Abstract
Cutaneous sensation deteriorates with age. It is not known if this change is consistent over the entire hand or if sensation is affected by changes in skin mechanics. Cutaneous perceptual thresholds were tested at eight sites in the glabrous skin and two in the hairy skin of both hands in 70 subjects (20–88 years), five male and five female per decade, using calibrated von Frey filaments, two-point discrimination, and texture discrimination. Venous occlusion at the wrist (40 ± 10 mmHg) and moisturizer were used to alter skin mechanics. Cutaneous thresholds increased significantly with age (p < 0.001); von Frey thresholds were 0.04 g [0.02–0.07] (median and interquartile range) in the 20s and 0.16 g [0.04–0.4] in the 80s, with differences between hands for older females (p = 0.044) but not males. The pattern of changes in cutaneous sensation varied according to the site tested with smaller changes on the fingers compared to the palm. Two-point discrimination deteriorated with age (p = 0.046), but with no interaction between sex, handedness, or changes in skin mechanics. There were no significant differences for texture discrimination. Changes in skin mechanics improved cutaneous thresholds in the oldest males after moisturizing (p = 0.001) but not otherwise. These results emphasize the complex pattern of age-related deterioration in cutaneous sensation with differences between sexes, the hands, sites on the hand, and the mode of testing. As the index fingertip is not a sensitive indicator of sensory decline, the minimum assessment of age-related changes in cutaneous sensation should include both hands, and sites on the palm.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cutaneous sensation is an important source of information about the external environment. The skin of the hands is highly specialized to detect the spatial and temporal cues that subserve texture and form, particularly the glabrous or hairless skin on the palmar surface. However, cutaneous sensitivity declines with age, a change associated with reduced hand function and an increased risk of injury (Bell-Krotoski 1995). The feedback from sensory receptors in both the glabrous and hairy skin have been shown to play a role in the modulation of fine movement (Caccia et al. 1973; Johansson and Westling 1984; Deuschl et al. 1995; Macefield and Johansson 1996; McNulty et al. 1999), and sensory impairments may exacerbate the decline in fine motor skills with ageing (Potvin et al. 1980; Jette et al. 1990). However, as age-related changes in cutaneous sensation are primarily investigated on the glabrous skin of the fingertips, it is not clear if sensory changes are consistent across different skin types or innervation territories.
The gold standard for testing cutaneous sensation is calibrated von Frey filaments (Bell-Krotoski 1995; Dannenbaum et al. 2002) with which the smallest consciously perceived mechanical skin deformation can be quantified. Age-related changes in sensation are usually investigated at a single site, typically the index fingertip (e.g., Thornbury and Mistretta 1981; Desrosiers et al. 1996; Tremblay et al. 2005; Murata et al. 2010), although the tip of the little finger (Bruce 1980), two to three fingertips (Cole et al. 1998; Bear-Lehman et al. 2003), or all five fingertips (Kalisch et al. 2008; Aoki and Fukuoka 2010), have been compared. Changes in cutaneous sensation are more frequently reported using two-point discrimination, again most often at the fingertips (e.g., Bovenzi and Zadini 1989; Woodward 1993; Desrosiers et al. 1996; Stevens and Choo 1996; Kalisch et al. 2008; van Nes et al. 2008) although the palm and dorsal surface have been studied (Axelrod and Cohen 1961; Gellis and Pool 1977; Stevens and Choo 1996). Despite the natural variability of cutaneous thresholds across the hand (Weber 1834; Stevens and Choo 1996), only a single study has compared two-point discrimination on the dominant hand at multiple sites that include both palmar and dorsal aspects (Gellis and Pool 1977). Similarly, age-related threshold changes for both two-point discrimination and von Frey filaments have only been compared at the fingertips of one hand (Desrosiers et al. 1996; Tremblay et al. 2005; Kalisch et al. 2008), and at two sites on the palm (Axelrod and Cohen 1961). Despite methodological differences, these studies suggest that thresholds for von Frey and two-point discrimination may increase in the fingertips by as much as 10-fold between 20 and 90 years. Age-related changes differ between the sexes with von Frey filament testing (Desrosiers et al. 1996; Bear-Lehman et al. 2003), although the results are not always consistent for either von Frey or two-point discrimination (Thornbury and Mistretta 1981; Woodward 1993; van Nes et al. 2008).
The physiological mechanisms contributing to changes in cutaneous sensation are not well understood. In the upper limb, morphological changes and decreased numbers of both myelinated afferent fibers and cutaneous receptor end-organs are thought to explain the progressive decline in sensation (Cottrell 1940; Swensson 1939 in Rexed 1944; Cauna 1965; O'Sullivan and Swallow 1968). Changes in the mechanics of the skin itself, including dehydration (Verrillo et al. 1998), may contribute to reduced sensation with age (Woodward 1993; Vega-Bermudez and Johnson 2004). Dehydration is clinically assessed as turgor or the ability of the skin to return after deformation (Dorrington 1981). Turgor may be exacerbated in older people by reduced skin moisture content (Potts et al. 1984), altered skin elasticity (Daly and Odland 1979), or poor peripheral blood flow (Evans et al. 1993).
In this study, we made a comprehensive survey of age-related changes in cutaneous perceptual thresholds across the glabrous and hairy skin on both hands. Up to 10 sites on both hands were tested using three modalities: von Frey filaments, two-point discrimination, and texture discrimination (Miller et al. 2009). To investigate the role of skin mechanics while minimizing the impact on neural properties, we used venous occlusion to alter the fluid volume of the hand; moisturized the skin; and tested turgor with skin deformation. We hypothesized that sites on the fingers would show greater age-related change than sites on the palm, and these changes would be exacerbated in older decades by changes in skin mechanics. However, our results suggest a complex pattern of changes in cutaneous sensation that vary not only with age but also across the hand, between hands, and between the sexes. Changes in skin mechanics were not associated with age-related changes in cutaneous sensation.
Methods
General procedures
Studies were performed on 70 neurologically healthy subjects over seven decades from the 20s to the 80s (20 to 88 years, 35 males and 35 females). Subjects were screened for overt symptoms of sensory or motor dysfunction including peripheral neuropathies, diabetes, and other neurological conditions prior to testing. Older subjects who reported osteoarthritis were asymptomatic at the time of testing. The dominant and non-dominant hands were tested in five males and five females for each decade (mean, range): 20s (24.1 years, 20–29 years), 30s (34.6 years, 30–39 years), 40s (45.6 years, 42–49 years), 50s (53.8 years, 50–59 years), 60s (64.5 years, 60–69 years), 70s (74.6 years, 71–78 years), and 80s (84.1 years, 81-88 years). To exclude higher functional deficits including dementia, cognitive performance was screened as Mini-Mental State Examination (MMSE) scores ≥24 (Folstein et al. 1975). All subjects gave written, informed consent. Ethical approval was given by the Human Research Ethics Committee, University of New South Wales, and experiments were conducted in accordance with the Declaration of Helsinki.
Perceptual thresholds
Experimental procedure
Subjects nominated their dominant hand (Van Turnhout et al. 1997); in all cases, this corresponded to the hand used when signing the consent form. After familiarization with test procedures, the dominant hand was tested before the non-dominant hand. Subjects sat with their test hand resting on a table and masked from view. No feedback was provided until testing was completed. All assessments were performed by the first author and were completed in a single session of ~90 min.
von Frey thresholds
Calibrated von Frey filaments (North Coast Medical, USA) were used to establish perceptual thresholds to punctuate cutaneous stimuli. Eight sites on the glabrous skin and two sites on the hairy skin were tested to cover the innervation territories of the median, ulnar, and radial nerves (Fig. 1a). The location of a perceived stimulus was identified according to the numbered picture (Fig. 1a). The timing and location of the stimuli were randomly altered, and the size of the filament decreased until the stimuli were no longer perceived. Filament size was then increased to confirm perceptual thresholds. The force exerted by the lowest perceived filament was recorded in grams as the threshold. Care was taken to ensure a single stimulus was applied orthogonal to the skin surface at each presentation. If the filament slipped or made multiple contacts on the skin, the stimulus was repeated as part of the random sequence.
Experimental setup. a Sites for von Frey threshold testing. Sites 1–8 are located on the glabrous skin and sites 9–10 on the hairy skin. The dashed line indicates the approximate delineation between ulnar and median nerve territories. b Two-point discrimination was tested at sites a–c. Texture discrimination thresholds were measured at site 1 and turgor at site 3. c The AsTex measure of texture discrimination is illustrated here for testing the right hand. d Turgor setup up for the left hand
Two-point stimulation
Three sites on the glabrous skin were tested using static two-point discrimination (Fig. 1b). A small- and large-interval Mackinnon-Dellon Disk-Criminator (US Neurologicals, USA) were used to vary the stimulus interval from 2 to 8 mm and 9 to 20 mm, respectively. Stimuli were randomly alternated between test sites, test intervals, and between one and two points. In addition to the single stimulus, a minimum of three intervals were tested on the fingertips, and five on the hand sites. Two points were applied across the medio-lateral axis of the hand with care taken to ensure equal and even pressure. The minimum spacing where the stimulus was perceived as two points was recorded in millimeters as the threshold.
Texture discrimination
Texture discrimination was assessed using the AsTex (University of Melbourne, Australia). The acrylic surface of the board is engraved with 190 grooves that progressively and logarithmically decrease in size (Fig. 1c). The AsTex was positioned in front of the subject with the largest grooves contralateral to the test hand. The subject was instructed to slide the pad of the index finger slowly along the surface, starting from the largest grooves, and stop when it felt “smooth.” The index finger was used to allow comparison with established norms (Miller et al. 2009) and because, when unconstrained, 9 out of 10 subjects chose to use the index finger during pilot testing. A single trial was performed on each hand, and the distance to the stopping point was recorded to the nearest 5 mm and converted to groove width in millimeters using a conversion chart (Miller et al. 2009).
Skin mechanics
Skin mechanics were varied with minimal impact on neural properties in two ways. First, the fluid volume of the hand was altered with venous occlusion by inflating a pediatric blood pressure cuff around the wrist to 40 ± 10 mmHg for 10 min. Second, the mechanical transduction properties of the skin were altered by applying moisturizer to both hands (males 5–6 mL, females 2–3 mL, Biotech Pharmaceuticals, Australia) allowing 10 min for absorption before testing. von Frey thresholds and two-point discrimination were repeated after each intervention with moisturizing undertaken last. The minimum time (10 min) to elicit maximum changes for venous occlusion and moisturizing was established in four subjects (20–49 years) during pilot studies. The efficacy of occlusion was noted as distinct color changes in the hand with apparent blood congestion (red, mottled appearance), especially in older subjects. During venous occlusion, subjects were asked to report the onset of sensory symptoms indicative of nerve compression such as tingling, pins and needles, or any general discomfort caused by the cuff.
Skin compliance in the fingertip was measured as a surrogate of turgor. A subset of subjects (n = 30), five per decade were studied from the 20s to the 70s (for logistical reasons, the 80s could not be tested). Two males and three females, or vice versa, were tested per decade. Turgor was measured at the center of the pulp on the distal phalanx of the little finger (i.e., site 3, Fig. 1b) using a 1-mm probe connected to an isometric force transducer (FT03, Grass Technologies, USA) (Fig. 1d). The probe was standardized to the diameter of the largest 300 g von Frey filament. Force (newton) was filtered (bandwidth DC-500 kHz), amplified (gain 102), and digitized (2 kHz) using a 1401 data acquisition card and Spike2 analysis software (CED, UK).
The test hand was secured in a semi-pronated position against a fixed surface with Velcro straps. The test digit was immobilized by taping string to the fingernail and securing this to the fixed surface so that there was nothing in contact with the glabrous skin (Fig. 1d). The transducer tip was positioned to just make contact with the finger pulp without any discernible skin deformation. The probe was then advanced and withdrawn in 1-mm increments against the finger to a maximum of 5 mm. Turgor was measured as the average force exerted against the probe over 10 s at each 1-mm increment and expressed as absolute change (newton) between the 0- and 5-mm indentation. These measurements were repeated during venous occlusion.
Data and statistical analysis
Data were analyzed by age (seven decades), sex, and hand. Data for age, sex, handedness, and site were analyzed using a Kruskal–Wallis one-way ANOVA. Interactions were assessed with a two-way ANOVA with age and sex as between-subject factors, and hand and site as within-subject factors. Two-way repeated measures ANOVAs were used to investigate threshold differences after venous occlusion and moisturizing. A linear regression was used to assess the relationship between texture discrimination and von Frey sensory thresholds of the distal phalanx of the index finger. Normally distributed data are presented as mean ± standard error of the mean with Holm–Sidak post-hoc analyses. Data that were not normally distributed are reported as median and interquartile range with Tukey post-hoc analyses. Results were considered significant when p < 0.05.
Results
An increase in perceptual threshold reflects a decrease in cutaneous sensation. To avoid confusion, we will refer only to increased thresholds. All subjects scored ≥28 on the Mini-Mental State Examination.
von Frey stimuli
Absolute values for all sites and all conditions are illustrated in Fig. 2. The von Frey threshold averaged across all 10 sites increased in the hand as a function of age, with a fourfold increase from 0.04 g [0.02–0.07 g] for the 20s to 0.16 g [0.04–0.4 g] (p < 0.001) for the 80s. Significant interactions were seen between age and sex (p < 0.001) with thresholds higher in males (Fig. 2a). The absolute difference in threshold between the sexes became significant in later decades being 0.17 ± 0.02 g, p < 0.001 in the 60s; 0.05 ± 0.02 g, p = 0.028 in the 70s; and 0.15 ± 0.02 g, p < 0.001 in the 80s compared to no difference in decades <60. Thresholds were also higher in the dominant compared to the non-dominant hand. Although these differences were not significant (Fig. 2a), they became more prominent after 60 years, with a mean threshold difference between hands of 0.03 ± 0.02 g for the 60s, 0.06 ± 0.02 g for the 70s, and 0.07 ± 0.02 g for the 80s, compared to no difference in those aged <60 years.
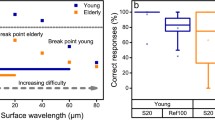
Age-related changes in von Frey and two-point discrimination thresholds. a von Frey thresholds presented by hand and decade (p < 0.001). Higher thresholds indicate poorer sensation. The changes in dorsal sites (9–10) are largely obscured by prominent changes at sites on the hand, particularly site 8. b Two-point discrimination thresholds by decade (p = 0.046) with hands combined (p > 0.05). Differences in thresholds were seen between the finger (site a) and hand (sites b and c). Overall, changes in two-point discrimination were smaller than von Frey thresholds
The pattern of sensation changes with age was different for males and females. For all 10 sites on both hands combined, significant increases in cutaneous thresholds occurred from the 60s for males and the 70s for females. Separate two-way ANOVAs were undertaken for each sex with age and hand as factors. Thresholds were always highest in the 80s, the lowest threshold varied between decades with sex and hand (Fig. 2a). The differences between hands are therefore reported relative to the decade with the lowest threshold. For females, the interaction between age and hand (p = 0.044) became significant from the 70s, but only for the dominant hand (Fig. 2a). Thresholds were lowest for females in the 20s for both hands. The mean difference between hands for 70s females was 0.16 ± 0.03 g, and 0.11 ± 0.03 g for 80s, p < 0.001. In contrast, thresholds were lowest for males in the 30s on the dominant hand and the 20s on the non-dominant hand. As both thresholds increased significantly with age, there was no interaction between age and hand for males.
There were significant interactions for cutaneous thresholds between age, sex, and site (p = 0.001)(Table 1). The largest change for males was for sites in the palm (sites 5 to 8, Fig. 2a) and the proximal phalanx of the little finger (site 4, Fig. 2a). The only significant increases for females were on the hypothenar eminence and the proximal phalanx of the little finger (sites 8 and 4) of the dominant hand. This difference was greatest for males. The threshold increase for females was only 25–50 % of that for males, matched for site. In contrast to the glabrous skin, sites on the hairy skin showed little change with age. The only significant increase was seen in females at site 10 on the back of the hand (Table 1).
To compare our results to previous studies which predominantly examine sensation at the tip of the index finger, von Frey thresholds at this site (site 1, Fig. 1a) were examined using a two-way ANOVA. There was a significant increase in thresholds at this site with age, but post-hoc pairwise comparisons show that this only occurs after 80 years for both males and females (both p = 0.003). Thresholds for males increased from 0.05 ± 0.03 g in the 30s to 0.25 ± 0.03 g in the 80s; and those for females from 0.03 ± 0.03 g in the 20s to 0.20 ± 0.03 g in the 80s.
We compared the combined results for thresholds measured across sites 1, 2, and 7 to sites 3, 4, and 8 on both hands, i.e., the ulnar versus median nerve territories. There was no significant difference in the thresholds measured between innervation territories or any interaction between hands. The median threshold for both areas of skin innervation was 0.07 g [0.04–0.16 g].
Two-point discrimination
The threshold for two-point discrimination increased significantly with age (p = 0.046)(Fig. 2b). Thresholds were lowest in the 20s with a median interval of 5 mm [3–8 mm] and highest in the 60s with a median interval of 7 mm [4–11 mm]. Thresholds in the 80s were slightly lower with a median interval of 6 mm [4–11 mm]. Consistent with von Frey results, thresholds were higher for males, with a median of 7 mm [4–10 mm], compared to the median for females of 6 mm [3–9 mm] (p = 0.023). Likewise, the median threshold interval for both sites on the palms were 8 mm [6–11 mm] (sites b and c) which was significantly higher than that on the fingertip (site a), 3 mm [3–4 mm] (p < 0.001). There was no significant difference between the dominant and non-dominant hands, and no interaction was seen between age and sex, hand, or site (Fig. 2b). The relationship between the force exerted on the skin during standard two-point discrimination and von Frey testing was examined in 10 subjects. Two-point discrimination stimuli were held in contact with the skin for ~400 ms, longer than von Frey filaments at <3 ms, and the force applied by the single prong of the test wheel was equivalent to either of the two largest von Frey filaments, 150 or 300 g (both 1 mm in diameter).
We compared the change in threshold for two-point discrimination at sites a, b, and c to those for von Frey filaments at the equivalent sites, i.e., 1, 6, and 8 (Fig. 1a, b) by pooling the data for all ages. A significant correlation between methods was only found for males and only at the fingertip (site 1/site a) with a coefficient of determination of 0.115 (p = 0.026).
Texture discrimination
The threshold for texture discrimination increased with age, although not significantly. Thresholds increased steadily until the 80s, after which they improved again. Texture discrimination thresholds ranged from 0.27 mm [0.2–0.4 mm] in the 20s to 0.44 mm [0.3–0.6 mm] in the 70s returning to 0.31 mm [0.3–0.4 mm] in the 80s. There was no interaction with age for either sex or hand. There was a positive linear regression between texture discrimination and von Frey thresholds on the non-dominant index finger (r 2 = 0.16, p < 0.001) but not the dominant finger. AsTex thresholds reported previously (Miller et al. 2009) were substantially higher, 0.59 mm [0.35–0.97 mm] in the 20s to 0.97 mm [0.52–1.20 mm] in subjects >70 years (median and 90 % confidence interval).
Skin mechanics
Significant improvements in von Frey thresholds were seen after moisturizing (p = 0.005), but not with venous occlusion (Fig. 3). This pattern predominantly occurred in males and was age dependent. von Frey thresholds deteriorated linearly after moisturizing from 20s to 60s by 0.05 ± 0.01 g (p = 0.046) before significantly improving by 0.08 ± 0.01 g in the 80s (p = 0.001) (Fig. 3a). After venous occlusion, thresholds for males improved by 0.03 ± 0.01 g in the 70s and a further 0.02 ± 0.01 g in the 80s; however, this was not significant (Fig. 3b). There was no improvement in von Frey thresholds for females after either intervention, and two-point discrimination did not change for any group.
Change in von Frey thresholds after moisturizing and venous occlusion are shown by decade and sex as the absolute change from the pre-intervention threshold (grams) for each decade; filled bars males, open bars females (p > 0.05). Note the change in direction of the response for males after the 60s for both interventions. *p < 0.05; **p < 0.01
There was no change in turgor with age when measured as fingertip compliance on the little finger. The measured force was higher in males than females (p = 0.026), but there was no interaction between age and either sex or hand, and no change with venous occlusion. Because there was no evidence of a hysteresis in skin compliance between the indentation and withdrawal phases, only the indentation data were analyzed. The combined data for both hands were best represented by a quadratic relationship (r 2 = 0.29, p < 0.001) between indentation and force. The relationship was stronger for males (r 2 = 0.42, p < 0.001) than females (r 2 = 0.20, p < 0.001).
Discussion
We made a detailed survey of age-related changes in cutaneous sensation across multiple sites on both hands. Our results demonstrate a complex pattern of perceptual thresholds that change not only with age but between the sexes, the dominant and non-dominant hands, and across sites on the same hand. These data emphasize how age-related deterioration in sensation varies with the test modality and that von Frey filaments provide the most sensitive test of age-related changes in cutaneous sensation (compare Fig. 2a, b). von Frey and two-point discrimination thresholds were higher in males than females; von Frey thresholds were higher in the dominant than the non-dominant hand; and age-related changes in sensation on the palms deteriorated more than on the fingertips or dorsal surface. Texture discrimination was not a sensitive test of age-related changes in cutaneous sensation. Threshold changes at the hypothenar eminence increased consistently with age, regardless of sex or hand. If only one site were to be tested, our results suggest the hypothenar eminence is the site with the greatest age-related change in the hand. Although the effect of healthy ageing on cutaneous sensation is significant, the magnitude of sensory thresholds remained low, albeit with an approximately fourfold increase across all sites due to ageing. The most important finding of this comprehensive survey is the complexity of the pattern of the changes, and that the decline in cutaneous sensation accelerates in healthy people after the age of 60 for males and 70 for females.
Methodological considerations
The magnitude of age-related deterioration in cutaneous sensation may have been underestimated in this study by the self-selecting nature of the volunteer participants who came to the laboratory for testing. The majority of subjects were either retired or in occupations not regularly exposed to excessive vibration or high-impact forces. Younger participants (20s) were mostly university students and older subjects were healthy, active, and living independently. All were neurologically healthy at the time of testing although some older participants reported asymptomatic osteoarthritis. The incidence of subclinical carpal tunnel syndrome cannot be excluded in this population; however, the similarity of von Frey thresholds for sites within both median and ulnar nerve territories argues against this. Similarly, the MMSE may not identify subtle cognitive changes that may impact perceptual responses. However, because the lowest MMSE score in this cohort was 28, we do not believe that reduced cognitive ability was a factor in this study. Despite the apparent good physical and cognitive health, a spectrum of age-related changes in sensation was present even in this healthy cohort.
We used a numbered picture during von Frey testing, but not otherwise. The picture was introduced to facilitate identification of the 10 test sites and to restrict the total test duration to ~90 min, the concentration limit for older subjects. The test site for the distal median nerve territory was shifted from the index fingertip to the middle finger for two-point discrimination to minimize the incidence of additional pressure being inadvertently exerted against the test prongs by the index finger (which markedly altered thresholds). We do not believe that this invalidates the comparisons between von Frey and two-point discrimination thresholds, as thresholds for the latter are less sensitive and do not differ between these sites (Gellis and Pool 1977). The influence of skin hydration was more difficult to assess. While we are confident that our test of turgor was a valid measure of skin compliance, but it may not sufficiently account for changes in hydration (Dorrington 1981). Although the use of moisturizer was designed to alter skin hydration, the only effect was for 80s males. A more sensitive measure might be obtained from the electrical capacitance of the stratum corneum, tested with corneometry (Girard et al. 2000).
Are tests of cutaneous sensation equivalent and what do they measure?
The assessments used in this study were selected as those commonly employed in clinical practice and sufficiently portable to allow use in the field. We also chose tests that were appropriate for assessing sensory impairments in neurological conditions such as stroke and spinal cord injury where patients may have poor concentration, aphasia, and joint stiffness and contracture that limit upper-limb positioning in static devices. Therefore, the test battery needed to be quick, appropriate for patient populations, require simple responses, and allow the assessor to easily access different areas of the hand. We acknowledge that there are more sophisticated methods of assessing sensory thresholds, but they were not appropriate for this study.
Our results emphasize the extent to which the test method affects the measurement of age-related changes in sensation. Differences were found between von Frey and two-point discrimination thresholds, even when assessed at the same site. von Frey thresholds highlighted the subtle differences between age, sex, hand, and site whereas two-point discrimination only showed differences between sex and age, but not between hands. Two-point discrimination (sites a, b, and c) was less sensitive between sites with the range of thresholds three to four times lower than von Frey thresholds at the equivalent sites (sites 1, 6, and 8). Texture discrimination was only measured at the index fingertip and did not discriminate between age, sex, or hand, although the thresholds in this study were lower than those reported previously (Miller et al. 2009).
The magnitude of threshold changes varied with each of the three methods. This presumably reflects differences in both the application of the stimulus, and the number and sensitivity of the mechanoreceptors responding to the stimulus. von Frey filaments deliver a brief, punctuate stimulus with a known force using a filament of minimal diameter. The force, diameter, and application duration for two-point discrimination were all at least 10 times greater than those of the largest von Frey filament used. Thus, even a single prong of the two-point discrimination test must evoke more repetitive discharges from a larger population of cutaneous receptors than the von Frey filaments, while two prongs distribute skin stretch over a larger surface (see below) activating even more receptors. The width of the index fingertip is maintained in constant contact with the AsTex for ~2–5 s with an uncontrolled force during texture discrimination. Skin stretch is presumably even greater as the finger moves across the textured surface further increasing the pool of activated sensory receptors.
All three methods require different cognitive processes. A response is given only when the presence and location of a von Frey stimulus is perceived. False positives do occur, but because thresholds are double-checked their influence is minimized (Bell-Krotoski et al. 1993). Two-point discrimination employs a forced-choice paradigm in which subjects must nominate whether one or two points are perceived. The incidence of guessing is difficult to quantify. Texture discrimination requires a co-ordinated response so that movement is halted when a change in sensation is perceived. To what extent the vibration induced by the surface itself impacts on sensation has not been investigated.
Changes across the hand
The magnitude of age-related changes varied according to the site of testing. Contrary to our hypothesis, thresholds were highest, and increased most, in males at sites on the palm of the dominant hand. In general, cutaneous sensation changed less on the fingers, whether distal or proximal, and on the back of the hand. Although age-related changes on the back of the hand have not been reported previously, it is not surprising that sensation on the hairy skin deteriorates less with age, particularly for males. This reflects the distribution of thick terminal hairs (Tur 1997) which may provide greater protection for the hair follicle sensory receptors that are exquisitely sensitive to movement (Vallbo et al. 1995).
In the glabrous, or hairless, skin of the palmar surface of the hand there are four low-threshold mechanoreceptors that subserve cutaneous sensation (for review, see Johansson and Vallbo 1983). Human microneurographic studies show all receptors types respond to von Frey filaments at or above threshold (Johansson and Vallbo 1979), and that there is a proximal to distal gradient in the density of the two receptors with the greatest spatial and temporal acuity, Meissner’s corpuscles, and Merkel cell neurite complexes (Johansson and Vallbo 1979). Presumably, the lower receptor density of these more proximally in the hand contributes to higher thresholds in the hypothenar eminence. The Pacinian corpuscles and Ruffini endings are more evenly distributed (Cauna and Mannan 1958; Johansson and Vallbo 1979). A decline in the population of sensory receptors with age has only been demonstrated for Meissner's corpuscles (Cauna 1956; Bruce 1980) although morphological changes have been reported for Meissner’s, Merkel, and Pacinian receptors (Cauna 1956, 1965).
Two factors may protect sensory discrimination at the fingertip. First, the density of Meissner and Merkel receptors (Johansson and Vallbo 1979) may afford a greater redundancy, providing resilience against the effects of age-related mechanoreceptor loss. This may be particularly evident in women or men with smaller fingers where the more densely packed receptors have been suggested to improve acuity (Peters et al. 2009). Second, Merkel receptors have the highest acuity (Phillips et al. 1990) but are the only low-threshold receptors in the glabrous skin of the hand for which a role in fine motor control could not be demonstrated (McNulty et al. 1999; McNulty and Macefield 2001). This suggests that Merkel receptors may have stronger connections to the somatosensory cortex than other low-threshold mechanoreceptors and so provide a learnt attentional focus to cutaneous inputs (McNulty and Macefield 2001).
Sensory thresholds may also be influenced by changes to skin mechanics. The performance of gross motor activities, such as the power grip, predisposes the palm to greater external forces and excessive wear caused by stresses such as friction. The greater morphological changes and reduced numbers of Meissner’s corpuscles seen in the hands of older manual workers and to a lesser extent, older males in general (Cauna 1956, 1965), suggest that increased damage may occur to neuromuscular structures in high contact areas (Cauna 1965). Previous studies found no difference between sensory declines on the dorsal and ventral sides of the finger (Stevens et al. 2003) and foot (Mitchell and Mitchell 2000) with age, and suggested increases in skin thickness (Mitchell and Mitchell 2000) and skin wear (Stevens et al. 2003) did not contribute to sensory decline. However, in these studies, the skin of the palm was not investigated.
Do changes in skin mechanics contribute to declines in cutaneous sensation?
The results from interventions designed to change skin mechanics were not conclusive. The change was minimal for females and complex for males (Fig. 3a–b). These results agree with previous studies that found no relationship between skin compliance or conformity and cutaneous sensation in those aged <80 years (Woodward 1993; Vega-Bermudez and Johnson 2004). Although skin thickness declines with age for both sexes (Roberts et al. 1975; Hall et al. 1981), males have thicker skin than females across the life span with greater sebum content (Escoffier et al. 1989; Fruhstorfer et al. 2000). The reduction in skin compliance is presumably due to less compartmentalization of circulating fluid in the fingertips as the confining protein matrix and terminal elastic fibers of the skin change with age (Montagna and Carlisle 1979). We hypothesized that the resulting change in interstitial pressure at the fingertip would reflect turgor (Fig. 1d). However, the measured forces did not change with age, contrary to our hypothesis, but consistent with the minimal changes in von Frey thresholds at the fingertip of digit V. During this test, care was taken to position the probe in the middle of the pulp, although the dense arrangement of capillary beds in the terminal pad of the finger evenly distributes blood volume in the fingertip (Wood Jones 1920). We could not test our preferred site on the distal phalanx of the index finger (site 1); however, our results suggest the hypothenar eminence may be a more appropriate testing location, and that this measure of turgor may change in the 80s.
Functional implications
These results provide age-appropriate data for cutaneous thresholds in healthy older subjects across multiple sites of the hand, especially in people aged >75 years for whom less data are currently available. Age-appropriate data are critical for estimating the magnitude of sensory loss that commonly occurs in neurological conditions such as stroke or diabetes (Young et al. 1993; Carey and Matyas 2011). In this study, the mean increase in cutaneous thresholds with age was relatively small, 0.13 g for females and 0.24 g for males. A change of ≥0.6 g is classified as diminished protective sensation that significantly impacts fine motor control of the hand (Bell-Krotoski 1995). Threshold changes of this magnitude, or greater, were seen in this study in at least one site in 16 subjects aged >55 years (8 males, 8 females). Nine subjects had high thresholds at multiple sites, yet only two subjects had this level of impairment on the fingertips. It has been suggested that testing multiple sites may be more effective at identifying sensory neuropathies in older patients in the foot (Modawal et al. 2006). To our knowledge, there are no similar studies in the hand, although our data suggest testing at multiple sites may be useful in identifying isolated sensory deficits compared to more systemic peripheral neuropathies.
Reduced cutaneous sensation has also been correlated with poor hand function (Dellon et al. 1997; Melchior et al. 2007), but the relationship between higher cutaneous thresholds at the fingertips and impaired motor performances are inconsistent (Cole et al. 1998; Ranganathan et al. 2001; Aoki and Fukuoka 2010; Murata et al. 2010). It has also been suggested that work-related expertise in fine dexterous manipulation does not attenuate age-related changes in cutaneous sensation at the fingertip (Reuter et al. 2012). Rather, changes in cutaneous thresholds on the palm may have implications for changes in motor control, especially for tasks involving the whole hand, rather than just the fingers, e.g., power grip versus precision grip. The relationship between reduced cutaneous sensation on the palm and fine motor control has not been explored previously and may be an area for future study.
In conclusion, our results emphasize the complex pattern of changes in sensation in the hands. Age-related declines vary between sexes, the hands, sites on the hand, and the mode of testing. von Frey filaments provided the most sensitive discrimination of age-related changes across the hand, highlighting the differences between the palm, the fingertips, and the dorsal surface. The role of skin mechanics in sensory loss was not conclusive, but it may be that overuse and high forces, particularly on the palms, are implicated, but this requires further investigation. Age-related changes in sensation are typically tested on the index fingertip which may underestimate the magnitude of sensory loss. Our results suggest that a better site is the hypothenar eminence where we found the greatest and most consistent changes with age. Due to the multifaceted nature of the age-related declines in cutaneous sensation in the hands, we suggest that multiple sites within the territory of all three nerves be tested, preferably including both the fingers and the palm.
References
Aoki T, Fukuoka Y (2010) Finger tapping ability in healthy elderly and young adults. Med Sci Sports Exerc 42:449–455
Axelrod S, Cohen LD (1961) Senescence and embedded figure performance in vision and touch. Percept Mot Skills 12:283–288
Bear-Lehman J, Miller PA, Adler M, Buonocore JM, Coles N, Kneafsey BS, Katz-Sillman F, Sherman-Amsel H (2003) An exploration of hand strength and sensation in community elders. Top Geriatr Rehabil 19:127–136
Bell-Krotoski J (1995) Sensibility testing: current concepts. In: Hunter JM, Mackin EJ, Callahan AD (eds) Rehabilitation of the hand: Surgery and therapy, 4th edn. Mosby, St. Louis
Bell-Krotoski J, Weinstein S, Weinstein C (1993) Testing sensibility, including touch-pressure, two-point discrimination, point localization, and vibration. J Hand Ther 6:114–123
Bovenzi M, Zadini A (1989) Quantitative estimation of aesthesiometric thresholds for assessing impaired tactile sensation in workers exposed to vibration. Int Arch Occup Environ Health 61:431–435
Bruce MF (1980) The relation of tactile thresholds to histology in the fingers of elderly people. J Neurol Neurosurg Psychiatry 43:730–734
Caccia MR, McComas AJ, Upton AR, Blogg T (1973) Cutaneous reflexes in small muscles of the hand. J Neurol Neurosurg Psychiatry 36:960–977
Carey LM, Matyas TA (2011) Frequency of discriminative sensory loss in the hand after stroke in a rehabilitation setting. J Rehabil Med 43:257–263
Cauna N (1956) Nerve supply and nerve endings in Meissner's corpuscles. Am J Anat 99:315–350
Cauna N (1965) The effects of aging on the receptors organs of the human dermis. In: Montagna W (ed) Advances in Biology of Skin, vol VI, Aging. Pergamon Press, New York, pp 63–96
Cauna N, Mannan G (1958) The structure of human digital Pacinian corpuscles (corpus cula lamellosa) and its functional significance. J Anat 92:1–20
Cole KJ, Rotella DL, Harper JG (1998) Tactile impairments cannot explain the effect of age on a grasp and lift task. Exp Brain Res 121:263–269
Cottrell L (1940) Histologic variations with age in apparently normal peripheral nerve trunks. Arch Neurol Psychiatry 43:1138–1150
Daly CH, Odland GF (1979) Age-related changes in the mechanical properties of human skin. J Invest Dermatol 73:84–87
Dannenbaum RM, Michaelsen SM, Desrosiers J, Levin MF (2002) Development and validation of two new sensory tests of the hand for patients with stroke. Clin Rehabil 16:630–639
Dellon ES, Keller KM, Moratz V, Dellon AL (1997) Validation of cutaneous pressure threshold measurements for the evaluation of hand function. Ann Plast Surg 38:485–492
Desrosiers J, Hébert R, Bravo G, Dutil É (1996) Hand sensibility of healthy older people. J Am Geriatr Soc 44:974–978
Deuschl G, Feifel E, Guschlbauer B, Lucking CH (1995) Hand muscle reflexes following air puff stimulation. Exp Brain Res 105:138–146
Dorrington KL (1981) Skin turgor: do we understand the clinical sign? Lancet 317:264–266
Escoffier C, de Rigal J, Rochefort A, Vasselet R, Lévêque J-L, Agache PG (1989) Age-related mechanical properties of human skin: an in-vivo study. J Investig Dermatol 93:353–357
Evans E, Rendell M, Bartek J, Connor S, Bamisedun O, Dovgan D, Giitter M (1993) Thermally-induced cutaneous vasodilatation in aging. J Gerontol 48:M53–57
Folstein MF, Folstein SE, McHugh PR (1975) Mini-mental state. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12:189–198
Fruhstorfer H, Abel U, Garthe CD, Knüttel A (2000) Thickness of the stratum corneum of the volar fingertips. Clin Anat 13:429–433
Gellis M, Pool R (1977) Two-point discrimination distances in the normal hand and forearm: application to various methods of fingertip reconstruction. Plast Reconstr Surg 59:57–63
Girard P, Beraud A, Sirvent A (2000) Study of three complementary techniques for measuring cutaneous hydration in vivo in human subjects: NMR spectroscopy, transient thermal transfer and corneometry – application to xerotic skin and cosmetics. Skin Res Technol 6:205–213
Hall DA, Blackett AD, Zajac AR, Switala S, Airey CM (1981) Changes in skinfold thickness with increasing age. Age Ageing 10:19–23
Jette AM, Branch LG, Berlin J (1990) Musculoskeletal impairments and physical disablement among the aged. J Gerontol 45:M203–M208
Johansson RS, Vallbo ÅB (1979) Tactile sensibility in the human hand: relative and absolute densities of four types of mechanoreceptive units in glabrous skin. J Physiol 286:283–300
Johansson RS, Vallbo ÅB (1983) Tactile sensory coding in the glabrous skin of the human hand. Trends Neurosci 6:27–32
Johansson RS, Westling G (1984) Roles of glabrous skin receptors and sensorimotor memory in automatic control of precision grip when lifting rougher or more slippery objects. Exp Brain Res 56:550–564
Kalisch T, Tegenthoff M, Dinse HR (2008) Improvement of sensorimotor functions in old age by passive sensory stimulation. Clin Interv Aging 3:673–690
Macefield VG, Johansson RS (1996) Control of grip force during restraint of an object held between finger and thumb: responses of muscle and joint afferents from the digits. Exp Brain Res 108:172–184
McNulty PA, Macefield VG (2001) Modulation of ongoing EMG by different classes of low-threshold mechanoreceptors in the human hand. J Physiol 537:1021–1032
McNulty PA, Turker KS, Macefield VG (1999) Evidence for strong synaptic coupling between single tactile afferents and motoneurones supplying the human hand. J Physiol 518:883–893
Melchior H, Vatine JJ, Weiss PL (2007) Is there a relationship between light touch-pressure sensation and functional hand ability? Disabil Rehabil 29:567–575
Miller KJ, Phillips BA, Martin CL, Wheat HE, Goodwin AW, Galea MP (2009) The AsTex: clinimetric properties of a new tool for evaluating hand sensation following stroke. Clin Rehabil 23:1104–1115
Mitchell PD, Mitchell TN (2000) The age-dependent deterioration in light touch sensation on the plantar aspect of the foot in a rural community in India: Implications when screening for sensory impairment. Lepr Rev 71:169–178
Modawal A, Fley J, Shukla R, Rudawsky D, Welge J, Yang J (2006) Use of monofilament in the detection of foot lesions in older adults. J Foot Ankle Surg 45:76–81
Montagna W, Carlisle K (1979) Structural changes in aging human skin. J Invest Dermatol 73:47–53
Murata J, Murata S, Hiroshige J, Ohtao H, Horie J, Kai Y (2010) The influence of age-related changes in tactile sensibility and muscular strength on hand function in older adult females. Int J Gerontol 4:180–183
O'Sullivan DJ, Swallow M (1968) The fibre size and content of the radial and sural nerves. J Neurol Neurosurg Psychiatry 31:464–470
Peters RM, Hackeman E, Goldreich D (2009) Diminutive digits discern delicate details: fingertip size and the sex difference in tactile spatial acuity. J Neurosci 29:15756–15761
Phillips JR, Johansson RS, Johnson KO (1990) Representation of braille characters in human nerve fibres. Exp Brain Res 81:589–592
Potts RO, Buras EM Jr, Chrisman DA Jr (1984) Changes with age in the moisture content of human skin. J Investig Dermatol 82:97–100
Potvin AR, Syndulko K, Tourtellotte WW, Lemmon JA, Potvin JH (1980) Human neurologic function and the aging process. J Am Geriatr Soc 28:1–9
Ranganathan VK, Siemionow V, Sahgal V, Yue GH (2001) Effects of aging on hand function. J Am Geriatr Soc 49:1478–1484
Reuter EM, Voelcker-Rehage C, Vieluf S, Godde B (2012) Touch perception throughout working life: effects of age and expertise. Exp Brain Res 216:287–297
Rexed B (1944) Fibre size in the peripheral nervous system of adults and old persons. Acta Physiol Scand 19:164–186
Roberts MA, Andrews GR, Caird FI (1975) Skinfold thickness on the dorsum of the hand in the elderly. Age Ageing 4:8–15
Stevens JC, Choo KK (1996) Spatial acuity of the body surface over the life span. Somatosens Mot Res 13:153–166
Stevens JC, Alvarez-Reeves M, Dipietro L, Mack GW, Green BG (2003) Decline of tactile acuity in aging: a study of body site, blood flow, and lifetime habits of smoking and physical activity. Somatosens Mot Res 20:271–279
Thornbury JM, Mistretta CM (1981) Tactile sensitivity as a function of age. J Gerontol 36:34–39
Tremblay F, Mireault AC, Dessureault L, Manning H, Sveistrup H (2005) Postural stabilization from fingertip contact II. Relationships between age, tactile sensibility and magnitude of contact forces. Exp Brain Res 164:155–164
Tur E (1997) Physiology of the skin: differences between women and men. Clin Dermatol 15:5–16
Vallbo ÅB, Olausson H, Wessberg J, Kakuda N (1995) Receptive field characteristics of tactile units with myelinated afferents in hairy skin of human subjects. J Physiol 483:783–795
van Nes SI, Faber CG, Hamers RMTP, Harschnitz O, Bakkers M, Hermans MCE, Meijer RJ, van Doorn PA, Merkies ISJ (2008) Revising two-point discrimination assessment in normal aging and in patients with polyneuropathies. J Neurol Neurosurg Psychiatry 79:832–834
Van Turnhout AA, Hage JJ, De Groot PJ, De Lange-De Klerk ES (1997) Lack of difference in sensibility between the dominant and non-dominant hands as tested with Semmes-Weinstein monofilaments. J Hand Surg Br 22:768–771
Vega-Bermudez F, Johnson KO (2004) Fingertip skin conformance accounts, in part, for differences in tactile spatial acuity in young subjects, but not for the decline in spatial acuity with aging. Percept Psychophys 66:60–67
Verrillo RT, Bolanowski SJ, Checkosky CM, McGlone FP (1998) Effects of hydration on tactile sensation. Somatosens Mot Res 15:93–108
Weber EH (1834) The sense of touch. Academic Press for Experimental Psychology Society, London, trans: Ross HE, Murray DJ, 1978
Wood Jones F (1920) The principles of anatomy as seen in the hand. Churchill, London
Woodward KL (1993) The relationship between skin compliance, age, gender, and tactile discriminative thresholds in humans. Somatosens Mot Res 10:63–67
Young M, Boulton A, Macleod A, Williams D, Sonksen P (1993) A multicentre study of the prevalence of diabetic peripheral neuropathy in the United Kingdom hospital clinic population. Diabetol 36:150–154
Acknowledgments
This work was supported by the National Health and Medical Research Council of Australia; the New South Wales Office of Science and Medical Research; and the University of New South Wales.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Bowden, J.L., McNulty, P.A. Age-related changes in cutaneous sensation in the healthy human hand. AGE 35, 1077–1089 (2013). https://doi.org/10.1007/s11357-012-9429-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11357-012-9429-3