Abstract
Purpose
The aim of this article was to assess the sleep behaviors that serve as risk factors related to bruxism in children ages 0 to 12 years by performing a systematic review and meta-analysis of published studies.
Methods
Seven databases were searched to identify all peer-reviewed articles potentially relevant to the review. Data were pooled for random-effects modeling. Sleep risk factors related to bruxism in this age group are summarized using pooled odds ratios (ORs), 95% confidence intervals (CIs), and P values.
Results
Of 5637 initially identified articles, 14 met inclusion criteria. Study qualities of all case-control studies were high. Quality of cross-sectional studies was more variable. The pooled ORs, 95% CIs, and P values were as follows: snoring (2.86, 1.85–4.42, <0.0001), mouth breathing (1.51, 1.04–2.18, 0.029), restless sleep (2.31, 1.89–2.83, <0.0001), drooling (1.79, 1.07–2.97, 0.026), stomach position during sleep (1.70, 1.0–2.39, 0.003), and inadequate sleep time (2.56, 1.48–4.43, 0.001).
Conclusions
Snoring, mouth breathing, restless sleep, drooling, stomach position during sleep, and lack of sleep were the risk factors related to bruxism in children.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bruxism is a repetitive jaw-muscle activity characterized by clenching or grinding of the teeth and/or by bracing or thrusting of the mandible. Bruxism has two distinct circadian manifestations: (1) occurring during sleep (termed sleep bruxism) or (2) occurring during wakefulness (awake bruxism) [1]. Bruxism is a source of many dental and neuromuscular problems, including tooth wear, periodontal disease, hypertrophy of the masticatory muscles, headaches, and temporomandibular disorders [2–5]. Quality of life in patients with bruxism, especially those with pain, is also affected.
Due to differences in definitions, diagnostic methods, population characteristics, and research methods between studies, there is a wide variation of reported prevalence of bruxism in children. A recent review reported a variability of prevalence between 3.5 and 40.6% with a commonly described decrease with age and no gender differences [6]. Briefly put, its prevalence rate is high and its associated complications are frequent. Since childhood is the most critical period for human growth and development, bruxism in children is an important public health problem.
Bruxism is associated with multiple risk factors though many unresolved issues remain concerning the etiology of bruxism. These unresolved issues carry consequences for clinical management strategies [7]. Since 1928, bruxism has been associated with psychological factors. Many scholars believed that bruxism was an expression of neurological and psychological problems [8]. However, more current literature suggests that certain behaviors that occur during sleep are also risk factors associated with bruxism.
The purpose of the current study is to conduct a systematic review and meta-analysis of the existing literature to determine which behaviors during sleep are risk factors for bruxism in children of ages 0 to 12 years.
Materials and methods
Search strategy
This systematic review was conducted according to the PRISMA statement [9] and according to guidelines from the Cochrane Handbook for Systematic Reviews of Interventions [10]. We conducted a systematic search of seven online databases, with the last search updated on September 15, 2016. The seven databases were Pubmed, Excerpta Medica Database (Embase), Cochrane Library database, Web of Science, Chinese National Knowledge Infrastructure (CNKI), Chinese Biomedical Literature Database (CBM), and Wanfang Data (WF). All searches were conducted using a combination of subject headings and free-text terms; we determined the final search strategy through several pre-searches. The keywords used in the search strategy were as follows: (“Bruxism”[Mesh] OR “Sleep Bruxism”[Mesh] OR “Teeth Grinding Disorder”[Title/Abstract]) OR “Teeth Grinding Disorders”[Title/Abstract] OR “Sleep Bruxisms”[Title/Abstract] OR “Nocturnal Teeth Grinding Disorder”[Title/Abstract] OR “Nocturnal Bruxism”[Title/Abstract] OR “Nocturnal Bruxisms”[Title/Abstract] OR “Childhood Sleep Bruxism”[Title/Abstract] OR “Childhood Sleep Bruxisms”[Title/Abstract] OR “Sleep-Related Bruxism”[Title/Abstract] OR “Sleep-Related Bruxisms”[Title/Abstract] OR “Adult Sleep Bruxism”[Title/Abstract] OR “Adult Sleep Bruxisms”[Title/Abstract] OR bruxism[Title/Abstract] OR “teeth grinding”[Title/Abstract] OR “Sleep bruxism”[Title/Abstract]) AND (children[Title/Abstract] OR child[Title/Abstract] OR kid[Title/Abstract] OR kids[Title/Abstract] OR “Child”[Mesh]). There was no restriction on language or publication years. We also reviewed the reference lists of the identified articles to avoid missing relevant studies.
Inclusion and exclusion criteria
The following inclusion criteria were employed for this meta-analysis: (1) randomized clinical trial (RCT); (2) cohort study; (3) cross-sectional study; (4) case-control study; (5) bruxism was assessed through a questionnaire for parents or guardians; (6) all considered participants were bruxers, with tooth grinding and/or clenching; (7) all considered participants’ age of 0 to 12 years; and (8) published in Chinese or English.
The following were the exclusion criteria: (1) case report, (2) reviews, (3) abstract and author debates or editorials, (4) lack of effective statistical analysis, (5) lack of standardized measures for bruxism evaluation, and (6) studies on patients with systemic diseases or syndromes, or neurological or psychiatric disorders.
Data extraction
Following the inclusion criteria, two authors (Guo and Wang) independently selected the literature by reading the titles and abstracts. The full text of each identified article was then read to determine whether it was suitable for inclusion. Disagreements were resolved through consensus or by discussion with a third author (Niu). For each eligible study, the following information was independently extracted by two authors (Guo and Wang) and examined by the third author (Niu): name of the first author, date of publication, trial type, children’s ages, bruxism definition, bruxism diagnostic means, sample size of cases and controls, OR and 95% CI, and behaviors that occur during sleep (Table 1).
Quality assessment
According to the PRISMA statements and to the Centre for Reviews and Dissemination (CRD), the evaluation of methodological quality gives an indication of the strength of evidence provided by the study because flaws in the design or in the conduction of a study can result in biases [25, 26].
According to the Newcastle-Ottawa scale (NOS) on case-control studies [27], we evaluated the qualities of all included case-control studies based on object selection, comparability, and exposure. A star was described as an appropriate entry, with each star representing one point. The possible quality assessment score ranged from zero to nine points with a high score indicating a good quality study. We evaluated the qualities of all included cross-sectional studies by criteria of the cross-sectional/prevalence study quality [28]. There were 11 questions, and every question had three options, such as yes, no, and unclear.
Statistical analysis
Statistical analysis was performed using Stata version 12.0 (StataCorp LLC, College Station, TX, USA). In some included studies, there were no ORs or 95% CIs, but we were able to calculate the ORs and 95% CIs through sample size of cases and controls. Pooled ORs and 95% CIs were calculated by the Stata program. In some included studies, there were no ORs or 95% CIs nor could they be calculated. In those circumstances, we extracted the P value and analyzed with the pooled OR and 95% CI. A P value of <0.05 was considered statistically significant. A chi-square-based Q test was applied to check the heterogeneity among studies. An I-squared less than 40% indicated no significant heterogeneity among studies. The random-effects model (the DerSimonian and Laird method) was applied in the meta-analysis. When the included trials were less than ten, we did not analyze the publication bias [29].
Results
Study selection
The search strategy identified 5637 potential articles. After removal of duplicates, 2812 papers were analyzed. Subsequently, 2755 papers were excluded because they were not relevant to the subject of the study. Of the remaining 57 papers, 43 were excluded because they did not meet the inclusion and exclusion criteria. The remaining 14 papers were included in the meta-analysis (Fig. 1).
Quality assessment
In evaluation of the quality of case-control studies, the total scores of all included studies were greater than or equal to 8 indicating high quality studies (Table 2). The quality of cross-sectional studies was not as uniformly excellent (Table 3). All studies did not indicate the time period used for identifying patients nor did they all record follow-up. One trial [16] did not summarize patient response rates and completeness of data collection (Table 4).
Study results
-
1.
Regarding the relationship between snoring and bruxism, five trials were included in the analysis [12, 16, 17, 21, 24], including 10,902 subjects. One trial [16] had only OR and did not include 95% CI, so it could not be combined with other trials. Pooled OR was 2.86, 95% CI was 1.85–4.42, and P value was <0.0001, but Q-analysis indicated non-homogeneity, so we conducted a sensitivity analysis on the main snoring symptoms and omitted a single trial [12]. This changed the I-squared statistic from 86 to 0% (Figs. 2 and 3). The newly calculated pooled OR was 3.56, 95% CI was 2.88–4.38, and the P value was <0.0001 (Fig. 3).
-
2.
Four trials were included in the analysis of mouth breathing and bruxism [15, 17, 18, 20], including 712 subjects. Q-analysis indicated homogeneity, the pooled OR and 95% CI were 1.51 (1.04–2.18), and the P value was 0.029 (Fig. 4).
-
3.
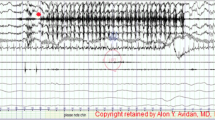
Three trials were used in the analysis of the relationship between restless sleep and bruxism [11, 13, 14], including 2170 subjects. In Figs. 5 and 6, Q-analysis indicated homogeneity, the pooled OR and 95% CI were 2.31 (1.89–2.83), and the P value was <0.0001.
-
4.
Four trials were included in the analysis of awakening at night and bruxism [12, 15–17], including 6381 subjects. Q-analysis indicated homogeneity, the pooled OR and 95% CI were 0.87 (0.63–1.21), and the P value was 0.424 (Figs. 7 and 8).
-
5.
One article [24] assessed the relationship between awakening or crying at night and bruxism [24], demonstrating an OR = 1.503, 95% CI = 1.112–2.032, and P = 0.008.
-
6.
For evaluation of position during sleep and bruxism, there were four conditions as follows:
-
(1)
Sleep with head arched back [12]: (OR 1.25, 95% CI 0.99–1.59, P = 0.065).
-
(2)
Side position during sleep, on back(ref) [17, 24]. Two trials were used for the analysis including 2110 subjects. Q-analysis indicated homogeneity (Fig. 7). The pooled OR and 95% CI were 1.48 (1.07–2.06), and the P value was 0.019.
-
(3)
Stomach position during sleep vs sleeping on back [17, 22, 24]. Three trials were used for the analysis, including 1611 subjects. Q-analysis indicated homogeneity (Fig. 8). The pooled OR and 95% CI were 1.70 (1.20–2.39), and the P value was 0.003.
-
(4)
Mixed position during sleep vs sleeping on back [22]. (OR 4.99, 95% CI 2.25–11.03, P < 0.0001).
-
(1)
-
7.
Four trials were assessed in the analysis of the relationship between sleep talking and bruxism [16, 17, 19, 23], including 397 subjects. One trial [16] possessed only OR and P value, without 95% CI. Another trial [19] involved only P values. These two trials could not be combined with other trials. Q-analysis indicated homogeneity (Fig. 9), with pooled OR and 95% CI 1.8 (1.02–3.18) and P value 0.043.
-
8.
Three trials were used in the analysis of the relationship between drooling and bruxism [15–17], including 354 subjects. One trial [16] possessed only OR and P value, without 95% CI. This trial could not be combined with other trials. Q-analysis indicated homogeneity (Fig. 10). The pooled OR and 95% CI were 1.79 (1.07–2.97), and the P value was 0.026.
-
9.
Two trials were used in the analysis of the relationship between nightmares and bruxism [16, 17], including 217 subjects totally. These trials showed a relationship between frequency of night mares and bruxism: more than once a week (OR = 5.62, 95% CI = 1.14–27.66, P = 0.044), once a week (P = 0.355), and once a month (P = 0.366).
-
10.
Two trials were used in the analysis of the relationship between sleep hours and bruxism [14, 15], including 499 subjects. Differing references for sleep duration showed different OR for bruxism: One trial [14] used sleep hours less than or equal to 8 h reference more than 8 h (OR = 2.56, 95% CI = 1.48–4.43, P = 0.001), and another trial [15] used sleep of 10 to 11 h as adequate sleep (OR = 5.1, 95% CI = 2.27–11.47, P < 0.0001).
-
11.
One article (Tachibana M, 2016) [12] putatively showed associations of sleep bruxism with obstructive sleep apnea: Move a lot during sleep (OR = 1.47, 95% CI = 1.29–1.68, P < 0.0001) and sleeps with mouth open (OR = 1.56, 95% CI = 1.35–1.81, P < 0.0001).
-
12.
One article (Serra-Negra JM, 2014) [14] demonstrated the relationship between bruxism and sleep with light on (OR = 2.37, 95% CI = 1.45–3.88, P = 0.001) and noise in room (OR = 2.70, 95% CI = 1.65–4.43, P < 0.001).
-
13.
The association of sleep bruxism and sleeping with hand on face (Soares KAN, 2016) [17] was demonstrated (OR = 2.41, 95% CI = 1.22–4.79, P = 0.011).
-
14.
One trial (Suwa S, 2009) [21] showed an association between sleep bruxism and frequency of sleep starts (high frequency vs low frequency) (OR = 2.80, 95% CI = 2.05–3.84, P < 0.0001).
-
15.
One trial (Jiang Y, 2010) [24] showed an association between sleep bruxism and not having a nap habit (OR = 1.35, 95% CI = 1.03–1.77, P = 0.028).
Discussion
The main findings of this systematic review and meta-analysis are that snoring, mouth breathing, restless sleep, drooling, stomach position during sleep, and lack of sleep are risk factors related to bruxism in children. We believe that these findings are convincingly demonstrated even though there were trials that used different study designs such as case control and cross-sectional studies, different definitions for conditions, differing ages of the sample populations, and variation in sample sizes. The associations that we report hold true even after excluding studies for inadequate quality and non-homogeneity. To show a relationship between bruxism and particular conditions such as mouth breathing, it may be necessary to perform studies using larger sample sizes to confirm the findings with a higher degree of certainty.
One previous systematic review had already demonstrated the association between restless sleep and bruxism, presenting a strong association [7]. However, this finding was based upon a single trial [14]. In our systematic review, we were able to incorporate an additional two trials. Since all three trials used logistic regression analysis and were determined by quality assessment to be of high quality, the findings showing the association were comprehensive and precise.
Position during sleep was one of the more complicated analyses to perform because four distinct positions have been reported: sleep with head arched back, side sleeping, stomach sleeping, and mixed position. This analysis was further complicated by the fact that when children fall asleep, they may move and spontaneously change sleeping position by themselves. In any case, we feel confident in the finding that side sleeping was not associated with bruxism while stomach sleeping appeared to have a strong association. Our finding suggests that parents should help their children assume a side sleeping position (avoiding stomach sleeping) in order to reduce the risk of bruxism or to relieve symptoms of bruxism.
Our assessment of sleep talking as a risk factor for bruxism revealed problems with study design (cross-sectional studies), sample sizes, and variance between the studies. We believe that further well-designed and adequately powered studies are necessary to confirm an association between bruxism and sleep talking.
With this systematic review and meta-analysis, we highlight the need for methodologically sound and well-conducted studies, with adequate statistical analysis and properly powered sample sizes to settle remaining questions about sleep behaviors and their associations with bruxism. Furthermore, there is a need to develop standardized and validated diagnostic criteria for sleep behaviors including clinical assessments associated with interviewing with parents or guardians. A final observation is that the use of validated portable devices to measure sleep behaviors objectively would be an enormous step forward in the assessment of risk factors for bruxism.
As outlined in the paragraphs above, there are a number of important limitations to this systematic review and meta-analysis. First, the use of data obtained from questionnaires may be subject to bias due to the potential lack of observation of bruxism by parents/guardians who are unaware of this activity in their children. Second, our analysis is dependent upon and limited by the design of available studies published in the literature. In particular, cross-sectional studies do not allow for detection of bruxism and its associations over time. Third, this analysis is further limited by the small sample sizes reported in numerous studies, a factor that may easily lead to bias.
Conclusion
This meta-analysis revealed that snoring, mouth breathing, restless sleep, drooling, stomach position during sleep, and lack of sleep were risk factors related to bruxism in children. It is recommended that parents consider ways to reduce these sleeping behaviors in so far as possible to minimize the risk of developing bruxism and its associated comorbidities.
Abbreviations
- OR:
-
Odds ratio
- CI:
-
Confidence interval
- ref.:
-
Reference
- NOS:
-
Newcastle-Ottawa scale
- PRISMA:
-
Preferred reporting items for systematic reviews and meta-analyses
- CRD:
-
Centre for Reviews and Dissemination, University of York
References
Lobbezoo F, Ahlberg J, Glaros AG, Katos T, Koyano K, Lavigne GJ et al (2013) Bruxism defined and graded: an international consensus. J Oral Rehabil 40:2–4. doi:10.1111/joor.12011
Glaros AG, Rao SM (1977) Bruxism: a critical review. Psychol Bull 84:767–781
Glaros AG, Rao SM (1977) Effects of bruxism: a review of the literature. J Prosthet Dent 38:149–157
Xhonga FA (1977) Bruxism and its effect on teeth. J Oral Rehab 4:65–76
Thompson BA, Blount BW, Krumholz TS (1994) Treatment approaches to bruxism. Am Fam Physician 49:1617–1622
Manfredini D, Winocur E, Guarda-Nardini L, Paesani D, Lobbezoo F (2013) Epidemiology of bruxism in adults: a systematic review of literature. J Orofac Pain 27:99–110. doi:10.11607/jop.921
Castroflorio T, Bargellini A, Rossini G, Cugliari G, Rainoldi A, Deregibus A (2015) Risk factors related to sleep bruxism in children: a systematic literature review. Arch Oral Biol 60:1618–1624. doi:10.1016/j.archoralbio.2015.08.014
Zhao AM, Qi JL (2008) An investigation on the personal characteristics and mental health of patients with bruxism. China Journal of Health Psychology 16(7):836–838
Moher D, Liberati J, Altman DG, the PRISMA group (2009) Preferred reporting items for systematic reviews and meta-analysis: the PRISMA statement. PLoS Med 6(7):e.000097. doi:10.1371/journal.pmed.1000097
Higgins JPT, Green S (2011) Cochrane handbook for systematic reviews of interventions version 5.1.0. The Cochrane Collaboration. http://www.cochrane-handbook.org. Accessed March 2011
Junqueira TH, Nahas-Scocate AC, Valle-Corotti KM, Conti AC, Trevisan S (2013) Association of infantile bruxism and the terminal relationships of the primary second molars. Brazilian oral research 27(1):42–47
Tachibana M, Kato T, Kato-Nishimura K, Matsuzawa S, Mohri I, Taniike M (2016) Associations of sleep bruxism with age, sleep apnea, and daytime problematic behaviors in children. Oral Dis 22(6):557–565. doi:10.1111/odi.12492
Nahas-Scocate AC, Coelho FV, de Almeida VC (2014) Bruxism in children and transverse plane of occlusion: is there a relationship or not? Dental Press Journal of Orthodontics 19(5):67–73. doi:10.1590/2176-9451.19.5.067-073.oar
Serra-Negra JM, Paiva SM, Fulgencio LB, Chavez BA, Lage CF, Pordeus IA (2014) Environmental factors, sleep duration, and sleep bruxism in Brazilian schoolchildren: a case-control study. Sleep Med 15(2):236–239. doi:10.1016/j.sleep.2013.08.797
Simoes-Zenari M, Bitar ML (2010) Factors associated to bruxism in children from 4–6 years. Pro-fono: revista de atualizacao cientifica 22(4):465–472
Alencar NA, Fernandes AB, Souza MM, Luiz RR, Fonseca-Goncalves A, Maia LC (2016) Lifestyle and oral facial disorders associated with sleep bruxism in children. Cranio: J Craniomandibular Pract 1–7. doi:10.1080/08869634.2016.1196865.
Soares KAN, Melo RMCS, Gomes MC, Perazzo MF, Granville-Garcia AF, Menezes VA (2016) Prevalence and factors associated to bruxism in preschool children. Journal of Public Health (Germany) 24(3):209–214
Miamoto CB, Pereira LJ, Ramos-Jorge ML, Marques LS (2011) Prevalence and predictive factors of sleep bruxism in children with and without cognitive impairment. Brazilian Oral Research 25(5):439–445
Zhu X, Zheng SG, Zheng Y, Fu KY, Zhou YS, Yu C (2009) The related factors of bruxism in children. Chinese Journal of Stomatology 44(1):15–18
Serra-Negra JM, Paiva SM, Auad SM, Ramos-Jorge ML, Pordeus IA (2012) Signs, symptoms, parafunctions and associated factors of parent-reported sleep bruxism in children: a case-control study. Braz Dent J 23(6):746–752
Suwa S, Takahara M, Shirakawa S, Komada Y, Sasaguri K, Onozuka M et al (2009) Sleep bruxism and its relationship to sleep habits and lifestyle of elementary school children in Japan. Sleep and Biological Rhythms 7(2):93–102
Zhang L, Ren XY, Yu LL, Cai SK (2000) Investigation of children’s nocturnal bruxism and sleep positions. Yun Nan Medicine 6:493
Wang XJ (2011) Study of influencing factors of deciduous dentition bruxism. Chinese Journal of Practical Stomatology 4(4):233–235
Jiang Y, Li JM, Luo XM, Cai YM, Liu JH (2010) Epidemic investigation of bruxism in 3 to 12 years old children in Changsha City. J Appl Clin Pediatr 25(5):363–365
Moher D, Liberati A, Tetzlaff J, Altman DG (2010) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg 8(5):336–341. doi:10.1016/j.ijsu.2010.02.007
Centre for Reviews and Dissemination (2008) Systematic reviews—CRD’s guidance for undertaking reviews in health care. Centre for Reviews and Dissemination, University of York, York
Stang A (2010) Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 25:603–605. doi:10.1007/s10654-010-9491-z
Rostom A, Dube C, Cranney A et al (2004) Celiac disease. Rockville (MD): Agency for Healthcare Research and Quality (US). Appendix D. Quality Assessment Forms. http://www.ncbi.nim.nih.ov/books/NBK35156/. Accessed Sept 2004
Lau J, Ioannidis JP, Terrin N et al (2016) The case of the misleading funnel plot. BMJ 333(7568):597–600. doi:10.1136/bmj.333.7568.597
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding sources
No funding was received for this research.
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Rights and permissions
About this article
Cite this article
Guo, H., Wang, T., Li, X. et al. What sleep behaviors are associated with bruxism in children? A systematic review and meta-analysis. Sleep Breath 21, 1013–1023 (2017). https://doi.org/10.1007/s11325-017-1496-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-017-1496-3