Abstract
Purpose
The collapsibility of the upper airway is a key factor in the pathogenesis of obstructive sleep apnea (OSA). The exact measurement of this parameter, typically performed by obtaining the critical pressure (Pcrit), has not been introduced into clinical practice. The techniques that are used to measure the upper airway resistance could provide information on its the collapsibility of the airway. The aim of this study was to associate resistance in the upper airway with the presence of OSA.
Methods
Using a cross-sectional design with a control group, consecutive cases that were seen in the Chest Diseases Sleep Unit were recruited after undergoing nocturnal polysomnography. The upper airway collapsibility was determined based on the change in its resistance from the standing position to the supine position with a flow interruption (Rint) device by measuring the angle formed between the pressure/flow lines (PF angle) between the two positions.
Results
The PF angle was greater in the OSA group than in the controls: 7.5° (4) vs. 4° (2) (P < .001), with a positive correlation between the width of the angle and the apnea-hypopnea index (AHI) (r: 0.28, P = .03). Placing the threshold level at 10°, a sensitivity of 25% was obtained, along with a specificity of 96%, for the diagnosis of OSA.
Conclusion
The measurement of resistance in the upper airway using flow interruption (Rint) can predict the presence of moderate and severe OSA with high specificity but low sensitivity.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Obstructive sleep apnea (OSA) consists of the total or partial obstruction of the upper airway during sleep. It is a public health problem with a high prevalence that often affects young people and is associated with cardiovascular morbidity and mortality, work or traffic accidents, and poor quality of life [1,2,3,4].
In the last 20 years, there has been an increase in the demand for consultations and diagnostic studies for this disorder, which often leads to delays in the diagnosis and the start of treatment. For this reason, it would be useful to have screening tools that could help to optimize this process, shortening the time for starting the treatment in the most severe patients [5]. Various questionnaires have been developed with the intention of identifying patients with OSA (Berlin, STOP, STOP-BANG, Epworth), and although some have been shown to be highly sensitive, their specificity is generally low [6].
In the pathogenesis of OSA, a key factor is the collapsibility of the upper airway since its presence is a determining factor in the appearance of obstructive apnea. The exact measurement of this parameter is achieved by measuring the pressure at which the passive collapse of the upper airway takes place, known as the critical pressure (Pcrit) [7]. This measurement should be made during nocturnal polysomnography and is currently not implemented in usual clinical practice. However, the diagnosis of an unstable upper airway with a tendency to collapse would be very useful for prioritizing higher risk patients. The availability of simple alternatives for this study could have a great impact on clinic doctors [8].
In lung function studies, different techniques are used to measure the resistance of the airways, with a portion of this resistance generated in the upper airway. Our hypothesis is that the measurement of the resistance in the upper airway can provide information on the tendency of the upper airway to collapse. Our objective was to associate the resistances measured in the upper airway with the presence of OSA determined by nocturnal polysomnography.
Material and methods
Our hospital has a catchment population of 350,000 patients, and the sleep unit annually performs 600–700 domiciliary respiratory polygraphs and 400–500 nocturnal polysomnographs. Using a cross-sectional and observational design with a control group, those cases that were seen in the Chest Diseases Sleep Unit between March and May 2018 were recruited after undergoing nocturnal polysomnography. Minors less than 18 years were excluded, along with those who would not cooperate adequately in the performing of the technique. Clinical details were obtained from the patients, as well as lung function studies and apnea-hypopnea indexes (AHIs) determined by the nocturnal polysomnography. Polysomnography was performed using a Grael (Compumedics, Australia) apparatus. To determine the sleep structure and obtain the AHI, electroencephalography signals were recorded (F4-M1; C4-M1; O2-M1), with electrooculography (EOG), electromyography (EMG), oximetry, air flow measurements (thermistor and nasal cannula), and chest and abdominal respiratory movements using a chest and abdominal bands, according to the recommendations of the American Sleep Disorders Association (ASDA) of 2012 [9]. Apnea was defined as a drop in the thermistor signal greater than 90% for at least 10 s and hypopnea as a reduction in the cannula signal > 30% for at least 10 s with a drop in the oxygen saturation of at least 3% or with arousal. The AHI was calculated as the total number of respiratory events (apneas and hypopneas) per hour of sleep. Individuals who had an AHI > 10/h were classified as OSA, and those who had an AHI < 11/h made up the control group.
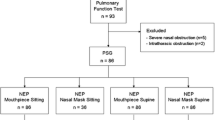
Measurement of upper airway resistance
A flow interruption (Rint) device (Micro 5000, Medisoft-Belgium, an MGCD Group Company) was used to measure airway resistance in the recruited patients (Fig. 1). To carry out the procedure, the patient was asked to breathe a tidal volume through the mouthpiece of the peak-flow meter with the nose occluded until his or her breathing pattern was established (approximately 30 s). Complete multiple occlusions of 100 microseconds were automatically carried out, with between 5 and 10 good quality measurements being obtained (absence of leaks and with an expired volume after occlusion of at least 80% of the previous exhalations). Tests with a variation greater than 14% were discarded [10, 11]. In the first 40 microseconds of each occlusion, a rapid increase in pressure in the mouth is produced with oscillations that reflect the distensibility in the upper airway. The pressure measured at that moment is generated in the upper airway (Pint). Afterwards, there is a second phase without oscillations, where the alveolar pressure is measured [12, 13]. With the determinations made and using the ExpAir Software 1.30.02, the Pint/flow line was calculated, showing the resistance in the upper airway expressed as the ratio between the pressure and the flow measured.
Measurements were made in the standing and supine positions. The collapsibility of the upper airway was estimated based on the changes detected between the resistances measured in the two positions by measuring the width of the angle formed between Pint/flow lines generated by the software of the device (PF angle) with an angle protractor. The width of that angle is the measure of the level of instability or collapsibility in the upper airway (Fig. 2). The value of Pint was determined in the supine position by calculating the mean between the measurements made.
The results are expressed as the means and standard deviations (SDs) for quantitative variables and percentages for qualitative variables. The quantitative variables were analyzed to determine the correlation and comparison of the means (Student’s t). A P value of < .05 was considered significant.
The PF angle was categorized by taking as a threshold the value that provided greater specificity (10°) according to ROC curve analysis to predict the presence of OSA. The ROC curve graphically represents the sensitivity and specificity of a technique in a study according to the variations in the decision threshold. The precision of that threshold is estimated according to the area under the curve (AUC), which varies between 0.5 (low discriminative capacity) and 1 (maximum discriminative capacity). The sensitivity, specificity, positive predictive value (PPV) (true positives/[true positives + false positives]) and negative predictive value (NPV) (true negatives/[true negatives + false negatives]) were calculated using the usual formulas.
The study was approved by the Research Ethics Committee of the Centre (Project No 93/18), and written informed consent was obtained from all participants.
Results
A total of 122 patients (91 cases and 31 controls) were included in the study, of which 51 (48%) cases had severe OSA with an AHI >30/h. The comparison between the anthropometric and functional data of both groups is shown in Table 1. No statistically significant differences were observed in age, BMI, or lung function. The PF angle was significantly wider in the patient group with OSA (7.5° (4)) compared to the control group (4° (2)).
In the correlation study, the value of the PF angle showed a significant relationship with the AHI obtained from polysomnography (r: .28; P = .03). In patients with severe OSA, the PF angle was 9° (SD 3°) compared to 5° (SD 3°) in the moderate OSA group (P = .002). There was a correlation between the Pint value in the supine position and the PF angle (r = 0.42 P = .0001) but not with the AHI.
The ROC curve determined with the PF angle to predict OSA had an AUC of 0.72. Placing the threshold at 10°, a sensitivity of 25% was obtained, with a specificity of 96%, a PPV of 95%, and an NPV of 30% for the diagnosis of OSA (Table 2).
Discussion
The main finding of our study is that an increase in upper airway resistance, obtained by measuring the interrupter resistance (Rint), was found in our patient series compared to that of the control group. These resistances are an expression of the collapsibility of the upper airway, are associated with the severity of the OSA and have a high specificity for its diagnosis.
The calculation of Pcrit is considered the reference method for diagnosing the collapsibility of the upper airway [7]. Here, we studied the variation in the resistance to the air flow expressed as the pressure/flow ratio. An upper airway with a greater resistance to air flow indicates that its collapsibility is greater. As the collapse is a dynamic fact, we carried out two measurements of these resistances, one with the patient standing up and the other with the patient in the supine position. Taking into account that the upper airway is more collapsible in the supine position [14,15,16], the patients who showed a greater change in their resistances, and thus a wider PF angle, would have increased instability in their upper airway.
The increase in Pcrit has been associated with the AHI [8], and it has been demonstrated that patients with OSA have Pcrit values superior to those of the controls and that increase with the severity of the OSA. However, this is not a simple system designed for measurements in clinical practice; rather, it is used mainly for research purposes [17]. This has led to other authors attempting to measure the collapsibility with simpler techniques. Landry et al. [18] demonstrated that in the process of titrating CPAP in patients with OSA, the cases that needed more elevated pressures had higher Pcrit values. Hirata et al. [17] measured collapsibility by applying negative pressure to the upper airway, and Genta et al. [19] analyzed the flow curves during sleep, checking collapsibility using bronchofibroscopy. Studies have also been carried out using imaging techniques that have associated some of the characteristics of the upper airway with the risk of suffering OSA [20, 21]. However, none of these techniques have spread to the clinical management of these patients. The method proposed by us is probably the most straightforward of those mentioned, as it can be performed in awake individuals, takes very little time, and provides immediate results in the same clinic, such that the doctor will be able to estimate the collapsibility in the upper airway with increased specificity and PPV in patients during their first assessment.
The strength of our study is that it provides a tool that can estimate, with a high specificity and PPV, the collapsibility of the upper airway in a simple way, with low use of recourses and within the reach of many sleep units. Not having compared our marker with that of the reference (Pcrit) is the limitation of our study. However, we believe that the theoretical foundations on which the measurement of resistances in the upper airway is based indicate that it measures the same phenomenon as Pcrit. Our study also has limitations due to the methodology since we use diurnal measurements with nasal occlusion to predict the phenomena that may occur during sleep, when the muscle tone and ventilation are different. However, we believe that the results of the specificity and the simplicity of the method counteract these limitations.
The pathogenesis of OSA not only influences the collapsibility of the upper airway but also potentially involves other factors. For this reason, the weakest point in the measurement of the collapsibility of the upper airway appears to be the low sensitivity of the tests; for this reason, in studies that already measure the Pcrit, there is a wide variation in the values obtained, such that while elevated values of Pcrit are the characteristics of OSA, a low value does not exclude its presence [8]. Our results, obtained by measuring the PF angle, have the same profile and show that the width of that angle is related to the AHI and to the severity of the OSA, although there were cases of OSA with acute PF angles. Situated the threshold value of the width of the PF angle at 10°, the specificity of the test was 96%, with a PPV of 95%.
Although we found a significantly higher Pint value in the supine position in patients with OSA than in the controls, it seems that the changes between the standing and supine positions measured with the PF angle have more consistent results and a closer relationship with the AHI than a single measurement of the Pint, since the dynamic aspect of the collapsibility is more obvious in the change in position.
In our series, although there were differences in gender between the cases and the control group, the PF angle in the control group did not show any significant differences between males (3.7° (2.4)) and females (4.3° (3); P = .2). If we compare the data of the PF angle in the whole series, we obtain 6.1° (5) in males and 6.4 ° (6) in females (P = .7), which makes us believe that gender does not have any influence on the PF angle.
Once a diagnosis of OSA is made and to determine the presence of upper airway collapsibility, instability of the respiratory center, muscular changes, or the arousal threshold, the patients could be directed toward different therapeutic options (CPAP or alternative treatments). In this sense, detecting an unstable upper airway could also help to personalize the treatments for patients with OSA [22, 23].
Another aspect to consider is that, in the care of patients suspected of OSA, nocturnal studies of prolonged duration need to be performed, with subsequent interpretation by trained staff. All of this often lengthens the care process and leads to resource management problems. The availability of this technique that provides specific information in a rapid and simple way should enable potentially more severe cases to be given priority. In our series, decisions could have been made in 25% of the cases. Taking into account the elevated specificity that we found, we would be able to standardize this procedure across sleep units, perhaps complemented by other, more sensitive tools [6, 24] to make better use of resources and establish priorities in the diagnosis waiting lists.
Conclusions
The measurement of resistance in the upper airway using flow interruption (Rint) can predict the presence of moderate and severe OSA with high specificity. Its use, probably combined with techniques of greater sensitivity (STOP-BANG or Epworth scale), could help in the management of patients with suspected OSA, particularly in the prioritization of the more severe cases. Our proposal is to design studies that add the measure of PF angle to the initial assessment of these patients.
References
McNicholas WT, Bonsignore MR, the Management Committee of EU COST ACTION B26 (2007) Sleep apnoea as an independent risk factor for cardiovascular disease: current evidence, basic mechanisms and research priorities. Eur Respir J 29:156–178
Garbarino S, Guglielmi O, Sanna A, Mancardi GL, Magnavita N (2016) Risk of occupational accidents in workers with obstructive sleep apnea: systematic review and meta-analysis. Sleep 39(6):1211–1218
Kales SN, Czeisler CA (2016) Obstructive sleep apnea and work accidents: time for action. Sleep 39:1171–1173
Tregear S, Reston J, Schoelles K, Phillips B (2009) Obstructive sleep apnea and risk of motor vehicle crash: systematic review and meta-analysis. J Clin Sleep Med 5:573–581
Mediano O, Barbé-Illa F, Montserrat JM (2017) A network management approach to sleep apnea-hypopnea syndrome: healthcare units. Arch Bronconeumol 53(4):184–185
Nagappa M, Liao P, Wong J, Auckley D, Ramachandran SK, Memtsoudis S et al (2015) Validation of the STOP-Bang questionnaire as a screening tool for obstructive sleep apnea among different populations: A systematic review and meta-analysis. PLoS One 10(12)
Carberry JC, Jordan AS, White DP, Wellman A, Eckert DJ (2016) Upper airway collapsibility(Pcrit) and pharyngeal dilator muscle activity are sleep stage dependent. Sleep 39(3):511–521
Eckert DJ, White DP, Jordan AS, Malhotra A, Wellman A (2013) Defining phenotypic causes of obstructive sleep apnea: identification of novel therapeutic targets. Am J Respir Crit Care Med 188:996–1004
Berry R, Budhiraja R, Gottlieb D, Gozal D, Iber C, Kapur V et al (2012) Rules for scoring respiratory events in sleep: update of the 2007 AASM manual for the scoring of sleep and associated events deliberations of the sleep apnea definitions task force of the American Academy of Sleep Medicine. J Clin Sleep Med 8:N.°5
Force T, Gappa M, Colin AA, Goetz I, Stocks J (2001) SERIES " STANDARDS FOR INFANT RESPIRATORY FUNCTION TESTING : ERS / ATS Passive respiratory mechanics : the occlusion techniques: 141–148
Oswald Mammosser M, Charloux A, Donato L, Albrech C, Speich JP, Lampert E et al (2000) Interrupter technique versus plethysmography for measurement of respiratory resistance in children with asthma or cystic fibrosis. Pediatr Pulmonol 29:213–220
Shephard RJ (1963) Mechanical characteristics of the human airway in relation to use of the interrupter valve. Clin Sci 25:263–280
Beydon N, On behalf of the ATS/ERS Working Group on Infants (2006) Young Children and Pulmonary Function Testing. Interrupter resistance: What’s feasible? Paediatr Respir Rev 7:55–57
Ong JSL, Touyz G, Tanner S, Hillman DR, Eastwood PR, Walsh JH (2011) Variability of human upper airway collapsibility during sleep and the influence of body posture and sleep stage. J Sleep Res 20:533–537
Joosten SA, O’Driscoll DM, Berger PJ, Hamilton GS (2014) Supine position related obstructive sleep apnea in adults: pathogenesis and treatment. Sleep Med Rev 18:7–17
Jan MA, Marshall I, Douglas NJ (1994) Effect of posture on upper airway dimensions in normal human. Am J Respir Crit Care Med 149:145–148
Hirata RP, Schorr F, Kayamori F, Moriya HT, Romano S, Insalaco G et al (2016) Upper airway collapsibility assessed by negative expiratory pressure while awake is associated with upper airway anatomy. J Clin Sleep Med 12:1339–1346
Landry SA, Joosten SA, Eckert DJ, Jordan AS, Sands SA, White DP et al (2017) Therapeutic CPAP level predicts upper airway collapsibility in patients with obstructive sleep apnea. Sleep 40:1–7
Genta PR, Sands SA, Butler JP, Loring SH, Katz ES, Demko BG et al (2017) Airflow shape is associated with the pharyngeal structure causing OSA. Chest 152(3):537–546
Schwab RJ, Pasirstein M, Pierson R, Mackley A, Hachadoorian R, Arens R et al (2003) Identification of upper airway anatomic risk factors for obstructive sleep apnea with volumetric magnetic resonance imaging. Am J Respir Crit Care Med 168:522–530
Chi L, Comyn FL, Mitra N, Reilly MP, Wan F, Maislin G et al (2011) Identification of craniofacial risk factors for obstructive sleep apnea using three-dimensional MRI. Eur Respir J 38:348–358
Eckert DJ (2018) Phenotypic approaches to obstructive sleep apnoea – new pathways for targeted therapy. Sleep Med Rev 37:45–59
Osman AM, Carter SG, Carberry JC, Eckert DJ (2018) Obstructive sleep apnea: current perspectives. Nat Sci Sleep 10:21–34
Gozal D, Jortani S, Snow AB, Kheirandish-Gozal L, Bhattacharjee R, Kim J et al (2009) Two-dimensional differential in-gel electrophoresis proteomic approaches reveal urine candidate biomarkers in pediatric obstructive sleep apnea. Am J Respir Crit Care Med 180:1253–1261
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Julia Herrero, Gemma Rubinos, and Ramón Fernández. The first draft of the manuscript was written by Ramón Fernández, Gemma Rubinos, and Julia Herrero. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interests
Dra. Gemma Rubinos Cuadrado declares that she has no conflict of interest, Dr. Ramón Fernández Álvarez declares that he has no conflict of interest, Dra. Julia Herrero Huertas declares that she has no conflict of interest, Dra. Maria Jose Vazquez Lopez declares that she has no conflict of interest, Dra. Marta Iscar Urrutia declares that she has no conflict of interest, Dr. Pere Casan Clara declares that he has no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The study was approved by the Clinical Research Ethics Committee of our hospital. Informed consent was obtained from all the individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cuadrado, G.R., Álvarez, R.F., Huertas, J.H. et al. Measurement of upper airway resistances: A simple way to assess its collapsibility?. Sleep Breath 24, 1531–1535 (2020). https://doi.org/10.1007/s11325-020-02026-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-020-02026-z