Abstract
The association between depression and dementia, particularly Alzheimer’s disease (AD) and cerebrovascular disease (CVD), remains an active area of research. This study aimed to investigate the relationship between a history of depression and biomarkers of AD and CVD in patients with dementia in a clinical setting. A total of 126 patients from the University Health Network (UHN) Memory Clinic with comprehensive clinical evaluations, including neuropsychological testing and medical examinations, were included. Lumbar puncture was performed to collect cerebrospinal fluid (CSF) for biomarker analysis, and brain magnetic resonance imaging (MRI) scans were obtained to assess white matter hyperintensity (WMH) burden. The presence of depression was determined through medical records. The study findings did not reveal significant differences between participants with and without a history of depression in terms of AD biomarkers, WMH burden, neurofilament light chain levels, cognitive scores, age of symptom onset, disease duration, or vascular risk scores. Logistic regression analysis did not indicate a meaningful predictive value of these variables for depression status. This clinical study contributes to our understanding regarding the association between depression and AD/CVD biomarkers in patients with cognitive impairment. Further research is needed to elucidate the complex relationship between depression and dementia and to explore the potential mechanisms linking depression, AD, and CVD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A growing body of research has explored the association between depression and dementia where individuals with a history of depression are not only at an increased risk of developing dementia, particularly Alzheimer’s disease (AD), but also have been reported to demonstrate accelerated cognitive decline [1,2,3]. The cognitive domains most consistently affected by depression include attention, executive functioning, processing speed, and memory [4]. The severity and extent of cognitive deficits in individuals with depression can vary widely, depending on factors such as the severity of the depressive episode, age, and comorbidities [5]. Moreover, while some cognitive impairments may persist even after the resolution of depressive symptoms, others may improve with successful treatment of depression [6].
Rather than a risk factor, one theory posits that depression may be an early symptom of AD [7]. In this view, depressive symptoms could arise from the same neurobiological changes that eventually lead to AD, such as amyloid-beta (Aβ) accumulation, tau pathology, and neuronal loss [8]. In older individuals without cognitive deficits, depression has been correlated with increased amyloid burden [9, 10]. Furthermore, higher levels of plasma Aβ42 have been linked to the development of late-life depression and the progression to AD [11].
Cerebrovascular disease (CVD), as represented by white matter hyperintensities (WMH), has been increasingly recognized as an important factor associated with AD. WMH are commonly observed on brain magnetic resonance imaging (MRI) scans and represent areas of white matter injury, often resulting from small vessel ischemic disease or other vascular-related changes [12].
The relationship between WMH and AD is complex, with several potential mechanisms linking the two conditions. First, WMH might contribute to the development of AD by disrupting the brain’s structural and functional connectivity, leading to cognitive decline and increased vulnerability to neurodegenerative processes [13]. Second, CVD and AD share common risk factors, such as hypertension, diabetes, and dyslipidemia, which can independently affect the brain’s vasculature and contribute to both WMH and AD pathology [14, 15]. Moreover, the presence of WMH may exacerbate the cognitive decline in AD by affecting the brain’s ability to compensate for the neuronal damage caused by AD pathology [16]. Some studies have found that individuals with both AD and WMH show a more rapid cognitive decline than those with AD alone [17].
There is also a significant relationship between CVD and depression as several studies demonstrate that CVD increases the risk of developing depressive symptoms, particularly in older adults [18, 19]. The mechanisms underlying the relationship between CVD and depression are multifaceted and may involve both direct and indirect pathways. Directly, CVD can result in ischemic lesions or WMH in brain regions involved in mood regulation, such as the prefrontal cortex, anterior cingulate cortex, and limbic system, thereby increasing the risk of depression [20, 21]. Additionally, CVD can disrupt the brain’s structural and functional connectivity, potentially affecting mood-regulating networks [22].
Indirectly, CVD may contribute to depression through shared risk factors, such as hypertension, diabetes, smoking, and obesity [23]. These risk factors can have adverse effects on both vascular and neural functioning, which may increase susceptibility to depressive symptoms. Furthermore, the presence of CVD may lead to increased disability, reduced quality of life, and social isolation, all of which could contribute to the development or exacerbation of depression [19].
To date, much of the research surrounding depression and either AD or CVD is conducted with participants specifically recruited for research studies. While there are strengths to this approach, there are several advantages to using a sample of clinical care or “real-world” patients. First, research study participants are often selected based on strict inclusion and exclusion criteria, potentially leading to a more homogenous sample that may not accurately represent the broader population of individuals with dementia [24]. Furthermore, research studies that recruit volunteers may be prone to selection bias, as individuals who choose to participate in such studies might be more motivated, have better access to healthcare, or have higher levels of education and social support [25]. Furthermore, it has been shown repeatedly that there is a lack of diversity in these studies, which comprised higher than census White participants and less women than seen in disease demographics when it comes to AD [26, 27]. This self-selection can limit the generalizability of the study findings. Conversely, clinical care patients may provide a more representative sample of the general dementia population, as they are not self-selected based on interest or motivation to participate in research. A disadvantage of employing a clinical care-based study approach is that clinical care patients with dementia may represent a more clinically severe cohort with more comorbid medical conditions compared to individuals recruited for research studies [28].
The aim of our study was to examine the association between a history of depression and biomarkers of AD and CVD in patients with cognitive impairment in a clinical “real-world” setting.
Materials and methods
Sample
The 126 patients included in this study presented to the UHN Memory Clinic (Toronto, ON, CA) with cognitive concerns and subsequently underwent a lumbar puncture for investigation of AD biomarkers. Given the exploratory nature of our study, no power analysis was conducted, as we included all patients who consented to participating. Individuals underwent a comprehensive clinical evaluation by a team of licensed medical professionals (neurologists, geriatric psychiatrists, geriatricians, nurse, social work, and occupational therapy), which included neuropsychological testing (i.e., Toronto Cognitive Assessment [29] or Montreal Cognitive Assessment [30]) and medical examination (i.e., history and physical). Patients were followed longitudinally with regular biannual visits. We conducted a retrospective review of clinical charts and obtained the following data: demographics (age, sex, education, and ethnicity), age of symptom onset, disease duration, medical comorbidities, and anti-depressant use. Informed consent was obtained from patients prior to data access.
Diagnosis of depression
As part of the diagnostic evaluation for patients presenting with memory concerns, the contribution of affective disorders, such as major depressive disorder, was assessed. A thorough history of previous psychiatric illness was also obtained. In our study, we classified patients positive for a history of depression by the presence of a past major depressive disorder diagnosis in their medical record. None of the patients included were actively depressed.
CSF collection and analysis
All patients underwent lumbar puncture and cerebrospinal fluid (CSF) analysis as part of their diagnostic evaluation. An ELISA was used to measure concentrations of Aβ42 (Innotest β-amyloid (1–42), Fujirebio), phosphorylated-tau (Innotest phospho-tau (181p), Fujirebio), and total-tau (Innotest hTAU-Ag, Fujirebio), and the results were interpreted according to clinically validated guidelines (Athena Diagnostics). CSF biomarkers were considered consistent with AD diagnosis (AD+) if phosphorylated tau > 68 pg/mL and Aβ42 to total tau index (ATI; calculated as (Aβ1–42)/(240 + 1.18 (t-tau))) < 0.8 [31,32,33]. A single molecule array (SIMOA) (Simoa NF-Light (SR-X) Advantage Kit or Simoa® Neuro 2-Plex B Advantage Kit) was used to measure concentration of neurofilament light chain (NfL), a non-specific marker of neurodegeneration [34].
Assessment of WMH burden
Clinical MRI imaging conducted within 6 months of CSF collection as part of routine diagnostic work-up was obtained for all participants. All of the fluid-attenuated inversion recovery (FLAIR) scans were examined by a trained neurologist (MCT) and classified according to the Fazekas scale [35]. For a subset of participants (n = 39), WMH volumes were also obtained from the raw FLAIR scans using an automated lesion segmentation approach. Lesions were segmented by the lesion prediction algorithm (Schmidt, 2017, Chapter 6.1), as implemented in the LST toolbox version 3.0.0 (www.statistical-modelling.de/lst.html) for SPM, at an initial threshold of 0.5 based on a Dice coefficient.
Cognitive testing
All patients underwent neuropsychological testing consisting of a Toronto Cognitive Assessment (TorCA) [29] at initial consult followed by Montreal Cognitive Assessments (MoCA) at 6-month follow ups. When deemed clinically necessary, the TorCA was repeated at follow up. The TorCA is a standardized neuropsychological test that is designed to detect changes [29]. Normative data for the TorCA were derived from large samples (n = 303) of healthy individuals spanning different age groups, education levels, and other demographic factors [29]. Cognitive testing conducted within 6 months of the LP was used to assign participants a global cognitive score as a measure of global impairment. For the cognitive scores, Z scores were calculated using either the TorCA or MoCA for each participant depending upon which test was closest to the lumbar puncture.
Vascular risk score
Patients were considered to have vascular risk factors if any of the following conditions were present in their medical records: myocardial infarction, angina, history of smoking, hypertension, stroke, hypercholesterolemia, diabetes, or use of anti-hypertensive medication [69]. A vascular risk score was calculated for each patient by summing the number of vascular risk factors present.
Statistical analysis
Statistical analysis was conducted using SPSS software (IBM SPSS 28). To identify group differences between those with a history of depression (Past Depression+) and those without (Past Depression− among demographics, age of symptom onset, AD status, WMH lesion volume, NfL levels, cognitive scores, and vascular scores, two-tailed independent sample t-test were used for continuous variables and chi-square test for categorical variables. An alpha of 0.003 denoted statistical significance after correcting for multiple comparisons.
A binary logistic regression model was used with depression status as the dependent variable. Age of symptom onset, WMH lesion volume (denoted as WMH in the model), NfL level, and cognitive scores were included as continuous predictor variables. Sex and AD status were included as categorical predictor variables.
Results
Participants
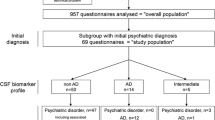
We obtained a sample of convenience consisting of 126 patients seen from October 2012 to February 2022, who had cognitive complaints, underwent CSF analysis for assessment of AD, agreed to contribute CSF to a research study on neurodegenerative diseases, and were diagnosed with a neurodegenerative disease as the cause of their cognitive impairment. All the patients included met criteria for dementia. The patients’ diagnoses were made according to the latest criteria and included AD [36], FTD and related FTD disorders [37, 38], vascular dementia [39], Lewy Body disease [40], and Parkinson’s disease [41]. Fig. 1 summarizes participant inclusion and exclusion and provides a breakdown of diagnosis categories for the patients included in our study. In brief, we excluded a total of 41 patients: 23 patients with MRI results that showed co-morbid pathologies that prevented accurate delineation of WMH (e.g., amyloid angiitis, and cerebral amyloid angiopathy); 7 patients whose cognitive impairment is not related to a neurodegenerative process (i.e., psychiatric, neurodevelopmental, or related to a traumatic brain injury); 6 patients whose clinical diagnoses were still being investigated/not confirmed at study onset; and 5 patients with subjective cognitive impairment. Table 1 provides demographic information of the 20 Past Depression+ patients and 65 Past Depression− patients. The sample was composed of predominantly White individuals (69.4%). Age, sex, self-reported race/ethnicity, or education did not differ between Past Depression+ and Past Depression− patients. Most patients in both groups were diagnosed with AD; however, FTD and related disorders, Lewy Body disease, Parkinson’s disease, and vascular dementia were also observed. This study was approved by the Research Ethics Board of the University Health Network, and written consent was obtained from all participants.
CSF biomarkers, WMH, cognitive performance, and vascular risk score
Table 2 summarizes the CSF biomarker, WMH lesion volume, cognitive performance and vascular risk scores in Past Depression+ and Past Depression−. Past Depression+ had a higher incidence of anti-depressant use compared to Past Depression− (X2(1, N = 85) = 14.6, p < 0.001). All Past Depression− who used anti-depressants (n = 13) did so for the off-label treatment of anxiety. No differences were observed in AD status, age of symptom onset, cognitive score, WMH lesion volume, vascular risk score, or NfL levels. Trends towards higher Fazekas scores in Past Depression− patients and a higher proportion of females with depression in Past Depression+ patients. However, these trends did not meet statistical significance after correcting for multiple comparisons.
Binary logistic regression
Table 3 summarizes the results of the binary logistic regression model. Age of symptom onset, sex, AD status, WMH lesion volume, NfL levels, cognitive score, or vascular risk scores were not statistically significant predictors of depression status.
Discussion
Our study focused on a sample of memory clinic patients with cognitive impairment to examine the association of past depression and several CSF and imaging biomarkers of AD, CVD, and neurodegeneration. We did not observe significant differences between Past Depression+ and Past Depression− participants in AD biomarkers, WMH burden, NfL levels, age of symptom onset, disease duration, vascular risk scores, or cognitive scores. Furthermore, these variables did not meaningfully predict depression status.
The relationship between depression and dementia is complex, with various hypotheses suggesting that depression may be an early symptom, reaction, or even a causal factor for dementia (Lenoir et al., 2011). Butters et al. [41] proposed the “multiple pathways model,” which considers brain and cognitive reserve. Depression is proposed to damage neurons through various mechanisms, including vascular disease [42], inflammation [43], elevated glucocorticoid production [44], and amyloid deposition [45]. These pathways lower reserve, leading to earlier or more frequent cognitive impairment contributing to dementia. The synergistic nature of these processes may explain the variability in presentation.
The timing of depression is important. Early-life depression (defined as a major depressive episode occurring before age 60 or 65) has been linked to a more than twofold increase in dementia risk [3, 46]. However, the relationship between late-life depression and dementia risk is unclear, with some studies suggesting late-life depression may be a prodrome to dementia rather than a risk factor [47]. It is important to note that several studies have failed to find an association between depression and dementia [48,49,50,51]. Our study also failed to find an association between early-life depression and AD.
One potential explanation for the inconsistency in the association of depression and dementia can be attributed to the broadness of the concept of depression itself. Depression is a highly heterogeneous disorder diagnosed based on a wide range of symptoms, such as persistent sadness, loss of interest, changes in appetite, and sleep disturbances, among others, with varying degrees of severity [52, 53]. Individuals diagnosed with depression may have different symptom profiles, making it difficult to identify a single, unified biological mechanism [1]. As well, there is likely a significant difference between patients with single episodes of depression compared to those with repeated, refractory depression [54, 55]. This heterogeneity has led some researchers to argue that depression should be considered a spectrum of related disorders, rather than a single diagnostic entity [56].
Certain symptoms of depression may have a stronger association with dementia risk than others. Apathy, characterized by a lack of motivation, interest, and emotional engagement, has been identified as a key neuropsychiatric symptom associated with an increased risk of cognitive decline and dementia [57, 58]. One study found that older adults with apathy, but without depression, were more likely to develop dementia than those with depression but without apathy [58]. Other depressive symptoms, however, such as sadness, may not be as strongly linked with dementia risk. Some research suggests that the presence of depressive symptoms without the core emotional feature of sadness, referred to as “depression without sadness,” may be more strongly associated with dementia risk [59]. Sleep disturbances such as insomnia or excessive sleepiness, may contribute to cognitive decline and the development of dementia by affecting the clearance of Aβ and disrupting the regulation of various neural and metabolic processes [60]. Our small sample size and lack of historical details surrounding the depressive episodes of our patients precluded an analysis of depression subtypes.
The strength of our study is our inclusion of clinic patients with CSF and neuroimaging biomarkers of AD and CVD. As noted above, including clinical patients as opposed to research participants provides the advantage of a more representative sample of the general dementia population. In addition to investigating the association between depression and AD, we also evaluated the effect of past depression on other neurodegenerative diseases, but no differences were noted. However, the range of clinical phenotypes observed in our patient population may have influenced the association between depression and dementia. For example, depression is frequently observed in and associated with an increased risk of AD [1,2,3], Parkinson’s Disease Dementia [61, 62], Lewy Body Dementia [63] and FTD [37]. However, in primary progressive aphasia, a rare form of FTD characterized by the progressive decline of language abilities, the association with depression is not as well established [64]. It is important to note that the relationship between depression and various types of dementia is an ongoing area of research. As new studies are conducted, our understanding of these relationships may change.
A limitation of our study is that our definition of depression lacks a certain degree of objectivity given that we relied on self-reporting. Generally, using standardized diagnostic criteria such as the Diagnostic and Statistical Manual of Mental Disorders (DSM) provides a more accurate and consistent measure of the incidence of depression compared to self-reported diagnoses, which are subject to recall bias and tend to underestimate prevalence [65, 66]. However, even with the use of well-validated diagnostic criteria of the DSM-5, diagnosing a remote major depressive episode remains relatively unreliable [67, 68]. The patients in our study were closely followed for years by a multi-disciplinary healthcare team consisting of neurologists, psychiatrists, and nurses. Each time the patients were assessed, careful attention was paid to psychiatric histories given that identifying the etiology of cognitive impairment requires the ruling out of comorbid psychiatric illness that may be confounding the clinical picture.
Another limitation of our study surrounds generalizability from the small sample size and lack of ethnic diversity. We also relied on clinical MR images obtained from different scanners. Variability in scanner-specific factors such as magnetic field strength, pulse sequences, and image resolution can lead to differences in image contrast, signal-to-noise ratio, and other aspects of image quality, which in turn can affect the accuracy and reliability of WMH lesion volume measurements. However, the automated segmentation algorithm we implemented has been shown to be robust to scanner-specific differences [68].
In conclusion, our study investigated the association between a history of depression and biomarkers of AD, CVD, and neurodegeneration in patients with dementia. We did not find significant differences in these biomarkers between patients with and without a history of depression, and these variables did not predict depression status. The relationship between depression and dementia is complex, with heterogeneity in depressive symptoms and the potential impact of specific symptoms on dementia risk. Further research with larger sample sizes and significantly greater diversity with respect to factors including but not limited to ethnicity and diseases is needed to understand the connection between depression and dementia, considering different depressive symptom profiles and specific types of dementia.
Data availability
The data supporting the findings of this study are available on reasonable request from the corresponding author.
References
Byers AL, Yaffe K. Depression and risk of developing dementia. Nat Rev Neurol. 2011;7:323–31.
Diniz BS, Butters MA, Albert SM, Dew MA, Reynolds CF. Late-life depression and risk of vascular dementia and Alzheimer’s disease: systematic review and meta-analysis of community-based cohort studies. Br J Psychiatry. 2013;202:329–35.
Livingston G, Huntley J, Sommerlad A, Ames D, Ballard C, Banerjee S, Brayne C, Burns A, Cohen-Mansfield J, Cooper C, Costafreda SG, Dias A, Fox N, Gitlin LN, Howard R, Kales HC, Kivimäki M, Larson EB, Ogunniyi A, et al. Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. Lancet. 2020;396:413–46.
Rock PL, Roiser JP, Riedel WJ, Blackwell AD. Cognitive impairment in depression: a systematic review and meta-analysis. Psychol Med. 2014;44:2029–40.
Bora E, Harrison BJ, Yücel M, Pantelis C. Cognitive impairment in euthymic major depressive disorder: a meta-analysis. Psychol Med. 2013;43:2017–26.
Bortolato B, Miskowiak KW, Köhler CA, Maes M, Fernandes BS, Berk M, Carvalho AF. Cognitive remission: a novel objective for the treatment of major depression? BMC Med. 2016;14:9
Geda YE, Roberts RO, Knopman DS, Petersen RC, Christianson TJH, Pankratz VS, Smith GE, Boeve BF, Ivnik RJ, Tangalos EG, Rocca WA. Prevalence of neuropsychiatric symptoms in mild cognitive impairment and normal cognitive aging: population-based study. Arch Gen Psychiatry. 2008;65:1193–8.
Jack CR, Knopman DS, Jagust WJ, Shaw LM, Aisen PS, Weiner MW, Petersen RC, Trojanowski JQ. Hypothetical model of dynamic biomarkers of the Alzheimer’s pathological cascade. Lancet Neurol. 2010;9:119–28.
Yasuno F, Kazui H, Morita N, Kajimoto K, Ihara M, Taguchi A, Yamamoto A, Matsuoka K, Kosaka J, Kudo T, Iida H, Kishimoto T, Nagatsuka K. High amyloid-β deposition related to depressive symptoms in older individuals with normal cognition: a pilot study. Int J Geriatr Psychiatry. 2016;31(8):920–8.
Donovan NJ, Locascio JJ, Marshall GA, Gatchel J, Hanseeuw BJ, Rentz DM, Johnson KA, Sperling RA. Longitudinal association of amyloid beta and anxious-depressive symptoms in cognitively normal older adults. Am J Psychiatry. 2018;175:530–7.
Blasko I, Kemmler G, Jungwirth S, Wichart I, Krampla W, Weissgram S, Jellinger K, Tragl KH, Fischer P. Plasma amyloid beta-42 independently predicts both late-onset depression and Alzheimer disease. Am J Geriatr Psychiatry. 2010;18:973–82.
Wardlaw JM, Valdés Hernández MC, Muñoz-Maniega S. What are white matter hyperintensities made of? Relevance to vascular cognitive impairment. J Am Heart Assoc. 2015;4:001140.
Prins ND, Scheltens P. White matter hyperintensities, cognitive impairment and dementia: an update. Nat Rev Neurol. 2015;11:157–65.
Toledo JB, Arnold SE, Raible K, Brettschneider J, Xie SX, Grossman M, Monsell SE, Kukull WA, Trojanowski JQ. Contribution of cerebrovascular disease in autopsy confirmed neurodegenerative disease cases in the National Alzheimer’s Coordinating Centre. Brain. 2013;136:2697–706.
Kivipelto M, Ngandu T, Fratiglioni L, Viitanen M, Kåreholt I, Winblad B, Helkala EL, Tuomilehto J, Soininen H, Nissinen A. Obesity and vascular risk factors at midlife and the risk of dementia and Alzheimer disease. Arch Neurol. 2005;62:1556–60.
Wardlaw JM, Smith EE, Biessels GJ, Cordonnier C, Fazekas F, Frayne R, Lindley RI, O’Brien JT, Barkhof F, Benavente OR, Black SE, Brayne C, Breteler M, Chabriat H, DeCarli C, de Leeuw FE, Doubal F, Duering M, Fox NC, Greenberg S, Hachinski V, Kilimann I, Mok V, van Oostenbrugge R, Pantoni L, Speck O, Stephan BCM, Teipel S, Viswanathan A, Werring D, Chen C, Smith C, van Buchem M, Norrving B, Gorelick PB, Dichgans M. Neuroimaging standards for research into small vessel disease and its contribution to ageing and neurodegeneration. Lancet Neurol. 2013;12:822–38.
Brickman AM, Provenzano FA, Muraskin J, Manly JJ, Blum S, Apa Z, Stern Y, Brown TR, Luchsinger JA, Mayeux R. Regional white matter hyperintensity volume, not hippocampal atrophy, predicts incident Alzheimer disease in the community. Arch Neurol. 2012;69:1621–7.
Alexopoulos GS. The vascular depression hypothesis: 10 years later. Biol Psychiatry. 2006;60:1304–5.
Lohner V, Brookes RL, Hollocks MJ, Morris RG, Markus HS. Apathy, but not depression, is associated with executive dysfunction in cerebral small vessel disease. PLoS One. 2017;12
Taylor WD, Aizenstein HJ, Alexopoulos GS. The vascular depression hypothesis: mechanisms linking vascular disease with depression. Mol Psychiatry. 2013;18:963–74.
Aizenstein HJ, Andreescu C, Edelman KL, Cochran JL, Price J, Butters MA, Karp J, Patel M, Reynolds CF. fMRI correlates of white matter hyperintensities in late-life depression. Am J Psychiatry. 2011;168:1075–82.
Gerritsen L, Comijs HC, Van Der Graaf Y, Knoops AJG, Penninx BWJH, Geerlings MI. Depression, hypothalamic pituitary adrenal axis, and hippocampal and entorhinal cortex volumes--the SMART Medea study. Biol Psychiatry. 2011;70:373–80.
Musselman DL, Evans DL, Nemeroff CB. The relationship of depression to cardiovascular disease: epidemiology, biology, and treatment. Arch Gen Psychiatry. 1998;55:580–92.
Katz MJ, Lipton RB, Hall CB, Zimmerman ME, Sanders AE, Verghese J, Dickson DW, Derby CA. Age-specific and sex-specific prevalence and incidence of mild cognitive impairment, dementia, and Alzheimer dementia in blacks and whites: a report from the Einstein Aging Study. Alzheimer Dis Assoc Disord. 2012;26:335–43.
Cherry MG, Taylor PJ, Brown SL, Rigby JW, Sellwood W. Guilt, shame and expressed emotion in carers of people with long-term mental health difficulties: a systematic review. Psychiatry Res. 2017;249:139–51.
Low LF, Barcenilla-Wong AL, Brijnath B. Including ethnic and cultural diversity in dementia research. Med J Aust. 2019;211:345–346.e1.
Babulal GM, Quiroz YT, Albensi BC, Arenaza-Urquijo E, Astell AJ, Babiloni C, Bahar-Fuchs A, Bell J, Bowman GL, Brickman AM, Chételat G, Ciro C, Cohen AD, Dilworth-Anderson P, Dodge HH, Dreux S, Edland S, Esbensen A, Evered L, et al. Perspectives on ethnic and racial disparities in Alzheimer’s disease and related dementias: update and areas of immediate need. Alzheimers Dement. 2019;15:292–312.
Zahodne LB, Stern Y, Manly JJ. Differing effects of education on cognitive decline in diverse elders with low versus high educational attainment. Neuropsychology. 2015;29:649–57.
Freedman M, Leach L, Carmela Tartaglia M, Stokes KA, Goldberg Y, Spring R, Nourhaghighi N, Gee T, Strother SC, Alhaj MO, Borrie M, Darvesh S, Fernandez A, Fischer CE, Fogarty J, Greenberg BD, Gyenes M, Herrmann N, Keren R, et al. The Toronto Cognitive Assessment (TorCA): normative data and validation to detect amnestic mild cognitive impairment. Alzheimers Res Ther. 2018;10:1–18.
Nasreddine ZS, Phillips NA, Bédirian V, Charbonneau S, Whitehead V, Collin I, Cummings JL, Chertkow H. The Montreal cognitive assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc. 2005;53:695–9.
Blennow K. CSF biomarkers for mild cognitive impairment. J Intern Med. 2004;256:224–34.
Blennow K, Hampel H. CSF markers for incipient Alzheimer’s disease. Lancet Neurol. 2003;2:605–13.
Schoonenboom NSM, Pijnenburg YAL, Mulder C, Rosso SM, Van Elk EJ, Van Kamp GJ, Van Swieten JC, Scheltens P. Amyloid beta(1-42) and phosphorylated tau in CSF as markers for early-onset Alzheimer disease. Neurology. 2004;62:1580–4.
Mielke MM, Syrjanen JA, Blennow K, Zetterberg H, Vemuri P, Skoog I, Machulda MM, Kremers WK, Knopman DS, Jack C, Petersen RC, Kern S. Plasma and CSF neurofilament light: relation to longitudinal neuroimaging and cognitive measures. Neurology. 2019;93:e252.
Fazekas F, Chawluk JB, Alavi A, Hurtig HI, Zimmerman RA. MR signal abnormalities at 1.5 T in Alzheimer’s dementia and normal aging. AJR Am J Roentgenol. 1987;149:351–6.
Rascovsky K, Hodges JR, Knopman D, Mendez MF, Kramer JH, Neuhaus J, Van Swieten JC, Seelaar H, Dopper EGP, Onyike CU, Hillis AE, Josephs KA, Boeve BF, Kertesz A, Seeley WW, Rankin KP, Johnson JK, Gorno-Tempini ML, Rosen H, et al. Sensitivity of revised diagnostic criteria for the behavioural variant of frontotemporal dementia. Brain. 2011;134:2456.
Gorno-Tempini ML, Hillis AE, Weintraub S, Kertesz A, Mendez M, Cappa SF, Ogar JM, Rohrer JD, Black S, Boeve BF, Manes F, Dronkers NF, Vandenberghe R, Rascovsky K, Patterson K, Miller BL, Knopman DS, Hodges JR, Mesulam MM, Grossman M. Classification of primary progressive aphasia and its variants. Neurology. 2011;76:1006–14.
Gorelick PB, Scuteri A, Black SE, Decarli C, Greenberg SM, Iadecola C, Launer LJ, Laurent S, Lopez OL, Nyenhuis D, Petersen RC, Schneider JA, Tzourio C, Arnett DK, Bennett DA, Chui HC, Higashida RT, Lindquist R, Nilsson PM, et al. Vascular contributions to cognitive impairment and dementia: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2011;42:2672–713.
McKeith IG, Dickson DW, Lowe J, Emre M, O’Brien JT, Feldman H, Cummings J, Duda JE, Lippa C, Perry EK, Aarsland D, Arai H, Ballard CG, Boeve B, Burn DJ, Costa D, Del Ser T, Dubois B, Galasko D, et al. Diagnosis and management of dementia with Lewy bodies: third report of the DLB Consortium. Neurology. 2005;65:1863–72.
Postuma RB, Berg D, Stern M, Poewe W, Olanow CW, Oertel W, Obeso J, Marek K, Litvan I, Lang AE, Halliday G, Goetz CG, Gasser T, Dubois B, Chan P, Bloem BR, Adler CH, Deuschl G. MDS clinical diagnostic criteria for Parkinson’s disease. Mov Disord. 2015;30:1591–601.
Butters MA, Young JB, Lopez O, Aizenstein HJ, Mulsant BH, Reynolds CF, DeKosky ST, Becker JT. Pathways linking late-life depression to persistent cognitive impairment and dementia. Dialogues Clin Neurosci. 2008;10:345–57.
Leonard BE. Inflammation, depression and dementia: are they connected? Neurochem Res. 2007;32:1749–56.
Köhler S, Thomas AJ, Lloyd A, Barber R, Almeida OP, O’Brien JT. White matter hyperintensities, cortisol levels, brain atrophy and continuing cognitive deficits in late-life depression. Br J Psychiatry. 2010;196:143–9.
Rapp MA, Schnaider-Beeri M, Grossman HT, Sano M, Perl DP, Purohit DP, Gorman JM, Haroutunian V. Increased hippocampal plaques and tangles in patients with Alzheimer disease with a lifetime history of major depression. Arch Gen Psychiatry. 2006;63:161–7.
Ownby RL, Crocco E, Acevedo A, John V, Loewenstein D. Depression and risk for Alzheimer disease: systematic review, meta-analysis, and metaregression analysis. Arch Gen Psychiatry. 2006;63:530.
Richard E, Reitz C, Honig LH, Schupf N, Tang MX, Manly JJ, Mayeux R, Devanand D, Luchsinger JA. Late-life depression, mild cognitive impairment, and dementia. JAMA Neurol. 2013;70:383–9.
Luppa M, Luck T, Ritschel F, Angermeyer MC, Villringer A, Riedel-Heller SG (2013) Depression and incident dementia. An 8-year population-based prospective study. PLoS One 8,.
Brommelhoff JA, Gatz M, Johansson B, McArdle JJ, Fratiglioni L, Pedersen NL. Depression as a risk factor or prodromal feature for dementia? Findings in a population-based sample of Swedish twins. Psychol Aging. 2009;24:373–84.
Li G, Wang LY, Shofer JB, Lou TM, Peskind ER, McCormick W, Bowen JD, Crane PK, Larson EB. Temporal relationship between depression and dementia: findings from a large community-based 15-year follow-up study. Arch Gen Psychiatry. 2011;68:970–7.
Becker JT, Chang YF, Lopez OL, Dew MA, Sweet RA, Barnes D, Yaffe K, Young J, Kuller L, Reynolds CF. Depressed mood is not a risk factor for incident dementia in a community-based cohort. Am J Geriatr Psychiatry. 2009;17:653–63.
Kendler KS, Zachar P, Craver C. What kinds of things are psychiatric disorders? Psychol Med. 2011;41:1143–50.
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Washington D.C.: 2013
Insel TR, Wang PS. Rethinking mental illness. JAMA. 2010;303:1970–1.
Dotson VM, Beydoun MA, Zonderman AB. Recurrent depressive symptoms and the incidence of dementia and mild cognitive impairment. Neurology. 2010;75:27–34.
Fried EI, Nesse RM. Depression is not a consistent syndrome: an investigation of unique symptom patterns in the STAR*D study. J Affect Disord. 2015;172:96.
Robert PH, Berr C, Volteau M, Bertogliati C, Benoit M, Sarazin M, Legrain S, Dubois B. Apathy in patients with mild cognitive impairment and the risk of developing dementia of Alzheimer’s disease: a one-year follow-up study. Clin Neurol Neurosurg. 2006;108:733–6.
Donovan NJ, Hsu DC, Dagley AS, Schultz AP, Amariglio RE, Mormino EC, Okereke OI, Rentz DM, Johnson KA, Sperling RA, Marshall GA. Depressive symptoms and biomarkers of Alzheimer’s disease in cognitively normal older adults. J Alzheimers Dis. 2015;46:63–73.
Geda YE, Knopman DS, Mrazek DA, Jicha GA, Smith GE, Negash S, Boeve BF, Ivnik RJ, Petersen RC, Pankratz VS, Rocca WA. Depression, apolipoprotein E genotype, and the incidence of mild cognitive impairment: a prospective cohort study. Arch Neurol. 2006;63:435–40.
Low DV, Wu MN, Spira AP. Sleep duration and cognition in a nationally representative sample of U.S. older adults. Am J Geriatr Psychiatry. 2019;27:1386–96.
Aarsland D, Brønnick K, Alves G, Tysnes OB, Pedersen KF, Ehrt U, Larsen JP. The spectrum of neuropsychiatric symptoms in patients with early untreated Parkinson’s disease. J Neurol Neurosurg Psychiatry. 2009;80:928–30.
Weintraub D, Burn DJ. Parkinson’s disease: the quintessential neuropsychiatric disorder. Mov Disord. 2011;26:1022–31.
Boot BP, Orr CF, Ahlskog JE, Ferman TJ, Roberts R, Pankratz VS, Dickson DW, Parisi J, Aakre JA, Geda YE, Knopman DS, Petersen RC, Boeve BF. Risk factors for dementia with Lewy bodies: a case-control study. Neurology. 2013;81:833–40.
Laganà V, Bruno F, Altomari N, Bruni G, Smirne N, Curcio S, Mirabelli M, Colao R, Puccio G, Frangipane F, Cupidi C, Torchia G, Muraca G, Malvaso A, Addesi D, Montesanto A, Di Lorenzo R, Bruni AC, Maletta R. Neuropsychiatric or behavioral and psychological symptoms of dementia (BPSD): focus on prevalence and natural history in Alzheimer’s disease and frontotemporal dementia. Front Neurol. 2022;13:832199.
Mojtabai R, Olfson M. Major depression in community-dwelling middle-aged and older adults: prevalence and 2- and 4-year follow-up symptoms. Psychol Med. 2004;34:623–34.
Kessler RC, Berglund P, Demler O, Jin R, Koretz D, Merikangas KR, Rush AJ, Walters EE, Wang PS. The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R). JAMA. 2003;289:3095–105.
Lieblich SM, Castle DJ, Pantelis C, Hopwood M, Young AH, Everall IP. High heterogeneity and low reliability in the diagnosis of major depression will impair the development of new drugs. BJPsych Open. 2015;1:e5–7.
Rajji TK, Bowie CR, Herrmann N, Pollock BG, Bikson M, Blumberger DM, Butters MA, Daskalakis ZJ, Fischer CE, Flint AJ, Golas AC, Graff-Guerrero A, Kumar S, Lourenco L, Mah L, Ovaysikia S, Thorpe KE, Voineskos AN, Mulsant BH. Design and rationale of the PACt-MD randomized clinical trial: prevention of Alzheimer’s dementia with cognitive remediation plus transcranial direct current stimulation in mild cognitive impairment and depression. J Alzheimers Dis. 2020;76:733–51.
Vanderbecq Q, Xu E, Ströer S, Couvy-Duchesne B, Diaz Melo M, Dormont D, Colliot O. Comparison and validation of seven white matter hyperintensities segmentation software in elderly patients. Neuroimage Clin. 2020;27:2.
Misquitta K, Dadar M, Louis Collins D, Tartaglia MC. White matter hyperintensities and neuropsychiatric symptoms in mild cognitive impairment and Alzheimer’s disease. Neuroimage Clin. 2020;28:102367.
Acknowledgements
We wish to express our profound gratitude to the patients and caregivers who generously provided their personal health data for this study.
Funding
Toronto Dementia Research Alliance Seed Funding Fund.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Tartaglia conducts clinical trials for Biogen, Avanex, UCB, Janssen, Novo Nordisk, Passage Bio and Green Valley, and holds CIHR and NIH-funded grants.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Salwierz, P., Thapa, S., Taghdiri, F. et al. Investigating the association between a history of depression and biomarkers of Alzheimer’s disease, cerebrovascular disease, and neurodegeneration in patients with dementia. GeroScience 46, 783–793 (2024). https://doi.org/10.1007/s11357-023-01030-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11357-023-01030-x