluated clinically and radiographically for union.
Results
Mean follow-up was 15.6 months, and the mean age was 59.2 years. Union was achieved in 14/15 (93%) of TMA thumbs. Improvement in QuickDASH scores was similar after TMA and LRTI (49 to 28 and 50 to 18, respectively). Postoperative patient-rated upper extremity function, health status, and pain were similar between groups. Pinch strength was significantly greater after TMA (5.9 vs 4.7 kg). No differences in thumb or wrist range of motion were observed postoperatively with the exception of greater total metacarpophalangeal joint motion after TMA. Complications after TMA included nonunion (7%), development of symptomatic scaphotrapezotrapezoidal (STT) arthrosis (7%), symptomatic hardware (7%), and superficial branch of the radial nerve (SBRN) paresthesia (7%). Complications after LRTI included subsidence (5%), MP hyperextension deformity (5%), and SBRN paresthesias (5%).
Conclusions
At early follow-up, patient-rated function was similar among patients undergoing TMA and LRTI. TMA produced 25% greater pinch strength compared with LRTI. Despite historical concerns regarding global loss of ROM with arthrodesis, motion was similar between groups. Our observed TMA nonunion rate of 7% is low relative to historically reported nonunion rates (7–16%). Locking cage plate technology affords rigid fixation for TMA with promising early results noting reliable bony union while minimizing complications.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The trapeziometacarpal joint of the thumb is commonly affected by osteoarthritis, second in frequency in the hand only to the distal interphalangeal joint, and it affects 1 in 4 women and 1 in 12 men [15, 19, 20, 24]. It is the most common site for surgery in the hand when surgery is sought to treat an arthritic condition [20]. The surgical treatment options offered to patients who fail nonoperative treatment vary depending on the patient’s age, medical comorbidities, functional demands, and radiographic staging but include ligament reconstruction [8], metacarpal osteotomy [2], arthroscopy and debridement [12, 15], total joint arthroplasty [1, 15, 28], silicone arthroplasty [1], trapeziometacarpal arthrodesis (TMA) [1, 3, 10, 11, 13–15, 21–23, 26, 29], and trapezial excision with or without ligament reconstruction and soft tissue interposition (LRTI) [1, 2, 4, 6, 9, 14–16, 21–23, 27–30]. Multiple systematic reviews have demonstrated that no one surgical procedure is superior to another, and that comparative studies are warranted [20, 31–33]. One recent randomized study terminated early due to a high rate of complications after TMA using a locking T-plate [18].
To date, there is a lack of consensus among hand surgeons regarding surgical indications or surgical treatment choice for TMA arthritis. Arthrodesis may be preferable in younger and more active patient with moderate to severe thumb trapeziometacarpal arthritis who needs to maintain power grip and pinch secondary to his/her occupation [13, 14, 23]. However, studies have shown that arthrodesis is also a viable option for older patients with moderate to severe thumb trapeziometacarpal arthritis [23, 26]. Complications associated with arthrodesis include nonunion with rates of 7–16% cited in the literature [3, 10, 11, 14, 29], hardware complications [22], and a potential predisposition to arthritis at adjacent joints [11] with additional concerns for loss in range of motion and an inability to flatten the hand [14, 21]. Alternatively, criticisms associated with trapeziectomy include potential shortening of the first ray, which can lead to decreased thumb strength as well as subluxation or painful arthritis of the pseudarthrosis between the base of thumb metacarpal and the scaphoid [5, 6, 15, 23, 30]. Even with a loss in scaphometacarpal height seen in trapeziectomy alone when compared with LRTI, short-term follow-up studies have found no difference in pain/function scores or grip/pinch strength [6, 9, 19, 24]. Despite these reported complications, there are similar subjective and objective outcomes when comparing arthrodesis with arthroplasty [14, 23].
Previous studies have assessed TMA with K wires, tension band fixation, staples, compression screws, and nonlocking plates, screws, and locking T-plates [3, 10, 11, 14, 21–23, 26, 29]. Use of a locking cage plate construct has not been extensively studied for arthrodesis. However, when comparing the size and geometry of such a plate with commonly used T-plates, there is reason to believe its mechanical properties may provide robust stability and help to produce superior rates of bony union. The purpose of this study was to compare outcomes following locked cage plate arthrodesis and LRTI for trapeziometacarpal arthritis of the thumb. Our hypothesis was that TMA with a locking cage plate construct would improve bony union rates compared with historical results while producing greater subjective and objective outcomes in the operative hand when compared with LRTI at early follow-up.
Patients and Methods
Study Design
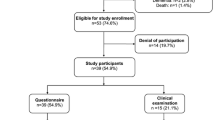
This study was performed in accordance with the strengthening the reporting of observational studies in epidemiology (STROBE) statement. After obtaining institutional review board approval for this longitudinal cohort study, we retrospectively identified 36 consecutive patients (14 TMA patients (15 thumbs), 22 LRTI patients (22 thumbs)) treated by 6 orthopedic hand fellowship-trained surgeons at our institution over 7 months in 2013 with either a TMA with a locking cage plate or with LRTI. Surgical treatment was based on surgeon and patient preference. These patients had failed to improve after nonsurgical treatment and had Eaton stages II, III, or IV primary osteoarthritis of the trapeziometacarpal joint [7, 8]. Exclusion criteria included prior surgical treatment of the trapeziometacarpal joint (arthroplasty or arthrodesis) and a lack of English proficiency by the patient. We did not observe any significant differences in baseline characteristics between the two groups (Table 1).
Clinical examination combined with preoperative plain radiographs or fluoroscopy images were used to establish the diagnosis of thumb trapeziometacarpal osteoarthritis. A preoperative Quick disabilities of the shoulder, arm, and hand questionnaire (Quick DASH) was available in all but three patients (1 TMA and 2 LRTI patients). To assess patient-rated health status, preoperative EQ-5D-3L scores were reviewed (9 TMA and 13 LRTI patients).
Surgical Technique
The TMA procedure was similar to the technique described by Goldfarb et al [13]. The procedure was modified by using a locking 4 × 2 or 3 × 2 hole cage plate with 2.0 mm screws (Medartis, Basel, Switzerland), as illustrated in Fig. 1a. First, a 3-cm incision was made on the skin over the dorsal radial aspect of the first carpal metacarpal joint. Abductor pollicis longus and extensor pollicis brevis tendons were identified and protected. Care was taken not to enter the scaphotrapezial joint when the capsulotomy and subperiosteal dissection was performed. Joint surfaces both at the first metacarpal base and the trapezium were denuded of cartilage and subchondral bone and contoured in a cup and cone fashion. Attention was then diverted to the radial styloid and a series of larger size curettes were used to harvest bone graft from the metaphysis of the distal radius. Bone graft was packed into the trapeziometacarpal joint, which was reduced into 30° of abduction, flexion, and pronation so that the thumb rested against the dorsal aspect of the index finger middle phalanx when the hand was held in a fist as described by Leach et al. [18]. This was provisionally maintained in position with a 0.062-in. Kirschner wire and then a plate was placed on the dorsal aspect of the joint. Nonlocking and locking screws were placed into the first metacarpal, and two locking screws were universally used in the trapezium. The joint reduction and position of the plate and screws were evaluated again under fluoroscopy. The remainder of the bone graft was tightly packed around the joint before closure. The thumb was immobilized in a thumb spica splint for two weeks followed by a thumb spica cast for an additional 4 weeks. The cast was then replaced by a removable thumb spica brace and a hand therapist started standardized hand therapy focusing on increasing mobility prior to strength.
The LRTI procedure was performed similarly to that described by Kriegs-Au et al. [17] (Fig. 1b). A curvilinear 3–4-cm incision was made at the glabrous/nonglabrous skin junction over the base of the thumb metacarpal and extended proximally to the wrist crease. Abductor pollicis longus and extensor pollicis brevis tendons were identified and protected as well as the radial artery. After a trapeziometacarpal and scaphotrapezial capsulotomy and subperiosteal dissection were performed, the trapezium was excised in its entirety. The flexor carpi radialis (FCR) tendon was identified and dissected towards its insertion at the base of the second metacarpal. A 1.5-cm second incision was then made 7-cm proximal to the wrist crease over the FCR tendon. With proximal and distal retraction, the tendon was divided in its entirety and retracted into the distal wound. The proximal incision was irrigated and the skin closed. Progressively larger drill bits were used to create a bony passage through the base of the thumb metacarpal. The FCR tendon was passed from deep to superficial through this osseous tunnel and then sutured back onto itself in the space vacated by the excised trapezium while the thumb was gently pulled distally to allow thumb suspension. After wound and skin closure, the LRTI group had the same immobilization period and standardized hand therapy as the arthrodesis group.
Cohort Assessment and Statistical Analysis
We collected all follow-up data during study related examinations at 6 weeks and 3, 6, 9, and 12 months, postoperatively. We obtained validated patient related questionnaires in all enrolled patients to assess disability including QuickDASH, Michigan Hand Questionnaire (MHQ), Visual Analog Pain (VAS-pain), and EQ-5D-3L overall health status scores postoperatively. The study was powered to detect a minimal clinically important difference (MCID) of 14 on the QuickDASH questionnaire between the treatment groups [25]. Physical examination outcome data were also collected. We measured grip and lateral pinch strength using a hydraulic hand dynamometer and pinch gauge (Lafayette Instrument, Lafayette IN, USA). Active range of motion measurements were evaluated in distance in centimeters of thumb tip to small finger proximal digital crease (Fig. 2a), distance in centimeters of volar index finger MCP joint to table (Fig. 2b), degrees of total affected thumb MCP motion, interphalangeal (IP) joint motion, affected thumb palmar, and radial abduction motion, and wrist motion (flexion, extension, radial, and ulnar deviation). We determined whether fusion had occurred for TMA patients both clinically (absence of fusion site tenderness to palpation) and radiographically (bridging bone on plain radiographs). Radiographic assessment was performed by a board certified attending radiologist and was part of the official medical record. The treating hand surgeon obtained and evaluated fluoroscopic images for each LRTI patient to evaluate for subsidence. Similarly, the treating hand surgeon documented all complications that occurred in each group.
To test the study hypothesis, grip and pinch strength, motion measurements, VAS-pain scores, and EQ-5D-3L scores were analyzed with a student t test. MHQ and QuickDASH scores were analyzed with a student t test and one-way ANOVA. Any significant findings on one-way ANOVA were further analyzed with Holm Sidak post-hoc analysis. The threshold for significance was set at p < 0.05.
Results
Despite nonrandomization, the cohorts were similar preoperatively with regard to age, and distribution of both gender and Eaton stage (Table 1). Preoperative Quick DASH and EQ-5D-3L scores did not differ between the two groups, indicating similar levels of baseline disability and general health, respectively. Both groups demonstrated statistically significant improvement in their Quick DASH scores that exceeded the MCID (20.6 and 31.7 for TMA and LRTI, respectively (Fig. 3).
With respect to the secondary outcomes the VAS-Pain score (11 vs. 12) and the total MHQ score (63 vs. 74) were similar between the respective TMA and LRTI groups (Table 2). The operative one-handed activities of daily living (ADL) subset score of the MHQ were greater after LRTI (61 vs. 87); however, there was no significant difference in two-handed ADL scores. Remaining MHQ subcategories were also similar between groups (overall function, pain, work, aesthetics, and satisfaction). In addition, there was no difference in patient reported overall health status between the TMA and LRTI groups (69 vs. 81, p = 0.09).
Lateral pinch strength was significantly greater in the arthrodesis group (5.9 vs. 4.7 kg, p = 0.03); however, no difference in grip strength was observed (25.0 vs. 27.9 kg, p = 0.38). Total thumb MCP joint motion (59° vs. 45°, p = 0.02) and thumb palmar abduction (66° vs. 59°, p = 0.02) were greater in the TMA group. There were no significant differences in other range of motion metrics including total thump IP joint motion (69° vs. 63°, p = 0.40), thumb radial abduction (69° vs. 63°, p = 0.13), index finger MCP joint to table distance (0.5 vs. 0.1 cm, p = 0.08), and thumb tip to small finger MCP joint distance (0.5 vs. 0.4 cm, p = 0.55).
A total of four complications occurred in the TMA group (Table 3). Union was confirmed in all but one thumb at latest follow-up, representing a nonunion rate of 7%. Because of functionally limiting pain, this patient was treated with removal of hardware, trapeziectomy, and LRTI. One patient experienced persistent pain and radiographs lacking bridging bone 4 months postoperatively, and was taken to the operating room for nonunion repair. However, after removal of the locking plate and screws, an assessment of the fusion site revealed definitive bony union. The patient’s pain improved after the second surgery, which suggests that the symptoms were due to painful hardware (7%). Another patient developed symptomatic STT arthrosis (7%), which has been managed with a guided corticosteroid injection. One patient experienced paresthesias along the dorsoradial incision in the SBRN distribution (7%), which resolved without intervention.
A total of three complications occurred in the LRTI group (Table 3). One patient experienced a hyperextension deformity at the thumb MP joint 4 weeks postoperatively (5%), which was managed with splinting. At later follow-up, their deformity had corrected and they remained asymptomatic. One patient experienced persistent pain and subjectively decreased strength and function 6 months postoperatively and was noted to have subsidence (5%) of the thumb metacarpal but has not required revision surgery. One LRTI patient experienced paresthesias in the SBRN distribution (5%), which resolved without intervention.
Discussion
While the main goals of treatment of thumb trapeziometacarpal arthritis are pain relief, strength, range of motion, and stability, the optimal operative treatment to accomplish these goals is still up for debate. Multiple systematic reviews have either shown studies to have insufficient evidence or confirm that there is no additional benefit of LRTI when compared with arthrodesis [20, 31–33]. There also have been varied results of trapeziometacarpal arthrodesis, mainly owing to the fact that the fusion can be accomplished via a multitude of fixation options [3, 14, 21, 23, 29]. The purpose of this study was to compare outcomes following locked cage plate arthrodesis and LRTI for the treatment of trapeziometacarpal arthritis. We used subjective and objective criteria to compare the outcomes of LRTI with TMA using locking cage plate technology. Both groups showed improvement in their QuickDASH scores postoperatively that exceeded the MCID. There was no significant difference when comparing all patient-rated pain and general health measures between the TMA and LRTI groups. Patient-rated upper extremity function was similar between groups based upon the MHQ total score.
This study has several limitations. It is a longitudinal comparative study with a small sample size with a total of 37 thumbs (15 in the TMA group). One patient we encountered during our enrollment period did not meet inclusion criteria (prior failed artelon spacer); however, nonunion resulted after attempted TMA. It is unclear how a larger sample size would have affected the reported nonunion rate in the TMA group. With a short-term mean follow-up of 15.6 months, it is impossible to fully comment on the potential risk of arthritis at nearby joints with arthrodesis or on the potential risk of first ray shortening/subluxation with LRTI. A more complete investigation of these issues would require a longer-term longitundinal cohort study. Additionally, despite similar baseline demographics, patients were not randomized to a treatment arm and potential selection bias by the surgeons cannot be ruled out. Assessment of nonunion following TMA was limited by use of plain radiograph; CT scan or MRI may have provided more certainty in the diagnosis. However, the confirmatory power of plain radiograph was improved by the ability to perform repeat radiographic and clinical examination over time. Lastly, the results of this study are only applicable to arthrodesis with a locked cage plate and screw fixation and not to other fixation techniques. The locked cage plate used in this study was not specifically designed for TMA arthrodesis. Design of a more anatomy-specific plate, especially one that provides compression across the arthrodesis site, may lead to improved outcomes and a lower nonunion rate. Finally, it is unclear if the observation of a greater one-handed ADL score after LRTI represents a true finding, especially in the setting of a similar two-handed ADL score.
Multiple studies have either shown no difference in grip and/or pinch strength or loss of range of motion in patients undergoing arthrodesis [14, 21, 26, 29]. We observed that the TMA group had significantly greater lateral pinch strength. The increase seen in lateral pinch strength may be explained by the more rigid construct allowed with locking plate technology that permitted earlier return to use. We did not observe any loss in range of motion after TMA as compared with LRTI. Most likely, remaining motion at the scaphotrapezial articulation compensates for the loss of motion of the trapeziometacarpal joint after fusion. However, this raises concerns for increased wear of the scaphotrapezial joint, and development of symptomatic arthrosis was observed in one of the TMA patients. Longer-term study is required to better understand the effect of TMA on the scaphotrapezial joint.
In this study, we observed four complications in the TMA group and three complications in the LRTI group. The one nonunited TMA patient was treated with conversion to LRTI. Our study found a 7% nonunion rate, which compares very favorably with the current literature on nonunion rates following attempted arthrodesis of the trapeziometacarpal joint. Another TMA patient required surgery for removal of symptomatic hardware in which bony union was observed intraoperatively. All three complications in the LRTI group were managed nonoperatively at latest follow-up. One patient in both groups experienced paresthesias in the SBRN distribution that subsequently resolved.
Study strengths include that all of these procedures were performed by fellowship trained hand orthopedic surgeons and thus it is very likely that there was not any learning curve effect that could alter the results. The inclusion of the Quick DASH, EQ-5D-3L, VAS-Pain, and MHQ scores provides multiple patient-rated validated outcome measures to allow us to gauge the effect of the procedures on improving upper extremity function and decreasing pain and disability. Moreover, our patient population was not limited to a certain age group, gender, or Eaton classification stage and thus our results are applicable to a wide range of patients with thumb trapeziometacarpal arthritis.
In the most recent randomized study comparing arthrodesis with LRTI, Vermeulen et al. demonstrated significantly more complications that were of clinical relevance or that required revision surgery (71% vs. 29%, p = 0.016) in the arthrodesis group [29]. Patients also were significantly more likely to consider having the surgery again in the LRTI group (86% vs. 53%, p = 0.025) [29]. Therefore, they decided to prematurely terminate the study. However as a result of ending the study early, they were not able to include the full number of patients deemed necessary to attain statistical power and as a result, most primary and secondary outcome measures were underpowered without reporting of p values. Our group has abandoned use of the locking T-plates used in this study, as in our experience this construct has been fraught with hardware failure, presumably from cyclic bending. Furthermore, while we do not know whether the lack of bone grafting in the Vermeulen study played a role in their observed rate of nonunion, we strongly advocate for and routinely use autologous bone grafting as an adjunct to TMA arthrodesis. The findings of our study may add needed context to the findings of Vermeulen and highlights the need for additional high quality therapeutic studies.
In conclusion, locking cage plate technology affords rigid fixation for TMA with promising early results noting reliable bony union while minimizing complications.
References
Amadio PC, De Silva SP. Comparison of the results of trapeziometacarpal arthrodesis and arthroplasty in men with osteoarthritis of the trapeziometacarpal joint. Ann Chir Main Membr Super: Organe Off Soc Chir Main = Ann Hand Upper Limb Surg. 1990; 9(5): 358-363.
Atroshi I, Axelsson G, Nilsson EL. Osteotomy versus tendon arthroplasty in trapeziometacarpal arthrosis: 17 patients followed for 1 year. Acta Orthop Scand. 1998; 69(3): 287-290.
Bamberger HB, Stern PJ, Kiefhaber TR, McDonough JJ, Cantor RM. Trapeziometacarpal joint arthrodesis: a functional evaluation. J Hand Surg. 1992; 17(4): 605-611.
Belcher HJ, Nicholl JE. A comparison of trapeziectomy with and without ligament reconstruction and tendon interposition. J Hand Surg. 2000; 25(4): 350-356.
Burton RI, Pellegrini VD Jr. Surgical management of basal joint arthritis of the thumb. Part II. Ligament reconstruction with tendon interposition arthroplasty. J Hand Surg. 1986; 11(3): 324-332.
Davis TR, Brady O, Dias JJ. Excision of the trapezium for osteoarthritis of the trapeziometacarpal joint: a study of the benefit of ligament reconstruction or tendon interposition. J Hand Surg. 2004; 29(6): 1069-1077.
Eaton RG, Glickel SZ. Trapeziometacarpal osteoarthritis. Staging as a rationale for treatment. Hand Clin. 1987; 3(4): 455-471.
Eaton RG, Littler JW. Ligament reconstruction for the painful thumb carpometacarpal joint. J Bone Joint Surg Am. 1973; 55(8): 1655-1666.
Field J, Buchanan D. To suspend or not to suspend: a randomised single blind trial of simple trapeziectomy versus trapeziectomy and flexor carpi radialis suspension. J Hand Surg Eur Vol. 2007; 32(4): 462-466.
Forseth MJ, Stern PJ. Complications of trapeziometacarpal arthrodesis using plate and screw fixation. J Hand Surg. 2003; 28(2): 342-345.
Fulton DB, Stern PJ. Trapeziometacarpal arthrodesis in primary osteoarthritis: a minimum two-year follow-up study. J Hand Surg. 2001; 26(1): 109-114.
Furia JP. Arthroscopic debridement and synovectomy for treating basal joint arthritis. Arthroscopy: J Arthrosc Relat Surg: Off Publ Arthrosc Assoc N Am Int Arthrosc Assoc. 2010; 26(1): 34-40.
Goldfarb CA, Stern PJ. Indications and techniques for thumb carpometacarpal arthrodesis. Tech Hand Upper Extrem Surg. 2002; 6(4): 178-184.
Hartigan BJ, Stern PJ, Kiefhaber TR. Thumb carpometacarpal osteoarthritis: arthrodesis compared with ligament reconstruction and tendon interposition. J Bone Joint Surg Am. 2001; 83-A(10): 1470-1478.
Kapoutsis DV, Dardas A, Day CS. Carpometacarpal and scaphotrapeziotrapezoid arthritis: arthroscopy, arthroplasty, and arthrodesis. J Hand Surg. 2011; 36(2): 354-366.
Kriegs-Au G, Petje G, Fojtl E, Ganger R, Zachs I. Ligament reconstruction with or without tendon interposition to treat primary thumb carpometacarpal osteoarthritis. A prospective randomized study. J Bone Joint Surg Am. 2004; 86-A(2): 209-218.
Kriegs-Au G, Petje G, Fojtl E, Ganger R, Zachs I. Ligament reconstruction with or without tendon interposition to treat primary thumb carpometacarpal osteoarthritis. Surgical technique. J Bone Joint Surg Am. 2005; 87(Suppl 1(Pt 1)): 78-85.
Leach RE, Bolton PE. Arthritis of the carpometacarpal joint of the thumb. Results of arthrodesis. J Bone Joint Surg Am. 1968; 50(6): 1171-1177.
Li YK, White C, Ignacy TA, Thoma A. Comparison of trapeziectomy and trapeziectomy with ligament reconstruction and tendon interposition: a systematic literature review. Plast Reconstr Surg. 2011; 128(1): 199-207.
Martou G, Veltri K, Thoma A. Surgical treatment of osteoarthritis of the carpometacarpal joint of the thumb: a systematic review. Plast Reconstr Surg. 2004; 114(2): 421-432.
Mureau MA, Rademaker RP, Verhaar JA, Hovius SE. Tendon interposition arthroplasty versus arthrodesis for the treatment of trapeziometacarpal arthritis: a retrospective comparative follow-up study. J Hand Surg. 2001; 26(5): 869-876.
Raven EE, Kerkhoffs GM, Rutten S, Marsman AJ, Marti RK, Albers GH. Long term results of surgical intervention for osteoarthritis of the trapeziometacarpal joint: comparison of resection arthroplasty, trapeziectomy with tendon interposition and trapezio-metacarpal arthrodesis. Int Orthop. 2007; 31(4): 547-554.
Schroder J, Kerkhoffs GM, Voerman HJ, Marti RK. Surgical treatment of basal joint disease of the thumb: comparison between resection-interposition arthroplasty and trapezio-metacarpal arthrodesis. Arch Orthop Trauma Surg. 2002; 122(1): 35-38.
Shuler MS, Luria S, Trumble TE. Basal joint arthritis of the thumb. J Am Acad Orthop Surg. 2008; 16(7): 418-423.
Sorensen AA, Howard D, Tan WH, Ketchersid J, Calfee RP. Minimal clinically important differences of 3 patient-rated outcomes instruments. J Hand Surg. 2013; 38(4): 641-649.
Taylor EJ, Desari K, D’Arcy JC, Bonnici AV. A comparison of fusion, trapeziectomy and silastic replacement for the treatment of osteoarthritis of the trapeziometacarpal joint. J Hand Surg. 2005; 30(1): 45-49.
Tomaino MM, Vogt M, Weiser R. Scaphotrapezoid arthritis: prevalence in thumbs undergoing trapezium excision arthroplasty and efficacy of proximal trapezoid excision. J Hand Surg. 1999; 24(6): 1220-1224.
Ulrich-Vinther M, Puggaard H, Lange B. Prospective 1-year follow-up study comparing joint prosthesis with tendon interposition arthroplasty in treatment of trapeziometacarpal osteoarthritis. J Hand Surg. 2008; 33(8): 1369-1377.
Vermeulen GM, Brink SM, Slijper H, et al. Trapeziometacarpal arthrodesis or trapeziectomy with ligament reconstruction in primary trapeziometacarpal osteoarthritis: a randomized controlled trial. J Bone Joint Surg Am. 2014; 96(9): 726-733.
Vermeulen GM, Brink SM, Sluiter J, Elias SG, Hovius SE, Moojen TM. Ligament reconstruction arthroplasty for primary thumb carpometacarpal osteoarthritis (Weilby technique): prospective cohort study. J Hand Surg. 2009; 34(8): 1393-1401.
Vermeulen GM, Slijper H, Feitz R, Hovius SE, Moojen TM, Selles RW. Surgical management of primary thumb carpometacarpal osteoarthritis: a systematic review. J Hand Surg. 2011; 36(1): 157-169.
Wajon A, Ada L, Edmunds I. Surgery for thumb (trapeziometacarpal joint) osteoarthritis. Cochrane Database Syst Rev. 2005; 4, CD004631.
Wajon A, Carr E, Edmunds I, Ada L. Surgery for thumb (trapeziometacarpal joint) osteoarthritis. Cochrane Database Syst Rev. 2009; 4, CD004631.
Acknowledgments
The authors acknowledge the efforts of Andre Guthrie, whose efforts were integral to the management and completion of this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Nikolas H. Kazmers, MD, MSE; Kirk J. Hippensteel, MD; and Lindley B. Wall, MD have declared that they have no conflict of interest. Charles A. Goldfarb, MD reports personal fees from Wolters-Kluwer Publishing, independent Expert witness, and ASSH Board Meetings, outside the work. Richard H. Gelberman, MD reports personal fees from JBJS Board of Trustees and Healthpoint Capital: Member of the Scientific Advisory Board, grants from the National Institutes of Health R01 AR062947 and personal fees from Wolters-Kluwer and Medartis, outside the work. Daniel A. Osei, MD, MSc reports grants from NIH KL2 Training Grant, during the conduct of the study. Ryan P. Calfee, MD, MSc reports grants from ASSH and Medartis and personal fees from Depuy/Synthes, outside the work. Martin I. Boyer, MD, MSc reports personal fees from OrthoHelix, Acumed, LLC, Hand Surgical Medicolegal Consultation, LLC, Wolters-Kluwer Publishing, Tournier, and OrthoHelix, outside the work.
Human/Animal Rights
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008 (5).
Informed Consent
Informed consent was obtained from all patients for being included in the study.
Required Author Forms
Disclosure forms provided by the authors are available with the online version of this article.
Funding
This publication was supported by the Institute of Clinical and Translational Sciences Award program of the National Center for Advancing Translational Sciences (NCATS) at the National Institutes of Health (NIH), grant numbers UL1 TR000448, KL2TR000450.
Additional information
Level of Evidence: Therapeutic Study-Level III
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
ESM 1
(PDF 1225 kb)
Rights and permissions
About this article
Cite this article
Kazmers, N.H., Hippensteel, K.J., Calfee, R.P. et al. Locking Plate Arthrodesis Compares Favorably with LRTI for Thumb Trapeziometacarpal Arthrosis: Early Outcomes from a Longitudinal Cohort Study. HSS Jrnl 13, 54–60 (2017). https://doi.org/10.1007/s11420-016-9527-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11420-016-9527-3