Abstract
Background
Reports of sex differences in self-reported mood, sleep quality, daytime function, and excessive daytime sleepiness in people with obstructive sleep apnea (OSA) have been inconsistent. The purpose of this study was to investigate sex differences in these subjective sleep outcomes in participants with type 2 diabetes (T2D) either at high risk for OSA or diagnosed with OSA.
Methods
Measures included OSA severity by apnea-hypopnea index (AHI) and self-reported questionnaires: Pittsburgh sleep quality index (PSQI), Epworth sleepiness scale (ESS), functional outcomes of sleep quality questionnaire (FOSQ), and the profile of mood states (POMS). Relevant individual, social, and health determinants were included as covariates.
Results
A total of 350 participants with T2D [Mean A1C 8.0% (SD ±1.8)] had mean age 56.5 (SD ±10.5) and were balanced by sex (51% men) and race (60% white, 40% non-white). Reports of sleep quality and daytime function were worse in women than in men (p <0.05), whereas men had more severe OSA than women (p <0.05). In fully adjusted models, there was no moderation by sex in the relations between AHI and the sleep outcome measures. AHI showed a significant association with ESS but not PSQI, FOSQ, or POMS.
Conclusion
In participants with T2D at high risk for or diagnosed with OSA, excessive daytime sleepiness was independently associated with OSA severity, but not self-reported sleep quality, daytime function, or mood. While women reported worse outcomes associated with sleep, these outcomes were not associated with OSA severity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obstructive sleep apnea (OSA) is when a person holds their breath (apneas) resulting in reduced airflow and oxygen desaturation (hypopnea) while sleeping. OSA has traditionally been considered a disease that is found primarily found in men; it is now understood that by the time of menopause, the rates of OSA in women approach those of men [1]. It is possible that in the USA, up to 90% of women may not know they have this condition [2]. Retrospective studies summarized by the Society for Women’s Health Research have suggested that women might not perceive or experience the same rates of symptoms commonly presented in men such as excessive daytime sleepiness, waking up gasping for air at night, and snoring. They suggest that women who have OSA be may prone to report different symptoms such as depressed mood, insomnia, daytime fatigue, and poor sleep quality than men [2]. It remains unclear if women experience different symptoms of OSA or if they report different symptoms because they simply do not recognize or prioritize them.
There is ample evidence that differences between men and women in the pathophysiology of OSA support the claim that women experience symptoms that are different than men. Women with OSA have greater rates of obesity at each level of OSA severity than men; prior to menopause, they are less susceptible to upper airway collapse and have more upper airway resistance than men during sleep [1, 3, 4]. It has been suggested that upper airway resistance in women may affect reports of increased daytime fatigue and depression [5]. However, there are few established biological mechanisms in women that explain their different symptom reports from men. Moreover, people with type 2 diabetes (T2D) are at increased risk for OSA, and their difficulties with disease self-management can severely impact daytime function, sleepiness, and mood. As depression, insomnia, sleep quality, fatigue, and sleepiness are subjective measures frequently associated with individual characteristics (e.g., sex, age, health status) and social determinants (e.g., environment, socioeconomic status), they should be fully considered in analyses examining the outcomes of impaired sleep in all populations. The purpose of this study, in participants with T2D and either OSA or at high risk for OSA, was to examine the effect of sex differences, including possible moderation of any effect found, on the relationship of OSA severity to sleep quality, daytime sleepiness, daytime function, and mood in activities sensitive to impaired sleep.
Methods
Design
A cross-sectional secondary analysis was conducted using data from the baseline assessments of Diabetes Sleep Treatment Trial (DSTT; R01-DK096028). The multisite parent study examined the effect of treating OSA using continuous positive airway pressure (CPAP) and sham-CPAP to compare effects on glycemic control and disease self-management in persons with T2D. A full description of the study is available [6].
Sample
The sample was recruited from a research registry, primary care, diabetes, and sleep clinics and from advertisements in the community, social media platforms, and the electronic health record. Potential participants with symptoms of OSA (e.g., “snoring or breath holding” or “poor sleep quality”) underwent telephone screening to determine their eligibility for the baseline assessment which included home testing for OSA. Full consent was acquired prior to any research activity with the participant. Eligibility criteria was determined from a screening phone call prior to the baseline assessment and included age 18 years or older, self-reported diagnosis of T2D, no recent hospitalizations, able to read and write English, CPAP naïve, and being ambulatory. Exclusionary criteria included a near miss or automobile accident because of sleepiness, work in an occupation where sleepiness is a safety hazard, or refusal to be randomized to sham-CPAP.
Measures
Dependent variables
Pittsburgh sleep quality index
The PSQI subjectively identifies people who sleep well from those who have impaired sleep. It consists of seven components (sleep efficiency, duration, latency, sleep disturbances, perceived sleep quality, medication use for sleep, and daytime dysfunction). Scores > 5 indicate worse sleep quality [7]. The PSQI is reliable (Cronbach’s α = 0.83) and has good validity (sensitivity 89.6% and specificity 86.5%). In a sample of Black and White older women, it has been found to be reliable and valid [8]. A factor analysis by sex indicated that men and women may perceive sleep quality differently; men may associate it more with sleep duration and efficiency, women with sleep disturbance, and daytime dysfunction [9].
Epworth sleepiness scale
The ESS is a commonly utilized measure of subjective daytime sleepiness in eight ordinary situations. Possible scores are from 0 to 24; a score ≥ 10 indicates excessive daytime sleepiness. It is reliable (Cronbach’s α = 0.88) [10]. Two studies have previously suggested that the ESS is a more reliable measure in men than women [11, 12].
Functional outcomes of sleep quality
The FOSQ is used to assess daytime function in those who report excessive daytime sleepiness [13]. Thirty questions are grouped into five subscales (i.e., general productivity, activity level, vigilance, social outcomes, and intimate relationships and sexual activity). Responses on the FOSQ range from 1, “extreme difficulty” due to sleepiness, to 4, “no difficulty”; the participant can also choose “don’t do activity for other reasons.” Total scores on the FOSQ range from 5 to 20 with lower scores indicating more difficulty in completing activities because of daytime sleepiness. The FOSQ is reliable (Cronbach’s α for the total score = 0.95) and is sensitive to identifying those without sleep impairment (total FOSQ ≥ 18) from those with sleep impairment (p < 0.001). The original long-form instrument was validated in a sample that was two-thirds men [13]. Sex differences in psychometric properties have not been evaluated.
Profile of mood states
The POMS measured mood state of the participants. It consists of 65 adjectives (e.g., tense, listless, discouraged) used to assess feelings during the past week with a 5-point Likert scale from 0, “not at all,” to 4, “extremely”[14]. Six components of mood are found in the POMS (i.e., depression-dejection, fatigue-inertia, anger-hostility, tension-anxiety, vigor-activity, and confusion-bewilderment). These components are added to find the summary total mood disturbance (TMD) score (vigor-activity is reversed) [15]. The POMS is able to detect impaired mood in sleep studies. All six POMS components are internally consistent with the TMD score (Cronbach’s α = 0.84). While the norming analysis for “gender” in the instrument developer’s original samples had small but significant differences, the developers said they were not significant enough to support separate standards for women and men. Several studies have used the POMS to assess mood in people with diabetes to good success [16,17,18]. Total adult normative scores are men,14.8 and Women,20.3; higher scores indicate worse mood.
Independent variables
ApneaLink Pro®
OSA severity, operationalized as the apnea/hypopnea Index (AHI), was tested with the ApneaLink Pro®, an FDA approved level III portable device used in the participant’s home. Participants were instructed to take the test the night immediately after their baseline assessment. The ApneaLink Pro® scores the recordings according to the American Association of Sleep Medicine scoring guidelines. They were then corroborated by a registered polysomnography technician. Apneas and hypopneas were scored according to the AASM guidelines [19] for hypopneas of a 4% or greater desaturation and a reduction in respiration of one-third or greater. AHI was determined by dividing the total number of apneas and hypopneas by the total time of evaluated nasal airflow.
Demographic questionnaire
Sex, age, marital or partner status, education attainment, and race were self-reported in this questionnaire.
Financial difficulty
Perceived financial difficulty was measured through the use of one question: “how difficult is it for you to meet your basic needs (i.e., food, housing, utilities, and healthcare).” The three possible responses were “no difficulty,” “some difficulty,” and “extreme difficulty.” In the present study, responses were dichotomized as “no difficulty” and “some to extreme difficulty.” Previous literature has reported that sleep quality and financial security are often associated [20].
Body mass index (kg/m2)
A Tanita scale calculated the weight and height for body mass index.
Glycemic control
During the clinical evaluation, serum A1C was collected to measure glycemic control. The A1C provides a consistent estimation of glycemic control within the past 2 to 3 months [21].
Statistical analysis
IBM® SPSS® Statistics v24 was used to conduct the analyses [22]. Preliminary analyses included analysis of univariate and bivariate sample distributions for normality. The POMS was completed by the participant during their baseline assessment, while the PSQI, FOSQ, and ESS were sent home and returned to the study office. Questionnaires that were not returned were assessed using an available case approach. They were considered missing at random and therefore not included in the analyses. Men were less likely to return the questionnaires representing 6–8% of the total missing in the sample; women represented 3–4% of the total missing in the sample. Differences in the continuous variables including demographic and clinical characteristics and continuous type study variables (AHI, BMI, A1C, age, sleep quality, daytime sleepiness, daytime function, mood) between males and females were analyzed using Student’s t test. After assessing for outliers, data transformations were considered when a continuous type variable showed a skewed distribution. Chi-square tests of independence are determined if the distributions of categorical demographic variables (educational level, race, marital status, financial ability) were different by sex. Hierarchical multiple linear regression modeling was conducted to explore if sex moderates the relations between AHI and the self-reported sleep outcome measures and mood. We entered covariates in the first block, AHI in the second block, and two-way interaction terms between sex and AHI in the third block. Categorical independent variables were coded as (0, 1) indicator variables with the following reference categories: men, married/partnered, White, ≥ 2 years post-high school education, and “no financial difficulty.” Both covariate-adjusted and unadjusted regression models were fitted, and results were compared. Because the distributions of demographic variables of age, race, marital status, and financial difficulty varied between men and women, they were included in the covariate-adjusted models. In addition, we adjusted for A1C and BMI to account for possible effects of T2D. Since we included both participants with OSA as well as those at high risk for OSA, AHI was not categorized but treated as a continuous-type predictor variable. Using AHI as a continuous variable also increased statistical power to identify relationships between AHI and the outcome variables. Statistical significance was established as p < .05.
Results
Sample
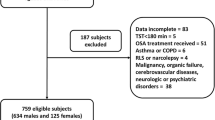
The descriptive demographic and clinical characteristics for the complete sample and by sex are reported in Table 1. In general, the sample (N = 350) was balanced by sex, middle aged, and racially diverse. Most of the participants fell into the overweight or obese (90% with BMI ≥ 25) categories and had poor glucose control. The majority of participants were within the American Academy of Sleep Medicine [19] guidelines for an OSA diagnosis after home sleep testing (AHI > 5, n = 249, range 0–95, IQR 4–19) indicating a high burden of OSA in this sample. Men were statistically significantly older, with a higher AHI, and were more often married or in a committed partnership than women, whereas women reported statistically significantly worse sleep quality, daytime function, and financial ability than men. Measures of excessive daytime sleepiness, overall mood, education, BMI, or A1C levels were not significantly different by sex.
Regression
The results of simple and multiple linear regression analyses of OSA severity based on AHI on the selected sleep outcomes variables are presented in Tables 2 and 3, respectively. In unadjusted models, lower AHI was significantly correlated with worse sleep quality, but was not significantly correlated with daytime function, mood, or excessive daytime sleepiness. Of the covariates, women were significantly associated with worse sleep quality and daytime function. Additionally, worse perceived financial ability and younger age were significantly associated with worse sleep quality, daytime function, and mood. Being younger in the sample was significantly associated with increased rates of daytime sleepiness.
In the models adjusted for sex, financial ability, BMI, A1C, marital status, age, and race, AHI had a significant independent association with excessive daytime sleepiness but not with the other outcome variables including sleep quality. In the fully adjusted models, younger age, being White, and having a stronger perceived financial ability had significant associations with worse mood, while younger-aged participants and those with worse perceived financial ability continued to have the strongest associations with poorer sleep quality and daytime function. There was no significant moderation by sex in any of the models.
Because perceived financial ability accounted for the greatest variance in the models, we assessed for significant correlations with the other covariates and AHI. Better perceived financial ability was significantly correlated with being older (r = 0.214 p < .01), with higher education (r = 0.220, p < 0.01), being White (r = 0.200, p < 0.01), male (r = 0.180, p < 0.01), married/partnered (r = 0.194, p = < 0.01), and with a higher AHI (r = 0.234, p < 0.01); perceived financial ability was not significantly correlated with BMI or A1C (p > 0.05).
Discussion
The aims of this study were to investigate sex differences and potential moderation by sex of the relations between OSA severity and symptoms commonly associated with impaired sleep that of overall sleep quality, daytime sleepiness, and function and mood in persons at increased risk for OSA (i.e., having T2D and reporting trouble sleeping). While many of the demographic and health-related measures demonstrated significant sex differences, sex did not moderate the relations between OSA severity and sleep quality, daytime sleepiness, daytime function, or mood. Additionally, there were no significant associations between OSA severity and the self-reported daytime function and mood. Having lower AHI values was associated with worse sleep quality in the unadjusted model, but not in the adjusted model. OSA severity independently contributed to worse excessive daytime sleepiness.
Perceived sleep quality
While it seems to make intuitive sense that those with more severe OSA would report worse sleep quality, our results do not support this in the adjusted models. Instead, we found that younger age and perceived inability to meet financial needs both had stronger associations with poor reported sleep quality than OSA severity. Other researchers have reported similar findings. Kang et al. suggested that subjective sleep quality had a stronger association with quality of life measures than OSA severity [23]. In a study testing alternative screening measures for OSA, reports of poor sleep quality did not predict OSA severity [24]. A possible reason is that being excessively sleepy (for those without insomnia) makes it easier to fall back to sleep during nighttime awakenings, thus minimizing the perception of poor sleep quality.
Excessive daytime sleepiness
Higher AHI values were associated with increased daytime sleepiness and are not a surprising finding as excessive daytime sleepiness is common in people with OSA [25]. However, sex did not moderate these associations. Because men had more severe OSA than women; it might be predicted that men would have also reported more daytime sleepiness; nevertheless, sex differences in ESS did not reach significance. The literature is inconsistent regarding sex differences in excessive daytime sleepiness in OSA, as some studies have found no differences [26, 27], while other studies have found either women or men with OSA to experience worse rates of daytime sleepiness [27,28,29,30]. Additionally, previous research has suggested that women are symptomatic for OSA at lower mean AHI [5]. Considering that both men and women reported similar rates of daytime sleepiness in our sample, it may be that women report similar symptoms to men but at lower values of AHI.
Functional outcomes
This measure reports functional outcomes that result from excessive daytime sleepiness. While women did not report worse daytime sleepiness than men, in the unadjusted analyses, they did report worse daytime function that resulted from being sleepy. However, in the adjusted model, sex no longer had significant associations with daytime function, and it did not moderate these relations. While previous research on participants with T2D have reported that women who experienced greater daytime sleepiness also experienced worse daytime productivity [31], in this study, financial difficulty and younger age had the largest associations with impaired daytime function.
Mood
There were no differences between men and women in mood and no significant associations between OSA severity and mood in either the complete sample or moderation by sex. Studies that have examined the relationship between OSA and depressive symptomology found 5 to 63% in the rates of depression in people with OSA [32]. The studies comprising this review were heterogeneous in that they were not powered to examine sex differences, or they were not assessed, and they used several different measures of depressive symptoms, including measures that incorporated sleep disturbance as a symptom of depression. When questionnaires that measure depression symptomology contain questions that incorporate symptoms that overlap with a chronic disease such as OSA, they are more likely to find an association between depression and OSA [33]. Consequently, it is likely that since the POMS does not include questions about symptoms that overlap with those of OSA, we did not find any association of OSA severity and mood.
Previous research has suggested that women with OSA experience more depressive symptoms and poorer mood than men with OSA, but these suppositions may have been confounded by women’s greater propensity to depression than men in the general population [1, 27,28,29]. We did find associations for White race and better perceived financial ability with worse mood in the adjusted models. These findings are not uncommon in the health disparities literature for despite the economic disadvantages and discrimination that African Americans face, depressive symptoms are disproportionately higher in Whites [34]. It is also more common to find depression in those in higher income brackets than in those at lower income brackets [34]. Our sample reflects these findings and suggests that social determinants and not OSA severity have a stronger association with mood in this sample.
Individual and social determinants
Economic stability is one of the primary social determinants of health according to Healthy People 2020 [35]. Our findings suggest that perceived financial difficulty was the most significant predictor of worse sleep quality and daytime function as a result of sleepiness and may be related to race as the women in our sample were majority African American. In Pittsburgh, PA, one-third of the African American population lives in poverty [36]. The women were also significantly younger than the men. Therefore, older age may protect sleep quality and daytime function in that it was significantly associated with men, White race, and having a higher perceived financial ability. These findings are supported by previous studies that have ascertained that social determinants such as economic stability partially explain symptoms of impaired sleep in midlife women [37, 38]. In a Canadian population of healthy adults, subjective lower socioeconomic position was found to have a greater effect on reports of daytime sleepiness, sleep duration, and weekend oversleep suggesting that perceptions of financial ability may be an underappreciated factor in poor overall sleep quality [20].
Limitations
While the sample was sizeable and well distributed by race and sex, recruitment was not meant to evaluate the aims in this study; therefore, no power analysis was conducted. Insomnia, which is more common in women than in men, was not included in the models because questions that measure insomnia overlap with the PSQI, ESS, and FOSQ. Insomnia may be a symptom of OSA in some participants and may have impacted reports of impaired sleep [39]. If all of the questionnaires had been returned, results may have been different. Additionally, as men were less likely to return the questionnaires than women, they may have been underrepresented in the sample. Finally, OSA severity (AHI) was not tested in a sleep lab; instead, it was tested using a portable home sleep study which does not distinguish sleep from wakefulness and thus may have underestimated OSA severity.
Conclusion
OSA severity was not significantly associated with the adverse subjective symptoms of impaired mood, sleep quality, and daytime function that frequently accompany OSA. These relations were also not affected by the sex differences in demographic, social, and subjective sleep outcomes measures. Financial difficulties and younger age were more strongly associated with reports of sleep quality, daytime function, and mood than the participant’s sex or OSA severity. While this analysis did not find sex moderated on the effect of OSA on selected outcome variables, it underscores the importance of studies designed with an adequate sample size and distribution to examine sex differences and the social determinants that affect both men and women differently.
References
Ye L, Pien GW, Ratcliffe SJ, Weaver TE (2009) Gender differences in obstructive sleep apnea and treatment response to continuous positive airway pressure. J Clin Sleep Med 5(6):512–518
Miller AM, Redline S, Professor M, et al (2017) Women & Sleep: A Guide for Better Health. www.swhr.org
Lin CM, Davidson TM, Ancoli-Israel S (2008) Gender differences in obstructive sleep apnea and treatment implications. Sleep Med Rev 12(6):481–496. https://doi.org/10.1016/j.smrv.2007.11.003
Mallampalli MP, Carter CL (2014) Exploring sex and gender differences in sleep health: a society for women’s health research report. J Womens Health 23(7):553–562. https://doi.org/10.1089/jwh.2014.4816
Wimms A, Woehrle H, Ketheeswaran S, Ramanan D, Armitstead J (2016) Obstructive sleep apnea in women: specific issues and interventions. Biomed Res Int 2016:1764837. https://doi.org/10.1155/2016/1764837
Chasens ER, Atwood CW, Burke LE, Korytkowski M, Stansbury R, Strollo PJ, Sereika SM (2019) Diabetes sleep treatment trial: premise, design, and methodology. Contemp Clin Trials 76:104–111. https://doi.org/10.1016/j.cct.2018.11.014
Buysse DJ, Reynolds CF, Monk TH et al (1989) The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res 28(2):193–213. https://doi.org/10.1016/0165-1781(89)90047-4
Beaudreau SA, Spira AP, Stewart A, Kezirian EJ, Lui LY, Ensrud K, Redline S, Ancoli-Israel S, Stone KL, Study of Osteoporotic Fractures (2012) Validation of the Pittsburgh sleep quality index and the Epworth sleepiness scale in older black and white women. Sleep Med 13(1):36–42. https://doi.org/10.1016/j.sleep.2011.04.005
Morris JL, Rohay J, Chasens ER (2017). Sex Differences in the Psychometric Properties of the Pittsburgh Sleep Quality Index. J Women’s Health. 00(00):jwh.2017.6447. https://doi.org/10.1089/jwh.2017.6447
Johns MW (1991) A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep 14(6):540–545
Chervin RD, Aldrich MS (1999) The Epworth sleepiness scale may not reflect objective measures of sleepiness or sleep apnea. Neurology 52(1):125–131 http://www.ncbi.nlm.nih.gov/pubmed/9921859. Accessed 17 Dec 2015
Zou J, Guan J, Yi H, Meng L, Xiong Y, Tang X, Su K, Yin S (2013) An effective model for screening obstructive sleep apnea: a large-scale diagnostic study. PLoS One 8(12):e80704. https://doi.org/10.1371/journal.pone.0080704
Weaver TE, Laizner AM, Evans LK, Maislin G, Chugh DK, Lyon K, Smith PL, Schwartz AR, Redline S, Pack AI, Dinges DF (1997) An instrument to measure functional status outcomes for disorders of excessive sleepiness. Sleep 20(10):835–843
McNair DM, Heuchert JW (2008) Profile of Mood States Technical Update
McNair D Lorr M, Druppleman L (1971) EITS Manual for Profile of Mood States
Baptista LC, Machado-Rodrigues AM, Martins RA (2017) Exercise but not metformin improves health-related quality of life and mood states in older adults with type 2 diabetes. Eur J Sport Sci 17(6):794–804. https://doi.org/10.1080/17461391.2017.1310933
Brinkworth GD, Luscombe-Marsh ND, Thompson CH, Noakes M, Buckley JD, Wittert G, Wilson CJ (2016) Long-term effects of very low-carbohydrate and high-carbohydrate weight-loss diets on psychological health in obese adults with type 2 diabetes: randomized controlled trial. J Intern Med 280(4):388–397. https://doi.org/10.1111/joim.12501
Van Der Does FEE, Nic J, Ling N, et al. (1996) Symptoms and well-being in relation to glycemic control in type II diabetes
Kapur VK, Auckley DH, Chowdhuri S, Kuhlmann DC, Mehra R, Ramar K, Harrod CG (2017) Clinical practice guideline for diagnostic testing for adult obstructive sleep apnea: an American Academy of sleep medicine clinical practice guideline. J Clin Sleep Med 13(03):479–504. https://doi.org/10.5664/jcsm.6506
Jarrin DC, McGrath JJ, Silverstein JE, Drake C (2013) Objective and subjective socioeconomic gradients exist for sleep quality, sleep latency, sleep duration, weekend oversleep, and daytime sleepiness in adults. Behav Sleep Med 11(2):144–158. https://doi.org/10.1080/15402002.2011.636112
American Diabetes Association (2014) Glycemic Targets. Diabetes Care 38(Supplement 1). http://care.diabetesjournals.org/content/38/Supplement_1/S33. Accessed 14 Jul 2017
IBM Corp. IBM SPSS Statistics for Windows. Version 25
Kang JM, Kang S-G, Cho S-J, Lee YJ, Lee HJ, Kim JE, Shin SH, Park KH, Kim ST (2017) The quality of life of suspected obstructive sleep apnea patients is related to their subjective sleep quality rather than the apnea-hypopnea index. Sleep Breath 21(2):369–375. https://doi.org/10.1007/s11325-016-1427-8
Scarlata S, Pedone C, Curcio G, Cortese L, Chiurco D, Fontana D, Calabrese M, Fusiello R, Abbruzzese G, Santangelo S, Zito A, Incalzi RA (2013) Pre-polysomnographic assessment using the Pittsburgh sleep quality index questionnaire is not useful in identifying people at higher risk for obstructive sleep apnea. J Med Screen 20(4):220–226. https://doi.org/10.1177/0969141313511591
Greenberg H, Lakticova V, Scharf SM. Obstructive sleep apnea. In: Principles and Practice of Sleep Medicine. Elsevier; 2017:1110–1124.e6
Lee M, Lee S-A, Lee G, Ryu HS, Chung S, Chung YS, Kim WS (2014) Gender differences in the effect of comorbid insomnia symptom on depression, anxiety, fatigue, and daytime sleepiness in patients with obstructive sleep apnea. Sleep Breath 18(1):111–117. https://doi.org/10.1007/s11325-013-0856-x
Ye L, Pien GW, Weaver TE (2009) Gender differences in the clinical manifestation of obstructive sleep apnea. Sleep Med 10(10):1075–1084. https://doi.org/10.1016/j.sleep.2009.02.006
Wahner-Roedler DL, Olson EJ, Narayanan S, Sood R, Hanson AC, Loehrer LL, Sood A (2007) Gender-specific differences in a patient population with obstructive sleep apnea-hypopnea syndrome. Gend Med 4(4):329–338
Shepertycky MR, Banno K, Kryger MH (2005) Differences between men and women in the clinical presentation of patients diagnosed with obstructive sleep apnea syndrome. Sleep. 28(3):309–314
McCall WV, Harding D, O’Donovan C (2006) Correlates of depressive symptoms in patients with obstructive sleep apnea. J Clin Sleep Med 2(4):424–426
Chasens ER, Morris JLJL, Strollo PJPJ, Sereika SMSM, Burke LELE, Korytkowski M (2015) Gender differences in the response to impaired sleep in adults with diabetes. Behav Sleep Med 14(4):1–10. https://doi.org/10.1080/15402002.2015.1017100
Ejaz SM, Khawaja IS, Bhatia S, Hurwitz TD (2011) Obstructive sleep apnea and depression: a review. Innov Clin Neurosci 8(8):17–25
Nanthakumar S, Bucks RS, Skinner TC (2016) Are we overestimating the prevalence of depression in chronic illness using questionnaires? Meta-analytic evidence in obstructive sleep apnoea. Health Psychol 35(5):423–432. https://doi.org/10.1037/hea0000280
Budhwani H, Hearld KR, Chavez-Yenter D (2015) Depression in racial and ethnic minorities: the impact of nativity and discrimination. J Racial Ethn Health Disparities 2(1):34–42. https://doi.org/10.1007/s40615-014-0045-z Accessed 24 Jun 2019
Office of Disease Prevention and Health Promotion. Social Determinants of Health | Healthy People 2020. Healthy People 2020 Top Object. 2015:5–8. https://www.healthypeople.gov/2020/topics-objectives/topic/social-determinants-of-health. Accessed 24 Jun 2019
(2018) Pittsburgh equity indicators a baseline measurement for enhancing equity in Pittsburgh. http://pittsburghpa.gov/equityindicators/documents/PGH_Equity_Indicators_2018.pdf. Accessed 24 Jun 2019
Hall MH, Casement MD, Troxel WM et al Chronic stress is prospectively associated with sleep in midlife women: the SWAN sleep study. Sleep. https://doi.org/10.5665/sleep.5066 Accessed 27 Jun 2015
Im E-O, Ko Y, Chee E, Chee W (2015) Cluster analysis of midlife women’s sleep-related symptoms: racial/ethnic differences. Menopause. 22(11):1182–1189. https://doi.org/10.1097/GME.0000000000000460
Luyster FS, Buysse DJ, Strollo PJ Jr (2010) Comorbid insomnia and obstructive sleep apnea: challenges for clinical practice and research. J Clin Sleep Med 6(2):196–204
Funding
This study was supported by NIH F31-NR017336–01(PI: Morris); Margaret E. Wilkes Scholarship Fund Award, University of Pittsburgh School of Nursing; T32-HL-007779 (PI: D. Buysse); the National Institute of Diabetes and Digestive and Kidney Diseases (R01DK096028); and the Clinical +Translational Research Institute grants UL1TR001857 and UL1TR000005.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Jonna L. Morris and Susan M. Sereika declare that they have no conflict of interest. Eileen R. Chasens has received equipment (ApneaLink) from Resmed and Respironics (CPAP machines).
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Morris, J.L., Sereika, S.M. & Chasens, E.R. Sex differences in subjectively reported symptoms of obstructive sleep apnea in community-dwelling adults with type 2 diabetes. Sleep Breath 25, 181–188 (2021). https://doi.org/10.1007/s11325-020-02074-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-020-02074-5