Abstract
Purpose
To determine whether sleep and sleep disordered breathing (SDB) contribute to the neuropsychological deficits of patients with Down syndrome, and whether treatment of SDB results in improvement in cognitive function.
Methods
In this cohort study, 25 children with Down syndrome underwent overnight polysomnography (PSG), Multiple Sleep Latency Testing (MSLT), and a battery of neuropsychological tests. Patients with SDB underwent a follow up PSG after treatment. All patients repeated the neuropsychological tests 13 months later.
Results
At baseline, there was no relationship between SDB and performance on the neuropsychological tests. However, total sleep time and sleep latency were related to tests of cognitive ability (p < 0.05) and comprehension (p < 0.01). The amount of time in slow-wave sleep correlated with tests of achievement (p < 0.01), and adaptive behavior (p < 0.01). Ten patients had SDB confirmed on PSG. Five of these patients were treated successfully with adenotonsillectomy and/or continuous positive airway pressure. The five who did not tolerate treatment were deficient in tests of adaptive behavior (Vineland p < 0.05) visual–motor integration (Beery p < 0.01) and achievement (Woodcock–Johnson p < 0.05) compared to those successfully treated. After treatment the patients improved in ratings of attention (Conners p < 0.05).
Conclusions
Although SDB is common in children with Down syndrome, it is not a major contributor to their cognitive deficits. Cognitive function is related to the amount of sleep and particularly slow wave sleep. Successful treatment of SDB may improve their attention.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Children with Down syndrome (DS) have many features that may predispose them for obstructive sleep apnea (OSA), including hypotonia, mandibular hypoplasia, glossoptosis, obesity and a relatively small upper airway [1–4]. The prevalence of OSA in children with DS has been reported to be between 22 % and 79 %, depending on patient selection criteria, definitions, and methodology [3, 5–8]. OSA may contribute to pulmonary hypertension in patients with DS [9, 10], defects in cognitive function in obese children [11], and behavior problems in children with DS or adenotonsillar enlargement [12]. Since patients with OSA can have impaired cognitive function as a result of sleep fragmentation [13] and/or hypoxia [14], we hypothesized that at least a portion of the neuropsychological deficits in patients with DS may be due to OSA. Furthermore, since patients with OSA can show improvement in cognitive function following treatment [15], we hypothesized that effective treatment of their sleep disorders might result in improved neuropsychological function in patients with DS.
To determine whether sleep disorders adversely impact their daytime cognitive function, 26 patients with DS had their sleep architecture and cardiopulmonary function assessed by full overnight polysomnography (PSG) followed by a five-nap multiple sleep latency test (MSLT) to quantitate sleepiness, and a battery of neuropsychological tests. Patients in whom a sleep disorder was diagnosed returned for the full battery of tests after the condition was corrected to assess any improvement in sleep architecture, cardiopulmonary function, and cognitive function. We expected to find greater cognitive impairment in patients with poorer sleep, particularly those in whom a sleep disorder was diagnosed. Additionally, we hypothesized that cognitive function would improve in sleep-disordered patients following successful treatment.
Methods
Subjects were recruited through the ARC/Edward I. and Fannie L. Baker International Resource Center for Down syndrome, and by word of mouth. Patients were invited “to participate in a study of sleeping patterns of patients with Down syndrome” but no mention was made of snoring or OSA, in an attempt to minimize selection bias. Patients and/or their parent or guardian gave written informed consent to the study, as approved by the Institutional Review Board. All patients underwent baseline PSG, MSLT, and neuropsychological testing. Patients in whom a sleep disorder was diagnosed repeated all tests approximately 1 year after treatment was initiated. Patients without sleep disorders repeated the neuropsychological tests only.
Polysomnography
Patients reported to the sleep laboratory for PSG about 1 h before their usual bedtime. Sixteen parameters were recorded. Six electroencephalographic leads (bilateral frontal, central, and occipital), bilateral electro-oculographic leads, and submental electromyographic leads were applied. These surface leads were used to measure the stages of sleep, including time spent in rapid eye movement sleep. Motion of the chest wall and abdomen were measured by respiratory inductance plethysmography (Respitrace; Ambulatory Monitoring Inc., Ardsley, NY, USA). Airflow from the nose and mouth were measured with thermocouples. Oxyhemoglobin saturation was measured by pulse oximetry (N-200; Nellcor Inc., Hayward, CA, USA). Body motions were recorded with pretibial electromyographic leads. Cardiac rhythm was monitored with standard electrocardiographic leads. All signals were recorded by an 18-channel recorder (Model 78D; Grass Instruments, Quincy, MA, USA). The patient and the recording were viewed using split screen technology to allow simultaneous review of physical and electrophysiological findings. The children were allowed to sleep as long as they wanted; the longest recording time was 600 min.
Sleep staging was scored by standard criteria [16] by a trained technologist who was unaware of the purpose of the study. The scoring was reviewed by one of the authors (LJB), who is an experienced and accredited polysomnographer. Sleep efficiency, sleep latency, and the number and duration of arousals and awakenings were calculated.
Central apnea was defined as a 10-s period without airflow or respiratory effort. Obstructive apnea was defined as a cessation of airflow for at least 10 s with paradoxical respiratory effort. Shorter events were scored if they resulted in arousal or oxyhemoglobin desaturation of at least 4 %. Obstructive hypopnea was defined as a reduction but not complete cessation of airflow with paradoxical chest wall and abdominal motion, resulting in arousal or oxyhemoglobin desaturation of at least 4 %. Central hypopnea was defined as a reduction but not complete cessation of airflow despite synchronous chest wall and abdominal motion, resulting in either arousal or oxyhemoglobin desaturation of at least 4 %.
The type, number, and duration of respiratory events were noted, as well as the median (Sat 50) and minimal (low sat) oxyhemoglobin saturation. The apnea hypopnea index (AHI) was calculated as the average number of respiratory events per hour of sleep.
Multiple sleep latency test
The Multiple Sleep Latency Test (MLST) was administered as a gold standard, objective assessment for daytime sleepiness. The sleep latency (time to sleep onset) and REM latency were recorded for each nap period according to standard criteria [16, 17] and the mean sleep latency for the five-nap periods was calculated.
Neuropsychological tests
Standardized measures of neuropsychological abilities and academic achievement were administered in the sleep lab at the time of both baseline sleep testing and follow-up testing (Table 1). The parent(s) was interviewed to obtain background medical history and information on adaptive behavior performance. The parent(s) and teacher (when available) also completed questionnaires on the child’s behavior and performance at home and school (Table 1). Standardized scores and Z scores were used in analysis. For certain tests (Vineland Adaptive Behavior Scales, Developmental Test of Visual–Motor Integration and Woodcock–Johnson Tests of Achievement—Revised), an age-adjusted score was computed. To calculate this score, the age equivalent score for the test was subtracted from the chronological age at the time of testing [18]. The age-adjusted score assessed the extent to which the child’s performance fell below age expectations. This provided a more sensitive assessment of variation in performance at the bottom end of the normative range and in this manner minimized “floor effects” in test scores.
Statistical analysis
Anthropometric variables were compared using the group t-test and chi-square (Fisher exact) test. Relationships between baseline sleep and neuropsychological variables were assessed using stepwise multiple regression and one way analysis of variance (ANOVA). The difference between sleep and neuropsychological variables at baseline and follow-up was assessed with paired t-tests and repeated measures ANOVA. A p value <0.05 was considered statistically significant.
Results
Twenty-six patients volunteered for the study. One patient presented with a markedly reduced height and weight. He was found to be hypothyroid and was treated with thyroid replacement therapy. The data from this individual were excluded from analyses, leaving a total of 25 subjects. There were 14 males and 11 females, ranging in age from 7.2 to 18.7 years (Table 2).
Baseline
Fourteen patients (56 %) were reported to snore “often or always.” Eleven patients (44 %) had apneas observed by a parent. In 15 patients (60 %), daytime somnolence such as falling asleep in school or during activities was reported.
Nineteen of 25 patients had an AHI >1.5, and ten (40 %) had OSA diagnosed on PSG, defined for the purposes of this study as an AHI of 5 or greater. There were no differences in parental reports of snoring, witnessed apneas, or daytime somnolence between the patients who did and did not have OSA. By definition the patients with OSA had more frequent respiratory events on PSG, resulting in more severe oxyhemoglobin desaturation (Table 2). They had more fragmented sleep, with more frequent arousals and awakenings. Thirty percent of patients with OSA and 20 % of patients without OSA had a body mass index (BMI) >25. Sixty percent of patients with OSA and 53 % of patients without OSA had a BMI Z score >1.5. There were no differences in the age, weight, height or BMI between the patients who did and did not have OSA, although there was a preponderance of females in the OSA group (Fisher exact test, p < 0.005). Both groups had low percent REM sleep, as has been previously described in children with intellectual disability [19].
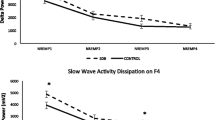
The subjects’ cognitive function, as measured by the Stanford–Binet, was related to sleep (total sleep time, measured by PSG), and sleepiness (measured by sleep latency on the MSLT). Adaptive behavior (Vineland) and achievement (Woodcock–Johnson) were predicted primarily by minutes of slow wave (Stage N3) sleep (Table 3). Stepwise multiple regression revealed no independent associations of sleep disordered breathing (SDB) (AHI, low sat, sat 50) with any of the neuropsychological tests, and there was no difference in any of the neuropsychological tests between the patients who did and did not have OSA.
To summarize the baseline findings:
-
1.
Clinical findings did not predict the presence of sleep apnea.
-
2.
There was no difference in any of the neuropsychological tests between the children who did and did not have OSA.
-
3.
Cardiorespiratory parameters measured on the PSG were not associated with neuropsychological function; rather, measures of the quantity and quality of sleep, particularly slow-wave sleep were better predictors of neuropsychological function.
Treatment
Five of the ten patients with OSA had had adenotonsillectomies in the past; in these children, there was no tonsillar tissue visible on inspection, but we did not perform endoscopy or lateral neck roentgenograms to assess for adenoid regrowth. Nasal continuous positive airway pressure (CPAP) was initiated in these patients, as well as in two other patients who preferred a nonsurgical approach. The remaining three patients had adenotonsillectomies. All ten patients had follow-up PSG a mean of 17.9 months after their initial study (range 9–26 months). Treatment was successful in normalizing the PSG and improving clinical symptoms of snoring and daytime sleepiness (by parental report) in five of these patients (three CPAP, two adenotonsillectomy). Four patients were unable to use CPAP in the home despite successful titration in the laboratory. A fifth patient did not improve sufficiently following adenotonsillectomy, but was unable to properly use CPAP at home. Thus, five of ten patients with OSA received effective treatment. CPAP was successful in three of seven patients, and adenotonsillectomy was successful in two of three.
There were no differences at baseline in any anthropometric, sleep, or cardiopulmonary parameters between the patients with OSA who were successfully treated and those who were not, except that the unsuccessfully treated group had less sleep (363.8 ± 82.8 SD vs. 436.8 ± 20.9 min, ANOVA p < 0.05) with poorer sleep efficiency (70.4 ± 18.8 % vs. 86.6 ± 6.2 %, p < 0.05). However, these differences were solely due to a single individual who had only 224 min of sleep and 37 % sleep efficiency.
At baseline, the patients with OSA in whom treatment was subsequently unsuccessful were deficient relative to those successfully treated in tests of adaptive behavior (Vineland Adaptive Behavior Composite, p < 0.05), visual–motor integration (Beery, p < 01), and achievement (Woodcock–Johnson, Applied Problems, p < 0.05; and Dictation, <0.05).
Five of the 15 patients with normal PSG’s were subsequently started on methylphenidate and/or clonidine by their private physicians because of the physician’s clinical impression of hyperactivity. When compared to the ten other patients with normal PSG, the patients who received medications had some deficiencies in cognitive function (Stanford–Binet Quantitative, p < 0.05), and were rated as more hyperactive (Conners hyperactivity scale, p < 0.01).
Follow-up
Follow-up testing was performed a mean of 13.3 ± 6.6 months after the initial assessment. All of the patients with OSA in whom treatment was successful showed a lower AHI and higher oxyhemoglobin saturation after treatment. In this group, the lowest oxyhemoglobin saturation rose from a mean ± SD of 80.6 ± 6.3 to 90.2 ± 3.0 (p < 0.05) and the mean AHI dropped from 17.8 ± 14.6 to 3.0 ± 2.4 (p < 0.05). There was no significant change in any sleep parameters after treatment.
Although comparisons can only be considered exploratory in view of the limited sample, patients who were successfully treated for OSA showed greater improvement in attention (Conners Hyperactivity Index p < 0.05) than did the other patients (paired t-test). In contrast, the patients who received methylphenidate did not show any consistent improvement in their attention when compared to the other patients.
Discussion
Although we were unable to demonstrate a relationship between cardiorespiratory parameters and neuropsychological function, the improvement in attention following successful treatment of OSA underscores the importance of recognizing and treating OSA to insure children may reach their full potential. Indeed, the American Academy of Pediatrics recommends routine screening for OSA in children with DS [20]. A new and important finding is the relationship between cognitive function and sleep parameters, including total sleep time and amount of slow-wave sleep, in children with DS. These results provide important new information not only for physicians and nurses, but also for educators and psychologists involved in assessment and educational management of children with DS.
Many studies have shown a relationship between SDB and neuropsychological function. Snoring and sleep-associated gas exchange abnormalities have been associated with poorer academic performance in otherwise normal children [21, 22]. Cognitive function, memory, and learning are impaired in adults with snoring, OSA and hypoxemia [14, 23–28]. Frequent respiratory pauses have been shown to affect cognitive function in obese children and adults [11, 23, 27]. There was no relationship between SDB and neuropsychological function in our cohort of children with DS. Rather, we found a relationship between sleep architecture and cognitive function. The Woodcock–Johnson and Vineland tests, which measure acquired knowledge and abilities, were most closely correlated with the amount of SWS. We also found sleep time and latency to be associated with the Stanford–Binet. As a test of cognitive functioning, the Stanford–Binet may be more sensitive to the temporary state of wakefulness, and therefore is more closely related to TST and sleep latency than adaptive behavior as assessed by the Vineland.
Our patients differed from previous reports of children with OSA in several important aspects. Our patients all had poor baseline neuropsychological function secondary to DS, which might have overshadowed subtle differences in function between the patients with and without OSA. Our patients also had milder OSA than previous reports describing adults with OSA who had as many as 46–48 respiratory events per hour of sleep with oxyhemoglobin desaturations to 67 % [25, 26]. It is possible that more frequent and more severe respiratory events would lead to more severe cognitive defects. Even so, our patients with OSA did improve in ratings of attention following successful treatment, consistent with previous reports in normal adults [15, 29]. The mean age of our patients was 10 years, and it is possible that earlier identification and treatment of sleep-disordered breathing may have a greater effect on neuropsychological function. However, our numbers are very small. Future studies might include a large population of DS patients with severe OSA studied before and after effective treatment.
We attempted to minimize self-selection by avoiding mention of snoring, breathing, or apnea in recruiting materials. However, it is possible that patients who volunteered for the study were perceived by their parents to have sleep disorders, and therefore 40 % may overestimate the prevalence of OSA in this population. Nevertheless, this prevalence is comparable to other studies that estimated the prevalence of SDB in children with DS to be 22–79 % [3, 5–8]. The prevalence of OSAS may be even higher in adults with DS, with abnormal PSG in up to 94 % of patients [30].
Despite the high prevalence of OSA in our patients, neither AHI nor oxyhemoglobin desaturation were related to neuropsychological function. Since respiratory events can influence sleep architecture, it is important to analyze these data using a stepwise regression to examine the effects of one variable controlling for another. This method treats AHI as a continuous variable, rendering the choice of a “cutoff” for the presence of OSA moot.
We thoroughly evaluated both quality and quantity of sleep using both full nocturnal PSG as well as MSLT. Sleep, particularly time spent in SWS (stage 3), was the major correlate of neuropsychological function in our patients. Our study tested many more comparisons than would normally be permitted by the limited number of subjects and all conclusions merit confirmation in subsequent studies. However, previous studies have been consistent with our results, also showing a relationship between cognitive function and the amount, but not the percent, of time spent in SWS [15, 16]. This suggests that a certain amount of SWS, considered to be “restorative sleep,” may be necessary to maximize neuropsychological function. This is supported by animal studies that indicate learning is impaired when SWS is disrupted [31]. A recent review [32] of studies of sleep and learning in children suggest that SWS plays a major role in memory consolidation and learning, particularly during early development. However, it is also possible that the amount of SWS is merely an index of brain integrity, rather than a direct contributor to neuropsychological function. Overall, the evidence supports the role of SWS in memory processing and its importance before learning, to prepare the brain for initial memory encoding, and after learning, for the offline consolidation of new memories. The precise mechanisms by which sleep mediates learning and memory processing remain to be fully elucidated. Further studies are necessary to confirm these findings in a normal population and in different age groups.
Five of the patients, all with OSA, had previously undergone adenotonsillectomy. This is consistent with other reports documenting the difficulty in treating OSA in children with DS. Adenotonsillectomy is reported to be effective in 13–50 % of the patients [3, 33–35] prompting some authors to suggest more invasive pharyngopalatal surgery [34]. Two of the three patients in our study who had an adenotonsillectomy after OSA had been confirmed by PSG had a normal PSG on follow-up. In comparison, four of the seven patients we started on CPAP were unable to continue using it in the home, despite the best efforts of the family, including positive reinforcement with stickers and rewards. This is in contrast to our overall success rate of over 75 % for long term CPAP use in children [36, 37]. The patients who were unable to tolerate CPAP in the home had poorer adaptive behavior, visual–motor integration and achievement than did the patients who did well with CPAP. It is possible that inattention is a barrier to CPAP adherence, or that untreated OSA contributes to inattentiveness. It is important to recognize that this is a cohort study and cannot prove cause and effect. Although further research is needed to examine this issue, the clinician may consider evaluation and treatment of any attention deficit disorders in children with difficulty tolerating CPAP in the home.
These data was acquired before the publication of pediatric scoring guidelines by the American Academy of Sleep Medicine [38]. However, similar scoring criteria have been successfully used in many other studies and we feel that these minor differences are unlikely to alter the overall findings of our study. We chose an AHI of 5 as a conservative cutoff for treatment since these are children who had volunteered for a research study rather than presenting to a clinician for treatment, wherein an AHI >1.5 is often considered abnormal. We also did not monitor esophageal pressure which may mean that some respiratory-effort related arousals were missed. However, we used respiratory inductance plethysmography to assess chest and abdominal efforts and carefully inspected the tracings, which has been shown to have reasonable agreement with the gold-standard esophageal manometry [39] without subjecting the children to an uncomfortable esophageal probe that may have altered sleep architecture.
In summary, we confirm that OSA is common in patients with DS, but the presence of OSA does not markedly affect their neuropsychological function. Rather, the quality and quantity of sleep, particularly the quantity of slow-wave sleep, is a strong predictor of adaptive behavior and academic achievement. Cognitive ability is better predicted by measures of total sleep and sleepiness. Successful treatment for sleep disorders, including OSA, may improve neuropsychological function in children with DS. CPAP is a useful therapy for OSA when adenotonsillectomy is unsuccessful or not indicated, but children with attention defects may have more difficulty adjusting to their CPAP at home. We speculate that therapy for their attention deficits may improve compliance with CPAP.
Abbreviations
- CPAP:
-
Continuous positive airway pressure
- ECG:
-
Electrocardiogram
- EOG:
-
Electrooculogram
- EEG:
-
Electroencephalogram
- EMG:
-
Electromyogram
- MSLT:
-
Multiple Sleep Latency Test
- OSA:
-
Obstructive sleep apnea
- PSG:
-
Polysomnography
- REM:
-
Rapid eye movement
- SWS:
-
Slow wave sleep
- SDB:
-
Sleep disordered breathing
- AHI:
-
Apnea hypopnea index
- DS:
-
Down syndrome
References
Jones KL (1997) Smith’s recognizable patterns of human malformation. WB Saunders, Philadelphia, pp 8–13
Silverman M (1988) Airway obstruction and sleep disruption in Down’s syndrome. Br Med J 296:1618–1619
Marcus CL, Keens TG, Baustista DB, von Pechmann WS, Ward SLD (1991) Obstructive sleep apnea in children with Down syndrome. Pediatrics 88:132–139
Uong EC, McDonough JM, Tayag-Kier CE, Zhao H, Haselgrove J, Mahboubi S, Schwab RJ, Pack AI, Arens R (2001) Magnetic resonance imaging of the upper airway in children with Down syndrome. Am J Respir Crit Care Med 163:731–736
Stebbens VA, Dennis J, Samuels MP, Croft CB, Southall DP (1991) Sleep related upper airway obstruction in a cohort with Down’s syndrome. Arch Dis Child 66:1333–1338
Dyken ME, Lin-Dyken DC, Poulton S, Zimmerman MB, Sedars BS (2003) Prospective polysomnographic analysis of obstructive sleep apnea in Down syndrome. Arch Pediatr Adolesc Med 157:655–660
Ng DK, Hui HN, Chan CH, Kwok KL, Chow PY, Cheung JM, Leung SY (2006) Obstructive sleep apnea in children with Down syndrome. Singap Med J 47:774–779
Shott SR, Amin R, Chini B, Heubi C, Hotze S, Akers R (2006) Should all children with Down syndrome be tested? Ach Otolaryngol Head Neck Surg 132:432–436
Loughlin GM, Wynee JW, Victorica BE (1981) Sleep apnea as a possible cause of pulmonary hypertension in Down syndrome. J Pediatr 98:435–437
Rowland TW, Nordstrom LG, Bean MS, Burkhardt H (1981) Chronic upper airway obstruction and pulmonary hypertension in Down’s syndrome. Am J Dis Child 135:1050–1052
Rhodes SK, Shimoda KC, Waid LJ, O’Neil PM, Oexmann MJ, Collop NA, Willi SM (1995) Neurocognitive defects in morbidly obese children with obstructive sleep apnea. J Pediatr 127:741–744
Carskadon MA, Pueschel SM, Millman RP (1993) Sleep disordered breathing and behavior in three risk groups: preliminary findings from parental reports. Childs Nerv Syst 9:452–457
Bonnet MH (1993) Cognitive effects of sleep and sleep fragmentation. Sleep 16:565–567
Roehrs T, Merrion M, Pedrosi B, Stepanski E, Zorick F, Roth T (1995) Neuropsychological function in obstructive sleep apnea syndrome (OSAS) compared to chronic obstructive pulmonary disease (COPD). Sleep 18:382–388
Engleman HM, Martin SE, Deary IJ, Douglas NJ (1994) Effect of continuous positive airway pressure treatment on daytime function in sleep apnea/hypopnea syndrome. Lancet 343:572–575
Rechtschaffen A, Kales A (eds) (1968) A manual of standardized terminology, techniques and scoring system for sleep stages of human subjects. Brain Information Service, Los Angeles
Carskadon MA, Dement WC, Mitler MM, Roth T, Westbrook PR, Keenan S (1986) Guidelines for the Multiple Sleep Latency Test (MSLT): a standard measure of sleepiness. Sleep 9:519–524
Baron IS, Fennel EB, Voeller KS (1995) Pediatric neuropsychology in the medical setting. Oxford University Press, New York
Miano S, Bruni O, Elia M et al (2008) Sleep phenotypes of intellectual disability: a polysomnographic evaluation in subjects with Down syndrome and Fragile-X syndrome. Clin Neurophysiol 119:1242–1247
Bull MJ (2011) Health supervision for children with Down syndrome. Pediatrics. doi:10.1542/peds.2011-1605
Gozal D (1998) Sleep-disordered breathing and school performance in children. Pediatrics 102:616–620
Gozal D, Pope DW (2001) Snoring during early childhood and academic performance at ages thirteen to fourteen years. Pediatrics 107:1394–1399
Greenberg GD, Watson RK, Deputla D (1987) Neuropsychological dysfunction in sleep apnea. Sleep 10:25–262
Cheshire K, Engleman H, Deary I, Shapiro C, Douglas NJ (1992) Factors impairing daytime performance in patients with sleep apnea/hypopnea syndrome. Arch Intern Med 152:538–541
Findley LG, Barth JT, Powers DC, Wilhoit SC, Boyd DG, Suratt PM (1986) Cognitive function in patients with obstructive sleep apnea and associated hypoxemia. Chest 90:686–690
Telakivi T, Kajaste S, Partinen M, Koskenvuo M, Salmi T, Kaprio J (1988) Cognitive function in middle-aged snorers and controls: role of excessive daytime somnolence and sleep-related hypoxic events. Sleep 11:454–462
Decary A, Rouleau I, Montplaisir J (2000) Cognitive deficits associated with sleep apnea syndrome: a proposed neuropsychological test battery. Sleep 23:369–381
Bucks RS, Olaithe M, Eastwood P (2013) Neurocognitive function in obstructive sleep apnoea: a meta-review. Respirology 18:61–70
Derderian SS, Bridenbaugh RH, Rajagopal KR (1988) Neuropsychological symptoms in obstructive sleep apnea improve after treatment with nasal continuous positive airway pressure. Chest 94:1023–1027
Trois MS, Capone GT, Lutz JM, Melendres MC, Schwartz AR, Collop NA et al (2009) Obstructive sleep apnea in adults with Down syndrome. J Clin Sleep Med 5:317–323
Hars B, Hennevin E (1987) Impairment of learning by cueing during postlearning slow-wave sleep in rats. Neurosci Lett 79:290–294
Wilhelm I, Prehn-Kristensen A, Born J (2012) Sleep-dependent memory consolidation—what can be learnt from children? Neurosci Biobehav Rev 36:1718–1728
Suen JS, Arnold JE, Brooks LJ (1995) Adenotonsillectomy for treatment of obstructive sleep apnea in children. Arch Otolaryngol Head Neck Surg 121:525–530
Strome M (1986) Obstructive sleep apnea in Down syndrome children: a surgical approach. Laryngoscope 96:1340–1342
Southall DP, Stebbens VA, Mirza R, Lang MH, Croft CB, Shinebourne EA (1987) Upper airway obstruction with hypoxaemia and sleep disruption in Down syndrome. Dev Med Child Neurol 29:734–742
Brooks LJ, Sleeper G (1991) Use of nasal CPAP by children in the home. J Sleep Res 20:212
Brooks LJ, Crooks RL, Sleeper GP (1992) Compliance with nasal CPAP by children with obstructive sleep apnea. Am Rev Respir Dis 145:A556
The AASM manual for the scoring of sleep and associated events: rules, terminology and technical specification (2007) Iber C (ed) American Academy of Sleep Medicine
Loube DI, Andrada T, Howard RS (1999) Accuracy of respiratory inductance plethysmography for the diagnosis of upper airway resistance syndrome. Chest 115:1333–1337
Thorndike RL, Hagen EP, Sattler JM (1986) The Stanford–Binet intelligence scale, 4th edn. Riverside Publishing Company, Rolling Meadows
Gardner R (1979) The objective diagnosis of minimal dysfunction. Creative Therapies, Cresskill
Beery KE (1989) Revised administration, scoring, and teaching manual for the Developmental Test of Visual–Motor Integration. Modern Curriculum Press, Cleveland
Woodcock R, Mather N (1989) Woodcock–Johnson tests of achievement—revised: standard and supplemental batteries. DLM Teaching Resources, Allen TX
Achenback T (1991) Manual for the child behavior checklist. Department of Psychiatry, University of Vermont, Burlington
Achenbach T (1991) Manual for the teacher report form. Department of Psychiatry, University of Vermont, Burlington
Barkley RA (1990) Attention deficit hyperactivity disorder: a handbook for diagnosis and treatment. Gilford Press, New York
Sparrow SS, Balla DA, Cicchetti DV (1984) Vineland Adaptive Behavior Scales. American Guidance Service, Circle Pines
Acknowledgements
This work was funded by a grant from the American Lung Association of Ohio.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Brooks, L.J., Olsen, M.N., Bacevice, A.M. et al. Relationship between sleep, sleep apnea, and neuropsychological function in children with Down syndrome. Sleep Breath 19, 197–204 (2015). https://doi.org/10.1007/s11325-014-0992-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-014-0992-y