Abstract
Purpose
The arousal index (AI) quantifies cortical arousal relative to total sleep time and is widely used to determine the severity of sleep fragmentation. It usually includes arousals secondary to respiratory events, limb movements, and spontaneous arousals. No systematic studies have been undertaken to determine AI cutoff in subjects with negative polysomnography.
Methods
Three hundred fifty polysomnograms of subjects ≥18 years of age with no sleep disorders (apnea-hypopnea index (AHI) <5, periodic limb movement index (PLMI) <10, no upper airway resistance syndrome) or minimum oxygen saturation > 90 % and no comorbid health problems were reviewed.
Results
Basic sleep architecture appears within normal range, except for increased stage N2 and decreased stage N3. AI significantly correlated with age (r = 0.7), sleep efficiency (r =−0.16), sleep latency (r = 0.14), rapid eye movement (REM) latency (r = 0.12), stage N1 (r = 0.15), stage N2 (r = 0.12), stage N3 (r = −0.27), AHI (r = 0.24), PLMI (r = 0.18), and nadir oxygen saturation (r = −0.17) [p < 0.05 for all]. A significant correlation was noted between age and sleep efficiency (r = −0.19), REM latency (r = 0.13), stage N1 (r = 0.16), stage N2 (r = 0.21), stage N3 (r = −0.39), and nadir oxygen saturation (r = −0.16) [p < 0.05 for all]. Multiple linear regression analysis showed that age is only the independent predictor of AI (R 2 = 0.70, p < 0.01). The prediction equation for the arousal index in subject with negative polysomnography is AI = 0.276 × age (year) + 8.018.
Conclusions
Age is the most important independent factor in predicting increasing AI in subjects with negative polysomnography.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Arousals are known to reflect a progressive activation from the subcortical to the cortical region [1, 2] and subcortical arousals often consist of autonomic and brainstem arousals, which can occur without any changes in cortical activity [3, 4]. Sleep fragmentation characterized by repetitive short sleep interruptions is one of the recognized determinants of excessive daytime sleepiness [5]. Notwithstanding, the measurement of cortical arousals during sleep is useful in quantifying sleep fragmentation, though numerous variables have been examined to characterize this complex physiology of sleep. Cortical arousal refers to brief abrupt increases in electroencephalographic (EEG) frequency, mostly alpha and beta (excluding spindle), that interrupt the continuity of the sleep state background with or without accompanied increases in chin electromyographic (EMG) activities. The arousal index (AI) quantifies cortical arousal relative to total sleep time and is widely used to determine the severity of sleep fragmentation. The arousal index usually includes arousals secondary to respiratory events, limb movements, and spontaneous arousals. Each of these arousals can be classified by changes in EEG frequency, EMG amplitude, and/or the presence of limb movements. New measurements to quantify sleep fragmentation have been developed, including other measures of EEG activity (e.g., cyclic alternating pattern (CAP)) [6–8] and measures of autonomic activity (e.g., pulse transit time (PTT) or peripheral arterial tonometry (PAT)) [9–12]. However, the American Academy of Sleep Medicine (formerly, the American Sleep Disorders Association (ASDA)) 3-s rule is still the most widely used definition of arousal in the majority of sleep laboratory [13, 14] and scoring EEG arousal is thus far the best validated approach for quantifying sleep fragmentation, with relatively high reliability and validity [7, 14]. In addition, the significance of autonomic arousals that are not associated with EEG arousals in contributing to daytime impairment is uncertain and studies have not shown that autonomic arousals without EEG arousals are predictive of daytime sleepiness [10, 13, 15]. Studies in human have reported, in correlation with increasing cortical arousals, increased objective and subjective sleepiness [5, 16–18], decreased psychomotor performance [16–18], changes in hormone secretion patterns [19], decreased upper airway function [20], increased whole body metabolic rate [21], and increased sensory arousal thresholds [22, 23], as compared to baseline. It is therefore very important to quantify cortical arousals accurately and identify the norms of arousal index in polysomnogram (PSG).
Age-dependent alterations in sleep architecture include a decrease in total sleep time, reduced sleep efficiency, and decreased percentage of slow wave sleep and rapid eye movement (REM) sleep [24, 25]. Regarding a correlation between aging and arousals, there has been minimal evidence indicating that the number of brief arousals, like other metrics of sleep quantity, was influenced by increasing age [25–28]. In those studies, however, sleep was recorded from normal and sleep-related breathing disorders subjects [25, 27, 28] or respiratory events were measured by limited procedure (i.e., no nasal pressure transducer or abdominal effort detector) [26].
We therefore hypothesized that sleep-related cortical arousals in apparently normal subjects, as indicated by negative polysomnography and absent coexisting sleep disorders, will increase with increasing age. The second purpose was to identify the other factors influencing sleep-related cortical arousals and to identify the norms of sleep-related cortical arousals in those subjects. Accordingly, this study was undertaken to evaluate the correlation between sleep-related cortical arousals and age and to identify the norms of age-dependent sleep-related cortical arousals.
Methods
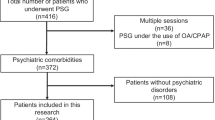
The clinical interview, sleep questionnaire, and polysomnographic raw data of 12,719 patients who attended at Cleveland Clinic Sleep Disorders Center, Ohio, from July 2005 to October 2008 were reviewed. Given that the studies performed before 2007 were scored according to previous PSG criteria, all chosen polysomnograms of candidates satisfying the inclusion and exclusion criteria were then rescored to see if they satisfied the American Academy of Sleep Medicine (AASM) scoring criteria 2007. All polysomnograms were performed using a standard procedure, including video recording, left and right electrooculogram (EOG), central and occipital electroencephalogram (EEG), mental and submental electromyogram (EMG), left and right anterior tibialis EMG, single electrocardiogram (ECG) waveform, snoring, continuous airflow with thermistor, nasal pressure transducer, chest and abdominal effort, and oxygen saturation with pulse plethysmography. Sleep stages were scored according to standard AASM 2007 criteria [29] on 30-s epoch, as follows: wakefulness and sleep stage non-rapid eye movement (NREM) 1, 2, and 3&4 (stages N1, N2, and N3, respectively) and REM sleep. Cortical arousal in this study was scored using the criteria proposed by ASDA [13]. Arousal was identified as an abrupt shift in EEG frequency, which may include theta, alpha, and/or frequencies greater than 16 Hz, but not spindle. Ten seconds of continuous sleep must have preceded the arousal and the arousal must last ≥3 s and must have been accompanied by an increase in chin EMG if it occurred during REM sleep.
We limited this study to subjects who met the following criteria:
-
(1)
Age ≥18 years;
-
(2)
Apnea-hypopnea index (AHI) <5/h (apnea was defined as airflow cessation for more than 10 s and hypopnea was defined as nasal pressure signal excursions (or those of the alternative hypopnea sensor) that drop by ≥50 % of baseline and the duration of this drop lasted at least 10 s and was associated with a decrease in oxygen saturation of at least 3 % or followed by an arousal);
-
(3)
Periodic limb movement index <10/h;
-
(4)
Adequate polysomnogram as determined by total sleep time more than 6.5 h and a sleep efficiency of ≥65 %;
-
(5)
Minimum oxygen saturation >90 % (The oximetry data was visually reviewed to identify its association with an acceptable plethysmographic signal. All SpO2 values were calculated only sleep to decrease the impact of wake after sleep onset (WASO) on oxygen saturation);
-
(6)
Absence of cardiopulmonary, neurological, and psychiatric disorders;
-
(7)
Absence of previously diagnosed sleep disorders identified by clinical interview or sleep questionnaire; and
-
(8)
Absence of findings suggestive of upper airway resistance syndrome (UARS) as determined by respiratory disturbance index (RDI) greater than 5/h. (RDI is similar to the AHI. However, RDI also includes respiratory events that do not technically meet the definitions of apneas or hypopneas but do disrupt sleep. This is also referred to as respiratory effort related arousal (RERA). For this study, RERA was defined as either snoring-related arousal, crescendo-related arousal, or inspiratory flow limitation-related arousal).
Clinical interviews were reviewed and subjects were excluded if they described current use of sedatives, hypnotic, or other medications known to cause sleep disturbance; the use of alcohol (>7 drinks/week); or illicit drug abuse. Positive airway pressure (PAP) titration studies, including split and full night studies, were also excluded. Candidates with other comorbidities that resulted in sleep disturbance or sleep fragmentation, such as cardiopulmonary, neurological, pain syndrome, and other medical and psychiatric disorders, were also excluded. Subjects diagnosed with any sleep disorders after the initial PSG, at any time before the study enrollment, were also excluded from the study. The clinical or office interviews and sleep questionnaires, including available investigations, were reviewed for these purposes.
According to these inclusion and exclusion criteria, 361 subjects were selected from our database and their PSGs were rescored using AASM 2007 scoring criteria. All scoring was performed by one of our three readers (authors) and then systematically reviewed. After rescoring, 350 subjects were included into statistical analysis. This study was approved by the Institutional Review Board (IRB) at the Cleveland Clinic, Cleveland, Ohio, USA.
Data on the following variables were collected: age, gender, body mass index (BMI), past medical history, Epworth Sleepiness Scale (ESS) scores, sleep efficiency, sleep and REM latencies, sleep stage distribution, arousal index, AHI, RDI, periodic limb movement index (PLMI), periodic limb movement arousal index (PLMAI), and nadir oxygen saturation.
Data analysis
Data analysis was performed using SPSS version 11.5 and JMP version 6.1. Sample size was estimated at 336, based on previous data, a power of 0.9, and alpha of 0.05 [25–28]. Database characteristics with normal distribution were summarized and expressed as mean but otherwise as median or ratio (%). To determine whether the distributions of all continuous data were normal, a Kolmogorov-Smironov test was performed. Pearson correlation was used to analyze the correlation between arousal index and various continuous variables and between aging and various continuous variables. Otherwise, one-way ANOVA with post hoc or contrast test was used. Across different age groups, overall differences between macro-structural parameters, number of arousals, and arousal indices were analyzed by one-way ANOVA. Multiple linear regression analyses were performed to evaluate the contribution of each basic demographic and sleep variable to models predicting the arousal index. Collinearity among the variables in the regression model was measured by means of tolerance and the variance inflation factor (VIF). Statistical significance was set at p < 0.05.
Results
A total of 364 subjects matched the inclusion and exclusion criteria for this study and were then rescored using AASM 2007 criteria. Fourteen rescored subjects were excluded because they no longer met the inclusion and exclusion criteria. Thus, a total of 350 subjects remained for final analysis. Demographic data and polysomnographic variables are shown in Table 1. The indication for performing PSG included snoring (340/350, 97.14 %), witnessed apneas (211/350, 60.29 %), excessive daytime sleepiness (289/350, 82.57 %), daytime fatigue (339/350, 96.86 %), and recurrent awakenings from sleep or maintenance insomnia (299/350, 85.43 %). The majority had more than one indication (342/350, 97.71 %).
As noted in Table 1, these individuals had no apparent obstructive sleep apnea and no increased periodic limb movement. The overall sleep architecture appeared relatively normal with only slightly decreased slow wave sleep and slightly prolonged sleep and REM sleep onset latency. There was no significant difference between the number of men and women (p > 0.005). These individuals also had relatively high average BMI in the upper normal limits (29.97 ± 8.26). Subjects spent 81.2 % of sleep time in the supine position. In the morning questionnaires, all subjects reported the quality and quantity of the previous night’s sleep as satisfactory and similar to their habitual sleep at home.
The arousal index was significantly predicted by age (p < 0.001), ESS (p < 0.05), sleep efficiency (p < 0.05), sleep and REM sleep onset latencies (p < 0.05), NREM sleep (p < 0.05), AHI (p < 0.001), RDI (p < 0.001), PLMI and PLMAI (p < 0.001), and finally nadir oxygen saturation (p < 0.01) [Table 2]. There was no statistically significant difference between the arousal index of men compared with that of women (p = 0.213). In addition and as shown in Table 3, we found a significant association between age and sleep efficiency (p < 0.001), REM latency (p < 0.05), NREM sleep (p < 0.05), AHI (p < 0.05), RDI (p < 0.05), arousal index (p < 0.001), PLMAI (p < 0.05), and nadir oxygen saturation (p < 0.01). The correlation between age and ESS was nearly statistically significant (p = 0.05). Nevertheless, increasing age was found to be the most important predictor of arousal index after controlling of contributing factors by means of the multiple linear regression analysis (Table 4 and Fig. 1). Further, the equation predicting increasing arousal index can be calculated by using the regression formula as follow: arousal index (/h) = 0.276 × age (year) + 8.018.
Correlation between arousal index and aging in “negative polysomnography individuals.” The figure showed that arousal index significantly linearly correlates with increasing age [n = 350; R 2 = 0.4534, p < 0.001] as described by scatter plot with regression lines. The equation predicting arousal index (Y-axis) using age (X-axis) is as shown: Y = 0.276X + 8.018
Considering individuals in different age groups, post hoc tests revealed that the arousal index was significantly lower in those 59 years or younger, as compared with older individuals (Table 5 and Fig. 2). No gender-related differences in terms of arousal index were detected across all age groups (p > 0.05).
Discussion
In this study, we used the database of standardized PSG, sleep questionnaire, and clinical interview. Only one night PSG was included for analysis. This results in some limitations resulting from the first night effect and different PSG criteria used for scoring the study before and after 2007. To reduce these limitations, we rescored the study again using AASM 2007 scoring criteria and, fortunately, the data revealed only minor first night effect on PSG results (very slightly delayed sleep and REM onsets, as well as slightly decreased slow wave sleep). Night-to-night variability in terms of macro and microstructure of sleep might be the case, even though the effect on the arousal index should be small. Sleep deprivation prior to the day of PSG (which can influence the arousal index) was also not controlled.
On the morning questionnaires, all subjects reported their night’s sleep as satisfactory and similar to their habitual sleep at home. Subjects sound somewhat nearly obese (BMI, 29.97 ± 8.26); none, however, were ever diagnosed with any sleep disorders. Pediatrics subjects (age <18 years) were not included in this study; thus, our findings could not be generalized to those age groups. We also followed up all included subjects to make sure that none were diagnosed with any sleep disorders prior to the completion of this research manuscript. The findings in this study should thus be generalizable to “healthy” adults. In this study, we did not measure respiratory effort in order to diagnose UARS, which may limit the validity of UARS diagnosis. In addition, arousals related to sleep position changes were not analyzed. These issues may limit the validity of the study conclusion. Additionally, the visual scoring of cortical arousal as used in this study corresponded to complete arousals, which included both cortical and autonomic activation. Thus, the arousal reactions that included autonomic, but no cortical changes (the so-called subcortical arousal), that could not be visually scored in this study might have led to a different outcome. However, scoring EEG arousal based on AASM 2007 scoring criteria is, to date, the best validated approach, with relatively high reliability and validity in quantifying sleep fragmentation [7, 14].
The change in sleep architecture with aging, including sleep efficiency, REM sleep onset latency, NREM sleep distribution, respiratory and leg movement events, and nadir oxygen saturation is somewhat similar to the previous studies [24–28]. The most prominent changes include reduction in sleep stage 3&4 and increased arousal index. Gender has been found to account for differences in sleep measures [25], but this study did not undertake to verify this difference; thus, the effect of gender on sleep architecture could not be determined. However, in subgroup analysis, the effect of gender on arousal index in different age groups was statistically insignificant.
Based on our review of the literature, this is the first large study to explore the effect of aging on increasing arousal index in negative polysomnography individuals who have never been diagnosed with any sleep disorders using standard full channel PSG. The effect of aging on increasing arousal index has been widely described. Redline et al. [25] published data from the Sleep Heart Health Study (SHHS) and revealed that the mean (±SD) significantly, although relatively small, increase with age, ranging from 16 (±8.2) for the age 37–54 years old group to 18.4 (±10) for the 55–61 years old group, to 20.3 (±10.5) for the 62–70 years old group, and to 21 (±11.6) for those older than 70 years. However, the study included subjects with sleep-related breathing disorders and revealed that RDI was by far the single most powerful predictor of increasing cortical arousals. Boselli et al. [26] reported the distribution of EEG arousals quantified under limited PSG recording (no air flow or respiratory effort detection) in normal sleepers (no ESS data) of different age groups (10–19, 20–39, 40–59, and ≥60 years) and they found an evolution with age of arousal frequency during total sleep time (r = 0.852, p < 0.001). Mathur et al. [27] reported a positive correlation between age and cortical EEG arousals. However, sleep studies were recorded form a total of 55 subjects, including both normal subjects and subjects with sleep-related breathing disorders. Given that total sleep time (TST) varies across age groups, Boselli et al. [26] found that the increase of arousal index/TST was mainly charged to NREM sleep, especially in sleep stages 1 and 2, rather than to REM sleep. Recently, a large cohort study from Brazil revealed that, in the general population (both men and women), a large effect size was observed for the age-related increase in arousal index and WASO; however, the increase in the arousal index was mainly due to respiratory-related arousals [28].
Unlike previous studies in which limited PSGs were mostly used, few subjects were involved, and SBD patients were included, our study included adequate number of subjects and none of these had any sleep, medical, or psychiatric disorders that could have potentially influenced the arousal index and sleep architecture. Although all of the subjects were symptomatic at the time the polysomnogram was being performed, none of them had been diagnosed with any sleep disorders at the time of enrollment. In unadjusted analyses, the arousal index was influenced by age, ESS, sleep efficiency, sleep and REM sleep onset latency, NREM sleep, AHI, RDI, PLMI and PLMAI, as well as nadir oxygen saturation. However, after adjusting and controlling for ESS, sleep efficiency, sleep and REM sleep onset latency, NREM sleep, AHI, RDI, PLMI and PLMAI, as well as nadir oxygen saturation, we found age to be the most significant influence on arousal index in negative polysomnography individuals. We were also able to formulate an equation that can calculate the norms for arousal index for different age groups in “negative polysomnography” adults (age >18 years), as follows: Arousal index (/h) = 0.276 × age (year) + 8.018.
In conclusion, this study demonstrated the significant effect of age on sleep architecture and arousal index, as identified in the literatures. However, this study included a large number of subjects and none of these had any sleep, medical, or psychiatric disorders. Normal aging increases the number of EEG arousals throughout sleep, after controlling for the other contributing factors. An equation predicting the norms for cortical EEG arousals for “negative polysomnography” or “apparently healthy” adults (age >18 years) is also disclosed for consideration and review. However, determining a cutoff may not be the ideal way to measure norms for arousal indices. Measuring norms by ranging or including autonomic arousals should be determined significant.
Abbreviations
- OSAS:
-
Obstructive sleep apnea syndrome
- EDS:
-
Excessive daytime sleepiness
- ESS:
-
Epworth Sleepiness Scale
- TST:
-
Total sleep time
- PSG:
-
Polysomnogram
- AHI:
-
Apnea-hypopnea index
- RDI:
-
Respiratory disturbance index
- AI:
-
Arousal index
- PLMI:
-
Periodic limbs movements index
- PLMAI:
-
Periodic limbs movements arousal index
- BMI:
-
Body mass index
- CPAP:
-
Continuous positive airway pressure
- REM:
-
Rapid eye movement
- SPSS:
-
Statistical Package for the Social Sciences
- EOG:
-
Electrooculogram
- EMG:
-
Electromyogram
- ECG:
-
Electrocardiography
- SpO2:
-
Pulse oxygen saturation
- WASO:
-
Wake after sleep onset
- ASDA:
-
American Sleep Disorders Association
References
Lijowska AS, Reed NW, Chiodini BAM, Thach BT (1997) Sequential arousal and airway-defensive behavior of infants in asphyxial sleep environments. J Appl Physiol 83:219–228
McNamara F, Wulbrand H, Thach BT (1998) Characteristics of the infant arousal response. J Appl Physiol 85:2314–2321
Rees K, Spence DPS, Earis JE, Calverley PMA (1995) Arousal responses from apneic events during non-rapid-eye-movement sleep. Am J Respir Crit Care Med 152:1016–1021
Davies RJO, Belt PJ, Roberts SJ, Ali NJ, Stradling JR (1993) Arterial blood pressure responses to graded transient arousal from sleep in normal humans. J Appl Physiol 74:1123–1130
Stepanski E, Lamphere J, Badia P, Zorick F, Roth T (1984) Sleep fragmentation and daytime sleepiness. Sleep 7:18–26
Terzano M, Mancia D, Salati M et al (1985) The cyclic alternating pattern as a physiologic component of normal NREM sleep. Sleep 8:137–145
Parrino L, Smerieri A, Rossi M et al (2001) Relationship of slow and rapid EEG components of CAP to ASDA arousals in normal sleep. Sleep 24:881–885
Terzano M, Parrino L, Smerieri A et al (2002) Atlas, rules, and recording techniques for the scoring of cyclic alternating pattern (CAP) in human sleep. Sleep Med 3:187–199
Pillar G, Bar A, Shlitner A, Schnall R, Shefy J, Lavie P (2002) Autonomic arousal index: an automated detection based on peripheral arterial tonometry. Sleep 25:541–547
Pitson DJ, Stradling JR (1998) Autonomic markers of arousal during sleep in patients undergoing investigation for obstructive sleep apnoea, their relationship to EEG arousals, respiratory events and subjective sleepiness. J Sleep Res 7:53–59
Poyares D, Guilleminault C, Rosa A et al (2002) Arousal, EEG spectral power and pulse transit time in UARS and mild OSAS subjects. Clin Neurophysiol 113:1598–1606
Pitson D, Chhina N, Knijn S et al (1994) Changes in pulse transit time and pulse rate as markers of arousal from sleep in normal subjects. Clin Sci (Lond) 87:269–273
Bonnet M, Carley D, Carskadon M et al (1992) EEG arousals: scoring rules and examples: a preliminary report from the sleep disorders atlas task force of the American Sleep Disorders Association. Sleep 15:173–184
Bonnet MH, Doghramji K, Roehrs T et al (2007) The scoring of arousal in sleep: reliability, validity, and alternatives. J Clin Sleep Med 3:133–145
Stradling JR, Barbour C, Glennon J et al (2000) Prevalence of sleepiness and its relation to autonomic evidence of arousals and increased inspiratory effort in a community based population of men and women. J Sleep Res 9:381–388
Stepanski E, Lamphere J, Roehrs T et al (1987) Experimental sleep fragmentation in normal subjects. Int J Neurosci 33:207–214
Bonnet MH (1986) Performance and sleepiness following moderate sleep disruption and slow wave sleep deprivation. Physiol Behav 37:915–918
Bonnet MH (1986) Performance and sleepiness as a function of frequency and placement of sleep disruption. Psychophysiology 23:263–271
Spath-Schwalbe E, Gofferje M, Kern W et al (1991) Sleep disruption alters nocturnal ACTH and cortisol secretory patterns. Biol Psychiatry 29:575–584
Brooks D, Horner RL, Kimoff RJ et al (1997) Effect of obstructive sleep apnea versus sleep fragmentation on responses to airway occlusion. Am J Respir Crit Care Med 155:1609–1617
Bonnet MH, Berry RB, Arand DL (1991) Metabolism during normal, fragmented, and recovery sleep. J Appl Physiol 71:1112–1118
Bonnet MH (1985) Effect of sleep disruption on sleep, performance, and mood. Sleep 8:11–19
Bonnet MH (1987) Sleep restoration as a function of periodic awakening, movement, or electroencephalographic change. Sleep 10:364–373
Bliwise DL (1993) Sleep in normal aging and dementia. Sleep 16:40–81
Redline S, Kirchner HL, Quan SF et al (2004) The effects of age, sex, ethnicity, and sleep-disordered breathing on sleep architecture. Arch Intern Med 164:406–418
Boselli M, Parrino L, Smerieri A, Terz MG (1998) Effect of age on EEG arousals in normal sleep. Sleep 361–367
Mathur R, Douglas NJ (1995) Frequency of EEG arousals from nocturnal sleep in normal subjects. Sleep 18:330–333
Moraes W, Piovezan R, Poyares D, Bittencourt LR, Santos-Silva R, Tufik S (2014) Effects of aging on sleep structure throughout adulthood: a population-based study. Sleep Med 15:401–409
Iber C, Ancoli-Israel S, Chesson A, Quan SF, American Academy of Sleep Medicine (2007) The AASM manual for the scoring of sleep and associated events: rules, terminology, and technical specification, 1st edn. Westchester, Illinois
Acknowledgments
The authors gratefully acknowledge the contribution of Dr. Nancy Foldvary-Schaefer and Kingman P. Strohl for their thoughtful review and comments of the manuscript and Nengah Hariadi and Zahreddin Alsheikhtaha for technical support.
Conflict of interest
The authors declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jaimchariyatam, N., Rodriguez, C.L. & Budur, K. Sleep-related cortical arousals in adult subjects with negative polysomnography. Sleep Breath 19, 989–996 (2015). https://doi.org/10.1007/s11325-014-1090-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-014-1090-x