Abstract
Purpose
The purpose of this study was to determine the impact of insomnia in Veterans with post-traumatic stress disorder (PTSD) and obstructive sleep apnea (OSA) on health-related outcomes before and after 12 weeks of continuous positive airway pressure (CPAP) treatment.
Methods
We conducted a prospective cohort study of Veterans with PTSD and documented apnea hypopnea index (AHI) ≥ 5 with and without clinically significant insomnia as determined by the Insomnia Severity Index (ISI). Health-related outcomes including PTSD checklist (PCL-M), SF-36, and Pittsburgh Sleep Quality Index (PSQI) were assessed at baseline and 12 weeks after initiation of OSA treatment. CPAP adherence was retrieved at each visit.
Results
Seventy-two Veterans including 36 with comorbid insomnia and OSA (COMISA) and 36 OSA-only were enrolled. Veterans with COMISA were younger (p = 0.03), had lower BMI (p < 0.001), and were more likely to report depression than those with OSA-only (p = 0.004). Although AHI was higher in the COMISA (p = 0.01), both groups expressed comparable daytime sleepiness (p = 0.16). The COMISA group had no significant change in SF-36 and PSQI after 12 weeks of treatment and used CPAP much less frequently than OSA-only group (p = 0.001).
Conclusions
COMISA in Veterans with PTSD is associated with worse quality of life than those with OSA-only. Insomnia should be assessed in Veterans with PTSD who are not adherent to CPAP treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In the last decade, several studies have documented a broad array of comorbid sleep disorders in subjects with PTSD including insomnia, nightmares, sleep-disordered breathing (SDB), and dream enactment behavior [1, 2]. Sleep impairment accounts for a significant portion of the variance in physical health complaints even after controlling for pain and depression [3]. In studies of active duty service members with PTSD who underwent polysomnography, 56.6 to 67.3% were diagnosed with obstructive sleep apnea (OSA) [4, 5]. This combination of OSA and PTSD results in worsened somnolence, fatigue, poor daytime function, and sleep-related quality of life compared with those with either condition alone and normal subjects [5]. Not infrequently, these same symptoms are experienced by Veterans suffering from insomnia, which makes the diagnosis and management of these cases quite challenging when both OSA and insomnia co-exist. In military personnel with combat exposure, comorbid insomnia and OSA, a condition originally termed “COMISA,” were identified in 38.2% of subjects presenting for initial evaluation of sleep disturbances [6].
The interaction between OSA and insomnia in Veterans with PTSD has not been fully elucidated. The conceptual framework for the link between the two ailments conjectures a reciprocal relationship whereby each disorder amplifies the other. The disordered breathing events often result in transient arousals or complete awakening from sleep leading to difficulties in initiating and maintaining sleep. The somatic arousal experienced from recurrent apneic events may become conditioned to the bedroom producing a heightened state of arousal prior to sleep onset. PTSD acts as a catalyst promulgating maladaptive reinforcement. Due to sleep fragmentation of sleep apnea, interruption of memory consolidation contributes to resurgence of fear and anxiety [7]. As a result, a state of hyperarousal dominates sleep onset leading to chronic insomnia. The latter engenders sleep deprivation which adversely affects the tone of the pharyngeal muscles, particularly the genioglossus muscle, which in turn contributes to worsening of OSA increasing its severity [8].
The extent to which COMISA worsens PTSD or represents a by-product of PTSD remains ambiguous. Contemporary clinical studies of COMISA have provided informative data about incidence and risk factors, although most of those studies have emanated from cross-sectional studies or patients attending medical practices [9,10,11,12,13]. These characteristics varied as a function of the primary condition and were based on self-reported insomnia. More importantly, none of these studies have examined the influence of PTSD on the overall quality of life in the presence of these sleep comorbidities.
In this study, we aimed at exploring the health outcomes of Veterans with PTSD and COMISA before and following 12 weeks of CPAP treatment. We hypothesized that COMISA confers a worse quality of life and lower CPAP adherence in Veterans afflicted with PTSD and COMISA compared to a cohort of OSA-only Veterans.
Methods
Study population
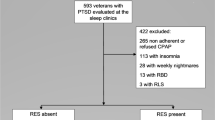
Veterans with history of PTSD who presented to the sleep clinic at the VA Western New York Healthcare System (VAWNYHS) for management of sleep disorders between January 2014 and December 2016 were eligible to participate in the study. Inclusion criteria included the following: (1) diagnosis of PTSD established by a psychiatrist at least 6 months prior to the sleep clinic visit, (2) clinically stable with no change in psychotherapy regimen for at least 4 weeks before enrollment, (3) documented OSA by polysomnography, and (4) ability to provide an informed consent. Patients with mixed or central apnea, acute medical or psychiatric condition, or suicidal ideation were excluded from participation. Similarly, Veterans who were receiving opioids or who had prior CBT treatment for insomnia were not eligible for enrollment. Some of these enrollees were part of a cohort group under study for the association between PTSD and obstructive sleep apnea [14]. The study was approved by the Institutional Review Board of VAWNYHS and all patients provided voluntary informed consent.
Baseline assessment and follow-up visits
After obtaining informed consent, demographic, anthropomorphic, and socioeconomic characteristics were obtained from all participants, including include age, sex, body mass index (BMI), comorbidities, and medication list. Each patient was asked to complete the Epworth Sleepiness Scale (ESS) [15], the Insomnia Severity Index (ISI) [16], the PTSD checklist (PCL-M) [17], the Pittsburgh Sleep Quality Index (PSQI) [18], and the SF36 [19]. Subjects who scored greater than or equal to 15 points on the Insomnia Severity Index were categorized as having COMISA. An OSA-only group of Veterans with PTSD and OSA whose ISI score was < 15 was recruited simultaneously. Within 2 weeks of enrollment, a manual CPAP titration was performed according to standard criteria [20]. During CPAP setting, all participants received counseling on sleep hygiene using published materials to suggest ways to improve the regularity and duration of sleep, aiming for 7–8 h of sleep per night. Verbal and written directions on the use of CPAP were also provided, with instructions reinforced after the initial period of CPAP setup is completed, and then at interim telephone follow-up calls. A repeat assessment was conducted during a face-to-face visit scheduled 12 weeks following CPAP initiation.
Assessment tools
Epworth Sleepiness Scale
The ESS is a self-administered 8-item questionnaire used index to measure subjective sleepiness in OSA. Scores range from 0 to 24, with a cutoff of > 10 representing clinically significant sleepiness [15].
Insomnia Severity Index
The ISI is a 7-item measure of perceived insomnia severity [16]. The ISI assesses sleep difficulties and distress, and impairment related to the sleep disturbance. Total scores range from 0 to 28, with a higher score indicative of greater insomnia severity. The ISI has excellent internal consistency (Cronbach α = 0.74) and temporal stability (r = 0.80), has been validated with both sleep diary and polysomnography [16], and is sensitive to clinical treatment response [21]. Scoring guidelines consist of the following: score of 0–7 (no clinical insomnia), 8–14 (subthreshold insomnia), 15–21 (clinical insomnia of moderate severity), and 22–28 (severe insomnia).
PTSD checklist
The 17-item PTSD checklist (PCL-M) is a validated self-report scale for assessing PTSD symptoms [17]. Items correspond to the DSM-IV symptoms of PTSD. Scores range from 17 to 85, with higher scores indicating more severe PTSD symptoms.
SF-36
The SF-36 [19] is a generic 36-item Short-Form Medical Outcomes Survey (SF-36). It has eight main domains: physical functioning, role limitation due to physical problems, role limitation due to emotional problems, social functioning, mental health, energy/vitality, bodily pain, and general health perception. Each dimension item score is coded, summed, and transformed onto a scale from 0 to 100 (worst to best possible health). In addition, the 8 scales are used to form 2 distinct high-order summary scales: the physical component summary (PCS) and the mental component summary (MCS). The PCS includes the physical functioning, role physical, bodily pain, and general health scales, and the MCS includes the vitality, social functioning, role emotional, and general mental health scales. The raw scores for each subscale and the 2 summary measures are standardized, weighted, and scored according to specific algorithms.
Pittsburgh Sleep Quality Index
The PSQI [18] is a self-rating questionnaire resulting in a global score between 0 and 21, which consists of seven dimensions of sleep quality. Since its introduction in 1989, the Pittsburgh Sleep Quality Index (PSQI) has gained widespread acceptance as a useful tool to measure sleep quality in different patient groups. Its good reliability and validity have been shown for patients with psychiatric and sleep disorders [22] and for patients with different somatic diseases [23]. The PSQI has internal consistency and a reliability coefficient (Cronbach’s alpha) of 0.83 for its seven components.
CPAP adherence
CPAP compliance was assessed at 12 weeks after initiation of therapy. Objective measures of CPAP use were obtained from a downloadable “smart card” compliance monitoring device. The percent of days used, the average time used per night for all nights, the average time used on nights CPAP worn, and the percentage of nights with ≥ 4 h of use were recorded. Similar to prior studies, adherence to CPAP was defined as the use of CPAP for ≥ 4 h per night on > 70% of nights [24]. At the end of the study, participants answered two questions on a 7-point Likert scale indicating the extent of any discomfort/stress or interference in sleep that was a function of the CPAP.
Statistical analysis
All analyses were performed with STATA software, version 13 (StataCorp, College Station, TX). Results for quantitative variables were expressed as means ± standard deviation. Data normality was assessed with the Shapiro-Wilk test. Discrete variables are summarized as frequency (group percentage). Proportions were compared using the Chi square test with Yates correction or Fisher’s exact test when necessary. Continuous variables were compared using two-tailed t tests for variables with normally distributed data and Mann-Whitney rank sum test for non-normally distributed data. Spearman’s rank correlation coefficients were used to assess the degree of association between two not normally distributed variables. A multivariate regression analysis to assess the association between the presence of COMISA and baseline MCS of SF-36, and PSQI after adjusting for severity of PTSD and AHI was performed. Subsequently, a multivariate logistic regression analysis was used to examine predictive factors of COMISA with those variables found to be contributory toward this outcome based on bivariate analysis. Only significant clinical and demographic variables from the initial group comparisons (p ≤ 0.1) were entered as confounders in the logistic regression analyses. A multicollinearity test was performed using the variance inflation factor to assess the degree of correlation between covariates. Results are presented as odds ratios (OR) with 95% confidence intervals (CI). All tests are 2-tailed with a 0.05 significance level. The p value was corrected for multiple comparisons using the Bonferroni adjustment when indicated.
Results
Baseline characteristics of the study population are shown in Table 1. Veterans with COMISA were younger and had lower BMI than those with OSA-only (p = 0.03 and p < 0.001; respectively). Female Veterans reported more frequently having insomnia in the presence of OSA than male Veterans did but the difference was not statistically significant (p = 0.15). The prevalence of hypertension, chronic heart disease, and chronic pulmonary disease were similar in the two groups. However, depression was more common in Veterans with COMISA that those with OSA-only (p = 0.004). Of the 49 patients in the entire sample receiving psychotropic medications, 63% were in the COMISA group and 37% in the OSA-only group (p = 0.001). Overall, 5 patients with COMISA and one with OSA-only were receiving medications with sedating properties (p = 0.19) [Fisher’s exact test] (Table 1).
There was no difference between the two groups in excessive daytime sleepiness (p = 0.16). The ISI score was 26.0 ± 6.4 in the COMISA group versus 11.8 ± 2.3 in the group of OSA alone (p < 0.001). In Veterans with OSA who were experiencing insomnia, no significant correlation was noted between AHI and ISI (r = − 0.07, p = 0.64). On polysomnography, the COMISA group experienced reduced total sleep time (p = 0.01) and longer sleep latency (p < 0.001) than Veterans with OSA-only. However, there was no significant difference in the time spent in NREM sleep or nadir oxygen saturation between the two groups. AHI was significantly higher in Veterans with OSA than those with COMISA (AHI 40.7 ± 19.2 and 29.8 ± 18.3/h, respectively; p = 0.01). By category, sleep apnea was more severe in the OSA-only group with 67% having AHI ≥ 30/h compared to 50% in the group with COMISA. In multivariate analysis, two factors-AHI and PCL-M-were included in the logistic regression after omitting age, depression, and BMI from the final model due to interrelatedness. Both AHI (OR 0.95; 95% CI 0.93–0.98, p = 0.01) and PCL-M (OR 1.21; 95% CI 1.05–1.19, p < 0.001) were highly predictive of COMISA in this population.
CPAP response and adherence
Average CPAP pressure was not different between the COMISA group (9.0 ± 2.4 cm H2O) and OSA-only group (9.8 ± 2.2 cm H2O) (p = 0.13). In both groups, the frequency of apnea and hypopnea events was reduced significantly following CPAP from 29.8 ± 18.3 to 4.2 ± 2.1/h in the COMISA group and from 40.7 ± 19.2 to 3.2 ± 2.6/h in the OSA-only group, respectively; p < 0.001). However, Veterans with PTSD and COMISA demonstrated significantly lower CPAP adherence. Those with OSA alone used CPAP on 49.5% ± 32.6% of nights, for 3.5 ± 2.2 h/night. In comparison, patients with PTSD and COMISA used CPAP on 32.9% ± 29.3% of nights (p = 0.001), for an average of 2.2 ± 1.8 h/night (p = 0.03). Resolution of sleepiness (ESS ≤ 10) occurred in 31.5% of PAP-adherent and 12.8% of PAP-non-adherent patients with COMISA, compared with 52.1% of PAP-adherent and 30.4% of non-adherent patients with PTSD and OSA-only. The ISI decreased in the COMISA group from 26.0 ± 5.9 at baseline to 24.8 ± 5.5 after CPAP but the difference did not attain statistical significance (p = 0.12). Eight (22%) of the 36 patients with COMISA whom insomnia symptoms have abated had moderate to severe sleep apnea (AHI range 18–62). A positive correlation was observed between CPAP interference and onset of sleep (derived from PSQI) at 12 weeks follow-up visit (r = 0.48, p = 0.03).
PTSD severity
At baseline, Veterans with COMISA exhibited worse PTSD symptomatology than those with OSA (67.5 ± 12.8 vs. 57.1 ± 10.3; p < 0.001) (Fig. 1). Following CPAP treatment, the PTSD severity declined in both groups in comparison to baseline (67.5 ± 12.8 to 52.9 ± 11.8; p < 0.001 in the COMISA group and 57.1 ± 10.3 to 37.0 ± 8.2; p < 0.001 in the OSA-only group). However, the change in PCL-M between baseline and 12 weeks of CPAP was smaller in Veterans with COMISA than those with OSA-only (14.6 ± 11.3 vs. 20.1 ± 10.8; p = 0.03).
Sleep quality of life
Veterans with COMISA had a lower baseline MCS than those with OSA-only (35.5 ± 14.4 versus 46.1 ± 16.9; p = 0.031). Mental health, vitality, and role-emotional were the three domains of the SF-36 that had lower scores in the COMISA group in comparison to the OSA-only group. After eliminating age and BMI from the analysis due to multicollinearity, COMISA remained highly correlated with both the physical and mental component summary of SF-36 (Table 2). Only one domain-role emotional-showed an improvement in the COMISA group post-CPAP therapy (Table 3). However, the overall MCS was not different between baseline and week 12 of CPAP treatment (p = 0.27). In contrast, the MCS for Veterans with OSA-only increased from 46.1 ± 16.9 at baseline to 61.8 ± 19.6 post-treatment (p < 0.001). The improvement was observed in all four domains: mental health, vitality, social functioning, and role emotional. Interestingly, there was no improvement in the standardized physical component of SF-36 after treatment in either group.
At enrollment, PSQI results (Table 3) showed that perceived daytime dysfunction and sleep quality were significantly worse in the COMISA group compared to the OSA-only group (p = 0.008 and p = 0.002; respectively), as well as in the overall PSQI score (p = 0.003). Perceived sleep efficiency, sleep duration, and sleep latency were comparable between the two groups at baseline. In multivariate analysis, COMISA was independently associated with baseline PSQI (Table 2). After 12 weeks of CPAP therapy, no significant changes were reported in any of the PSQI measures by Veterans with COMISA. However, there was a significant amelioration in the perceived sleep disturbances, sleep duration, and sleep latency in the OSA-only group after treatment. Similarly, the overall PSQI score decreased from 10.2 ± 1.8 to 7.8 ± 2.5 (p < 0.001).
Discussion
In this case series of Veterans with PTSD, we have demonstrated that COMISA imparts greater morbidity than those experiencing a single disorder. Not surprisingly, COMISA was responsible for greater daytime impairment and worse quality of life than PTSD with OSA-only. Although treatment with CPAP remains the most effective therapy for OSA, the presence of concomitant insomnia appears to reduce adherence and lessens the benefits engendered by abolishing these respiratory events.
Evidence from prior clinical investigations in non-PTSD participants suggests that both OSA and insomnia co-exist with over half of the patients undergoing evaluation for OSA reporting at least one insomnia complaint [25, 26]. In Veterans with PTSD, the unusually erratic night-to-night changes in sleeping patterns as well as the nightmares-triggered fear of sleep add to the complexity of insomnia symptomatology. Currently, there is a dearth of epidemiologic studies on COMISA in civilians with PTSD. In one study involving 44 crime victims with nightmares and insomnia, almost half of participants had evidence of OSA [27]. To our knowledge, the prevalence of COMISA in Veterans with PTSD has not been determined. Given that OSA and insomnia are the two predominant sleep disorders in Veterans with PTSD, the causes and possible mechanisms of the reported association between OSA, insomnia, and PTSD require further evaluation in order to establish an effective therapy.
Data examining the relationship between severity of OSA and insomnia have been conflicting. While Yang and colleagues [28] denoted a lower probability of insomnia in patients with OSA, Gold and coworkers [29] found that AHI was positively correlated with the appearance of difficulty maintaining sleep in OSA; specifically, higher AHI corresponded to a greater probability of insomnia in patients with OSA. Yet Krakow et al. [30] reported that the appearance of insomnia in a group of patients with OSA was independent of AHI. In the current study, we observed no correlation between AHI and ISI in the COMISA group. However, a higher AHI predicted a lower likelihood of having COMISA. The conflicting observations among these studies suggest that the population profile, the methods used in establishing the presence of insomnia, and the myriad of underlying comorbid disorders such as depression and substance abuse should be accounted for in delineating the association between these disorders. Because these findings were observed in Veterans with PTSD, the interaction between insomnia and OSA may not be reproducible in other population. Hitherto, no study has assessed the temporal sequence of disease occurrence on the clinical manifestations of these two sleep disorders. It can be hypothesized that Veterans with OSA who acquire insomnia may have the capacity to overcome interruption in sleep pattern while Veterans with insomnia who develop OSA may have considerable reduction in sleep perception that any compensatory mechanism would be unable to adjust for sleep fragmentation. Whatever the mechanism involved or the order of disease occurrence, the co-existence of sleep apnea and insomnia is not uncommon, and the identification of these disorders is the first step in instituting a successful therapeutic management. Interestingly, we have observed no difference in the reported excessive daytime sleepiness between COMISA and OSA-only group. It is plausible that the sleep homeostatic pressure generated by the co-existence of insomnia and milder sleep apnea is displayed as excessive daytime sleepiness with similar intensity to those who have more severe OSA alone. We cannot dismiss the fact that underlying psychiatric disorders, more commonly observed in COMISA, may have amplified hypersomnia. Unless objective assessment of excessive daytime sleepiness is undertaken, a distinction between reported and actual excessive sleepiness would be difficult to ascertain.
Consistent with previous clinical studies [12, 13, 25, 28], we have observed that Veterans with PTSD and COMISA experience increased morbidity and reduced quality of life. The co-occurrence of insomnia with OSA imparts serious clinical implications on existing comorbidities that would be otherwise under control had these conditions been independently associated with either of these ailments. Previously, Smith and colleagues [10] reported that patients with OSA and comorbid insomnia experienced more symptoms of depression, anxiety, and stress than those with OSA. Similarly, Krell and Kapur [25] reported a higher prevalence of psychiatric disorder in patients with OSA and comorbid insomnia than in patients with OSA alone. We found that all participants in our study population had PSQI total scores above the traditional cut-off score of 5, but the average scores were two points higher among those with PTSD and COMISA compared to those without indicating that both sleep quality and daytime functioning were severely deranged.
Given the significant decrease in PTSD severity following CPAP treatment [14], it was expected that the Veterans with COMISA would experience a reprieve from insomnia. Contrary to our expectations, insomnia severity did not change after OSA treatment. The poor adherence to CPAP in Veterans with COMISA may have curbed any benefits that may have resulted from suppression of apneic events. Contemporary investigations have found evidence for the negative impact of insomnia on CPAP use starting with the first 7 days of use and up to 2 years of follow-up. In a sleep clinic cohort of South Florida Hispanic veterans, the Insomnia Severity Index was the only independent predictor of 7 days CPAP use [31]. Another longitudinal study of 705 OSA individuals treated with positive airway pressure revealed that patients who reported symptoms of initial insomnia at baseline were more likely to be non-adherent at follow-up and this effect remained significant after adjusting for age, sex, BMI, smoking, and OSA severity [32]. Alternatively, the significant correlation between CPAP interference and sleep onset indicates that any improvement in insomnia that have occurred as a result of OSA treatment may have been abrogated by the interference of the CPAP itself. We cannot exclude however that there may a subgroup of patients that would experience relief from insomnia. Although we have not assessed the type of insomnia experienced by our participants, Bjornsdottir and coworkers [32] reported that patients who had frequent awakening at night were more likely to adhere to CPAP treatment while those who had difficulty falling asleep or going back to sleep after waking up early in the morning did not improve on CPAP treatment. In contrast, Wickwire and colleagues [33] have reported that difficulty maintaining sleep was consistently associated with less CPAP use as well as lower rates of adherence. Neither difficulty initiating sleep nor early morning awakening was associated with CPAP use. These observations have led to the belief that insomnia does not represent a symptom of sleep-disordered breathing but both insomnia and OSA represent distinct entity [34].
Despite the evidence-based proven treatments for insomnia disorder and OSA when they occur in isolation, treatment of COMISA and PTSD has not been widely studied, and few studies of treatment for COMISA in Veterans with PTSD have included sleep measures as outcomes [35, 36]. One study of VA providers treating Veterans with PTSD found that approximately 40% taught sleep hygiene techniques to PTSD patients with sleep problems [37]; however, prior studies and clinical guidelines suggest sleep hygiene education alone does not produce significant improvements in insomnia [38]. Recent research has demonstrated that use of behavioral sleep interventions can be effective as a means to reduce symptom severity and improve functional outcomes among individuals with PTSD and COMISA [39, 40]. Alternate models have used hypnotics with CPAP to overcome phobia and enhance adherence [41]. While none of our participants received any intervention for insomnia during the course of the study, available CBT modalities targeting COMISA in subjects with PTSD may only achieve a partial response. We conjecture that within the COMISA population there are different phenotypes depending on the presence of comorbid conditions, and type of insomnia with or without EDS [42]. Identifying these phenotypes would increase our ability to deliver a tailored adjunct therapy that can lead to sustainable CPAP treatment.
The current study has several limitations. First, the sample size was small and consisted primarily of Caucasian Veterans with PTSD. Given that the correlation between insomnia and OSA in PTSD remains scarce, whether such patterns are evident in other PTSD populations and geographical settings are not known. Second, because these data were derived from a clinical setting, the PTSD treatment delivered was tailored to individual needs and was not standardized. Third, despite the findings that Veterans with both insomnia and OSA had lower quality of life than those with OSA alone, a causality cannot be established, as we did not discern whether insomnia precipitated poor quality of life in patients with OSA or whether poor quality of life was a risk factor for insomnia in OSA [43]. Fourth, the lack of a control group makes it difficult to determine whether the changes in PTSD severity and quality of life measures can be attributed to natural progression of the disease or CPAP treatment. However, the established efficacy of CPAP in improving symptoms of OSA poses an ethical challenge in performing randomized controlled trials in symptomatic patients with a control arm. Fifth, CPAP treatment in Veterans with COMISA showed less impact on quality of life measures compared to OSA-only Veterans following CPAP treatment. Although this blunted response suggests that the co-existence of insomnia with OSA may have been the culprit, it is plausible that the lower adherence to CPAP in COMISA patients would have yielded the same response. Due to the relatively low rate of CPAP adherence in our population, adjusting for average of CPAP use in a small sample limits interpretability of the results.
In conclusion, COMISA in the context of PTSD has a potentially detrimental effect on psychological health and overall well-being for Veterans. While recent military conflicts have drawn attention to the associations between poor sleep and health among military personnel, there remains limited research on the relationship between PTSD and COMISA, particularly among Veterans who are at higher risk for both sleep difficulties. Further research is needed to better identify risk factors for PTSD and COMISA and to develop and disseminate effective screening tools and treatments for this growing segment of the Veteran population.
References
Krakow B, Hollifield M, Johnston L, Koss M, Schrader R, Warner TD, Tandberg D, Lauriello J, McBride L, Cutchen L, Cheng D, Emmons S, Germain A, Melendrez D, Sandoval D, Prince H (2001) Imagery rehearsal therapy for chronic nightmares in sexual assault survivors with posttraumatic stress disorder: a randomized controlled trial. JAMA 286(5):537–545. https://doi.org/10.1001/jama.286.5.537
Krakow B, Germain A, Tandberg D, Koss M, Schrader R, Hollifield M, Cheng D, Edmond T (2000) Sleep breathing and sleep movement disorders masquerading as insomnia in sexual-assault survivors. Compr Psychiatry 41(1):49–56. https://doi.org/10.1016/S0010-440X(00)90131-7
Clum GA, Nishith P, Resick PA (2001) Trauma-related sleep disturbance and self-reported physical health symptoms in treatment-seeking female rape victims. J Nerv Ment Dis 189(9):618–622. https://doi.org/10.1097/00005053-200109000-00008
Williams SG, Collen J, Orr N, Holley AB, Lettieri CJ (2015) Sleep disorders in combat-related PTSD. Sleep Breath 19(1):175–182. https://doi.org/10.1007/s11325-014-0984-y
Lettieri CJ, Williams SG, Collen JF (2016) OSA syndrome and posttraumatic stress disorder: clinical outcomes and impact of positive airway pressure therapy. Chest 149(2):483–490. https://doi.org/10.1378/chest.15-0693
Mysliwiec V, Gill J, Lee H, Baxter T, Pierce R, Barr TL, Krakow B, Roth BJ (2013) Sleep disorders in US military personnel: a high rate of comorbid insomnia and obstructive sleep apnea. Chest 144(2):549–557. https://doi.org/10.1378/chest.13-0088
Jaoude P, Vermont LN, Porhomayon J, El-Solh AA (2015) Sleep-disordered breathing in patients with post-traumatic stress disorder. Ann Am Thorac Soc 12(2):259–268. https://doi.org/10.1513/AnnalsATS.201407-299FR
Leiter JC, Knuth SL, Bartlett D Jr (1985) The effect of sleep deprivation on activity of the genioglossus muscle. Am Rev Respir Dis 132(6):1242–1245. https://doi.org/10.1164/arrd.1985.132.6.1242
Subramanian S, Guntupalli B, Murugan T, Bopparaju S, Chanamolu S, Casturi L, Surani S (2011) Gender and ethnic differences in prevalence of self-reported insomnia among patients with obstructive sleep apnea. Sleep Breath 15(4):711–715. https://doi.org/10.1007/s11325-010-0426-4
Smith S, Sullivan K, Hopkins W, Douglas J (2004) Frequency of insomnia report in patients with obstructive sleep apnoea hypopnea syndrome (OSAHS). Sleep Med 5(5):449–456. https://doi.org/10.1016/j.sleep.2004.03.005
Ong JC, Gress JL, San Pedro-Salcedo MG, Manber R (2009) Frequency and predictors of obstructive sleep apnea among individuals with major depressive disorder and insomnia. J Psychosom Res 67(2):135–141. https://doi.org/10.1016/j.jpsychores.2009.03.011
Krakow B, Melendrez D, Ferreira E, Clark J, Warner TD, Sisley B, Sklar D (2001) Prevalence of insomnia symptoms in patients with sleep-disordered breathing. Chest 120(6):1923–1929. https://doi.org/10.1378/chest.120.6.1923
Bjornsdottir E, Janson C, Gislason T, Sigurdsson JF, Pack AI, Gehrman P, Benediktsdottir B (2012) Insomnia in untreated sleep apnea patients compared to controls. J Sleep Res 21(2):131–138. https://doi.org/10.1111/j.1365-2869.2011.00972.x
El-Solh AA, Vermont L, Homish GG, Kufel T (2017) The effect of continuous positive airway pressure on post-traumatic stress disorder symptoms in veterans with post-traumatic stress disorder and obstructive sleep apnea: a prospective study. Sleep Med 33:145–150. https://doi.org/10.1016/j.sleep.2016.12.025
Johns MW (1991) A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep 14(6):540–545. https://doi.org/10.1093/sleep/14.6.540
Bastien CH, Vallieres A, Morin CM (2001) Validation of the insomnia severity index as an outcome measure for insomnia research. Sleep Med 2(4):297–307. https://doi.org/10.1016/S1389-9457(00)00065-4
Weathers FW, Huska JA, Keane TM (1993) The PTSD Checklist (PCL): Reliability, Validity, and Diagnostic Utility. Annual Convention of the International Society for Traumatic Stress Studies, San Antonio
Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ (1989) The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res 28(2):193–213. https://doi.org/10.1016/0165-1781(89)90047-4
McHorney CA, Ware JE Jr, Raczek AE (1993) The MOS 36-Item Short-Form Health Survey (SF-36): II. Psychometric and clinical tests of validity in measuring physical and mental health constructs. Med Care 31(3):247–263. https://doi.org/10.1097/00005650-199303000-00006
Kushida CA, Chediak A, Berry RB, Brown LK, Gozal D, Iber C, Parthasarathy S, Quan SF, Rowley JA (2008) Clinical guidelines for the manual titration of positive airway pressure in patients with obstructive sleep apnea. J Clin Sleep Med 4(2):157–171
Morin CM, Belleville G, Belanger L, Ivers H (2011) The Insomnia Severity Index: psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep 34(5):601–608. https://doi.org/10.1093/sleep/34.5.601
Doi Y, Minowa M, Uchiyama M, Okawa M, Kim K, Shibui K, Kamei Y (2000) Psychometric assessment of subjective sleep quality using the Japanese version of the Pittsburgh Sleep Quality Index (PSQI-J) in psychiatric disordered and control subjects. Psychiatry Res 97(2–3):165–172. https://doi.org/10.1016/S0165-1781(00)00232-8
Carpenter JS, Andrykowski MA (1998) Psychometric evaluation of the Pittsburgh Sleep Quality Index. J Psychosom Res 45(1):5–13. https://doi.org/10.1016/S0022-3999(97)00298-5
Kribbs NB, Pack AI, Kline LR, Smith PL, Schwartz AR, Schubert NM, Redline S, Henry JN, Getsy JE, Dinges DF (1993) Objective measurement of patterns of nasal CPAP use by patients with obstructive sleep apnea. Am Rev Respir Dis 147(4):887–895. https://doi.org/10.1164/ajrccm/147.4.887
Krell SB, Kapur VK (2005) Insomnia complaints in patients evaluated for obstructive sleep apnea. Sleep Breath 9(3):104–110. https://doi.org/10.1007/s11325-005-0026-x
Chung KF (2003) Relationships between insomnia and sleep-disordered breathing. Chest 123(1):310–311; author reply 311-313. https://doi.org/10.1378/chest.123.1.310
Krakow B, Melendrez D, Pedersen B, Johnston L, Hollifield M, Germain A, Koss M, Warner TD, Schrader R (2001) Complex insomnia: insomnia and sleep-disordered breathing in a consecutive series of crime victims with nightmares and PTSD. Biol Psychiatry 49(11):948–953. https://doi.org/10.1016/S0006-3223(00)01087-8
Yang CM, Liao YS, Lin CM, Chou SL, Wang EN (2011) Psychological and behavioral factors in patients with comorbid obstructive sleep apnea and insomnia. J Psychosom Res 70(4):355–361. https://doi.org/10.1016/j.jpsychores.2010.12.005
Gold AR, Gold MS, Harris KW, Espeleta VJ, Amin MM, Broderick JE (2008) Hypersomnolence, insomnia and the pathophysiology of upper airway resistance syndrome. Sleep Med 9(6):675–683. https://doi.org/10.1016/j.sleep.2007.08.013
Krakow B, Ulibarri VA, Romero EA (2010) Patients with treatment-resistant insomnia taking nightly prescription medications for sleep: a retrospective assessment of diagnostic and treatment variables. Prim Care Companion J Clin Psychiatry 12(4). https://doi.org/10.4088/PCC.09m00873bro
Wallace DM, Vargas SS, Schwartz SJ, Aloia MS, Shafazand S (2013) Determinants of continuous positive airway pressure adherence in a sleep clinic cohort of South Florida Hispanic veterans. Sleep Breath 17(1):351–363. https://doi.org/10.1007/s11325-012-0702-6
Bjornsdottir E, Janson C, Sigurdsson JF, Gehrman P, Perlis M, Juliusson S, Arnardottir ES, Kuna ST, Pack AI, Gislason T, Benediktsdottir B (2013) Symptoms of insomnia among patients with obstructive sleep apnea before and after two years of positive airway pressure treatment. Sleep 36(12):1901–1909. https://doi.org/10.5665/sleep.3226
Wickwire EM, Smith MT, Birnbaum S, Collop NA (2010) Sleep maintenance insomnia complaints predict poor CPAP adherence: a clinical case series. Sleep Med 11(8):772–776. https://doi.org/10.1016/j.sleep.2010.03.012
Kapur VK, Baldwin CM, Resnick HE, Gottlieb DJ, Nieto FJ (2005) Sleepiness in patients with moderate to severe sleep-disordered breathing. Sleep 28(4):472–477. https://doi.org/10.1093/sleep/28.4.472
Schnurr PP, Friedman MJ, Engel CC, Foa EB, Shea MT, Chow BK, Resick PA, Thurston V, Orsillo SM, Haug R, Turner C, Bernardy N (2007) Cognitive behavioral therapy for posttraumatic stress disorder in women: a randomized controlled trial. JAMA 297(8):820–830. https://doi.org/10.1001/jama.297.8.820
Spoormaker VI, Montgomery P (2008) Disturbed sleep in post-traumatic stress disorder: secondary symptom or core feature? Sleep Med Rev 12(3):169–184. https://doi.org/10.1016/j.smrv.2007.08.008
Rosen CS, Chow HC, Finney JF, Greenbaum MA, Moos RH, Sheikh JI, Yesavage JA (2004) VA practice patterns and practice guidelines for treating posttraumatic stress disorder. J Trauma Stress 17(3):213–222. https://doi.org/10.1023/B:JOTS.0000029264.23878.53
Gellis LA, Lichstein KL (2009) Sleep hygiene practices of good and poor sleepers in the United States: an internet-based study. Behav Ther 40(1):1–9. https://doi.org/10.1016/j.beth.2008.02.001
Fung CH, Martin JL, Josephson K, Fiorentino L, Dzierzewski JM, Jouldjian S, Tapia JC, Mitchell MN, Alessi C (2016) Efficacy of cognitive behavioral therapy for insomnia in older adults with occult sleep-disordered breathing. Psychosom Med 78(5):629–639. https://doi.org/10.1097/PSY.0000000000000314
Krakow B, Melendrez D, Lee SA, Warner TD, Clark JO, Sklar D (2004) Refractory insomnia and sleep-disordered breathing: a pilot study. Sleep Breath 8(1):15–29. https://doi.org/10.1007/s11325-004-0015-5
Lettieri CJ, Quast TN, Eliasson AH, Andrada T (2008) Eszopiclone improves overnight polysomnography and continuous positive airway pressure titration: a prospective, randomized, placebo-controlled trial. Sleep 31(9):1310–1316
Saaresranta T, Hedner J, Bonsignore MR, Riha RL, McNicholas WT, Penzel T, Anttalainen U, Kvamme JA, Pretl M, Sliwinski P, Verbraecken J, Grote L, Group ES (2016) Clinical phenotypes and comorbidity in European sleep apnoea patients. PLoS One 11(10):e0163439. https://doi.org/10.1371/journal.pone.0163439
LeBlanc M, Merette C, Savard J, Ivers H, Baillargeon L, Morin CM (2009) Incidence and risk factors of insomnia in a population-based sample. Sleep 32(8):1027–1037. https://doi.org/10.1093/sleep/32.8.1027
Acknowledgments
The views expressed in this manuscript do not communicate an official position of the Department of Veterans Affairs.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the VA WNYHS institutional review board and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
This article is part of the Topical Collection on Comorbid Insomnia and OSA (COMISA) in Veterans
Rights and permissions
About this article
Cite this article
El-Solh, A.A., Adamo, D. & Kufel, T. Comorbid insomnia and sleep apnea in Veterans with post-traumatic stress disorder. Sleep Breath 22, 23–31 (2018). https://doi.org/10.1007/s11325-017-1618-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-017-1618-y