Abstract
Purpose
Although obstructive sleep apnea (OSA) syndrome is a common disorder; the connection between OSA and smoking habits is still controversial. In this study, we investigated whether active smoking and pack × years of smoking have an impact on the severity of the disease regarding the patients with OSA.
Methods
This study included 964 patients referred to the Sleep Disorders Clinic between 01.01.2007 and 01.03.2013 with an overnight polysomnographic diagnosis of OSA. The correlation between smoking habits and polysomnographic parameters has been studied in detail.
Results
There were 684 male (79 %) and 280 female (21 %) patients, 367 (50.6 %) of whom never smoked. Of all, 20.7 % of the smokers were current smokers (n = 150) while 28.2 % were former smokers (n = 208). Active smokers had a mean age of 49.53 (SD 10.17) while former smokers and never smokers had a mean age of 51.37 (SD 10.62), 54.2 (SD 11.56), respectively, which was statistically significant (p < 0.0001). There was a significant male predominance in smoking (p < 0.0001). In addition, male patients displayed more severe OSA than female patients. (p = 0.001). Desaturation time during sleep was found to be significantly longer in the group of former smokers in comparison to never smokers (73.84 SD 97.1–52 SD 85.8) (p = 0.005). Besides, as the apnea hypopnea index increased, the mean pack × years rose significantly (p = 0.01). Severe smokers compared to mild smokers had higher AHI, lower NREM 3, higher NREM1-2 stages (p = 0. 017, p = 0.007, p < 0.001).
Conclusion
In this study, we found that cigarette smoking was associated with early age disease; heavy smokers had more severe OSA.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obstructive sleep apnea syndrome (OSA) is a common chronic disorder characterized by snoring, repeated episodes of airflow cessation, hypoxemia during sleep, and daytime hypersomnolence [1]. Its prevalence is 16 to 33 % in men and 8 to 19 % in women, with 80 % underdiagnosed [2, 3]. OSA has been shown to increase the risk of hypertension, stroke, and cardiovascular disease [4–6]. Furthermore, it has been demonstrated to increase morbidity as well. Therefore, focusing on the diagnosis and risk factors is essential for the prevention of OSA [2].
OSA has well-known risk factors such as male sex, older age, alcohol consumption, genetic factors, and a narrowed upper airway. But the connection between exposure to smoke and OSA is not clear. Smoking may be a risk factor for sleep apnea or snoring [3, 7–9]. Studies have confirmed the effect of smoking on OSA and found that the morbidity of sleep-related respiratory disorders is higher for smokers [7–10].
The correlation between smoking and OSA has not been studied in detail and the available evidence does not conclusively establish a clinically significant relationship [11]. In particular, the direct impact of smoking on OSA and the polysomnographic results, and the correlation between current or former smoking and the severity of OSA have not been adequately demonstrated [12]. For this reason, we aimed to study the relationship of OSA and OSA severity with current and former cigarette smoking as potential risk factors for sleep-disordered breathing.
Materials and methods
Study design and subjects
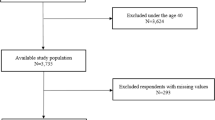
This study included 964 patients referred to the Sleep Disorders Clinic within the department of pulmonary diseases between 01.01.2007 and 01.03.2013 and diagnosed with OSA. Throughout this period, totally 5892 patients had been hospitalized in our Sleep Disorders Clinic. The diagnosis of OSA was established by overnight polysomnography. Medical and polysomnographic records of 964 patients were reviewed retrospectively. Patients with unclear smoking history or missing data in their polysomnography records were excluded (n = 239). The study protocol was approved by the Institutional Review Board of the research hospital.
Smoking habits
Patients with an active smoking history >2 years were considered current smokers, and patients with no smoking history were nonsmokers. Smokers were divided into two groups: current and former smokers. Former smoker referred to smokers who quit smoking for at least 6 months. Smoking history was quantified in number of pack years (PYs) as (packs smoked per day) × (years as a smoker). Also, we divided smokers according to their pack × years of smoking into three categories; mild (≤9 PYs), moderate (10–19 PYs), and severe (≥20 PYs). All of these data were obtained from medical records of the patients recruited in the study.
Polysomnography
Polysomnography (PSG) was performed in the Sleep Laboratory with Grass Technologies Comet Series EEG/PSG with AS40 Amplifier System running Grass Technologies Twin software version 4 (Grass Technologies, Astro-Med Inc. Product Group, USA) and included four electroencephalography (EEG) channels (C3 to A1, C4 to A2, O1 to A2, and O2 to A1), right and left electrooculography (EOG) channels, one chin electromyography (EMG) channel and four tibialis anterior EMG channels, finger pulse oximeter, strain gauges for thoracoabdominal movements, one electrocardiography (ECG) lead, a nasal airflow (pressure cannula), a nasal thermistor, and a digital microphone for snoring detection. PSG recordings were scored in 30-s epochs for sleep, breathing, and oxygenation according to the standard criteria of the American Academy of Sleep Medicine (AASM) [12]. Obstructive apnea was defined as 90 % cessation of oro-nasal airflow for at least 10 s in the presence of chest-wall motion. Hypopnea was defined as 50 % or higher reduction in the airflow, associated with 3 % or higher arterial oxygen desaturation and/or arousal, or 30 % or higher reduction in the respiratory airflow associated with 4 % or higher arterial oxygen desaturation and/or arousal for at least 10 s. Apnea hypopnea index (AHI) was calculated as the total number of apneas and hypopneas per hour of sleep. Diagnosis of OSA was based on PSG findings, according to the International Classification of Sleep Disorders 2 (ICSD-2) [13]. Subjects with an AHI ≥5 were considered to have OSA, and OSA severity was classified as mild (5≤ AHI <15), moderate (15≤ AHI <30), or severe (AHI ≥30). The oxygen desaturation index (ODI) which measures the number of oxygen desaturations ≥3 % per sleeping hour was determined. Body mass index (BMI) and ODI were measured for each group in order to analyze the relationship between these variables and OSA severity [14, 15]. Excessive daytime sleepiness was defined as the score of Epworth sleepiness scale >10 [16].
Patients with severe lower lung diseases were excluded and the patients who have COPD as an accompanying disease were only mild in severity.
Statistical analysis
Data were expressed as mean ± standard deviation of median (interquartile range) for continuous variables, and in numbers with frequencies (%) for categorical variables. ANOVA, Tukey HSD, chi-squared, and Fisher exact test were used to assess the association between patient factors and respisomnography results. Descriptive of all available variables are given as numbers, percentages whereas results are expressed in terms of means (SD). Statistical correlations were calculated using the Statistical Package for the Social Sciences (SPSS, version 17.5) and p value <0.05 was considered statistically significant.
Results
A total number of 964 patients were recruited in the study. Polysomnographic records of twenty-one patients displayed missing data. There were 684 male (79 %) and 280 female (21 %) patients. Three hundred sixty-seven patients (50.6 %) never smoked. We divided smokers into two groups as current smokers (n = 150, 20.7 %) and former smokers (n = 208, 28.2 %). Former smokers had 26.77 (SD 21.5) PYs of smoking history while active smokers had 29.3 (SD 28.7) PYs. The mean age was 52.07 (SD 11.3). Active smokers had a mean age of 49.53 (SD 10.17) while former smokers and never smokers had a mean age of 51.37 (SD 10.62), 54.20 (SD 11.56), respectively (Fig. 1). The correlation between age and smoking status was found to be statistically significant (p = 0.000).
57.8 % of never smokers, 85.6 % of former smokers and 83.3 % of active smokers were men (Fig. 2). The correlation between smoking and gender was statistically significant (p = 0.000). Furthermore, male patients had more severe OSA than female patients (489 men with moderate or severe OSA vs. 154 women with the same) (p = 0.001). Accompanying diseases like hypertension, diabetes mellitus, coronary heart diseases (others; asthma, COPD, hypothyroidism, etc.), and demographic data are summarized in Table 1.
The mean body mass index was 32.3 (SD 6.4). There was a statistically significant correlation between BMI and smoking status. Never smokers had a mean BMI of 32.78 (SD 6.4), while active smokers had a mean BMI of 31.1 (SD 5.8) (p = 0.021).
There was no significant correlation between smoking status groups (never-former-current smokers) and accompanying diseases, Epworth score, AHI, total sleep time, sleep latans, REM latans, REM %, NREM 1–2 %, NREM 3 %, and minimum O2 saturation. Likewise, there was no significant correlation between OSA severity (mild, moderate, severe) and smoking habits (non-former-current smokers) (p = 0.49) (Fig. 3).
When we combined former and active smokers and compared them with nonsmokers, the age displayed by two groups was statistically significant, 50.6 (SD 10.4), 54.2 (SD 11.9) (p = 0.000). Moreover, total sleep time and sleep efficiency were higher and statistically significant in the group of smokers (328.8 SD 102.7–310.8 SD 105.6 p = 0.021), (83.7 SD 13.5–81.3 SD 13.8 p = 0.02) compared to that of nonsmokers.
Polysomnographic results are summarized in Table 2. Desaturation time during sleep was significantly higher in the group of former smokers compared to never-smokers (73.84 SD 97.1–52 SD 85.8) (p = 0.005).
Mild OSA patients displayed a mean PYs of 5.73 (SD 13.7), moderate 7.03 (SD 20.2), and severe patients 9.91 (SD 19.6) cigarette smoking, respectively (Table 2). If we look at the PYs and OSA severity, as the severity of OSA increases (as the AHI increases), the mean PYs increased significantly (p = 0.01) (Fig. 4).
When we divided the smokers into three groups like mild, moderate, and severe, we found that mild smokers have significantly lower AHI than severe smokers (36.3 vs 44.2 AHI) (p = 0.017). The percentage of NREM 1–2 stages during sleep was significantly lower in the mild smokers group compared to severe smokers (74.5 vs 80 %) (p = 0.007). The percentage of NREM 3 stage was significantly higher in the mild smokers group compared to severe smokers (14 vs 8.3 %) (p < 0.001) (Table 3). However, there was no significant correlation in terms of OSA severity and other parameters when we compared moderate smoking group with mild or severe smoking groups. Also, we separately compared mild former, mild current, moderate former and moderate current, and severe former and severe current smokers groups. There was no statistical significance between these smoking groups and parameters like the following: age, BMI, AHI, Epworth score, and PSG parameters (p < 0.05 for all).
As expected, as the AHI increases, the number of accompanying diseases significantly increased (p = 0.01). As AHI increases, the Epworth score increases (p = 0.001), total sleep time decreases (p = 0.001), REM % decreases (p = 0.001), NREM 1–2 increases (p = 0.001), NREM 3 decreases (p = 0.001), the level of minimum O2 saturation decreases (p = 0.001), and total desaturation time increases (p = 0.001) significantly (Table 2).
Discussion
In this study, we found that active smokers are diagnosed at a younger age than former and never smokers. We observed that male OSA patients smoked more than female OSA patients and male patients had more severe disease. Never smokers had higher BMI than current and former smokers. Desaturation time during sleep was higher in the group of former smokers compared to that of never smokers. The PYs history particularly increased as the AHI increased and severe smokers have higher AHI, higher NREM 1–2 stages, and lower NREM 3 stages.
Some studies have recognized that smoking might have an effect on sleep-related disorders, yet it is difficult to establish an independent effect of smoking on OSA [8–10, 17]. Previous studies have suggested that smoking may be an independent risk factor for habitual snoring [7–10] and that snoring frequency increases with the number of cigarettes smoked or the duration of exposure to smoke [18–20]. However, most studies compare patients’ smoking history with OSA prevalence while the relationship between exposure to smoking and OSA severity has not been meticulously investigated.
Most studies focus on sex, overweight, and upper airway abnormalities as risk factors for snoring and sleep apnea. In a recent study, Franklin et al. found that current smoking, former smoking, and second-hand smoking are all major risk factors for habitual snoring [20]. The snoring frequency increased with the amount of tobacco smoked and with the exposure to second-hand smoking, which further supports the hypothesis that smoking induces snoring.
In a study made by Kim et al., it is suggested that smoking may worsen OSA through exacerbation of the upper airway collapse at the level of the uvula, and that histological changes of the uvular mucosa correlated with smoking might be due to increased CGRP-related neurogenic inflammation [21]. The authors determined that CGRP expression might be stimulated by smoke which results in edema and thickness of the lamina propria in the uvulas of OSA patients. Also, another study demonstrated that nasal resistance was increased in smokers [22]. Indicators of nasal obstruction, which may be related with OSA, can be due to smoking-related chronic mucosal inflammation like thicker epithelium, cellular hyperplasia, mucosal edema, and damaged cilia function [23–25]. Other possible smoking-associated mechanisms such as decreased lung function, an increased rate of respiratory infections, and obstructive airway diseases might further affect breathing during sleep [26, 27].
In a study by Hızlı et al., the authors suggested that in patients with OSA and simple snoring, cigarette smoking was associated with early age disease [28]. Similarly, we also found that compared to former and never smokers, current smokers are of younger age when they are diagnosed with OSA. With more inflammation in the upper airways, these patients may display more symptoms and thus see the clinic at a younger age. Also, apneas during sleep may increase due to the rebound effect of nicotine withdrawal as the nicotine levels continue to decline through the night. Although the impact of nightly nicotine withdrawal does not exist in all smokers, this may be a possible reason for the OSA patients to be more symptomatic.
The prevalence rates of smoking in developed and developing countries are 20–40 % in women, 30–40 % in men and 2–10 % in women, 40–60 % in men, respectively [29]. In Turkey, the prevalence of smoking in women is 24 % and in men is 63 % [29]. Similar to what is described in the literature, we observed that there is a male predomination in smoking. In our study, we showed that male OSA patients smoke more than female OSA patients; furthermore, male patients displayed more severe OSA than female patients. Men, especially in their middle age and later are exposed to an increased risk of developing OSA because of increased mass in torso and neck [30]. Women suffer less frequently and to a lesser degree than men do, to some extent thanks to their physiology, but possibly also due to differential levels of progesterone [31]. Prevalence in post-menopausal women approximates to that of men in the same age range [31]. Our study group had more male patients with more severe OSA.
As expected, active smokers with OSA had less BMI than nonsmokers. Overweight is a well-known risk factor for OSA [17]. Smoking itself can be used for weight control and as it is known that nicotine intake reduces appetite and increases metabolic activity [32].
There was no significant correlation between smoking status groups and OSA severity (AHI), but we showed that there is data on the effect of smoking in patients with OSA. The data was based on the information; the severity of OSA increased (as the AHI increases) whereas the mean PYs significantly increased and mild smokers have lower AHI than severe smokers. Also, we demonstrated that compared to mild smokers, severe smokers have a worse sleep stability in association with an increase in lighter sleep stages. In addition, when we look at the PSG results, desaturation time during sleep was significantly higher in the group of former smokers compared to never smokers. Decreased hypoxia sensitivity, airway inflammation, and the effects of nicotine on airway muscles could be the possible mechanisms for these outcomes. Smoking may be a reason for hypoxia as the chemical irritants in smoke tend to inflame the soft tissue of the upper airway and promote fluid retention, both of which can result in the narrowing of the upper airway [33]. Various studies showed that active smokers were more likely to suffer from longer durations of hypoxia [34, 35]. Smoking can lead to decreased hypoxia sensitivity and potential failure to recover from apnea, which prolongs the durations of apneas with desaturation [36–38]. Additionally, Wetter et al. concluded that smokers have a high prevalence of sleep disturbance [39]. Recent studies also confirmed that active smokers experienced a lower sleep efficiency and lighter sleep stages which might be due to sleep disturbance caused by nightly nicotine withdrawal [40, 41].
In this study, we aimed to establish the correlation between tobacco smoking and the severity of OSA using medical records and polysomnographic results. We found that there was no significant correlation between smoking status groups (never-former-current smokers) and Epworth score as well as AHI. Likewise, no significant correlation was found between OSA severity (mild, moderate, severe) and smoking habits (never-former-current smokers) either. However, active smokers used to have the disease at a younger age with less BMI. Also, desaturation time during sleep was higher in the group of former smokers compared to never smokers, and the PY history particularly increased as the AHI rose. Severe smokers had lighter sleep stages with increased AHI.
References
Guilleminault C, Eldridge FL, Dement WC (1973) Insomnia with sleep apnea: a new syndrome. Science 31:856–858
Whitney CW, Enright PL, Newman AB, Bonekat W, Foley D, Quan SF (1998) Correlates of daytime sleepiness in 4578 elderly persons: the Cardiovascular Health Study. Sleep 21:27–36
Lindberg E, Gislason T (2000) Epidemiology of sleep-related obstructive breathing. Sleep Med Rev 4:411–433
Greenberg GD, Watson RK, Deptula D (1987) Neuropsychological dysfunction in sleep apnea. Sleep 10:254–262
Parati G, Lombardi C, Narkiewicz K (2007) Sleep apnea: epidemiology, pathophysiology, and relation to cardiovascular risk. Am J Physiol Regul Integr Comp Physiol 293:1671–1683
Peled N, Kassirer M, Shitrit D, Kogan Y, Shlomi D, Berliner AS, Kramer MR (2007) The association of OSA with insulin resistance, inflammation and metabolic syndrome. Respir Med 101:1696–1701
Bearpark H, Elliott L, Grunstein R, Cullen S, Schneider H, Althaus W, Sullivan C (1995) Snoring and sleep apnea. A population study in Australian men. Am J Respir Crit Care Med 151:1459–1465
Franklin KA, Gislason T, Omenaas E et al (2004) The influence of active and passive smoking on habitual snoring. Am J Respir Crit Care Med 170:799–803
Lindberg E, Taube A, Janson C, Gislason T, Svardsudd K, Boman G (1998) A 10-year follow-up of snoring in men. Chest 114:1048–1055
Wetter DW, Young TB, Bidwell TR, Badr MS, Palta M (1994) Smoking as a risk factor for sleep-disordered breathing. Arch Intern Med 154:2219–2224
Krishnan V, Dixon-Williams S, Thornton JD (2014) Where there is smoke there is sleep apnea: exploring the relationship between smoking and sleep apnea. Chest 146:1673–1680
Iber C, Ancoli-Israel S, Chesson AL, Quan SF (2007) The AASM manual for the scoring of sleep and associated events: rules, terminology, and technical specifications. Westchester, Ill, USA
The International Classification of Sleep Disorders: Diagnostic and Coding Manual (2005) 2nd edition. Westchester, Ill, USA
Berg S (2008) Obstructive sleep apnea syndrome: current status. Clin Respir J. doi:10.1111/j.1752-699X.2008.00076.x
Punjabi NM (2008) The epidemiology of adult obstructive sleep apnea. Proc Am Thorac Soc. doi:10.1513/pats.200709-155MG
Johns MW (1994) Sleepiness in different situations measured by the Epworth sleepiness scale. Sleep 17:703–710
Bloom JW, Kaltenborn WT, Quan SF (1988) Risk factors in a general population for snoring Importance of cigarette smoking and obesity. Chest 93:678–683
Ekici M, Ekici A, Keles H, Akin A, Karlidag A, Tunckol M, Kocyigit P (2008) Risk factors and correlates of snoring and observed apnea. Sleep Med 9:290–296
Lavie L, Lavie P (2008) Smoking interacts with sleep apnea to increase cardiovascular risk. Sleep Med 9:247–253
Franklin KA, Gislason T, Omenaas E et al (2004) The influence of active and passive smoking on habitual snoring. Am J Respir Crit Care Med 170:799–803
Kim KS, Kim JH, Park SY, Won HR, Lee HJ, Yang HS, Kim HJ (2012) Smoking induces oropharyngeal narrowing and increases the severity of obstructive sleep apnea syndrome. J Clin Sleep Med. doi:10.5664/jcsm.2024
Dessi P, Sambuc R, Moulin G, Ledoray V, Cannoni M (1994) Effect of heavy smoking on nasal resistance. Acta Otolaryngol 114:305–310
Young T, Finn L, Kim H (1997) Nasal obstruction as a risk factor for sleep-disordered breathing. The University Of Wisconsin Sleep and Respiratory Research Group. J Allergy Clin Immunol 99:757–762
Hadar T, Yaniv E, Shvili Y, Koren R, Shvero J (2009) Histopathological changes of the nasal mucosa induced by smoking. Inhal Toxicol 21:1119–1122
Cohen NA, Zhang S, Sharp DB, Tamashiro E, Chen B, Sorscher EJ et al (2009) Cigarette smoke condensate inhibits transepithelial chloride transport and ciliary beat frequency. Laryngoscope 119:2269–2274
Anthonisen NR, Connett JE, Murray RP (2002) Smoking and lung function of Lung Health Study participants after 11 years. Am J Respir Crit Care Med 166:675–679
Arcavi L, Benowitz NL (2004) Cigarette smoking and infection. Arch Intern Med 164:2206–2216
Hızlı Ö, Özcan M, Ünal A (2013) Evaluation of comorbidities in patients with OSAS and simple snoring. Scientific World Journal. doi:10.1155/2013/709292
İtil O (2000) Akciğer kanserlerinin epidemiyolojisi ve etyolojisi. In: Haydaroğlu A (ed) Akciğer kanserleri: Tanı ve tedavi. Ege Üniversitesi Basımevi, İzmir, pp 15–34
Chervin RD, Guilleminault C (1996) Obstructive sleep apnea and related disorders. Neurol Clin 14:583–609
Sahlin C, Franklin KA, Stenlund H, Lindberg E (2009) Sleep in women: normal values for sleep stages and position and the effect of age, obesity, sleep apnea, smoking, alcohol and hypertension. Sleep Med. doi:10.1016/j.sleep.2008.12.008
Hukkanen J, Jacob P, Benowitz NL (2005) Metabolism and disposition kinetics of nicotine. Pharmacol Rev. doi:10.1124/pr.57.1.3
Aksu K, Firat Güven S, Aksu F, Ciftci B, Ulukavak Ciftci T, Aksaray S, Sipit T, Peker Y (2009) Obstructive sleep apnea, cigarette smoking and plasma orexin-A in a sleep clinic cohort. J Int Med Res 37:331–340
Casasola GG, Álvarez-Sala JL, Marqués JA, Sánchez-Alarcos JM, Tashkin DP, Espinos D (2002) Cigarette smoking behavior and respiratory alterations during sleep in a healthy population. Sleep Breath 6:19–24
Conway SG, Roizenblatt SS, Palombini L, Castro LS, Bittencourt LR, Silva RS et al (2008) Effect of smoking habits on sleep. Braz J Med Biol Res 41:722–727
Lewis KW, Bosque EM (1995) Deficient hypoxia awakening response in infants of smoking mothers: possible relationship to sudden infant death syndrome. J Pediatr 127:691–699
Fewell JE, Smith FG (1998) Perinatal nicotine exposure impairs ability of newborn rats to autoresuscitate from apnea during hypoxia. J Appl Physiol 85:2066–2074
Hafström O, Milerad J, Sundell HW (2002) Prenatal nicotine exposure blunts the cardiorespiratory response to hypoxia in lambs. Am J Respir Crit Care Med 166:1544–1549
Wetter DW, Young TB (1994) The relation between cigarette smoking and sleep disturbance. Prev Med 23:328–334
Zhang L, Samet J, Caffo B, Punjabi NM (2006) Cigarette smoking and nocturnal sleep architecture. Am J Epidemiol 164:529–537
Zhang L, Samet J, Caffo B, Bankman I, Punjabi NM (2008) Power spectral analysis of EEG activity during sleep in cigarette smokers. Chest 133:427–432
Conflicts of interest
The authors declared that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Yelda Varol holds a degree in medicine, Dr. Suat Seren Chest Diseases and Chest Surgery Training and Research Hospital.
Ceyda Anar holds a degree in medicine, Dr. Suat Seren Chest Diseases and Chest Surgery Training and Research Hospital.
Ozlem Egemen Tuzel holds a degree in medicine, Dr. Suat Seren Chest Diseases and Chest Surgery Training and Research Hospital.
Salih Zeki Guclu holds a degree in medicine, Dr. Suat Seren Chest Diseases and Chest Surgery Training and Research Hospital.
Zeynep Zeren Ucar holds a degree in medicine, Dr. Suat Seren Chest Diseases and Chest Surgery Training and Research Hospital.
Rights and permissions
About this article
Cite this article
Varol, Y., Anar, C., Tuzel, O.E. et al. The impact of active and former smoking on the severity of obstructive sleep apnea. Sleep Breath 19, 1279–1284 (2015). https://doi.org/10.1007/s11325-015-1159-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-015-1159-1