Abstract
Although Ahvaz is considered as one of the warmest cities around the world, few epidemiological studies have been conducted on the adverse effects of temperature on human health using thermal indices in this city. This study investigates the relation between physiologically equivalent temperature (PET) and respiratory hospital admissions in Ahvaz. Distributed lag non-linear models (DLNMs) combined with quasi-Poisson regression models were used to investigate the relation between PET and respiratory disease hospital admissions, adjusted for the effect of time trend, air pollutants (NO2, SO2, and PM10), and weekdays. The analysis was performed by utilizing R software. Low PET values significantly decreased the risk of hospital admissions for total respiratory diseases, respiratory diseases in men and women, chronic obstructive pulmonary diseases (COPD), and bronchiectasis. However, low PET (16.9°C) in all lags except lag 0–30 significantly increased the risk of hospital admissions for asthma. The results indicate that in Ahvaz, which has a warm climate, cold weather decreased overall respiratory hospital admissions, except for asthma.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The hypothesis that meteorological variables can affect human health has been around since the middle of the twentieth century. Due to the intense heat events in the last 30 years, this period is considered to be the warmest period since 1880 (Guha-Sapir et al. 2016; NOAA 2017). According to credible evidence, both extreme temperatures (cold and heat) play a role in creating considerable physiological pressure on the human body that can cause a range of complications and mortality (Gasparrini et al. 2010; Gasparrini et al. 2015; Zhang et al. 2017). With increasing environmental changes, most industrialized and developing countries have seen an increase in the number of respiratory diseases in recent decades (D’Amato et al. 2015a; Haines and Ebi 2019). Some researchers think that respiratory diseases are closely related to high and low temperatures (Bunker et al. 2016).
So far, several studies around the world have reported a link between exposure to extreme ambient temperature and an increase in hospital admissions for respiratory diseases. For example, a study in Hong Kong during 2000–2016 indicated increased respiratory hospitalizations after hot weather, but decreased respiratory hospitalizations after cold weather (Sun et al. 2019). Also, a recent research showed that heat waves increased the number of outpatient hospital visits for respiratory diseases in Cangnan, China (Zhang et al. 2019). Moreover, in rural China, only low temperatures had a strong impact on increasing clinic visits due to respiratory illnesses (Zhao et al. 2018).
Thermal indices are used to estimate human comfort or thermal stress (Fröhlich et al. 2019). Human thermal comfort has been an important topic in academic discussions since the middle of the twentieth century on which different comparisons have been made (Abdel-Ghany et al. 2013). This suggests that the assessment and interpretation of heat stress is complex in terms of physiological and psychological stress. The proposed indicators for heat stress can be divided into three groups: “reasoning indicators,” “experimental indicators,” and “direct indicators.” Unlike the first two groups, which are complex indicators and cannot be used routinely, the last group includes simple indices based on the measurement of basic environmental variables (Epstein and Moran 2006). One of the most popular of these indicators is the physiological equivalent temperature (PET), which is a measure of human thermal comfort outdoors, and is estimated by considering the integral effects of meteorological parameters and other personal conditions related to heat exchange between the human body and its environment (Lai et al. 2018).
Observations clearly show that Iran has been warming rapidly in recent decades, resulting in a wide range of climatic effects. Meteorological records of several ground stations throughout Iran demonstrate that Iran’s temperature in 2013 was 1.3 °C warmer than in 1951(Alizadeh-Choobari and Najafi 2018; Lai et al. 2018; Saboohi et al. 2012). Although Ahvaz is one of the hottest cities in the world, no study has been done about ambient temperature and respiratory disease admissions in this city. The present study examined the impact of PET index changes on respiratory hospital admissions in Ahvaz which is located in the southwest of Iran. The findings of this study may help to plan strategies to mitigate the adverse effects of extreme weather conditions.
Materials and methods
Study site
Ahvaz is one of the metropolises of Iran, and the capital of Khuzestan province. It is the seventh most populous city in Iran. Ahvaz is located at 31° 20′ N and 48° 40′ E, with an area of 185 km2 and altitude of 12 m above sea level. According to the 2016 census, the city’s population was approximately 1,300,000 people (Statistical-Centre-of-Iran 2016).
Outcomes and exposures
Respiratory hospital admission data were obtained from the two main referral hospitals of Ahvaz, from 2008 to 2018, for 10 years. Outcomes data was classified according to the International Classification of Diseases (ICD-10) and included total respiratory diseases (J00-J99), asthma (J45.9), COPD (J44.1, J44.9), and bronchiectasis (J47).
Meteorological parameters including average daily temperature, maximum daily temperature, minimum daily temperature, average wind speed, relative humidity, and cloudiness were obtained from the Khuzestan Meteorological Department. The pollutants routinely measured in Ahvaz were NO2, PM10, and SO2 and were inquired from the Ahvaz Environmental Protection Organization.
PET index
The equations for calculating the PET index have been explained in our previous publications (Sharafkhani et al. 2018).
The no stress, thermal comfort zone for PET, similar to our previous studies (Sharafkhani et al. 2018), was assumed to be between 17.8 and 27 °C, which means there is no thermal stress for humans in this range. The median of PET in the no thermal stress zone (22.5 °C) was used as the basis for comparison. PET index analysis was performed using RayMan software. Details about this software can be found elsewhere (Lee and Mayer 2016).
The association of low values (1st, 5th, and 25th percentiles relative to no thermal stress) and high values (90th, 95th, and 99th percentiles relative to no thermal stress) of PET with risk of respiratory hospital admissions was calculated in cumulative models of 0, 0–2, 0–6, 0–13, 0–20, and 0–30 day lags. Also, similar to other studies (Lin et al. 2012; Luo et al. 2013; Sharafkhani et al. 2018; Sharafkhani et al. 2019), the association of cold thermal stress (1st percentile relative to 25th percentile) and hot thermal stress (75th percentile relative to 99th percentile) of the PET index with outcomes was evaluated in cumulative models of 0, 0–2, 0–6, 0–13, 0–20, and 0–30 day lags.
In order to investigate the effect of PET on respiratory outcomes, distributed lag non-linear models (DLNMs) combined with quasi-Poisson regression models were used (Gasparrini et al. 2010). A natural cubic spline DLNM was used to determine the non-linear relation of the PET index as well as the cumulative lag effects up to a maximum of 30 days, with respiratory hospital admission. Spline knots were set at equally spaced values on the log scale of lags. The long-term seasonal trend of the outcomes was adjusted by a natural cubic spline function of time with 7 degrees of freedom. PM10, SO2, and NO2 were controlled using the stratified distributed lag model for up to 7 days lag with 3 degrees of freedom, as done in previous studies (Sharafkhani et al. 2018). Also, the variable of holidays and weekdays was adjusted as a categorical variable in the final model (Sharafkhani et al. 2018). Akaike information criterion (AIC) models were used to select the most appropriate model and degrees of freedom (knots) for PET index and lags (Gasparrini et al. 2010). The risk ratio and 95% confidence intervals were reported. The analysis was performed by utilizing R software version 3.5.3 with the dlnm package.
Results
The descriptive statistics of respiratory hospital admissions, air pollutants, PET index, temperature, and humidity factors are presented in Table 1. During the 10-year study period, the total number of respiratory admissions was 28,041 cases with an average of 8 cases per day. More than half of the respiratory (59.2%) patients admitted were male. The daily mean of PET, temperature, and humidity were 27.6 °C, 27.0 °C, and 42.3%, respectively. The mean concentrations of PM10, NO2, and SO2 were 216.9, 46.4, and 48.8 μg/m3, respectively (Table 1).
The association between the PET index and respiratory hospital admissions in the 1st (6.4 °C), 5th (9.9 °C), 25th (16.9 °C), 90th (42.5 °C), 95th (43.6 °C), and 99th (45.4 °C) percentiles relative to the no thermal stress point (22.5°C) is presented in Table 2.
The results showed that low PET in the 1st percentile in lags 0–2 and 0–6 caused a decrease in total respiratory admissions and among the male population. In terms of specific respiratory disease, low PET in the 1st percentile in lags 0–6, 0–13, 0–20, and 0–30 significantly reduced bronchiectasis hospital admissions. Also, low PET in the 1st and 5th percentiles in lags 0–2 and 0–6 caused a significant reduction in COPD hospital admissions, while low PET in the 25th percentile in lags 0, 0–2, 0–6, 0–13, and 0–20 increased the risk of asthma hospital admissions. Also, low PET values in the 5th percentile in lags 0–20 and 0–30 increased respiratory admissions among women.
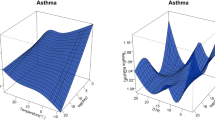
Table 3 and Fig. 1 illustrate the effects of intensified thermal stress, comparing the value of PET index in the first percentile to the 25th percentile (cold thermal stress) and comparing the value of PET index in the 99th percentile to the 75th percentile (hot thermal stress) in cumulative lags.
The results show that cold thermal stress significantly reduced the risk of total respiratory admissions in lags 0–2, 0–6, and 0–13; respiratory admissions in the male population in lags 0–2, 0–6, and 0–13; respiratory admissions in the female population in lag 0–6; and in the population < 65 years in lags 0–2, 0–6, 0–13, and 0–20. In terms of specific respiratory outcomes, cold thermal stress also significantly decreased the risk of bronchiectasis admissions in lags 0–6, 0–13, 0–20, and 0–30, and COPD hospital admissions in lags 0–2 and 0–6 (Table 3 and Fig. 1).
Hot thermal stress also significantly reduced the risk of asthma hospital admissions in lag 0 (Table 3 and Fig. 1).
Table 3 The cumulative relative risks of respiratory hospital admissions in intensified thermal stress of PET
Cold effect | Lag 0 | Lag 0–2 | Lag 0–6 | Lag 0–13 | Lag 0–20 | Lag 0–30 |
|---|---|---|---|---|---|---|
Total respiratory | 0.941 (0.853–1.039) | 0.852 (0.764–0.950)* | 0.767 (0.666–0.884)* | 0.751 (0.609–0.926)* | 0.775 (0.591–1.018)* | 0.751 (0.517–1.092)* |
Males | 0.909 (0.807–1.025) | 0.846 (0.742–0.966)* | 0.773 (0.651–0.918)* | 0.753 (0.584–0.972)* | 0.805 (0.580–1.118) | 0.755 (0.481–1.185) |
Females | 0.989 (0.858–1.139) | 0.857 (0.731–1.005) | 0.756 (0.616–0.929) | 0.743 (0.548–1.007) | 0.727 (0.489–1.082) | 0.739 (0.428–1.277) |
Under 65 years | 0.895 (0.795–1.006) | 0.809 (0.710–0.921)* | 0.725 (0.612–0.858)* | 0.666 (0.518–0.856)* | 0.665 (0.481–0.921)* | 0.679 (0.435–1.058) |
65–74 years | 1.059 (0.843–1.329) | 0.980 (0.76–1.264) | 0.908 (0.65–1.268) | 0.966 (0.59–1.582) | 1.027 (0.539–1.959) | 1.058 (0.431–2.600) |
≥75 years | 1.082 (0.881–1.33) | 0.970 (0.773–1.219) | 0.870 (0.648–1.168) | 1.043 (0.676–1.612) | 1.212 (0.691–2.125) | 0.879 (0.402–1.924) |
Asthma | 0.768 (0.560–1.054) | 0.711 (0.498–1.016) | 0.745 (0.468–1.186) | 0.863 (0.436–1.707) | 1.049 (0.428–2.57) | 1.058 (0.308–3.632) |
Bronchiectasis | 0.945 (0.661–1.349) | 0.802 (0.538–1.194) | 0.571 (0.342–0.953)* | 0.334 (0.159–0.701)* | 0.209 (0.080–0.543)* | 0.119 (0.033–0.433)* |
COPD | 0.876 (0.700–1.095) | 0.714 (0.557–0.915)* | 0.725 (0.529–0.994)* | 0.914 (0.577–1.447) | 0.909 (0.499–1.657) | 0.646 (0.281–1.489) |
Hot effect | Lag 0 | Lag 0–2 | Lag 0–6 | Lag 0–13 | Lag 0–20 | Lag 0–30 |
Total respiratory | 1.078 (0.956–1.215) | 1.064 (0.921–1.230) | 0.966 (0.802–1.164) | 0.907 (0.698–1.178) | 0.943 (0.674–1.319) | 1.099 (0.684–1.767) |
Males | 1.117 (0.964–1.294) | 1.055 (0.884–1.260) | 0.944 (0.751–1.187) | 0.893 (0.648–1.230) | 0.881 (0.584–1.328) | 1.074 (0.602–1.918) |
Females | 1.027 (0.866–1.218) | 1.075 (0.875–1.320) | 0.995 (0.763–1.296) | 0.921 (0.634–1.339) | 1.021 (0.630–1.653) | 1.110 (0.561–2.193) |
Under 65 years | 1.063 (0.925–1.221) | 1.013 (0.857–1.197) | 0.913 (0.737–1.132) | 0.855 (0.632–1.157) | 0.862 (0.585–1.270) | 1.050 (0.607–1.817) |
65–74 years | 1.149 (0.847–1.558) | 1.224 (0.849–1.766) | 1.110 (0.69–1.786) | 1.032 (0.526–2.023) | 1.087 (0.459–2.576) | 0.974 (0.289–3.281) |
≥75 years | 1.108 (0.843–1.457) | 1.270 (0.912–1.769) | 1.230 (0.801–1.888) | 1.242 (0.678–2.277) | 1.587 (0.728–3.46) | 1.829 (0.613–5.453) |
Asthma | 0.581 (0.350–0.967)* | 0.636 (0.343–1.18) | 0.866 (0.391–1.918) | 0.901 (0.289–2.814) | 0.984 (0.232–4.174) | 1.216 (0.171–8.617) |
Bronchiectasis | 1.356 (0.883–2.082) | 1.278 (0.762–2.141) | 1.199 (0.608–2.363) | 1.292 (0.485–3.446) | 1.255 (0.348–4.522) | 1.835 (0.301–11.190) |
COPD | 0.822 (0.598–1.130) | 1.000 (0.680–1.472) | 1.109 (0.676–1.819) | 0.945 (0.471–1.896) | 1.013 (0.415–2.47) | 1.081 (0.309–3.784) |
Discussion
Ahvaz is one of the hottest cities in the world; however, no study had been conducted on ambient temperature and respiratory hospital admission rates in this city.
The results of this study showed that the low values of PET index (1st, 10th, and 25th percentiles) affect hospital admissions more than the high values of PET (95th and 99th percentiles), and low levels of PET (cold weather) significantly decreased the risk of hospital admissions, due to total respiratory diseases, COPD, respiratory diseases, and bronchiectasis in most lags. But, low PET levels significantly increased the risk of asthma in all lags except 0–30, and in females in long lags.
Few studies have been conducted on the association between different temperature indices and respiratory disease incidence. There are studies that show warm weather can cause the release of inflammatory factors, increase ventilation, and exacerbate chronic obstructive pulmonary disease, which is common in the elderly (Anderson et al. 2013; Leon and Helwig 2010; Malik et al. 1983; Mannino 2011; White 2006). Anderson et al. noted that a few minutes of hot air inhalation can cause undesirable airway responses in the elderly (Anderson et al. 2013). However, one of the main reasons that hot weather did not show adverse effects in the present study was that due to the very hot weather in Ahvaz, most people stay at home or work under the cooling system especially in the middle of the day.
Contrary to our results, a study from New York City found a 2.7–3.1% increase in hospital admissions due to respiratory diseases for every 1 °C above the threshold temperature (29–36 °C) (Lin et al. 2009). Jenkins et al. (2012) reported that during the winter months, the severity of symptoms and hospital admissions due to COPD are almost doubled in the northern and southern regions of the world (Jenkins et al. 2012). In the extreme northern and southern parts of the world with more cold weather, the rate of exacerbation of COPD symptoms in the cold conditions of the year is higher than the warm months. However, no significant differences in COPD rates in different seasons were observed in tropical areas. Therefore, the climatic condition of an area seems to be influential in this regard (Jenkins et al. 2012). The study by Hansel (2016) also showed that COPD patients are more vulnerable, if cold weather persists for a week or more. Therefore, people with COPD should take necessary steps to minimize the effects of cold and reduce the risk of exacerbation. Extreme heat may also be associated with increased respiratory complications in COPD patients, because high temperatures can modify the effects of air pollution (Hansel 2016).
Our results showed that cold stress significantly reduced the risk of hospital admissions due to total respiratory diseases, bronchiectasis, and COPD in Ahvaz. In contrary to the present study, the results of a study by Chen et al. (2019) showed that cold weather generally increased respiratory hospital admissions, especially in the elderly over 75 years of age (Chen et al. 2019). And Tseng et al. showed in Taiwan that with a decrease of 5 °C at moderate temperatures, the exacerbation of COPD increases, especially in the elderly (Tseng et al. 2013). The reason for the differences between our results and the aforementioned studies is that the cold weather which has been reported to exacerbate diseases and increase hospital admissions is below 0 °C which is rarely experienced in Ahvaz.
However, in the present study, in colder weather, hospital admissions increased for asthma and among women. Likewise, Son et al., in eight major cities in Korea (2003–2008), reported that an absolute decrease in ambient temperature (comparing 2 °C to 15 °C) significantly increased hospital admissions due to respiratory disease, allergies, and asthma especially among women (Son et al. 2014). In Italy, D’Amato et al. reported that weather may directly affect irritability and cause asthma and airway diseases, or indirectly affect the respiratory system by its effect on the level of air allergens, air pollutants, or people’s exposure to viral illnesses (Buckley and Richardson 2012; D’amato et al. 2015b). Researchers think regardless of geographical and climatic conditions decreased temperature is a factor that exacerbates asthma symptoms (D’amato et al. 2015b). Studies have also shown that cold air can provoke obstruction of the respiratory tract and airways, lead to asthma (Giesbrecht 1995), and cause sensitivity to infection, with reduced mucosal discharge (Eccles 2002). Decreased temperature also contributes to lung dysfunction and exacerbation of cold-related illnesses, including chronic obstructive pulmonary diseases (Donaldson et al. 1999).
It seems that the relation between cold weather and increased hospital admissions due to asthma in the city of Ahvaz can be related to the seasonal effects and the density of allergens and pollen in the autumn, and respiratory infections and influenza (especially in recent years) in the winter. In the recent years, there have been several outbreaks of thunderstorm asthma in the autumn in Ahvaz (Idani et al. 2016).
In this present study, heat stress reduced the risk of asthma hospital admissions. However, in the research conducted by Lin et al, in New York City, the number of hospitalizations for asthma and chronic airway obstruction increased in high temperatures (Lin et al. 2009). Michelozzi et al. (2009) found a significant relation for high temperature and admission for respiratory disease especially in the European elderly over 75 years, as well; and, for every 1 °C increase in the apparent maximum temperature above the threshold, respiratory admissions increased by 4.5% and 3.1% in the Mediterranean and northern cities of Europe, respectively (Michelozzi et al. 2009). Different climatic conditions and avoiding staying outdoors in very hot temperatures in Ahvaz may be the main reason for these inconsistent results.
Overall, in the present study, heat stress and cold stress were associated with changes in hospital admissions due to respiratory diseases; and in both situations, hospital admissions in most types of respiratory diseases decreased, except for asthma and female respiratory hospital admissions which increased.
Conclusion
The results of the present study indicate that cold stress significantly decreased overall respiratory hospital admissions in Ahvaz, Iran, which has a warm climate.
References
Abdel-Ghany A, Al-Helal I, Shady M (2013) Human thermal comfort and heat stress in an outdoor urban arid environment: a case study. Adv Meteorol 2013:1–7
Alizadeh-Choobari O, Najafi M (2018) Extreme weather events in Iran under a changing climate. Clim Dyn 50:249–260
Anderson GB, Dominici F, Wang Y, McCormack MC, Bell ML, Peng RD (2013) Heat-related emergency hospitalizations for respiratory diseases in the Medicare population. Am J Respir Crit Care Med 187:1098–1103
Buckley JP, Richardson DB (2012) Seasonal modification of the association between temperature and adult emergency department visits for asthma: a case-crossover study. Environ Health 11:55
Bunker A, Wildenhain J, Vandenbergh A, Henschke N, Rocklöv J, Hajat S, Sauerborn R (2016) Effects of air temperature on climate-sensitive mortality and morbidity outcomes in the elderly; a systematic review and meta-analysis of epidemiological evidence. EBioMedicine 6:258–268
Chen T-H, Du XL, Chan W, Zhang K (2019) Impacts of cold weather on emergency hospital admission in Texas, 2004–2013. Environ Res 169:139–146
D’Amato G et al (2015a) Meteorological conditions, climate change, new emerging factors, and asthma and related allergic disorders. A statement of the World Allergy Organization. World Allergy Organization J 8:1–52
D’amato G et al (2015b) Effects on asthma and respiratory allergy of Climate change and air pollution. Multidiscipl Respir Med 10:1–8
Donaldson G, Seemungal T, Jeffries D, Wedzicha J (1999) Effect of temperature on lung function and symptoms in chronic obstructive pulmonary disease. Eur Respir J 13:844–849
Eccles R (2002) An explanation for the seasonality of acute upper respiratory tract viral infections. Acta Otolaryngol 122:183–191
Epstein Y, Moran DS (2006) Thermal comfort and the heat stress indices. Ind Health 44:388–398
Fröhlich D, Gangwisch M, Matzarakis A (2019) Effect of radiation and wind on thermal comfort in urban environments-application of the RayMan and SkyHelios model. Urban Clim 27:1–7
Gasparrini A, Armstrong B, Kenward MG (2010) Distributed lag non-linear models. Stat Med 29:2224–2234
Gasparrini A, Guo Y, Hashizume M, Lavigne E, Zanobetti A, Schwartz J, Tobias A, Tong S, Rocklöv J, Forsberg B, Leone M, de Sario M, Bell ML, Guo YLL, Wu CF, Kan H, Yi SM, de Sousa Zanotti Stagliorio Coelho M, Saldiva PHN, Honda Y, Kim H, Armstrong B (2015) Mortality risk attributable to high and low ambient temperature: a multicountry observational study. Lancet 386:369–375
Giesbrecht GG (1995) The respiratory system in a cold environment. Aviat Space Environ Med 66:890–902
Guha-Sapir D, Below R, Hoyois P (2016) The CRED/OFDA international disaster database. Nature
Haines A, Ebi K (2019) The imperative for climate action to protect health. N Engl J Med 380:263–273
Hansel NN (2016) McCormack MC, Kim V. The effects of air pollution and temperature on COPD COPD: J Chronic Obstructive Pulmonary Disease 13:372–379
Idani E, Dastoorpoor M, Goudarzi G, Khanjani N (2016) Severe outbreaks of respiratory syndromes following autumn rainfall in Khuzestan. Iran. Archives of Iranian Medicine 19:884–885
Jenkins C et al (2012) Seasonality and determinants of moderate and severe COPD exacerbations in the TORCH study. Eur Respir J 39:38–45
Lai PC et al (2018) Constructing a map of physiological equivalent temperature by spatial analysis techniques. In: Comprehensive geographic information systems. Elsevier, pp 389–401
Lee H, Mayer H (2016) Validation of the mean radiant temperature simulated by the RayMan software in urban environments. Int J Biometeorol 60:1775–1785
Leon LR, Helwig BG (2010) Heat stroke: role of the systemic inflammatory response. J Appl Physiol 109:1980–1988
Lin S, Luo M, Walker RJ, Liu X, Hwang S-A, Chinery R (2009) Extreme high temperatures and hospital admissions for respiratory and cardiovascular diseases. Epidemiology 20:738–746
Lin Y-K, Chang C-K, Li M-H, Wu Y-C, Wang Y-C (2012) High-temperature indices associated with mortality and outpatient visits: characterizing the association with elevated temperature. Sci Total Environ 427:41–49
Luo Y, Zhang Y, Liu T, Rutherford S, Xu Y, Xu X, Wu W, Xiao J, Zeng W, Chu C, Ma W (2013) Lagged effect of diurnal temperature range on mortality in a subtropical megacity of China. PLoS One 8:e55280
Malik A, Johnson A, Tahamont M, van der Zee H, Blumenstock F (1983) Role of blood components in mediating lung vascular injury after pulmonary vascular thrombosis. Chest 83:21S–24S
Mannino DM (2011) The natural history of chronic obstructive pulmonary disease. Advances in Respir Med 79:139–143
Michelozzi P, Accetta G, de Sario M, D'Ippoliti D, Marino C, Baccini M, Biggeri A, Anderson HR, Katsouyanni K, Ballester F, Bisanti L, Cadum E, Forsberg B, Forastiere F, Goodman PG, Hojs A, Kirchmayer U, Medina S, Paldy A, Schindler C, Sunyer J, Perucci CA, PHEWE Collaborative Group (2009) High temperature and hospitalizations for cardiovascular and respiratory causes in 12 European cities. Am J Respir Crit Care Med 179:383–389
NOAA (2017) Climate at a glance: Global Time Series
Saboohi R, Soltani S, Khodagholi M (2012) Trend analysis of temperature parameters in Iran. Theor Appl Climatol 109:529–547
Sharafkhani R, Khanjani N, Bakhtiari B, Jahani Y, Tabrizi JS (2018) Physiological equivalent temperature index and mortality in Tabriz (the northwest of Iran). J Therm Biol 71:195–201
Sharafkhani R, Khanjani N, Bakhtiari B, Jahani Y, Tabrizi JS, Tabrizi FM (2019) Diurnal temperature range and mortality in Tabriz (the northwest of Iran). Urban Clim 27:204–211
Son J-Y, Bell ML, Lee J-T (2014) The impact of heat, cold, and heat waves on hospital admissions in eight cities in Korea. Int J Biometeorol 58:1893–1903
Statistical-Centre-of-Iran (2016) Data on the 2016 census. Available at: https://wwwamarorgir
Sun S, Cao W, Mason TG, Ran J, Qiu H, Li J, Yang Y, Lin H, Tian L (2019) Increased susceptibility to heat for respiratory hospitalizations in Hong Kong. Sci Total Environ 666:197–204
Tseng C-M, Chen YT, Ou SM, Hsiao YH, Li SY, Wang SJ, Yang AC, Chen TJ, Perng DW (2013) The effect of cold temperature on increased exacerbation of chronic obstructive pulmonary disease: a nationwide study. PLoS One 8:e57066
White MD (2006) Components and mechanisms of thermal hyperpnea. J Appl Physiol 101:655–663
Zhang Y, Zhao Q, Zhang W, Li S, Chen G, Han Z, Guo Y (2017) Are hospital emergency department visits due to dog bites associated with ambient temperature? A time-series study in Beijing, China. Sci Total Environ 598:71–76
Zhang A, Hu W, Li J, Wei R, Lin J, Ma W (2019) Impact of heatwaves on daily outpatient visits of respiratory disease: a time-stratified case-crossover study. Environ Res 169:196–205
Zhao Q, Zhao Y, Li S, Zhang Y, Wang Q, Zhang H, Qiao H, Li W, Huxley R, Williams G, Zhang Y, Guo Y (2018) Impact of ambient temperature on clinical visits for cardio-respiratory diseases in rural villages in northwest China. Sci Total Environ 612:379–385
Acknowledgements
The authors wish to express their gratitude to Ms. Yalda Sabaghan for her kind assistance.
Availability of data and materials
Not applicable
Funding
This study was funded and supported by Ahvaz Jundishapur University of Medical Sciences (Grant No. APRD-9913).
Author information
Authors and Affiliations
Contributions
SHB and MD designed the project. MD acquired the data. MD analyzed and interpreted the data. NK1 and NK2 wrote the paper. All authors approved the final text.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The proposal of this study was approved by the Ethics Committee of Ahvaz Jundishapur University of Medical Sciences (IR.AJUMS.REC.1399.866).
Consent for publication
Not applicable
Competing interests
The authors declare no competing interests.
Additional information
Responsible Editor: Lotfi Aleya
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Borsi, S.H., Khodadadi, N., Khanjani, N. et al. Physiological equivalent temperature (PET) index and respiratory hospital admissions in Ahvaz, southwest of Iran. Environ Sci Pollut Res 28, 51888–51896 (2021). https://doi.org/10.1007/s11356-021-14345-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11356-021-14345-z