Abstract
The chronic inflammatory state at old age may contribute to the pathophysiology of or reflect chronic conditions resulting in loss of physical and mental functioning. Therefore, our objective was to examine the predictive value of a large battery of serum inflammatory markers as risk indicators for global functional decline and its specific physical and mental determinants in the oldest old. Global functional decline and specific aspects of physical and mental functional decline were assessed during an average of 1.66 years (±0.21) in a sample of 303 persons aged 80 years or older of the BELFRAIL study. Serum levels of 14 inflammatory proteins, including cytokines, growth factors, and acute phase proteins, were measured at baseline. Almost 20 % of the participants had a significant global functional decline over time. Interleukin (IL)-6 serum levels were uniquely positively associated with global functional decline, even after correcting for multiple confounders (odds ratio 1.51). Odds ratios for the individual aspects (physical dependency, physical performance, cognition, and depression) of functioning were lower, and composite scores of physical or mental decline were not significant. The proportion of global functional decline exhibited a dose–response curve with increasing levels of IL-6. Thus, IL-6 is an independent risk indicator for accelerated global functional decline in the oldest old. Our results suggest that simple serum levels of IL-6 may be very useful in short-term identification or evaluation of global functional status in the oldest old.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Low-grade chronic systemic inflammation has been associated with the process of aging and the pathogenesis or course of many age-related diseases (Alexandraki et al. 2006; Vasan et al. 2003; Joppa et al. 2006; Beenakker et al. 2010). Therefore, this chronic subclinical inflammatory state may be detrimental in older adults by contributing to the pathophysiology of or reflect chronic conditions that result in functional loss and disability or even directly impact muscle mass (e.g., cfr sarcopenia) (Roubenoff and Hughes 2000; Schaap et al. 2009). The latter may be accompanied by a reduction in muscle strength and has a profound effect on physical performance and dependency in a later stage. Chronic inflammation also plays a role in complex mental processes, such as neurogenesis, synaptic plasticity (McAfoose and Baune 2009), and clinical depression (Dowlati et al. 2010).
Due to the strong relationship between chronic inflammation and impaired functioning across numerous age-related diseases or health conditions (Brinkley et al. 2009), various inflammatory biomarkers have been proposed as potential risk indicators for functional decline over time. Interleukin (IL)-6 in particular has consistently been associated with muscle mass, muscle strength, and physical impairment and shown to predict onset of disability in older persons. Additionally, both IL-6 and C-reactive protein (CRP) were persistently associated with mortality risk in aging population studies (Singh and Newman 2011). The relationship between IL-6 or CRP and cognitive decline or occurrence of depressive symptoms has also been described in several population studies (Mooijaart et al. 2013; Bremmer et al. 2008).
Although the primary disease etiologies may differ, inflammation seems to be a common consequence or cause of both physical and mental impairment or dependency. This, together with the fact that impairment or decline in an individual aspect of functioning might also have varying degrees of effect on global functioning of older persons, and these dependencies affect each other, supports the idea of a global evaluation in clinical practice. The increasingly high burden and coexistence of mental and physical impairment is accompanying old age and consequently raises public health costs. For these reasons, focusing on the overall functional deterioration of the patient instead of individual aspects of functional status separately would be clinically more meaningful. Identifying short-term predictive biomarkers for global functional decline, allowing easy risk stratification, would be of great clinical value. Especially in the oldest age category, in which the burden is highest, this strategy would be beneficial. Additionally, an impaired functional status is known to highly predict major adverse outcomes, such as falls, dementia, and death in the oldest old.
Despite all the established associations with inflammatory markers and physical or mental functioning, there is no consensus on the relative importance of these chronic inflammatory markers as predictors of (sub)clinical decline in physical and mental performance, and information on global functional decline is limited. Only poor self-rated global health has been previously associated with elevated inflammatory markers in older persons (Christian et al. 2011; Cohen et al. 1997). Different sets of inflammatory markers have been measured in studies with diverse assays and in various settings, disabling inflammatory marker comparability between various studies.
Therefore, our study examined the predictive value of a panel of 14 potential serum inflammatory markers (cytokines, chemokines, growth hormones, and acute phase proteins) for global functional decline and the decline in specific determinants of functioning (physical dependency and performance, cognition, and suspected depression) in a sample of older persons aged 80 years or older.
Methods
Subjects
The BELFRAIL study is a prospective, observational, population-based cohort study performed in three areas of Belgium and is representative of the Belgian population older than 80 years of age. Details of the study’s methods and sampling design have been published elsewhere (Vaes et al. 2010). In summary, between November 2, 2008 and September 15, 2009, 567 subjects (age range 80 to 102 years) were included in the BELFRAIL study. Only three exclusion criteria were used: severe dementia reported by the GP, in palliative care, and medical emergency. The GP recorded background variables and medical history. The clinical research assistant performed an extensive examination, including performance testing, questionnaires, and technical examinations. In the present study, 152 of the 567 individuals were excluded because their serum inflammatory markers could not be determined due to a technical issue. This selection resulted in a population sample of 415 participants who were comparable to the initial sample (Vaes et al. 2010) on all demographic variables listed in Table 1. All study participants gave informed consent, and the Biomedical Ethics Committee of the Medical School of the Université catholique de Louvain (UCL) of Brussels approved the study.
Follow-up
The “clinical research associate” (CRA) repeated the detailed physical and mental examinations on 327 individuals after a mean period of 1.66 years (±0.21) from baseline. From the baseline study population of 415 individuals, 45 individuals had died, 43 individuals refused a second CRA visit, and 24 individuals did not complete all four examinations (Fig. 1). These factors resulted in a final sample of 303 individuals, comparable to the initial sample on all demographic variables described in Table 1, in which the global functional decline score could be determined.
Functional measures
Physical decline
The activities of daily living (ADL) and short physical performance battery (SPPB) were used as proxies for the patient’s physical dependency and performance, respectively. Details of the study’s physical parameters were published previously (Adriaensen et al. 2014). A significant decline in the physical summary performance scale, ranging from 0 to 14, was calculated with the formula (T0 − T1)*100/T0. To account for temporal variability in the SPPB score, only those with more than 20 % change in their scores were defined as having a significant SPPB decline. The Edwards–Nunnally index was calculated on the ADL scores to determine a significant increase in physical dependency over time. This index determines the probability of substantial individual change and avoids the problem of regression to the mean. Based on the scale reliability and the 95 % confidence interval (CI) of the mean score at T0, the index computes whether a significant change has occurred between T0 and T1 (Speer and Greenbaum 1995). The sum of the binary scores created an overall score of physical functional decline.
Mental decline
The Mini-Mental State Examination (MMSE) and Geriatric Depression Scale (GDS)-15 scores were used to assess the subject’s cognitive and depression status, respectively. Details of the study’s mental parameters have been published previously (Adriaensen et al. 2014). As described above, the Edwards–Nunnally index was used to calculate a significant change in cognitive function based on the MMSE score. Subjects who shifted from GDS-15 < 5 at baseline to GDS-15 > 5 at T1 were defined as having a significant worsening in depression status. The sum of the binary scores created an overall score of mental functional decline.
Global functional decline
Based on our previous definition of global functional impairment (Adriaensen et al. 2014), the sum of the binary scores of the four aspects of physical and mental decline created an overall score of global functional decline. Participants were identified as having stable functioning (0), limited decline (1), or global functional decline (2–4) (Fig. 1).
Serum inflammatory markers
Fasting blood samples were collected in the morning and stored within 4 h at −80 °C. The analytical process was organized to avoid several freeze–thaw cycles. An extensive panel of inflammatory cytokines, chemokines, and growth factors (IL-1α, IL-1β, IL-2, IL-4, IL-6, IL-8, IL-10, TNF-α, IFN-γ, MCP-1, VEGF, and EGF) was measured using biochip arrays with the Evidence Investigator Analyzer (Randox Laboratories Limited, Crumlin, UK), which enables the simultaneous analysis of 12 factors using a limited volume of serum (100 μl) without cross-reactivity. The UniCel® DxC 800 Synchron (Beckman Coulter, Brea, USA) was used to measure ultrasensitive CRP and prealbumin levels. Details on the analytical methods were previously published (Vaes et al. 2010).
Covariates
The Charlson Comorbidity Index (CCI) includes 19 chronic diseases that are weighted based on their association with mortality (Charlson et al. 1987). In the present study, the CCI was slightly modified because connective tissue disease could not be reliably reported by the GP, and various stages of liver disease, cancer, and diabetes could not always be differentiated. Consequently, the CCI assigned a minimum of 4 points for the high age and added the following weights: 1 point for myocardial infarction, congestive heart failure, peripheral vascular disease, cerebrovascular disease, chronic pulmonary disease (COPD or asthma), all liver diseases, and all cases of diabetes; 2 points for hemiplegia, renal disease, and all cancers with no metastases mentioned in the medical history; and 6 points for HIV. Smoking was dichotomized as having ever or never smoked, and alcohol usage was expressed as units per day. Low level of education was defined as having no diploma and a diploma from primary school or lower secondary school. Body mass index (BMI) was calculated as body mass in kilograms divided by height in meters squared. The CMV IgG concentrations were measured on the ARCHITECT® i4000SR (Abbott Diagnostics, Abbott Park, IL, USA).
Statistical analysis
Continuous data were presented as the mean and standard deviation (SD) or as the median and interquartile range (IQR). Categorical data were presented as numbers and frequencies. Comparisons between two categories of subjects were performed using Student’s t test or Wilcoxon rank sum test for continuous data and the χ 2 tests or Fisher’s exact test for categorical data. Comparisons between three categories of subjects were performed using the Kruskal–Wallis test. A p value <0.05 was considered to be statistically significant.
Multivariable logistic regression models were used to estimate the adjusted odds ratios (OR) and 95 % confidence intervals for the association between (individual aspects of) physical or mental functional decline and serum values of IL-6. The latter were log-transformed or divided into quintiles to account for the non-normal distribution and entered into all models. The relationship between global functional decline (dependent variable) and serum levels of IL-6 (independent variable) was assessed with multivariable ordered logistic regression models, due to the ordinal scale of the global functional decline variable. No violation of the proportional odds assumption was observed with the “likelihood ratio test” or “Brant test.” Three consecutive models including an increasing number of covariates were used: unadjusted (model 1); adjusting for age, gender, and Charlson Comorbidity Index (model 2); and adding institutionalization, BMI, and use of anti-inflammatory medication (model 3). Potential confounders were based on the bivariate analysis and our previous work (Adriaensen et al. 2014). Predicted probabilities for the ordinal global functional decline variable were calculated after fitting the third model with quintiles of the serum IL-6 levels. No colinearity or interaction was found with regard to the variables. For all of the analyses, robust estimates were used to account for influential outliers or non-constant variance (Lumley et al. 2002).
The statistical analyses were performed using Stata 11 (StataCorp, College Station, TX) and GraphPad Prism 6 (GraphPad Software, San Diego, CA).
Results
Prevalence of global functional decline with potential inflammatory biomarkers and confounders
Global functional decline was assessed in 303 individuals (Fig. 1); mean age was 84.3 years, and 37 % of the individuals were male (Table 1). Almost all had comorbidities at baseline, and 10 % were institutionalized. Moreover, 46, 34.7, and 19.1 % of the study population had a stable, limited, and global functional decline during the mean follow-up period of 1.66 years (±0.21), respectively. Patients with a global functional decline were characterized by a significantly higher age and CCI. Patients with a stable global function over time were less institutionalized at baseline. Additionally, serum IL-6 levels were significantly higher with increasing severity of global functional decline (p < 0.001). No bivariate associations could be found with the 13 additionally measured inflammatory markers, including usCRP.
Serum IL-6 and global functional decline
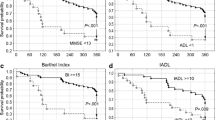
The association between serum levels of IL-6 and global functional decline was further investigated by calculating the unadjusted and adjusted odds ratios. In all three models, the association with log IL-6 and global functional decline remained significant with the odds ratios of 1.63, 1.55, and 1.51, respectively (p ≤ 0.001, Table 2). To better interpret the odds ratios of the log-transformed independent variable, the model was performed with quintiles of serum IL-6, and predicted probabilities for the various outcomes were calculated relative to the quintiles of serum IL-6 (Fig. 2a). The predicted probabilities for a stable global function over time increased from the highest to the lowest quintile of IL-6. The predicted probabilities for a limited and global functional decline increased from the lowest to the highest quintile of IL-6. This result was also reflected in the proportion of individuals with a stable, limited, or global functional decline (Kruskal–Wallis test, p < 0.001) (Fig. 2b). In contrast, the odds ratios of log IL-6 for the composite scores of physical or mental decline were not significant (Tables 3 and 4).
Predicted probabilities after ordered logistic regression analysis (a) and proportions of individuals (b) with a stable, limited, and global functional decline, with regard to increasing IL-6 quintiles. Differences in proportions were significant (Kruskal–Wallis test, p < 0.001). Pre Prob predicted probability, CI confidence interval
Relationship between serum IL-6 levels and specific aspects of global functional decline
The relationship with global functional decline was further explored by investigating the association between IL-6 and decline in the individual aspects of functioning. Of the 415 eligible participants, 22.9, 36.4, 18.7, and 5.7 % had a decline in ADL, SPPB, MMSE, and GDS over time, respectively (Fig. 1). Profound overlap of the individual declines was found in our older individuals (Table 5). The bivariate analysis showed significantly higher levels of IL-6 in those individuals with a decline in ADL, SPPB, and MMSE (Table S1). All these declines were associated with older age. Additionally, the CCI was significantly higher in individuals with a physical decline in ADL or SPPB score. The few individuals taking anti-inflammatory medication at baseline were uniquely in the group without MMSE or GDS decline. No associations were observed for individuals with a GDS decline. Additionally, no associations could be found between the 13 additional inflammatory markers and the physical or mental aspects of functioning. After consecutive correction of the association with the potential confounders, the associations with log IL-6 and ADL, SPPB, and MMSE remained significant with odds ratios of 1.39, 1.45, and 1.37, respectively (Table 6). The association with GDS decline remained non-significant.
Discussion
Main findings of the study
We described the unique prognostic value of serum IL-6 levels, among an extensive set of 14 inflammatory markers, for predicting global functional decline in the oldest old. Previously, we already defined global functioning and showed higher levels of IL-6 to be highly associated with impaired global functioning at baseline with odds ratios of 4 or more and suggested its use as a not-at-risk marker due to the very high negative predictive value. Therefore, in a similar way, we defined global functional decline during approximately 1.5 years, and approximately 20 % of our study population displayed a decline in global functioning. Despite the evidence that an individual’s global functioning declines with increasing age, identifying those individuals with an accelerated decline is clinically relevant. We showed that IL-6 was a common factor in all aspects of global functional decline, except worsening depression status (Table 6). This fact together with the coexistence of the individual aspects at old age (Table 5) makes a summary evaluation with the risk indicator IL-6 for the global functional decline of an older person clinically relevant. We showed that the probability of global functional decline gradually increased with higher levels of IL-6 and that the odds ratios were higher for the overall decline of functioning compared with the individual aspects, except depression, or composite scores of physical or mental functioning. Moreover, the associations were attenuated but remained highly significant after adjusting for multiple potential confounders, which rendered IL-6 as an independent risk indicator for accelerated global functional decline. The odds ratios for global functional decline were 1.51 times higher for each one-unit increase in log IL-6 (corresponding to a 1.72 times increase in untransformed IL-6 levels).
Serum IL-6 levels and physical decline
Initially, 15 years ago, IL-6 and CRP were shown to be strong predictors of incident physical disability in older individuals of the Established Populations for the Epidemiologic Study of the Elderly (EPESE) (Ferrucci et al. 1999). Until today, only a limited number of prospective population studies further reported on the positive association between IL-6 and physical decline in older individuals. However, these previous studies were all restricted to lower age categories (Ferrucci et al. 2002; Schaap et al. 2009; Penninx et al. 2004; Stenholm et al. 2010; Taaffe et al. 2000), high-functioning persons (Schaap et al. 2009; Penninx et al. 2004; Taaffe et al. 2000; Ferrucci et al. 1999), or longer follow-up periods (Schaap et al. 2009; Stenholm et al. 2010; Taaffe et al. 2000; Ferrucci et al. 1999) or were gender-specific (Ferrucci et al. 2002). Therefore, the generalizability of these findings in the oldest old might be limited. Only the Einstein Aging study was comparable because they included non-disabled subjects and both sexes; covered a wide age range; and used quantitative measures (Verghese et al. 2011). Despite all the above affirmative studies, Taaffe and coworkers could not find an association between IL-6 levels and change in performance (Taaffe et al. 2000). However, these results were restricted to high-functioning persons aged between 70 and 79 years, and only 67 % were retested after 7 years, during which many disabled persons could have died.
Consistent with our results, these previous studies reveal that increased IL-6 levels are independent of age, gender, race, body composition, and comorbidities associated with poorer physical function. Furthermore, Brinkley and coworkers showed, with standardized measures across multiple study populations, that these associations were consistent in individuals with chronic obstructive pulmonary disease (COPD), congestive heart failure (CHF), high cardiovascular risk, and self-reported disability (Brinkley et al. 2009).
Serum IL-6 levels and mental decline
IL-6 has been robustly associated with cognitive function and dementia in several population-based studies (Wright et al. 2006). However, data of the impact of IL-6 on cognitive decline over time are conflicting, and only a few of these prospective studies were population-based and included the oldest old. Two large population-based studies in older adults observed that participants with high IL-6 levels had higher rates of cognitive decline after 2.5, 3, and 7 years of follow-up, independent of race, other vascular risk factors, and C-reactive protein levels (Economos et al. 2013; Weaver et al. 2002). However, no association for IL-6 levels and cognitive decline was reported in two other studies of middle-aged or older adults (Dik et al. 2005; Gimeno et al. 2008). However, these inconsistent associations could be because of age differences. For instance, higher IL-6 levels were related to a steeper annual decline in memory function in persons aged 85 or older but was not noticeable in individuals aged younger than 85 years (Schram et al. 2007). These results suggest that systemic IL-6 would only be suitable for cognitive risk stratification in the oldest old. Furthermore, the PROSPER study and a stratified analysis of the NOMAS study reported high IL-6 levels to be associated with an increased rate of detailed assessments of cognitive decline in individuals aged older than 75 or 71 years, respectively (Mooijaart et al. 2013; Economos et al. 2013).
The relationship between inflammation and depression in old age is poorly understood but generally accepted, particularly because depression and dementia are strongly interrelated. In individuals aged 65 or older, a high plasma level of IL-6 was associated with an increased prevalence of major depression (Bremmer et al. 2008). Based on the average 12 years of follow-up in over 3000 middle-aged adults, Gimeno and coworkers reported that IL-6 could predict cognitive symptoms of depression but not the other way around (Gimeno et al. 2009). These results suggest that inflammation precedes depression, at least with regard to the cognitive symptoms of depression. However, we could not establish such a cross-sectional (Adriaensen et al. 2014) or longitudinal association with the occurrence of GDS-15 screen-positives in our oldest old. A possible explanation for our result could be our low number of newly detected depression cases and short follow-up period to detect new cases. Nevertheless, inconsistent results have been described in previous cross-sectional studies in older adults, in which no such relationship could be found between IL-6 and depressive symptoms (Baune et al. 2008; Dimopoulos et al. 2008; van den Biggelaar et al. 2007). However, despite its non-significant association, depression remains an important aspect of global functioning, as depressive symptoms constitute an important negative impact on daily functioning. Regardless, diagnosing (sub)clinical depression remains very difficult, and more detailed approaches are needed to investigate its role in global functioning.
The theory that vascular or neurodegenerative processes underlie these mental associations is still unclear. Vascular mechanisms have been proposed and strongly associated with IL-6 and cognitive decline. However, Wright and coworkers suggested a direct effect on the brain because adjusting for vascular disease and subclinical atherosclerosis did not attenuate the association with cognitive decline and IL-6 (Wright et al. 2006). Additionally, previous data suggest that IL-6 crosses the blood–brain barrier (BBB), and peripheral levels may represent the levels in the brain and can therefore reflect neural and systemic inflammation (Banks et al. 1995).
Is IL-6 a potent predictor for global functional impairment in the oldest old?
IL-6 has been proposed as the main circulating candidate in linking systemic inflammation with local pathology (Yudkin et al. 2000). Moreover, IL-6 is associated not only with many adverse outcomes and diseases but also with the number and severity of many medical conditions (Badolato and Oppenheim 1995). Furthermore, IL-6 was positively associated with the severity of comorbidity in our cohort or the CCI (Kruskal–Wallis, p = 0.005). Similarly, Penninx et al. showed that the relationship with IL-6 and physical decline was stronger for those with many difficulties or inabilities than for those with only limited dysfunction (Penninx et al. 2004). They also showed that CVD or the occurrence of general serious health events in those with high levels were not likely to simply explain their findings. Therefore, IL-6 is not likely to be an exclusive indicator of disease activity, and the causal pathway from IL-6 to physical disability in old age is most likely multifactorial. Nevertheless, IL-6 could simply be an indicator of biological frailty or immunosenescence in general, in which IL-6 is likely to represent a general down-spiral pathway involving multiple pathophysiological mechanisms and therefore reflects the associated patient’s global function (Penninx et al. 2004). Only two previous studies have reported that poorer self-rated global health is associated with elevated IL-6 levels in older adults (Christian et al. 2011; Cohen et al. 1997). We showed a clear dose–response relationship of global functional decline with increasing serum levels of baseline IL-6. A common pathway for physical and mental decline could explain why the association with IL-6 and the overall functional state of a person is so robust, compared with the associations with the individual aspects of functioning. To confirm this hypothesis, future research should investigate whether elevated levels of IL-6 reflect functional damage or whether it has a direct causal detrimental effect on certain aspects of overall functioning. However, both theories are possible, in which high levels of IL-6 released by damaged cells can have detrimental effects, causing an infinite loop leading to further global functional decline.
We provided evidence that IL-6 could be used not only in long-term but also in short-term prediction (approximately 1.5 years) of physical, cognitive, or global functional decline. This prognostic value could be confined to the oldest old because IL-6 may rise more into the measurable range, considering the older age of our participants, and larger magnitudes of differences could become apparent. Notwithstanding, diagnostic performance should be tested in multiple settings before we can propose IL-6 as a valuable candidate biomarker for functional deterioration in the oldest old. Studies are needed to define clinical useful cutoffs, and standardization of IL-6 measurements is vital. However, independent of the cohort and the equipment used, the proposed cutoffs are quite similar. The WHAS study proposed a cutoff of 3.1 pg/ml (Ferrucci et al. 2002), Harris and coworkers of 3.2 pg/ml (Harris et al. 1999), and Ferrucci and coworkers of 2.5 pg/ml (Ferrucci et al. 1999). Following a similar cutoff score of 2.98 pg/ml, inflammageing was apparent with 31.6 % of our participants having IL-6 values above the cutoff value. By comparing those with a stable or global functional decline, the proposed cutoff had a sensitivity and specificity of 40 and 80 %, respectively. This result supports our previous work, in which we suggested that IL-6 could be used as a not-at-risk indicator in the oldest old (Adriaensen et al. 2014). Future studies should further evaluate or improve its predictive value across multiple populations, and the causal pathway should be further explored in clinical trials to develop prevention strategies.
Value of CRP and other inflammatory markers
Remarkably, no association could be found with the other 13 tested inflammatory biomarkers in our oldest old. In a recent review, Singh and coworkers reported serum CRP and TNF-α to be the second and third most associated parameters, besides IL-6, with incident disease, disability, and mortality in most large, current epidemiologic studies of older adults. Despite previous associations with physical decline and dementia (Singh and Newman 2011), CRP loses its chronic inflammatory hallmark feature in the oldest old, as it had no additional value in our predictive models. Likewise, CRP was often found to exhibit a lesser or non-significant association with physical decline (Stenholm et al. 2010). The same holds for cognitive decline (Mooijaart et al. 2013; Economos et al. 2013; Schram et al. 2007) and occurrence of depression symptoms (Bremmer et al. 2008). Despite their biological connection, various pathways are proposed, as only a small correlation could be found between both measures (Pearson r = 0.15, p = 0.003). Previously, TNF-α was shown to have a strong association with loss of upper muscle strength in the Health ABC Study (Schaap et al. 2009). However, only those individuals aged 70–79 years who had completed the 7-year follow-up were included. These results could not be confirmed in more representative studies of the elderly (Verghese et al. 2011; Brinkley et al. 2009), including our findings (Legrand et al. 2013). Despite the biological interactions, TNF-α was shown to be less stable than IL-6, and only weak correlations could be found between these markers (Verghese et al. 2011) (Pearson r = 0.12, p = 0.012).
Strengths and limitations
Our study contains a large sample of Belgian persons aged 80 years and older. The association with IL-6 and global functional decline, corrected for a large number of confounders, may therefore be more evident compared with more selected (e.g., high-functioning) populations, but also with younger populations, where the level of IL-6 and presence of physical and mental disability are generally lower. An extensive set of potential inflammatory markers was used to compare their value in this age category because comparability between studies remains difficult due to a lack of standardization of physical and mental measures of decline and cytokine measurements. Caution is advised, as we used a non-validated instrument for global functional decline that should not be confused with an overall frailty measure because the latter does not objectify disability. Our findings could be strengthened if the IL-6 increase was measured over time. Despite this factor, studies have shown that intra-individual concentrations do not vary greatly over time. Due to our short follow-up period, baseline IL-6 would remain an indicator of chronic inflammatory states that both precede and follow the actual measurement (Rao et al. 1994; Picotte et al. 2009). Additionally, no soluble markers (e.g., sIL-6R) that could represent more prolonged and severe states of inflammation were included and were suggested to be more stable.
Conclusion
We combined physical and mental decline as a global endpoint in our study to provide new insights into the role of IL-6 in global functioning of the oldest old, due to the common association with IL-6 among the physical and mental aspects and the coexistence of these aspects at old age. Our previous cross-sectional and current prospective work indicated that of an extensive immune battery, only IL-6 serum levels were highly related to global functional status and decline in a large sample of the Belgian oldest old. High IL-6 levels also preceded the development of the individual physical and mental aspects of global functional decline with lower odds ratios, except for depressive symptoms. Our previous and current results suggest that serum levels of IL-6 might be useful in identifying or evaluating the severity of global functioning of a patient aged 80 or over.
References
Adriaensen W, Mathei C, van Pottelbergh G, Vaes B, Legrand D, Wallemacq P, Degryse JM (2014) Significance of serum immune markers in identification of global functional impairment in the oldest old: cross-sectional results from the BELFRAIL study. Age (Dordr) 36(1):457–467. doi:10.1007/s11357-013-9558-3
Alexandraki K, Piperi C, Kalofoutis C, Singh J, Alaveras A, Kalofoutis A (2006) Inflammatory process in type 2 diabetes: the role of cytokines. Ann N Y Acad Sci 1084:89–117. doi:10.1196/annals.1372.039
Badolato R, Oppenheim J (1995) Role of cytokines, acute-phase proteins, and chemokines in the progression of rheumatoid arthritis. Semin Arthritis Rheum 26(2):526–538
Banks W, Kastin A, Broadwell R (1995) Passage of cytokines across the blood-brain barrier. Neuroimmunomodulation 2(4):241–248
Baune BT, Ponath G, Golledge J, Varga G, Arolt V, Rothermundt M, Berger K (2008) Association between IL-8 cytokine and cognitive performance in an elderly general population—the MEMO-Study. Neurobiol Aging 29(6):937–944. doi:10.1016/j.neurobiolaging.2006.12.003
Beenakker K, Ling C, Meskers C, de Craen A, Stijnen T, Westendorp R, Maier A (2010) Patterns of muscle strength loss with age in the general population and patients with a chronic inflammatory state. Ageing Res Rev 9(4):431–436. doi:10.1016/j.arr.2010.05.005
Bremmer MA, Beekman AT, Deeg DJ, Penninx BW, Dik MG, Hack CE, Hoogendijk WJ (2008) Inflammatory markers in late-life depression: results from a population-based study. J Affect Disord 106(3):249–255. doi:10.1016/j.jad.2007.07.002
Brinkley TE, Leng X, Miller ME, Kitzman DW, Pahor M, Berry MJ, Marsh AP, Kritchevsky SB, Nicklas BJ (2009) Chronic inflammation is associated with low physical function in older adults across multiple comorbidities. J Gerontol A Biol Sci Med Sci 64(4):455–461. doi:10.1093/gerona/gln038
Charlson M, Pompei P, Ales K, MacKenzie C (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40(5):373–383
Christian LM, Glaser R, Porter K, Malarkey WB, Beversdorf D, Kiecolt-Glaser JK (2011) Poorer self-rated health is associated with elevated inflammatory markers among older adults. Psychoneuroendocrinology 36(10):1495–1504. doi:10.1016/j.psyneuen.2011.04.003
Cohen H, Pieper C, Harris T, Rao K, Currie M (1997) The association of plasma IL-6 levels with functional disability in community-dwelling elderly. J Gerontol A: Biol Med Sci 52(4):M201–M208
Dik MG, Jonker C, Hack CE, Smit JH, Comijs HC, Eikelenboom P (2005) Serum inflammatory proteins and cognitive decline in older persons. Neurology 64(8):1371–1377. doi:10.1212/01.WNL.0000158281.08946.68
Dimopoulos N, Piperi C, Psarra V, Lea RW, Kalofoutis A (2008) Increased plasma levels of 8-iso-PGF2alpha and IL-6 in an elderly population with depression. Psychiatry Res 161(1):59–66. doi:10.1016/j.psychres.2007.07.019
Dowlati Y, Herrmann N, Swardfager W, Liu H, Sham L, Reim EK, Lanctot KL (2010) A meta-analysis of cytokines in major depression. Biol Psychiatry 67(5):446–457. doi:10.1016/j.biopsych.2009.09.033
Economos A, Wright CB, Moon YP, Rundek T, Rabbani L, Paik MC, Sacco RL, Elkind MS (2013) Interleukin 6 plasma concentration associates with cognitive decline: the northern Manhattan study. Neuroepidemiology 40(4):253–259. doi:10.1159/000343276
Ferrucci L, Harris T, Guralnik J, Tracy R, Corti M, Cohen H, Penninx B, Pahor M, Wallace R, Havlik R (1999) Serum IL-6 level and the development of disability in older persons. J Am Geriatr Soc 47(6):639–646
Ferrucci L, Penninx B, Volpato S, Harris T, Bandeen-Roche K, Balfour J, Leveille S, Fried L, Md J (2002) Change in muscle strength explains accelerated decline of physical function in older women with high interleukin-6 serum levels. J Am Geriatr Soc 50(12):1947–1954
Gimeno D, Marmot MG, Singh-Manoux A (2008) Inflammatory markers and cognitive function in middle-aged adults: the Whitehall II study. Psychoneuroendocrinology 33(10):1322–1334. doi:10.1016/j.psyneuen.2008.07.006
Gimeno D, Kivimaki M, Brunner EJ, Elovainio M, De Vogli R, Steptoe A, Kumari M, Lowe GD, Rumley A, Marmot MG, Ferrie JE (2009) Associations of C-reactive protein and interleukin-6 with cognitive symptoms of depression: 12-year follow-up of the Whitehall II study. Psychol Med 39(3):413–423. doi:10.1017/S0033291708003723
Harris T, Ferrucci L, Tracy R, Corti M, Wacholder S, Ettinger WJ, Heimovitz H, Cohen H, Wallace R (1999) Associations of elevated interleukin-6 and C-reactive protein levels with mortality in the elderly. Am J Med 106(5):506–512
Joppa P, Petrasova D, Stancak B, Tkacova R (2006) Systemic inflammation in patients with COPD and pulmonary hypertension. Chest 130(2):326–333. doi:10.1378/chest.130.2.326
Legrand D, Adriaensen W, Vaes B, Mathei C, Wallemacq P, Degryse J (2013) The relationship between grip strength and muscle mass (MM), inflammatory biomarkers and physical performance in community-dwelling very old persons. Arch Gerontol Geriatr 57(3):345–351. doi:10.1016/j.archger.2013.06.003
Lumley T, Diehr P, Emerson S, Chen L (2002) The importance of the normality assumption in large public health data sets. Annu Rev Public Health 23:151–169. doi:10.1146/annurev.publheath.23.100901.140546
McAfoose J, Baune B (2009) Evidence for a cytokine model of cognitive function. Neurosci Biobehav Rev 33(3):355–366
Mooijaart SP, Sattar N, Trompet S, Lucke J, Stott DJ, Ford I, Jukema JW, Westendorp RG, de Craen AJ (2013) Circulating interleukin-6 concentration and cognitive decline in old age: the PROSPER study. J Intern Med 274(1):77–85. doi:10.1111/joim.12052
Penninx B, Kritchevsky S, Newman A, Nicklas B, Simonsick E, Rubin S, Nevitt M, Visser M, Harris T, Pahor M (2004) Inflammatory markers and incident mobility limitation in the elderly. J Am Geriatr Soc 52(7):1105–1113
Picotte M, Campbell CG, Thorland WG (2009) Day-to-day variation in plasma interleukin-6 concentrations in older adults. Cytokine 47(3):162–165. doi:10.1016/j.cyto.2009.05.007
Rao K, Pieper C, Currie M, Cohen H (1994) Variability of plasma IL-6 and crosslinked fibrin dimers over time in community dwelling elderly subjects. Am J Clin Pathol 102(6):802–805
Roubenoff R, Hughes V (2000) Sarcopenia: current concepts. J Gerontol A: Biol Med Sci 55(12):M716–M724
Schaap LA, Pluijm SM, Deeg DJ, Harris TB, Kritchevsky SB, Newman AB, Colbert LH, Pahor M, Rubin SM, Tylavsky FA, Visser M (2009) Higher inflammatory marker levels in older persons: associations with 5-year change in muscle mass and muscle strength. J Gerontol A Biol Sci Med Sci 64(11):1183–1189. doi:10.1093/gerona/glp097
Schram MT, Euser SM, de Craen AJ, Witteman JC, Frolich M, Hofman A, Jolles J, Breteler MM, Westendorp RG (2007) Systemic markers of inflammation and cognitive decline in old age. J Am Geriatr Soc 55(5):708–716. doi:10.1111/j.1532-5415.2007.01159.x
Singh T, Newman AB (2011) Inflammatory markers in population studies of aging. Ageing Res Rev 10(3):319–329. doi:10.1016/j.arr.2010.11.002
Speer D, Greenbaum P (1995) Five methods for computing significant individual client change and improvement rates: support for an individual growth curve approach. J Consult Clin Psychol 63(6):1044–1048
Stenholm S, Maggio M, Lauretani F, Bandinelli S, Ceda G, Di Iorio A, Giallauria F, Guralnik J, Ferrucci L (2010) Anabolic and catabolic biomarkers as predictors of muscle strength decline: the InCHIANTI study. Rejuvenation Res 13(1):3–11. doi:10.1089/rej.2009.0891
Taaffe D, Harris T, Ferrucci L, Rowe J, Seeman T (2000) Cross-sectional and prospective relationships of interleukin-6 and C-reactive protein with physical performance in elderly persons: MacArthur Studies of Successful Aging. J Gerontol A: Biol Med Sci 55A(12):M709–M715
Vaes B, Pasquet A, Wallemacq P, Rezzoug N, Mekouar H, Olivier PA, Legrand D, Mathei C, Van Pottelbergh G, Degryse J (2010) The BELFRAIL (BFC80+) study: a population-based prospective cohort study of the very elderly in Belgium. BMC Geriatr 10:39. doi:10.1186/1471-2318-10-39
van den Biggelaar AH, Gussekloo J, de Craen AJ, Frolich M, Stek ML, van der Mast RC, Westendorp RG (2007) Inflammation and interleukin-1 signaling network contribute to depressive symptoms but not cognitive decline in old age. Exp Gerontol 42(7):693–701. doi:10.1016/j.exger.2007.01.011
Vasan R, Sullivan L, D’Agostino R, Roubenoff R, Harris T, Sawyer D, Levy D, Wilson P (2003) Serum insulin-like growth factor I and risk for heart failure in elderly individuals without a previous myocardial infarction: the Framingham Heart Study. Ann Intern Med 139(8):642–648
Verghese J, Holtzer R, Oh-Park M, Derby CA, Lipton RB, Wang C (2011) Inflammatory markers and gait speed decline in older adults. J Gerontol A Biol Sci Med Sci 66(10):1083–1089. doi:10.1093/gerona/glr099
Weaver JD, Huang MH, Albert M, Harris T, Rowe JW, Seeman TE (2002) Interleukin-6 and risk of cognitive decline: MacArthur Studies of Successful Aging. Neurology 59(3):371–378. doi:10.1212/wnl.59.3.371
Wright C, Sacco R, Rundek T, Delman J, Rabbani L, Elkind M (2006) Interleukin-6 is associated with cognitive function: the Northern Manhattan Study. J Stroke Cerebrovasc Dis 15(1):34–38
Yudkin J, Kumari M, Humphries S, Mohamed-Ali V (2000) Inflammation, obesity, stress and coronary heart disease: is interleukin-6 the link? Atherosclerosis 148(2):209–214
Acknowledgments
We would like to thank all participating general practitioners and their patients. The BELFRAIL study (B40320084685) was supported by an unconditional grant from Fondation Louvain, Brussels, Belgium. Fondation Louvain is the support unit of Université catholique de Louvain and is charged with developing the educational and research projects of the university by collecting gifts from corporations, foundations, and alumni.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Table S1
(DOC 78 kb)
About this article
Cite this article
Adriaensen, W., Matheï, C., Vaes, B. et al. Interleukin-6 predicts short-term global functional decline in the oldest old: results from the BELFRAIL study. AGE 36, 9723 (2014). https://doi.org/10.1007/s11357-014-9723-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11357-014-9723-3