Abstract
Oral fluid (OF) is an advantageous matrix for cannabis detection, with on-site tests available for roadside drug-impaired driver screening. Limited data exist for device performance following consumption of vaporized cannabis, which reduces exposure to harmful combustion by-products. We assessed cannabinoid OF disposition, with and without alcohol, and evaluated on-site Dräger® DrugTest 5000 performance (Dräger) following controlled vaporization of cannabis. Forty-three cannabis smokers (≥1×/3 months, ≤3 days/week) reported 10–16 h prior to dosing, and drank placebo or low-dose alcohol [target ~0.065 % peak breath-alcohol concentration (BrAC)] 10 min prior to inhaling 500 mg of placebo, low-dose [2.9 % ∆9-tetrahydrocannabinol (THC)], or high-dose (6.7 % THC) vaporized cannabis (within-subjects; six possible alcohol–cannabis combinations; 19 completers). BrAC readings and OF (Quantisal™, Dräger) were collected before and up to 8.3 h post-dose. Median [range] maximum OF concentrations (C max) for low and high doses (no alcohol, N = 19) were 848 [32.1–18,230] and 764 [25.1–23,680] µg/l THC; 6.0 [0–100] and 26.8 [1.0–1106] µg/l cannabidiol; 54.4 [1.8–941] and 29.7 [0–766] µg/l cannabinol; and 24.1 [0–686] and 18.0 [0–414] ng/l 11-nor-9-carboxy-THC (THCCOOH). Lack of significant differences in THC concentration between low doses and high doses indicated that participants may have titrated doses. THC, cannabidiol and cannabinol C max values were immediately post-inhalation, but metabolite THCCOOH t max showed interindividual variability. Concurrent alcohol did not affect OF cannabinoid concentrations or on-site test sensitivity. With a THC confirmation cutoff of 5 µg/l, Dräger sensitivity, specificity, and efficiency were 60.8, 98.2, and 82.5 %. Dräger had lower sensitivity after 6.7 % THC vaporization (53.8 %, THC ≥2 µg/l confirmation cutoff) than reported following smoking a 6.8 % THC cigarette, but high specificity (99.3 %) and comparable efficiency (65.0 %). Vaporized THC bioavailability may be lower than that when smoked. Confirmation cutoff, time course, intake histories, and additional cannabinoid analytes also affect OF interpretation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cannabis is the most prevalent illicit drug identified in drivers [1, 2]. It is frequently consumed together with alcohol, the most common licit drug, and driving under the influence of drugs (DUID) cases often show this combination [3, 4]. Both drugs are associated with impairment, alone and combined [4–8]. States that decriminalized medical or recreational cannabis observed increased cannabis-driving cases [9, 10], presenting challenges for traffic safety enforcement. Oral fluid (OF) is an advantageous sampling matrix for drug screening because of ease of collection, noninvasiveness, and facility for on-site testing [11]. Observed collection is a deterrent to adulteration, and drugs in OF are frequently associated with recent intake [11–13]. OF is often collected in roadside surveys and case–control studies, wherein participants might elect not to undergo blood collection [1, 2, 14, 15]. With better knowledge of OF cannabinoid disposition, new workplace and DUID OF drug-testing cutoffs [∆9-tetrahydrocannabinol (THC, the primary psychoactive phytocannabinoid) ≥2 µg/l, and/or 11-nor-9-carboxy-THC (THCCOOH) ≥20 ng/l] were proposed by the Substance Abuse and Mental Health Services Administration (SAMHSA) [16]. The European Driving under the Influence of Drugs, Alcohol, and Medicines (DRUID) project used THC ≥1 µg/l to ensure identical analytical cutoffs in all laboratories participating in the program [17].
To date, most OF cannabinoid disposition research focused on smoking as the route of administration, because it remains the most prevalent route of intake [18]. By controlling inhalation topography (the manner in which the cannabis joint or blunt is smoked), individuals can titrate doses to their desired level, achieving maximum THC concentrations prior to the end of smoking [19–21]. Cannabis vaporization is increasing as a smoking alternative, because it produces lower combustion byproduct-to-THC ratios [22, 23]. Vaporizers reduce exposure to harmful polycyclic aromatic hydrocarbons and other respiratory-hazardous combustion products [24–26]. A survey querying 6,883 individuals who consumed cannabis at least once in the previous month indicated those who utilized vaporizers were significantly less likely (OR 0.40 controlling for age, sex, cigarette smoking, amount of cannabis consumed) to report respiratory problems than those who smoked or employed other inhalation techniques [27]. Subjective effects and plasma THC concentrations are similar for vaporization and smoking, and studies indicated participant preference for vaporization [24]. Increasingly, antismoking legislation in public facilities causes smokers to search for alternatives; popular e-cigarettes or “vape pens” can conceal cannabis consumption in public settings. As states continue to decriminalize medical or recreational cannabis, vaporization may become more common among health-conscious or discreet smokers. Quantifying OF cannabinoid disposition after vaporization is critical for guiding further development of OF as a test matrix for workplace and DUID investigation.
On-site cannabis screening tests have become common tools used in DUID cases in the past decade [2, 28–31]. The goals of these technologies include assisting law enforcement officers to evaluate drug-impaired driving at the roadside—before drug effects recede during lengthy arrest and booking procedures—and deterring DUID [2, 30]. The Dräger® DrugTest 5000 is considered among the most reliable devices for smoked cannabis testing [7, 30, 32, 33], but limited data exist for on-site OF devices following vaporization of cannabis [13].
We addressed these knowledge gaps by evaluating OF cannabinoids and an on-site screening device after vaporization, hypothesizing cannabis vaporization OF results similar to smoking. We quantified and assessed cannabinoid OF disposition, with and without alcohol, and evaluated on-site Dräger DrugTest 5000 performance (Dräger) following controlled vaporized cannabis administration.
Materials and methods
Participants
Healthy adult volunteers provided written informed consent for this University of Iowa Institutional Review Board-approved controlled cannabis administration study. Participants received comprehensive medical and psychological evaluations to ensure eligibility. Inclusion criteria included: ages 21–55 years; self-reported average cannabis consumption ≥1×/3 months but ≤3 days/week over the past 3 months; self-reported “light” or “moderate” alcohol consumption according to quantity-frequency-variability scale; or if “heavy”, not more than four servings in a typical drinking occasion. Exclusion criteria included: current clinically significant medical history or illness; history of clinically significant adverse event associated with cannabis or alcohol intoxication; ≥450 ml blood donation in 2 weeks preceding drug administration; pregnant or nursing (pregnancy tests conducted at screening and each dosing visit); interest in drug abuse treatment within 60 days preceding enrollment; and currently taking drugs contraindicated with cannabis or alcohol.
Study design
We utilized a 3 × 2 factorial design with three cannabis levels (placebo, low, high) and two alcohol levels (placebo, active). Participants entered the research unit approximately 10–16 h prior to drug administration to preclude intoxication at the time of dosing. Over 10 min ad libitum, participants drank low-dose 95 % grain alcohol [calculated to produce a peak breath alcohol concentration (BrAC) of approximately 0.065 %] mixed with juice or placebo (same volume of juice with alcohol-swabbed rim and topped with 1 ml alcohol for taste and odor). After drinking, participants inhaled 500 mg of vaporized cannabis plant material over 10 min (Volcano® Medic vaporizer, Storz & Bickel, Tuttlingen, Germany). Participants received placebo [0.008 ± 0.002 % THC, 0.001 ± 0.001 % cannabidiol (CBD), 0.009 ± 0.003 % cannabinol (CBN)], low (2.9 ± 0.14 % THC, 0.05 ± 0.00 % CBD, 0.22 ± 0.02 % CBN), or high (6.7 ± 0.05 % THC, 0.19 ± 0.01 % CBD, 0.37 ± 0.03 % CBN) cannabis [obtained through NIDA Chemistry and Physiological Systems Research Branch (Research Triangle Institute, Oxford, MS, USA)] doses. In this within-subjects design, completing participants received each alcohol/cannabis combination, for a total of six sessions. Sessions were separated by ≥1 week to prevent carryover from study drug administration in randomized order.
BrAC was measured with an on-site breath-testing device (Alco-Sensor® IV, Intoximeters, St. Louis, MO, USA) on admission, 0.8 h before, and 0.17, 0.42, 1.4, 2.3, 3.3, 4.3, 5.3, 6.3, 7.3, and 8.3 h after cannabis dosing started. This measurement device reports results in grams per 210 l of breath [limit of quantification (LOQ) 0.006 g/210 l], which is equivalent to approximate BAC. OF specimens were collected immediately following each BrAC measurement (except 0.42 h) with the Quantisal™ collection device (Immunalysis, Pomona, CA, USA) and the Dräger DrugTest 5000 (Dräger Safety Diagnostics, Lübeck, Germany) on-site test, in that order.
The Quantisal consists of an absorbent pad on a plastic stick, which is placed under the tongue to collect 1.0 ± 0.1 ml of OF. The device comes with a tube containing a standard amount of stabilizing buffer, into which the pad is deposited after collection. The Dräger cassette contains a polymeric noncompressible pad that is swiped throughout the mouth, tongue, and cheeks to collect 270 ± 40 µl. Both devices contain a volume adequacy indicator, which changes color when sufficient sample is collected. OF for each device was collected until the indicator turned blue, or after a maximum of 10 min. Low-volume specimens were noted and no weight correction was performed. Oral intake (eating, drinking, inhaling/smoking) was prohibited 10 min prior to OF collection.
Specimen analysis
Dräger specimens were analyzed in real time on the analyzer, producing a qualitative “Positive”/“Negative” or “Invalid” (if improper lateral flow was detected) response using a screening cutoff of 5 µg/l of THC as recommended by the manufacturer. Confirmatory (Quantisal) specimens were diluted in the elution/stabilization buffer at 4 °C for at least 12 h prior to pad removal and then transferred to cryotubes for storage at 4 °C. Specimens were analyzed 1 month ± 1 week after collection based on our previous stability study [34]. Specimens were quantified for THC, CBD, CBN, and the THCCOOH metabolite by a published validated two-dimensional gas chromatography–mass spectrometry method [35], with minor modifications as follows. Before loading the initial elution solvent, 0.4 ml of hexane was added to solid-phase extraction columns. THC, THCCOOH, CBD, and CBN respective linear ranges were 0.5–50 µg/l, 15–500 ng/l, 1–50, and 1–50 µg/l. Interassay and intraassay imprecision were <12.3 %, and inaccuracy was ≤14.4 % (n = 21). If concentrations exceeded the upper LOQ, OF specimens were diluted with drug-free Quantisal buffer to achieve concentrations within the linear range of the method.
Data analysis
Maximum concentration (C max), time to C max (t max), and time of last detection (t last) were calculated with concentrations observed post-dose. Because some individuals were cannabinoid-positive at baseline, an additional parameter was calculated (C max as difference from baseline, C max−C 0) to account for previously self-administered cannabis. The area under the curve from baseline to 8.3 h (AUC0–8.3h) was calculated by a linear trapezoidal method. If sessions were terminated early (voluntary participant withdrawal), provided specimens were analyzed and included in Dräger calculations. Other measures (C max, t max, t last) were assessed only if two or more successive subsequent samples were negative or <20 % of maximum. AUC0–8.3h was not evaluated for early terminations.
Statistical evaluation was performed with IBM SPSS Statistics Version 19 for Windows. For statistical purposes, concentrations <LOQ were set to 0, and times ≥8.3 h were set to 8.3 h. Within-subject medians were compared individually (placebo vs low dose vs high dose; with and without alcohol) with the Wilcoxon Matched-Pairs Test. Overall alcohol and cannabis effects were compared for each analyte with factorial repeated measures analysis of variance (ANOVA, factors: cannabis, alcohol) with Bonferroni correction for individuals who completed all six sessions. Friedman’s ANOVA was utilized to confirm that BrAC did not vary significantly by cannabis dose at any time. For alcohol-positive sessions, THC C max vs BrAC was compared for placebo, low, and high doses via linear regression on GraphPad Prism 5 (La Jolla, CA, USA). Dräger sensitivity [100 × true positives (TP)/(TP+ false negatives (FN))], specificity [100 × true negatives (TN)/(TN+ false positives (FP))], and efficiency [100 × (TN + TP)/(TN + TP + FN + FP)] were calculated for different confirmation cutoffs. Low-dose vs high-dose times of last detection (t last) were compared for different Dräger screening/confirmation cutoffs via the Mann–Whitney U Test. Fisher’s Exact Test was utilized to compare Dräger performance in the presence and absence of alcohol, at baseline and up to 4.3 h post-inhalation (median alcohol t last, to ensure comparison of the same time course and prevent over-representation from alcohol-negative sessions). Figures were created on GraphPad Prism 5.
Results
Participants
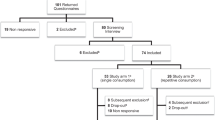
Forty-three healthy adults (26 men, 17 women), aged 21–42 years, provided OF for this study (Table 1). Self-reported cannabis history varied considerably between individuals. Two participants (21 and 25) reported most recent cannabis intake 4 and 6 months prior to admission, despite indicating overall average intake at least once/3 months. However, most had consumed cannabis within the past week. Nineteen participants completed all six dosing sessions. The 24 other participants withdrew for personal reasons (e.g., job obligations, scheduling, elected to withdraw) or adverse events (e.g., nausea/emesis or dizziness related to study drugs or other study procedures) (Table 1 lists doses received and reasons for withdrawal). There were no significant differences between completers and noncompleters in age, weight, body mass index (BMI), or self-reported cannabis history (p > 0.21, Mann–Whitney U [exact] test).
Alcohol
Completers’ breath alcohol C max, t max, t last, and AUC0–8.3h values are summarized in Table 2. For information purposes, pharmacokinetic data from all participants (including noncompleters) are provided in Online Resource 1. Within-subject alcohol doses produced similar AUC0–8.3h. Alcohol concentration did not differ significantly between alcohol-positive doses at any time point, nor did overall alcohol C max and AUC0–8.3h (Fig. 1). Active cannabis (relative to placebo) resulted in significantly later alcohol t max (ANOVA χ 2(2) = 6.621, p = 0.037), but alcohol t max did not differ significantly between active (low vs high) cannabis doses. Alcohol did not significantly affect THC C max (Fig. 2, no slope differed significantly from 0) or THC t max. Alcohol displayed a typical zero-order elimination profile [36, 37], and was not detected after 5.3 h.
Median [interquartile range] breath alcohol concentration (BrAC) in 19 completers following drinking placebo and three equivalent Everclear grain alcohol doses at separate sessions, with controlled inhalation of placebo, low (2.9 %), or high (6.7 %) ∆9-tetrahydrocannabinol (THC) vaporized cannabis. In total, there were three sessions (placebo, low, high cannabis) with no alcohol; alcohol was never detected in any of these sessions. Vertical dotted line represents start of cannabis administration. Asterisk, overall cannabis p ≤ 0.004 by repeated-measures analysis of variance (ANOVA) with Bonferroni correction for repeated measures. Significance level set to p < 0.05/12 measurements = p < 0.004
THC maximum oral fluid concentration vs BrAC for placebo, low (2.9 %), and high (6.7 %) THC doses (all participant data) following drinking alcohol and inhaling controlled cannabis by vaporizer. Line correlations were not significantly nonzero (THC concentrations did not vary with BrAC). Except for Participant 30, THC concentrations did not exceed 42.6 µg/l after the placebo dose, and did not exceed 21.0 µg/l when baseline OF THC was negative
Quantisal OF cannabinoids
Completers’ OF THC, CBD, CBN, and THCCOOH pharmacokinetic data and statistical analysis (Factorial ANOVA) are presented in Tables 2 and 3. No significant alcohol–cannabis interactions were observed. All participants’ data and pairwise comparisons (Online Resources 2–5) corroborated results from completers. THC C max was significantly higher after low and high doses (with and without alcohol) than placebo, and AUC0–8.3h was significantly higher than placebo after the low dose (high vs placebo had a trend for completers, p = 0.056) (Table 2, Online Resource 2). No dose difference was observed in THC t max (immediately after dosing). After active cannabis, the median t last was ≥8.3 h, which is not significantly different between low and high doses. No significant low-dose vs high-dose differences were observed for OF THC at any time post-dose (Fig. 3); however, the high dose showed greater interindividual variability, particularly after alcohol (Table 2). Placebo cannabis contained 0.008 ± 0.002 % THC, and low THC concentrations were detected in OF after this dose, even after accounting for baseline. However, OF THC never exceeded 42.6 µg/l after placebo, except for Participant 30 (described below). When baseline OF THC was 0, placebo THC t max did not exceed 21.0 µg/l. Online Resource 6 depicts THC and THCCOOH before dosing and over 8.3 h for placebo sessions.
Median (interquartile range) oral fluid a THC, b cannabidiol (CBD), c cannabinol (CBN), and d 11-nor-9-carboxy-THC (THCCOOH) vs time after controlled vaporized cannabis inhalation in 19 completers. Horizontal dotted line represents analyte limit of quantification (LOQ); vertical dotted line represents start of cannabis administration. Asterisk, doses significantly different overall by Friedman’s ANOVA (p ≤ 0.001). Hash symbol, overall dose effect p < 0.05 by Friedman’s ANOVA, for informational purposes. (Bonferroni correction sets significance level at p < 0.05/11 measurements = p < 0.005). Plus, all placebo doses significantly different to all active THC doses (p < 0.005), with no significant differences between any active doses. Double dagger, all placebo doses different to all active THC doses (p < 0.05), with no significant differences between any active doses. Alpha, p < 0.05 for placebo vs low (no alcohol), placebo vs high (with and without alcohol), and low vs high (with alcohol). Beta, p < 0.05 for placebo vs high (with and without alcohol), and for low vs high (with and without alcohol). Gamma, p < 0.05 for placebo vs high (with and without alcohol), and for low vs high (with alcohol). Delta, p < 0.05 for placebo vs low (with alcohol), and for placebo vs high (with alcohol). Epsilon, p < 0.05 for placebo vs high (with alcohol)
CBD C max was significantly greater and had substantial variability after high-dose cannabis when compared to low-dose cannabis (Table 2; Fig. 3). CBD t max occurred immediately after inhalation; after placebo and low doses, t last was typically 0.17 h. After the high dose, median t last shifted significantly (p = 0.033) to 2.3 and 3.3 [0.17 to ≥8.3] h for nonalcohol and alcohol conditions, respectively (Table 2). At individual sampling times over the first 7.3 h, there was a significant overall dose difference (p < 0.05, Fig. 3). Specific differences by post-dose time are provided in Fig. 3. CBD was only detected in OF after placebo (0.05 % potency) in one and two sessions without and with alcohol, respectively. In the placebo-without-alcohol session (Participant 24), C max−C 0 was −0.4 μg/l, indicating that the detected CBD was carryover from a previous self-administration. In the active-alcohol sessions, all participants were negative for CBD at baseline (C 0 = 0 μg/l), indicating that detected CBD (Participants 6 and 39) came from the placebo cannabis dose (Table 2). CBD low dose vs high dose differences can be explained by the fourfold difference in CBD potency of the cannabis. Participants titrated their dose based on psychoactive THC concentrations (only twofold low–high dose THC potency difference); titration was not based on CBD, because CBD is nonpsychoactive.
Low-dose vs high-dose CBN C max and AUC0–8.3h did not differ significantly (Tables 2 and 3). CBN t max occurred within 3.3 h post-dose, but was 0.17 h in 98 % of sessions. Participants 3 and 37 had CBN t max values of 1.4 and 3.3 h, respectively, in their high-dose/no-alcohol sessions; all other CBN t max values were 0.17 h. The only significant pairwise alcohol difference was for t last with high cannabis (Online Resource 4). As with CBD, alcohol produced significantly later CBN t last. CBN concentrations and specific differences by post-dose time are provided in Fig. 3. CBN was only detected in five participants’ OF after placebo cannabis, in both alcohol conditions.
THCCOOH displayed substantial interindividual OF concentration variability at all doses, reflecting participants’ smoking history (Table 2; Fig. 3). There was no significant low-dose vs high-dose difference in C max or AUC0–8.3h, but THCCOOH C max accounting for baseline was significantly higher after the high dose than after the low dose in completers (Table 3). Alcohol had no effect on any THCCOOH results. Low-dose and high-dose C max−C 0 were significantly higher than placebo, and C max−C 0 ranges demonstrated notable differences relative to C max ranges (Table 2). Median THCCOOH t max occurred 1.4–2.8 h post-dose for every condition; however, substantial variability attributed to smoking history/body burden and individual metabolic rates was noted. When detected, THCCOOH tlast was typically ≥8.3 h.
On admission the night prior to dosing, 51 % of Quantisal specimens were positive for THC (0.52–440.8 µg/l), 5 % for CBD (1.1–41.7 µg/l), 16 % for CBN (1.0–33.3 µg/l), and 38 % for THCCOOH (15.1–887 ng/l). The following morning at baseline, 47 % of all specimens remained positive for THC (0.54–72.9 µg/l), 0.6 % for CBD (2.1 µg/l), 2 % for CBN (1.1–3.6 µg/l), and 34 % for THCCOOH (15.1–911 ng/l). Participants 6, 7, 10, 27, and 38 were THCCOOH-positive at baseline (after overnight) for all doses received, and each had at least one baseline Quantisal OF with THCCOOH >100 ng/l. OF THC was ≥1 µg/l and THCCOOH ≥20 ng/l at baseline across all their sessions.
Based on pharmacokinetic data, Participant 30 may have accessed active cannabis during his placebo sessions, despite being under observation throughout his stay (Online Resource 7). For his placebo with alcohol session, THC was negative on admission to the unit, but positive prior to dosing; THC, CBD, and CBN C max were 569, 17.8, and 54.8 µg/l, respectively, at 0.17 h. It is possible these high concentrations resulted from dosing error; however, records were carefully reviewed and there was no indication that an error occurred. Because Participant 30 was negative on admission and positive at baseline, we cannot rule out clandestine intake prior to dosing. For his placebo without alcohol session, THC and CBN C max were 22.7 and 2.2 µg/l, respectively, at 5.3 h, despite being lower/negative earlier post-dose. His active doses did not contain anomalous findings. Data from these placebo-cannabis sessions were excluded from median [range] calculations for C max, t max, t last, and AUC0–8.3h and for matched-pairs analyses.
Dräger DrugTest 5000 performance and confirmation comparison
In total, 1,723 OF Dräger-Quantisal specimen pairs were obtained. Thirteen Dräger specimens (0.8 %) produced “invalid” results, leaving 1,710 for comparison. Dräger performance at various quantitative cutoffs examined previously for smoking (due to proposed SAMHSA guidelines or utilized in the DRUID program) [33, 38, 39] is summarized in Online Resource 8. Alcohol presence did not affect Dräger performance. Overall sensitivity at the manufacturer-specified confirmation cutoff for THC of 5 µg/l was 60.8 % over 8.3 h. Specificity was high at 98.2 %, yielding 82.5 % overall efficiency. At lower Quantisal THC confirmation cutoffs, sensitivity decreased. Including CBD and CBN as required confirmatory analytes produced higher sensitivity [89.2 % (CBD) and 86.4 % (CBN)] for THC ≥2 µg/l and for THC ≥1 µg/l. These numbers were identical for both THC cutoffs because CBD and CBN were not present when THC <2 µg/l. This also explains the higher sensitivity, because fewer confirmatory specimens were considered positive when CBD or CBN were required. Detection rates (from the 19 completers) vs post-dose time for several possible confirmation criteria are presented in Fig. 4. Data were identical for THC ≥2 or 1 µg/l for completers. Dräger tlast for the various cutoffs are presented in Table 4 (low vs high, completers) and Online Resource 8 (full study population). Overall, the DrugTest 5000 was positive for THC 3.3 [0.17 to ≥8.3] h [median (range)] after dosing. The only significant high vs low t last difference among the various confirmation cutoffs was when CBD and THC were required. This corresponds to the finding that CBD had significantly later low vs high t last. To make a comparison to smoking a 6.8 % THC cigarette [32], the 546 tests (549, 3 “invalid”) from high-dose sessions were also evaluated (Table 5). Sensitivity for the high dose only increased relative to overall results (for all confirmation cutoffs except those requiring CBD), but sensitivity was lower after vaporization than after smoking [32].
Discussion
We present, for the first time, THC, CBD, CBN, and THCCOOH disposition in OF following controlled vaporized cannabis administration. Prior clinical data following cannabis vaporization are limited. One other study examined OF after vaporization, but specimens were only collected 0.08 and 1.3 h post-inhalation [13].
Our data represent a broad cannabis history spectrum, suggested by the highly variable self-report data, residual cannabinoids present in some participants at baseline, and large intersubject variability (discussed below). We only recruited individuals who self-reported cannabis intake ≤3×/week, less than our cutoff for chronic frequent smoking (≥4×/week) [33, 38, 39]. Although some current study participants were occasional smokers (≤2×/week), several fitted into an intermediate category (2 or 3×/week), including eight completers. After a night at the research unit, previous frequent smokers were still positive for THC and THCCOOH in 79 and 100 % of participants [39]. In contrast, participants’ OF baseline (10–16 h after admission) was still positive in half (THC) and one third (THCCOOH) of study sessions. Previous frequent smokers were 100 % negative for CBD and CBN after a night at the research unit [39], but we detected CBD and CBN in 1/163 and 4/163 baseline specimens. This study was conducted in a geographic region (Iowa City, IA, USA) different from our previous work (Baltimore, MD, USA). Possibly, typical cannabinoid potencies are different in the two areas. CBD and CBN are often identified as markers of recent intake [20, 38, 39]; it may be prudent to consider potency in consumed cannabis when evaluating time since exposure. CBD potency in particular may become more variable as medical and recreational cannabis decriminalization increase, because of its other pharmacological properties (antiemetic, antipsychotic, anti-inflammatory, antiepileptic) [40–42].
Three high-dose THC OF C max values, exceeding 20,000 µg/l, were among the highest ever reported [13, 20, 31, 38, 39, 43]. After vaporizing two successive THC doses 80 min apart, Wille et al. [13] found a median (range) OF THC concentration of 1,952 (77.7–12,360) ng/g. Another controlled cannabis (smoking) study utilizing the Quantisal device had lower median (range) THC C max [644 (68.0–10,284) µg/l] [20]. Our ranges were considerably wider, but medians at any dose were <1,000 µg/l (Table 2). These data resemble those of Toennes et al. [31, 43] after controlled smoking of cannabis of similar potency. Both administration routes showed large intersubject variability. In that study, median C max was 4,800 ng/g. One frequent smoker displayed 71,747 ng/g maximum OF THC [43], and 5 out of 17 frequent smokers attained OF THC >20,000 ng/g with 0.5–0.7 g/l blood alcohol [31]. The authors asserted that concentrations in ng/g are comparable to µg/l because OF specific gravity is only 0.2–1.2 % different from 1 kg/l. After our low and high doses without alcohol, 75 % of THC C max values were <1,589 and <3,933 µg/l, respectively, compared to 75 % of THC C max values ≤6,236 ng/g in the Toennes study [31]. With alcohol, 75 % were <2,811 and <5,288 µg/l in our study, compared to 74 % with alcohol ≤9,210 ng/g [31]. As in that study, our findings indicated that alcohol did not produce significant OF THC effects. Collectively, these data indicate that vaporization produces similar but slightly lower OF THC concentrations relative to smoking.
The relative lack of significant dose effects on cannabinoid C max and AUC0–8.3h values after high doses vs low doses suggests that several participants titrated their cannabis dose to individual subjective and cardiovascular comfort levels. Despite similar median THC C max across all active doses, ranges varied more than 1000-fold (Table 2). However, in only 3 of the 151 complete sessions was the cannabis balloon not fully inhaled. This occurred twice for the high dose without alcohol (Participants 19 and 20), and once for the low dose without alcohol (Participant 20). The balloons were left approximately one quarter full. Participant 19 had an OF THC C max of 477 µg/l with this unfinished balloon. For comparison, his C max at low dose/no alcohol and high dose/alcohol were 209 and 2,348 µg/l, respectively. This dose-dependent intrasubject variability markedly contrasts with Participant 20, who had similar C max values for high dose/no alcohol, low dose/no alcohol, and low dose/alcohol (746, 707, and 735 µg/l, respectively). This could indicate titration, particularly given that Participant 20 did not finish the balloon in two sessions (those without alcohol). Her high dose/alcohol session produced a C max of 951 µg/l. Apart from these three instances, participants consumed the entire bag, except for three other sessions that were terminated for drug-related adverse events [panic attack (Participant 23) and emesis/dizziness (Participants 29 and 31)]. In a recent survey of 96 people who vaporize cannabis (open-ended questions on “best” and “worst” characteristics of vaporizing), more than 10 % claimed it provided more effect for the same cannabis quantity; one respondent indicated it was “easy to consume too much” [44]. It is unclear from that survey whether anyone thought it had less effect. Considering that our participants usually finished the entire balloon, perhaps titration occurred instead by controlling inhalation rate and depth, and hold time in the lungs. These factors may affect absorption and true t max. Participants were allowed to inhale ad libitum over 10 min, and the first post-dose specimen was not collected until after the full time elapsed. Thus, cannabinoid concentrations may have peaked earlier. Individual vaporizer experiences vary considerably with cannabis history and inhalation topography, contributing to the substantial variability observed. Experienced smokers often achieve higher THC concentrations with more practiced inhalation technique and some tolerance to its effects. The within-subjects design of this study was advantageous, providing a framework for examining participants’ data relative to their own unique smoking patterns.
High initial OF THC, CBD, and CBN concentrations arise mainly from contamination of the oral mucosa during inhalation because of minimal transfer from blood to OF [11, 12, 20, 31, 39, 45]. However, this effect is strongest within the first 0.75 h of exposure, dissipating thereafter such that OF cannabinoids better correlate with plasma, possibly because of transmucosal absorption [11, 13, 46]. Vaporized THC, CBD, and CBN t max immediately followed inhalation (active doses), which is consistent with smoking data [31, 38, 39], except in two instances after the high dose without alcohol. Participant 3 had a high-dose t max of 1.4 h for THC, CBD, and CBN, but results were within ±10 % at 0.17 and 1.4 h (159 vs 165, 7.1 vs 7.7, and 6.1 vs 6.6 µg/l, respectively). For both specimens, the Quantisal adequacy indicator did not turn blue at 0.17 h, indicating insufficient sample volume. Dry mouth is a well-documented phenomenon following cannabis exposure [47, 48], possibly explaining these inconsistent results. The concentrations of these specimens were likely underestimated because of analysis without weight correction [39]. Even under these unusual circumstances, initial THC concentrations >100 µg/l greatly exceeded the proposed SAMHSA [16] and DRUID analytical [17] cutoffs (2 and 1 µg/l THC, respectively). Although the results may not be quantitatively accurate, short samples generally contain sufficient cannabinoid concentrations to document recent exposure.
Because THCCOOH is not present in smoke but passively diffuses into OF from the bloodstream, it can help differentiate acute passive exposure from active cannabis exposure [11, 47, 49, 50]. When present, THCCOOH is detected at low ng/l concentrations. Even after the high cannabis dose, THCCOOH was not detected in OF in some participants. The median C max−C 0 was similar to C max, but accounting for baseline concentrations produced much lower maximum THCCOOH C max values for all doses. This demonstrates new vs residual (built up with more frequent intake) cannabinoid concentrations. THCCOOH t max varied throughout the session, reflecting differential metabolic rates and residual cannabinoid concentrations.
Although our inclusion criteria targeted occasional to moderate cannabis intake (≥1×/3 months but ≤3 days/week over the past 3 months), Participants 6, 7, 10, 27, and 38’s baseline cannabinoids (THCCOOH ≥20 ng/l and THC ≥1 µg/l after an overnight stay, at least one baseline THCCOOH >100 ng/l) suggested these five individuals were frequent smokers. Occasional smokers did not meet these conditions after 13 h post-smoking in a recent study [38]. Fabritius et al. [51] found mean and maximum levels of THCCOOH of 100 ng/l and 500 ng/l at baseline in frequent smokers, but it is unclear how long participants were admitted prior to baseline. Other participants in the current study had THC ≥1 µg/l and THCCOOH ≥20 ng/l at baseline during some, but not all, of their sessions, and baseline THCCOOH never exceeded 100 ng/l.
Residual THC content in placebo cannabis was only 0.008 ± 0.002 %, but this low vaporized quantity still produced observable OF THC, shown by C max−C 0 >0. This effect was not limited to participants with residual THC at baseline. Concentrations were always <21.0 µg/l (for baseline-negative participants) in these cases and decreased more rapidly than active doses. OF THC and THCCOOH following placebo sessions are presented in Online Resource 6. In participants positive for THCCOOH on admission, concentrations usually decreased by baseline, but some remained consistent or increased. In baseline-positive participants, THCCOOH concentrations increased and decreased without pattern throughout the time course after placebo dosing. Participants negative for THCCOOH at baseline remained THCCOOH-negative throughout placebo sessions, except in two instances. In the placebo with alcohol session for Participant 11, residual THC decreased throughout the session from 96.3 µg/l on admission and 7.5 µg/l at baseline to 0.65 µg/l at 8.3 h; THCCOOH was 16.9 ng/l on admission, 0 ng/l at baseline, and 0 ng/l at all times post-dose except 1.4 h (15.7 ng/l). Considering that both positive THCCOOH specimens were near the LOQ of 15 ng/l, it is likely residual THCCOOH was just below this limit during that time. In the placebo with alcohol session for Participant 13, THC and THCCOOH were negative prior to dosing and at all times post-dose except 0.17 h (3.7 µg/l and 72.6 ng/l, respectively). THCCOOH detected in both of these placebo sessions was consistent with residual cannabinoids from previous self-administration. Toennes et al. [43] observed similar THC-positive OF specimens following controlled placebo-cannabis smoking, and Wille et al. [13] found OF THC concentrations up to 746 ng/g (median 8 ng/g, no reported baseline) after vaporized placebo cannabis. In those studies, THCCOOH was not quantified in OF. This observation will not likely confound OF THC interpretation in forensic cases, because outside the laboratory setting there is little cause to consume placebo cannabis.
OF THC and THCCOOH were detectable in Quantisal specimens ≥8.3 h post-dose after active cannabis, consistent with smoking administration. Further study is required to adequately assess extended detection times following vaporization. Previous studies after smoking one similar-potency cannabis cigarette documented THC and THCCOOH in some individuals’ OF ≥22 h [20, 47] or ≥30 h [38, 39] post-smoking, especially for frequent smokers. During sustained monitored abstinence in chronic frequent cannabis smokers, THC was often present 48 h after admission, and THCCOOH for many days [52]. Participants in the present study were screened as occasional or moderate smokers, but because some were more frequent smokers based on cannabinoid concentrations, we hypothesize that OF detection times would be similar to or higher than those for occasional smokers. Such data (THC 13.5 to ≥30 h, CBD 1–6 h, CBN 2–13.5 h, THCCOOH 0–28 h) exist for other collection devices (StatSure, Oral-Eze) [38, 39]; our CBD and CBN data appear similar. Quantisal was only characterized for frequent smokers (THC and THCCOOH 6 to ≥22 h, CBD and CBN 2 to ≥6 h) [20], with no collection times between 6 and 22 h.
Although no overall alcohol–cannabis interactive effects were statistically significant (Table 3), high-dose vs low-dose AUC0–8.3h was only significantly different with coadministered alcohol (Online Resource 2). In addition, alcohol produced later t last values for CBD and CBN after high doses (Online Resources 3 and 4). AUC and t last both rely on longer-term analyte measurements, extending beyond the primary absorption and distribution phases. If only AUC0–8.3h (THC) and tlast (CBD, CBN) were affected without impacting on C max or t max, this may imply that alcohol slowed excretion slightly. Limited other data exist on OF cannabis combined with alcohol. An early controlled-administration study noted lower THC concentrations (58.3, 73.5 µg/l) 1 h post-dose in two participants who drank 200 ml of beer immediately after smoking 10 mg of THC, relative to two others (250, 96.0 µg/l) who did not drink [53]. The authors concluded that the differences resulted from a “washing” effect from the drink. This is possible, but given the low number of participants, it may be difficult to draw such a conclusion. Equally likely, their observations may have reflected normal interindividual variability unrelated to the beverage. No OF was collected prior to 1 h post-dose and all participants were cannabis-naïve. Another study examining OF THC in concert with alcohol found no significant difference between alcohol conditions [31]. The authors further noted that drinking a 300-ml alcoholic beverage would not affect roadside THC detectability; our results concur. Despite similar blood alcohol AUC0–8.3h, THC appeared to slightly alter the alcohol absorption phase (Fig. 1; Table 2), producing significantly lower and later alcohol C max. This corroborates previous findings [54]. It is possible this resulted from the slowing effects of cannabinoids on gastrointestinal motility and decreased gastric emptying [55, 56], considering that alcohol is absorbed via passive diffusion along concentration gradients in the stomach and small intestine [57]. It is important to consider that the 1.4-h median alcohol t max after the high cannabis dose (rather than 0.42 h from the low dose) reflected the immediate next alcohol measurement time, so median t max data should be interpreted with caution.
Factors affecting apparent on-site performance include chosen confirmation cutoff, frequency of cannabis intake, time course, and administration route. The DrugTest 5000 demonstrated good specificity and efficiency for OF obtained over 8.3 h after cannabis vaporization in these occasional smokers, but sensitivity was lower than observed in frequent smokers after smoking a cannabis cigarette with the same THC potency (sensitivity 90.7 % at THC ≥2 µg/l) [32]. At this confirmation cutoff, we observed 47.0 % sensitivity, but 99.6 % specificity (because of few FP) for overall 70.1 % efficiency. Low vaporized sensitivity arose from high FN rates, even within the first 4.3 h post-dose. Figure 4 demonstrates the effect of different confirmation cutoffs when evaluating on-site Dräger screening performance. After active THC, 70.7 % of tests over the first 3.3 h were positive by Dräger and confirmed at THC ≥2 µg/l (SAMHSA proposed cutoff). At 5.3 and 8.3 h, detection rates were 28.9 and 14.9 %, respectively. Confirming with THC ≥ 2 µg/l or another analyte (CBD, CBN, or THCCOOH) produced the same results, showing that in this occasional/moderate smoker cohort, when the Dräger was positive and CBD, CBN, or THCCOOH were ≥1 µg/l, ≥1 µg/l, or ≥20 ng/l, respectively, THC was always ≥2 µg/l. THCCOOH was proposed as a potential additional confirmatory criterion because it helps rule out passive environmental exposure, detects oral cannabis use, and can extend detection windows in chronic frequent cannabis smokers [49, 52]. In this population, THCCOOH was not always detected; so including THCCOOH as a requirement for confirmation decreased sensitivity. Additional CBD or CBN ≥1 µg/l confirmation requirements increased apparent sensitivity relative to THC ≥1 µg/l or THC ≥2 µg/l only. However, this finding should be interpreted carefully, because it reflects CBD and CBN as recent-use cannabinoid markers. FN were reduced by requiring minor cannabinoid detection to be considered “positive”. This created an on-site detection window similar to the performance-impairment window [4, 6] (Table 4; Fig. 4). Although CBD and CBN may be markers of recent intake, their absence does not preclude it. CBD and CBN decreased confirmed detection rates especially after 4 h. In a study with a longer time course, requiring these markers for confirmation would decrease apparent sensitivity relative to our results [32]. Using the manufacturer-specified 5-µg/l THC screening cutoff as the confirmation cutoff showed 60.8 % sensitivity, 98.2 % specificity, and 82.5 % overall efficiency, higher than all other evaluated THC cutoffs except those additionally requiring CBD or CBN.
Our results are similar to an early roadside Dräger study whose authors also noted high numbers of FN [58]. In contrast, recent smoked and roadside studies demonstrated higher sensitivity (58.3–94.4 %), but lower specificity (15.4–75 %) sometimes resulting from few TN [29–32, 59]. Some of these studies only quantified plasma rather than OF confirmations during Dräger performance evaluation. THC cutoffs in plasma were 1–2 µg/l [29, 30], and in OF were 2–5 µg/l [31, 32]. Roadside studies may have inherently fewer TP than controlled-administration studies, decreasing apparent sensitivity and efficiency (which depend upon total detected TP). Alcohol produced no impact on Dräger performance post-smoking [31], agreeing with our findings post-vaporization. To date, the only other on-site testing device evaluated with vaporized cannabis, the DrugWipe-5S, produced remarkably similar results to the Dräger at a 1-µg/l OF THC cutoff. Wille et al. [13] observed 43, 100, and 57 % DrugWipe-5S sensitivity, specificity, and efficiency, respectively; here, Dräger performance was 40.4, 99.8, and 60.7 %.
Volatilization by hot air is a different heating mechanism from combustion, altering the properties of inhaled vapor vs smoke [22, 60, 61]. As far as we are aware, pH and other chemical properties of cannabis smoke and vapor are not yet elucidated, but tobacco smoke can vary even during the process of smoking a cigar [62]. Cannabis vapor may interact with oral mucosa differently to smoke, altering Dräger performance. Lower volatilization heating temperature (210 °C) releases less THC than smoking (≥230 °C) [22, 63], and some THC could adhere to the balloon [64]. Vaporization causes less exposure to combustion by-products, cannabinoids, and other chemicals [22, 23]. It is possible that lower THC contamination of oral mucosa contributed to the lower vaporized sensitivity. Another possible explanation is that OF collection with the Dräger collection device involves moving it throughout the entire mouth, mildly stimulating saliva production, whereas the Quantisal device is held sublingually. Dräger also recommends collecting the confirmation OF specimen first, which may help stimulate OF production. We followed these guidelines in specimen collection. Stimulation can decrease OF drug concentrations because of further dilution [65]. These and other factors may contribute to observed sensitivity differences relative to smoking. Finally, the time course of the current experiment was shorter than our previous studies, and doses included placebo, low (2.9 %), and a comparable (6.7 %) THC dose. Including only high-dose results (Table 5) increased sensitivity overall but still resulted in lower sensitivity relative to smoking [32]. Another possible consideration is that the THC cigarettes contained more total cannabis (0.79 g) than the amount vaporized (0.5 g).
Median Dräger tlast was 3–4 h for evaluated cutoffs, but for all cutoffs some specimens were positive after 8.3 h. This coincides with previous smoking findings, showing that some Dräger OF specimens were positive ≥4 h [31] and 6 to ≥22 h [32]. More recently, significant differences in Dräger t last were observed between occasional and frequent smokers when OF confirmation results also considered the presence of THCCOOH [33]. Dräger t last varied considerably overall and by chosen confirmation cutoff criteria, highlighting the importance of careful interpretation. Further study is required to determine extended detection windows following vaporization.
Conclusions
For the first time following controlled cannabis vaporization, we have documented cannabinoid disposition in OF over 8.3 h with and without low-dose alcohol, and evaluated the performance of an on-site screening device. The Dräger on-site device best reflected the cannabis impairment window when combined with the recent use markers CBD and CBN, because these analytes shortened the detection windows to approximately 2–4 h. However, possible increased variability in CBD potency may result in different or extended CBD detection; future research with cannabis containing higher CBD is recommended. Chosen confirmation cutoff, time since dosing, length of monitoring, frequency of use, and additional detected analytes all affect interpretation. The Dräger DrugTest 5000 displayed lower sensitivity after vaporization than smoking, but high specificity and comparable efficiency. Concurrent alcohol (albeit at least 10 min prior to vaporization) did not affect cannabinoid OF concentrations or on-site test sensitivity. Future studies should directly compare cannabis vaporization to smoking over extended periods.
References
Lacey JH, Kelley-Baker T, Furr-Holden D, Voas RB, Romano E, Ramirez A, Brainard K, Moore C, Torres P, Berning A (2009) 2007 National roadside survey of alcohol and drug use by drivers: drug results. DOT HS 811 249 National Highway Traffic Safety Administration Office of Behavioral Safety Research, Washington, DC
Davey J, Leal N, Freeman J (2007) Screening for drugs in oral fluid: Illicit drug use and drug driving in a sample of Queensland motorists. Drug Alcohol Rev 26:301–307
Poulsen H, Moar R, Troncoso C (2012) The incidence of alcohol and other drugs in drivers killed in New Zealand road crashes 2004–2009. Forensic Sci Int 223:364–370
Hartman RL, Huestis MA (2013) Cannabis effects on driving skills. Clin Chem 59:478–492
Ramaekers JG, Robbe HWJ, O’Hanlon JF (2000) Marijuana, alcohol and actual driving performance. Hum Psychopharm 15:551–558
Ramaekers J, Kauert G, Theunissen E, Toennes S, Moeller M (2009) Neurocognitive performance during acute THC intoxication in heavy and occasional cannabis users. J Psychopharmacol 23:266–277
Bosker WM, Theunissen EL, Conen S, Kuypers KP, Jeffery WK, Walls HC, Kauert GF, Toennes SW, Moeller MR, Ramaekers JG (2012) A placebo-controlled study to assess standardized field sobriety tests performance during alcohol and cannabis intoxication in heavy cannabis users and accuracy of point of collection testing devices for detecting THC in oral fluid. Psychopharmacology 223:439–446
Charlton SG, Starkey NJ (2013) Driver risk from blood alcohol levels between 50 mg/100 ml and 80 mg/100 ml. NZ Transport Agency Research Report Traffic and Road Safety Research Group. University of Waikato, Hamilton
Johnson MB, Kelley-Baker T, Voas RB, Lacey JH (2012) The prevalence of cannabis-involved driving in California. Drug Alcohol Depen 123:105–109
Rocky Mountain High Intensity Drug Trafficking Area (2013) The legalization of marijuana in Colorado: the impact 1:1–66
Bosker WM, Huestis MA (2009) Oral fluid testing for drugs of abuse. Clin Chem 55:1910–1931
Drummer OH (2006) Drug testing in oral fluid. Clin Biochem Rev 27:147–159
Wille SM, Di Fazio V, Toennes SW, van Wel JH, Ramaekers JG, Samyn N (2014) Evaluation of Δ9-tetrahydrocannabinol detection using DrugWipe5S screening and oral fluid quantification after Quantisal collection for roadside drug detection via a controlled study with chronic cannabis users. Drug Test Anal. doi:10.1002/dta.1660
Bogstrand ST, Gjerde H (2014) Which drugs are associated with highest risk for being arrested for driving under the influence? A case–control study. Forensic Sci Int 240:21–28
Kelley-Baker T, Moore C, Lacey JH, Yao J (2014) Comparing drug detection in oral fluid and blood: data from a national sample of nighttime drivers. Traffic Inj Prev 15:111–118
Substance Abuse and Mental Health Services Administration (SAMHSA) (2004) Notice of proposed revisions to the mandatory guidelines for federal workplace drug testing programs. Fed Regist 69:19673–19732
Pil K, Raes E, Van den Neste T, Verstraete A (2007) Toxicological analyses in the DRUID epidemiological studies: analytical methods, target analytes and analytical cut-offs. Paper presented at the The European Integrated Project DRUID 2007
Baggio S, Deline S, Studer J, Mohler-Kuo M, Daeppen JB, Gmel G (2014) Routes of administration of cannabis used for nonmedical purposes and associations with patterns of drug use. J Adolesc Health 54:235–240
Huestis MA, Henningfield JE, Cone EJ (1992) Blood cannabinoids I. Absorption of THC and formation of 11-OH-THC and THCCOOH during and after smoking marijuana. J Anal Toxicol 16:276–282
Lee D, Schwope DM, Milman G, Barnes AJ, Gorelick DA, Huestis MA (2012) Cannabinoid disposition in oral fluid after controlled smoked cannabis. Clin Chem 58:748–756
Huestis MA, Sampson AH, Holicky BJ, Henningfield JE, Cone EJ (1992) Characterization of the absorption phase of marijuana smoking. Clin Pharmacol Ther 52:31–41
Pomahacova B, Van der Kooy F, Verpoorte R (2009) Cannabis smoke condensate III: the cannabinoid content of vaporised Cannabis sativa. Inhal Toxicol 21:1108–1112
Fischedick J, Van Der Kooy F, Verpoorte R (2010) Cannabinoid receptor 1 binding activity and quantitative analysis of Cannabis sativa L. smoke and vapor. Chem Pharm Bull (Tokyo) 58:201–207
Abrams DI, Vizoso HP, Shade SB, Jay C, Kelly ME, Benowitz NL (2007) Vaporization as a smokeless cannabis delivery system: a pilot study. Clinic Pharmacol Ther 82:572–578
Zuurman L, Roy C, Schoemaker R, Hazekamp A, den Hartigh J, Bender J, Verpoorte R, Pinquier J, Cohen A, van Gerven J (2008) Effect of intrapulmonary tetrahydrocannabinol administration in humans. J Psychopharmacol 22:707–716
Van Dam NT, Earleywine M (2010) Pulmonary function in cannabis users: support for a clinical trial of the vaporizer. Int J Drug Policy 21:511–513
Earleywine M, Barnwell SS (2007) Decreased respiratory symptoms in cannabis users who vaporize. Harm Reduct J 4:11
Toennes SW, Kauert GF, Steinmeyer S, Moeller MR (2005) Driving under the influence of drugs—evaluation of analytical data of drugs in oral fluid, serum and urine, and correlation with impairment symptoms. Forensic Sci Int 152:149–155
Musshoff F, Hokamp EG, Bott U, Madea B (2014) Performance evaluation of on-site oral fluid drug screening devices in normal police procedure in Germany. Forensic Sci Int 238:120–124
Wille SM, Samyn N, Ramírez-Fernández Mdel M, De Boeck G (2010) Evaluation of on-site oral fluid screening using Drugwipe-5+, RapidSTAT and Drug Test 5000 for the detection of drugs of abuse in drivers. Forensic Sci Int 198:2–6
Toennes SW, Schneider K, Wunder C, Kauert GF, Moeller MR, Theunissen EL, Ramaekers JG (2013) Influence of ethanol on the pharmacokinetic properties of Δ9-tetrahydrocannabinol in oral fluid. J Anal Toxicol 37:152–158
Desrosiers NA, Lee D, Schwope DM, Milman G, Barnes AJ, Gorelick DA, Huestis MA (2012) On-site test for cannabinoids in oral fluid. Clin Chem 58:1418–1425
Desrosiers NA, Milman G, Mendu DR, Lee D, Barnes AJ, Gorelick DA, Huestis MA (2014) Cannabinoids in oral fluid by on-site immunoassay and by GC-MS using two different oral fluid collection devices. Anal Bioanal Chem 406:4117–4128
Lee D, Milman G, Schwope DM, Barnes AJ, Gorelick DA, Huestis MA (2012) Cannabinoid stability in authentic oral fluid after controlled cannabis smoking. Clin Chem 58:1101–1109
Milman G, Barnes AJ, Lowe RH, Huestis MA (2010) Simultaneous quantification of cannabinoids and metabolites in oral fluid by two-dimensional gas chromatography mass spectrometry. J Chromatogr A 1217:1513–1521
Welling PG, Lyons L, Elliott R, Amidon GL (1977) Pharmacokinetics of alcohol following single low doses to fasted and nonfasted subjects. J Clin Pharmacol 17:199–206
Wilkinson PK (1980) Pharmacokinetics of ethanol: a review. Alcoholism Clin Exp Res 4:6–21
Newmeyer MN, Desrosiers NA, Lee D, Mendu DR, Barnes AJ, Gorelick DA, Huestis MA (2014) Cannabinoid disposition in oral fluid after controlled cannabis smoking in frequent and occasional smokers. Drug Test Anal 6:1002–1010
Anizan S, Milman G, Desrosiers N, Barnes AJ, Gorelick DA, Huestis MA (2013) Oral fluid cannabinoid concentrations following controlled smoked cannabis in chronic frequent and occasional smokers. Anal Bioanal Chem 405:8451–8461
Bergamaschi M, Queiroz R, Zuardi A, Crippa J (2011) Safety and side effects of cannabidiol, a Cannabis sativa constituent. Curr Drug Saf 6:237–249
Bergamaschi MM, Queiroz RHC, Chagas MHN, de Oliveira DCG, De Martinis BS, Kapczinski F, Quevedo J, Roesler R, Schroder N, Nardi AE, Martin-Santos R, Hallak JEC, Zuardi AW, Crippa JAS (2011) Cannabidiol reduces the anxiety induced by simulated public speaking in treatment-naive social phobia patients. Neuropsychopharmacology 36:1219–1226
Szaflarski JP, Martina Bebin E (2014) Cannabis, cannabidiol, and epilepsy—from receptors to clinical response. Epilepsy Behav. doi:10.1016/j.yebeh.2014.08.135
Toennes SW, Ramaekers JG, Theunissen EL, Moeller MR, Kauert GF (2010) Pharmacokinetic properties of Δ9-tetrahydrocannabinol in oral fluid of occasional and chronic users. J Anal Toxicol 34:216–221
Malouff JM, Rooke SE, Copeland J (2014) Experiences of marijuana-vaporizer users. Subst Abus 35:127–128
Lee D, Vandrey R, Mendu DR, Murray JA, Barnes AJ, Huestis MA (2014) Oral fluid cannabinoids in chronic frequent cannabis smokers during ad libitum cannabis smoking. Drug Test Anal. doi:10.1002/dta.1718
Huestis MA, Cone EJ (2004) Relationship of Δ9-tetrahydrocannabinol concentrations in oral fluid and plasma after controlled administration of smoked cannabis. J Anal Toxicol 28:394–399
Milman G, Schwope DM, Gorelick DA, Huestis MA (2012) Cannabinoids and metabolites in expectorated oral fluid following controlled smoked cannabis. Clin Chim Acta 413:765–770
Verstraete AG (2005) Oral fluid testing for driving under the influence of drugs: history, recent progress and remaining challenges. Forensic Sci Int 150:143–150
Moore C, Coulter C, Uges D, Tuyay J, van der Linde S, van Leeuwen A, Garnier M, Orbita J Jr (2011) Cannabinoids in oral fluid following passive exposure to marijuana smoke. Forensic Sci Int 212:227–230
Milman G, Barnes AJ, Schwope DM, Schwilke EW, Darwin WD, Goodwin RS, Kelly DL, Gorelick DA, Huestis MA (2010) Disposition of cannabinoids in oral fluid after controlled around-the-clock oral THC administration. Clin Chem 56:1261–1269
Fabritius M, Chtioui H, Battistella G, Annoni JM, Dao K, Favrat B, Fornari E, Lauer E, Maeder P, Giroud C (2013) Comparison of cannabinoid concentrations in oral fluid and whole blood between occasional and regular cannabis smokers prior to and after smoking a cannabis joint. Anal Bioanal Chem 405:9791–9803
Lee D, Milman G, Barnes AJ, Goodwin RS, Hirvonen J, Huestis MA (2011) Oral fluid cannabinoids in chronic, daily cannabis smokers during sustained, monitored abstinence. Clin Chem 57:1127–1136
Maseda C, Hama K, Fukui Y, Matsubara K, Takahashi S, Akane A (1986) Detection of Δ9-THC in saliva by capillary GC/ECD after marihuana smoking. Forensic Sci Int 32:259–266
Lukas SE, Benedikt R, Mendelson JH, Kouri E, Sholar M, Amass L (1992) Marihuana attenuates the rise in plasma ethanol levels in human subjects. Neuropsychopharmacology 7:77–81
Abalo R, Vera G, Lopez-Perez AE, Martinez-Villaluenga M, Martin-Fontelles MI (2012) The gastrointestinal pharmacology of cannabinoids: focus on motility. Pharmacology 90:1–10
Izzo AA, Sharkey KA (2010) Cannabinoids and the gut: new developments and emerging concepts. Pharmacol Therapeut 126:21–38
Dubowski KM (1985) Absorption, distribution and elimination of alcohol: highway safety aspects. J Stud Alcohol 10:98–108
Laloup M, del Mar Ramirez Fernandez M, Wood M, De Boeck G, Maes V, Samyn N (2006) Correlation of Δ9-tetrahydrocannabinol concentrations determined by LC-MS-MS in oral fluid and plasma from impaired drivers and evaluation of the on-site Dräger DrugTest. Forensic Sci Int 161:175–179
Logan BK, Mohr AL, Talpins SK (2014) Detection and prevalence of drug use in arrested drivers using the Dräger Drug Test 5000 and Affiniton DrugWipe oral fluid drug screening devices. J Anal Toxicol 38:444–450
Gieringer D, St. Laurent J, Goodrich S (2004) Cannabis vaporizer combines efficient delivery of THC with effective suppression of pyrolytic compounds. J Cannab Therapeut 4:7–27
Chemic Laboratories (2003) Evaluation of Volcano vaporizer for the efficient emission of THC, CBD, CBN and the significant reduction and/or elimination of polynuclear-aromatic (PNA) analytes resultant of pyrolysis. Report No. 1311619-0103-2563, Canton; pp 1–57
Henningfield JE, Fant RV, Radzius A, Frost S (1999) Nicotine concentration, smoke pH and whole tobacco aqueous pH of some cigar brands and types popular in the United States. Nicotine Tob Res 1:163–168
Hazekamp A (2010) The Volcano Medic cannabis vaporizer: optimal temperature for single-dose administration of 100 mg cannabis or 10 mg dronabinol. LabAssistent Phytochemical Services Project No. 2010-003c, Leiden; pp 1–13
Hazekamp A, Ruhaak R, Zuurman L, van Gerven J, Verpoorte R (2006) Evaluation of a vaporizing device (Volcano) for the pulmonary administration of tetrahydrocannabinol. J Pharm Sci 95(6):1308–1317
Drummer OH (2005) Review: pharmacokinetics of illicit drugs in oral fluid. Forensic Sci Int 150:133–142
Acknowledgments
We thank the nurses and staff of the University of Iowa Clinical Research Unit, as well as the staff of the National Advanced Driving Simulator, for contributions to data collection. We further acknowledge Cheryl Roe, Jennifer Henderson, Rose Schmitt, and Kayla Smith for data assembly and coordination, and Allan J. Barnes for instrumentation expertise. We acknowledge the University of Maryland, Baltimore Toxicology Program, and the Graduate Partnership Program, National Institutes of Health (NIH). The Dräger DrugTest 5000, Quantisal, and Volcano devices and supplies were provided by the manufacturers to NIH through Materials Transfer Agreements. This research was funded by the Intramural Research Program, National Institute on Drug Abuse, NIH, the United States Office of National Drug Control Policy, and the National Highway Traffic Safety Administration.
Conflict of interest
Ms. Hartman and Drs. Anizan, Jang, Yun, Gorelick, and Huestis report research funding through interagency agreements from the National Highway Traffic Safety Administration and the Office of National Drug Control Policy; and nonfinancial support (devices provided via Materials Transfer Agreements) from Storz-Bickel, Immunalysis, and Dräger, during the course of the study. Dr. Yun additionally reports grant funding from the National Key Technology R&D Program of China (2012BAK02B02-2). Drs. Brown, Milavetz, Spurgin, and Gaffney report contract research funding from the National Highway Traffic Safety Administration, the Office of National Drug Control Policy, and the National Institute on Drug Abuse; and nonfinancial support (devices provided via Materials Transfer Agreements) from Storz-Bickel, Immunalysis, and Dräger, during the course of the study. No commercial organization participated in study design, data analysis, or manuscript writing.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Hartman, R.L., Anizan, S., Jang, M. et al. Cannabinoid disposition in oral fluid after controlled vaporizer administration with and without alcohol. Forensic Toxicol 33, 260–278 (2015). https://doi.org/10.1007/s11419-015-0269-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11419-015-0269-6