Abstract
Urine is often sampled from patients participating in clinical and metabolomic studies. Biological homeostasis occurs in humans, but little is known about the variability of metabolites found in urine. It is important to define the inter- and intra-individual metabolite variance within a normal population before scientific or clinical conclusions are made regarding different pathophysiologies. This study investigates the variability of selected urine metabolites in a group of 60 healthy men and women over a period of 30 days. To monitor individual variation, 6 women from the normal population were randomly selected and followed for 30 days. To determine the influence of extraneous environmental factors urine was collected from 25 guinea pigs with similar genetics, diet, and living environment. For both studies, 24 metabolites were identified and quantified using high-resolution 1H nuclear magnetic resonance spectroscopy (NMR). The data demonstrated large inter and intra-individual variation in metabolite concentrations in both normal human and control animal populations. A defined normal baseline is essential before any conclusions may be drawn regarding changes in urine metabolite concentrations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
The human body is a complex and dynamic array of interacting metabolic pathways. These complex chemical reactions are generally kept in balance in a healthy individual; otherwise the slightest metabolic deviation can produce devastating results (Kraut and Kurtz 2005; Trachtenbarg 2005). It is believed that tight control over the metabolic profile of an individual, referred to as homeostasis, is required to maintain health.
Whether a primary cause, or a secondary indicator, metabolite changes have long been observed in diseased individuals (Shockcor and Holmes 2002; Kubitz et al. 2005; Green et al. 2002; Bollard et al. 2005; Moolenaar et al. 2003). Metabolomic studies attempt to detect, monitor, and in some cases predict the metabolic response to an insult or disease state (Weckwerth 2003). These studies include investigations of single-celled organisms, plants, animals, tissues, organs, and human subjects (Rastall et al. 2005; Keller et al. 2005; Singer 2005; Tate et al. 2001; Coen et al. 2005; Duarte et al. 2005; Stanley et al. 2005). Some metabolomic studies attempt to understand specific metabolic pathways and processes, while other studies have attempted to diagnose a particular disease (Kraut and Kurtz 2005; Trachtenbarg 2005; Sabatine et al. 2005; Wennergren 2000; Brindle et al. 2002; van Rhijn et al. 2005; de Jongste 2000). Therefore, such metabolic conclusions rely heavily upon having a well-defined healthy group with well-characterized metabolite homeostasis.
In relation to the metabolic pathway being investigated, it is important to consider what type of biological sample is appropriate. Biological samples usually range from highly invasive and specific (i.e., tissue biopsy), to more general biological samples that are easy to collect and noninvasive for human patients (i.e., urine). Urine is often used as a biological fluid for investigation due to its ease of collection, repeated samples, the rich metabolite composition, and the often-higher metabolite concentrations achieved relative to blood plasma. An array of analytical techniques have been used in metabolomic studies including different types of mass spectrometry, high performance liquid chromatography, and nuclear magnetic resonance spectroscopy (NMR)(Dunn et al. 2005; Lindon et al. 2004; Chadha et al. 2001; Aspevall et al. 2001; Assadi 2002). These techniques are further enhanced by multiple methods of data analysis, ranging from metabolite quantification to multivariate statistical analysis (Ekins et al. 2005; Crockford et al. 2005; Cavaluzzi et al. 2002; Somorjai et al. 2004).
High-resolution NMR (most often 1H-NMR) has emerged as a promising non-invasive technique for metabolomic studies due to its ability to simultaneously detect a large number of compounds in a rapid and high-throughput manner that requires little sample manipulation. The lack of invasive mechanical or chemical sample modification for NMR is important because it allows the samples to be analyzed, stored, and re-analyzed if methods improve at a later date. In addition, the data collected (spectra) may be analyzed by several techniques, including spectral integration, principal components analysis (PCA), partial least squares (PLS), and neural networks (Stoyanova and Brown 2001; Sardari and Sardari 2002; Gavaghan et al. 2002).
Currently, there is limited information available regarding normal metabolite concentrations and degrees of variance found in urine (Zuppi et al. 1997; Keun et al. 2002; Geigy 1981–1992). Due to limitations in laboratory resources most studies have tested samples from 10–30 patients, with a control or normal group of at least similar size. This limitation in the number of samples is compounded in human studies where subject compliance may be poor (Chung et al. 2005). Although reference to Geigy scientific tables is common, the information is based upon limited research with similarly small sample sizes (Geigy 1981–1992).
Many Phase I clinical or methodological studies recruit healthy volunteers based upon the absence of medical co-morbidities. The metabolite measurements of the normal cohort are then pooled and used for comparison with test subjects (usually those with a defined disease, i.e., diabetes). A certain degree of homeostasis is assumed to occur in the excretion of metabolites in normal urine; however, it is extremely important to define the inter- and intra-individual metabolite variance within the control group before conclusions are made regarding metabolite changes in diseased individuals. This definition of the normal metabolic profile is fundamental in human studies where additional variance is introduced through a number of uncontrolled factors (i.e., genetics, ethnicity, stress, exercise level, and diet) (Bollard et al. 2005; Lenz et al. 2004). The primary goal of this study was to investigate the degree of inter- and intra-subject metabolite variance in a group of normal healthy human subjects using 1H-NMR analysis of urine to provide a normal human urine metabolic baseline necessary for future metabolomic and clinical studies to build upon. For comparison, 25 guinea pigs of the same strain, gender, diet, and environment were also analyzed to investigate the influence of extraneous factors on urine metabolite excretion often observed in human clinical investigations.
2 Materials and methods
2.1 Human control sample collection
Informed consent was obtained from healthy normal volunteers (30 male, 30 female) in accordance with guidelines established by the University of Alberta Health Research Ethics Board. The study attempted to sample a representative cohort of normal or ‘relatively’ healthy control individuals. Each volunteer was accepted based upon a physician’s opinion that no chronic or major illness was present. For the normal population, each individual collected daily mid-stream urine samples after waking (early AM), and again mid-afternoon; sample collection continued for 30 days.
2.2 Human sample handling
The urine samples were treated with sodium azide (Sigma Aldrich) to a final concentration of 2.5 mM immediately following collection and stored at −10°C for periods <1-week. Samples were catalogued and stored at the Canadian National High Field NMR Centre (NANUC) at −80°C. To obtain a general understanding of inter-individual metabolite variation within a ‘normal’ group, 1 day of morning urine was randomly selected, for a total of 57 samples (30 male and 27 female). To determine intra-individual variation, 6 female subjects were randomly chosen and their morning urine samples were analyzed over the 30-day period. As a result of subject compliance to regular sample collection the female subjects (randomly numbered 1–6) had differing numbers of total samples over the 30 days (21, 24, 29, 30, 29, and 29 samples respectively). To investigate metabolite differences as a result of gender, 1 day was randomly chosen and the morning and afternoon urine samples from the female and male subjects were analyzed (total of 55 female, and 60 male samples from 1 day). Differences in urine metabolites due to time of sampling was investigated by using the same day selected for the ‘gender analysis’, and comparing the morning and afternoon urine samples from the male and female subjects (27 female morning and 28 female afternoon samples from 1 day; 30 male samples from both morning and afternoon collections from 1 day).
2.3 Guinea pig control sample collection
Urine samples were taken from 25 female Dunkin-Hartley guinea pigs (pathogen-free, 180–450 g, Charles River Laboratories). All animals were shipped in filtered crates and kept in high-efficiency, particulate-filtered air. Animals were allowed an acclimatization period in the facility of at least 1 week. All animals were fed a standard guinea pig diet (Prolab; Agway) including water ad libitum. Animals were handled in accordance with the Canadian Council on Animal Care guidelines. The Health Sciences Animal Policy and Welfare Committee, University of Alberta approved ethics for the use of the animals. The guinea pigs were anesthetized intraperitoneally with urethane (1.5 g/kg). Adequate depth of anesthesia was assessed via the pedal reflex. Urine samples were collected by trans-abdominal cystocentesis using a sterile 21-gauge needle. The needle was inserted at a 45° angle, on the midline, midway between the umbilicus and brim of the pelvis, while creating negative pressure by pulling back on the plunger of the syringe. If urine was not obtained with the first puncture, two additional punctures were attempted from 0.2 cm to 1.0 cm cranial or caudal to the initial puncture site. The needle was changed before making each attempt to avoid contamination. Previous work in our laboratory has shown the importance of urine preservation and sterile techniques when working with urine (Saude and Sykes 2007). Therefore, we chose to collect urine in a sterile manner by cystocentesis rather than by the use of metabolic cages or alternative collection methods. Urine samples (1.0–2.0 ml) were stored at −80°C for later 1H-NMR analysis.
2.4 Sample preparation
Urine samples were thawed in a biosafety fume hood and a 630 μl aliquot was removed and placed in a 1.5 ml Eppendorff tube followed by the addition of 70 μl of a reference buffer solution ((4.9 mM DSS (disodium-2, 2-dimethyl 2-silapentane-5-sulphonate) and 100 mM imidazole in D2O) Chenomx, Edmonton, AB). Each sample was then brought to a pH of 6.8 ± 0.1 using HCl and NaOH. An aliquot of 600 μl was taken and transferred to a standard 5 mm glass NMR tube (Wilmad, NJ, USA).
2.5 NMR analysis
All 1H-NMR spectra were acquired on a 600 MHz Inova (Varian Inc, Palo Alto, Ca.) spectrometer equipped with a 5 mm triple-resonance (HCN) probe with Z-axis gradient coil. One-dimensional 1H-NMR spectra were collected at 25°C with a tnnoesy pulse sequence (one-dimensional, three pulse NOESY, with a transmitter pre-saturation delay of 900 ms for water suppression during the pre-acquisition delay and 100 ms mixing time), and a spectral width of 7,200 Hz. The time-domain data points were 64 k complex points, acquisition time was 4 s, the 90° pulse was 6.8 μs, repetition time was 5 s, four steady state scans, and the number of acquired scans was 32. The data was apodized with an exponential window function corresponding to a line broadening of 0.5 Hz, zero-filled to 128 k complex points, and Fourier transformed (Kumar et al. 1980).
2.6 NMR quantification
The methyl singlet of the buffer constituent DSS served as internal standard for chemical shifts (set to 0 ppm), and for quantification. Spectral identification and quantification of 24 clearly identifiable metabolites was performed using the Chenomx NMR Suite Professional software package version 3.1 (database available at pH 7.0, Chenomx Inc., Edmonton, AB, Canada). Figure 1 shows the expanded aromatic (7.2–8.3 ppm) and aliphatic regions (3.3–4.7 ppm) of a 1D 1H-NMR spectrum of a typical human urine sample together with the spectral regions and resonant peaks of a reference sample of pure hippuric acid. For qualitative and quantitative analysis, Chenomx NMR Suite software takes a database of pure compounds (metabolites) and compares the spectral signatures to those found in the urine spectrum. A least-squares fit of the reference spectra to the urine spectra was used to quantify selected metabolites. The internal DSS signal is utilized as the concentration reference (0.49 mM). Work in our laboratory has demonstrated that this procedure provides absolute concentration accuracies in excess of 90% (Saude et al. 2006).
Expanded aromatic (6.7–8.7 ppm) and aliphatic (3.3–4.7 ppm) regions of a 600 MHz 1D 1H-NMR spectrum of healthy human urine (top). The bottom trace shows the reference spectrum of hippurate used by the Chenomx NMR Suite software for qualitative identification and quantitative determination for the metabolite hippurate
Metabolite concentrations were expressed as absolute values, and as ratios relative to creatinine to correct for dilution, assuming a constant rate of creatinine excretion for each urine sample. Following normalization of metabolite concentrations, a large degree of metabolite variability remained. Scaling the normalized metabolite concentrations according to the approximate population average concentration of creatinine (for the human samples:
and for the guinea pig samples:
returned metabolite values of a similar scale to the raw metabolite concentrations which allowed for graphical comparison to determine the remaining degree of metabolite variability. This scaling does not alter the metabolite variability (i.e., coefficients of variation remain constant), but does allow for graphical overlay of raw and normalized metabolite concentrations to determine if the degree of metabolite variability is reduced following dilution correction with creatinine.
2.7 Statistical analysis
Metabolite concentration and normalized results are expressed as means, ranges, and coefficients of variation ( \( {\text{(standard deviation/mean) }} \times {\text{ 100)}} \)). Differences between variables and sub-groups were investigated using Box–Cox transformation of normalized metabolite values followed by one-way analysis of variance (ANOVA). A P-value of <0.05 was considered to indicate statistical significance.
3 Results and discussion
The results from this study have important implications for those interested in examining urine for future metabolomic research. First, prior to describing a diseased state and the unique metabolic differences associated with the pathophysiology, it is important to define a ‘normal, or control population’. Often studies compare different test or disease subjects to a normal cohort of a similar sample size. The difficulty is that the limited sample size, particularly when dealing with human clinical studies, can influence the conclusions of the study. Moreover, without examining trends and variation over time, single comparisons of control values may generate misleading results.
3.1 Human demographics
In this study, questions may be raised regarding the sampled population, and the philosophical definition of a “healthy, or normal human population”. Our inclusion criteria rested upon a physician’s judgment that every subject had no underlying chronic illness or major medical problem, and a general understanding that the subject was ‘healthy’. We intentionally avoided choosing ‘idealized’ normal subjects, as this would not represent an actual ‘normal’ population (i.e., a complete absence of pharmaceuticals, or varsity athletes). No attempt was made to normalize diet, or other factors, in order to best determine the actual variation present in normal individuals. Any additional attempt to regulate extraneous factors like sleep or exercise would falsely skew results towards an unattainable clinical scenario. Most previously published metabolomic and clinical studies that compare disease and control cohorts have not insisted upon a regimented ‘control’ group with regulated sleep, diet, exercise, and stress. Therefore, our study samples a more inclusive normal population that better reflects the majority of human control subjects. Urine samples were collected from 30 women with a mean age of 41.3 (±16, range: 18–68), and 30 men with a mean age of 39.6 (±14, range: 20–74).
3.2 Metabolite identification
The 24 metabolites chosen for this study were all major metabolites found in urine and were unequivocally identified and quantified with concentrations ranging from 0.01 mM to 10.00 mM. The mean metabolite concentrations, standard deviation, range, and coefficient of variation for our normal population are listed in Table 1. The variability of metabolites in the urine were analyzed as group means, coefficients of variance, and in terms of intra-subject variance over time.
A key finding of this study was that the variance (standard deviation and coefficient of variation) of the pooled metabolite concentrations within the normal population was high, as was the degree of variation of metabolites for individuals over time. It is clear that individual metabolite profiles, as sampled in the urine, are capable of impressive variation and a clearer understanding of metabolite variability within control human subjects is needed in future metabolomic and clinical investigations.
3.3 Normalization to creatinine
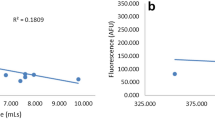
Absolute urine metabolite concentrations are affected by urine volume, which can be correlated with the amount of liquid taken in by the diet. The compound creatinine is easily identified in the urine, is correlated to overall body size (related to muscle mass), and in present literature is said to have little metabolic or excretory variance in healthy individuals. As a result, creatinine is often used to compensate for variations in urine volume, and metabolite concentrations are commonly expressed as ratios relative to creatinine (Zuppi et al. 1997). The variation of creatinine concentrations in 57 urine samples (30 male and 27 female, morning samples) from our cohort of normal subjects is shown in Fig. 2. The mean and standard deviation (9.034 ± 4.37 mM) demonstrates that there is substantial variation of the absolute creatinine concentration in our normal adult cohort.
Absolute creatinine concentrations of 57 healthy human subject urine samples from a single day (27 female, 30 male), and the morning sampling time (9.034 ± 4.37 mM). This sampling was randomly selected from a large dataset of serial samples collected from our normal population of 30 men and 30 women
Variation in urine volume as a result of dietary liquid intake has a direct effect on absolute metabolite concentrations. Previously, volume effects have been normalized by expressing metabolite concentrations as ratios relative to the endogenous creatinine levels for each urine sample. Creatinine is associated with overall muscle mass and body size and current literature states that creatinine exhibits little concentration variability related to normal biological function. Clinically, serum creatinine is often used as an indicator of kidney function. Therefore, it is reasonable to assume creatinine offers the best possible internal standard for correcting urine volume effects. From Table 1 we find that the standard deviations and coefficients of variation for absolute and normalized (Eq. 1) metabolite concentrations in the human control group are similar. Therefore volume effect (subject hydration) is not the major contributing factor to the observed variance in metabolite concentrations. The observed large coefficients of variation (i.e., up to 270 for the metabolite lactate) for normalized metabolite concentrations within our normal population is of interest because studies often attempt to diagnose pathological metabolic profiles based upon limited population information (i.e., small sample size). Our data shows that large variance in urinary metabolite concentrations in the normal human group is not due to urine volume effects, but rather reflects actual metabolite variance. Adequate knowledge and understanding of the variance of urinary metabolite concentrations in the normal human population is necessary for the interpretation of future metabolomic studies.
3.4 Inter-individual variability
To determine the effect of urine volume on metabolite concentration variance and the proper method of reporting metabolite concentrations, two clearly identifiable metabolites (hippurate and citrate) were chosen from the set of 24 metabolites. Absolute hippurate concentrations for normal subjects are shown graphically in Fig. 3A, (mean: 1.825 ± 1.24 mM). The normalized hippurate concentrations following individual standardization to creatinine (Eq. 1) are shown in Fig. 3B, (mean: 2.275 ± 1.43).
Urine hippurate concentrations for the normal human population (57 urine samples from a single day, morning sampling time, 30 male and 27 female) prior to (1.825 ± 1.24 mM, A), and following normalization to creatinine (see Eq. 1, 2.275 ± 1.43, B)
This analysis was repeated for the metabolite citrate (Fig. 4), whereby means for the absolute and scaled concentrations were 2.535 ± 1.81 mM, and 3.054 ± 1.98, respectively. The analysis of all 24 chosen metabolites revealed similarly large standard deviations and coefficients of variation for both absolute and scaled concentrations within our adult normal cohort (Table 1).
Citrate levels in the urine for the normal human population (57 urine samples from a single day, morning sampling time, 30 male and 27 female) prior to (2.535 ± 1.81 mM, A), and following normalization to creatinine (see Eq. 1, 3.054 ± 1.98, B)
3.5 Gender
Within the 30-day collection period a single day was randomly selected for analysis of gender differences in urinary metabolite secretion. Morning and afternoon urine samples were included for the male and female subjects (total of 55 samples for the female, and 60 samples for the male). Following Box–Cox transformation of the concentrations for the 24 metabolites identified in the normal urine, the following 12 metabolites were found to be statistically different (P < 0.05) for male versus female subjects: 2-hydroxyisobutyrate, 4-aminohippurate, aspartate, citrate, creatine, formate, hippurate, histidine, lactate, threonine, trans-aconitate, and N-methylhistidine.
Additional comparisons, such as the influence of age or BMI, within this large dataset of normal urine samples are possible, but these will be reported in following articles (Slupsky et al. 2007).
3.6 Sampling time
The same random day of urine collection selected for the analysis of gender differences was used to determine differences in urine metabolite concentrations as a result of urine collection time. Our studies also chose to look at sampling time because of the infrequency of collection observed in actual clinical settings. Although the morning sample is typically sought, there are many instances where this is not possible. Therefore it is important to determine if there is any urinary metabolite variation that results from differences in the timing of sample collection. Male and female morning urine samples for the day (57 samples) were included as the ‘morning urine samples’, as were the male and female afternoon urine collections (58 urine samples). Following Box–Cox transformation of the metabolite concentrations, the following nine metabolites were found to be statistically different (P < 0.05): 4-aminohippurate, aspartate, creatine, formate, glutamate, phenylalanine, salicylurate, tryptophan, and trans-aconitate.
Of the 24 metabolites examined during this study, the concentrations of nine were statistically different between morning and afternoon urine collection. Thus, differences in metabolite excretion should be noted during metabolic studies using urine as the biofluid. Urine metabolite variability has been seen in earlier metabolomic studies; such as public health and exposure limits to certain agents (Symanski and Greeson 2002). The metabolite variability observed in our human study is similar to that found in studies by Tate (Tate et al. 2001) and Holmes (Holmes et al. 2000).
3.7 Inter-individual variability
From the initial 57 subjects in our randomly selected normal population, 6 female subjects were randomly chosen and 10 unequivocally identifiable metabolites were followed over a 4-week period using morning voids only. Metabolite concentrations were normalized to creatinine levels according to Eq. 1 (see Methods section). Longitudinal values, the mean, and the coefficient of variance for six randomly selected normalized metabolites are shown in Table 2. Morning citrate concentrations for six normal female subjects over a 4-week period are shown in Fig. 5. The data demonstrates that normalized citrate concentrations for each individual remains relatively stable for periods of time; however, during other periods of time vary by over 1–2 times the female cohort standard deviation. Morning tyrosine normalized concentrations for the same 6 female subjects over the same 4-week period are shown in Fig. 6. In contrast, individual tyrosine variation for each individual female is ≤1 cohort standard deviation, except for one aberrant spike for female #2.
It is possible that the large population variance may be due to inter-subject variance (differences in individual mean values) due to gender, age, or diet, while each individual maintains a tight biological homeostasis. From 6 random healthy female volunteers 10 metabolites were monitored over a 4-week period. The data showed that individual citrate and tyrosine levels are capable of ranging through the full standard deviation of the entire population. Similar degrees of variability were observed for the other metabolites (Table 2, and similarly for the normal cohort, Table 1). This study clearly indicates that a single individual is capable of varying greatly over periods of time, and is able to span the same metabolite range as that for an entire group.
When we followed the 6 individual subjects over the 30-day period, some metabolite ‘spikes’ were observed in particular subjects (Figs. 5 and 6). We found no correlation with the changes in metabolite concentrations and changes in the subjects’ daily routine. However, female #1 had an increase in citrate excretion immediately before the beginning of her menstruation cycle. Although this only occurred for the one subject, it may point to an area requiring further investigation (Bollard et al. 2001).
3.8 Guinea pig variability
To investigate the possible influences of extraneous factors on the human population, urine metabolite concentrations and variability (i.e., genetics, diet, stress, environment, etc.) 25 guinea pigs were raised in a controlled sterile environment, fed identical food, and were from similar genetic background provided urine samples. Similar to the human data, guinea pig urine creatinine levels varied considerably (2.85 ± 2.1 mM) (Fig. 7). The metabolites hippurate and citrate, chosen randomly before for the human normal population, were also quantified in guinea pig urine and are shown in Figs. 8 and 9. Absolute urine hippurate concentrations for the guinea pig normal population are shown graphically in Fig. 8A, (mean: 9.69 ± 9.0 mM). The normalized hippurate concentrations following individual normalization to creatinine (Eq. 2) are shown in Fig. 8B, (mean: 10.16 ± 7.3). For citrate the absolute concentration mean was 0.23 ± 0.42 (Fig. 9A), and the normalized mean concentration was 0.57 ± 1.4 (Fig. 9B). Analysis for 23 metabolites revealed similarly large standard deviations and coefficients of variation for both absolute and normalized concentrations for the guinea pig group (Table 3).
Guinea pig urine hippurate concentrations prior to (9.58 ± 8.95 mM, A), and following normalization to creatinine (see Eq. 2, 10.2 ± 7.31,B)
Citrate levels in control guinea pig urine prior to (0.22 ± 0.42 mM, A), and following normalization to creatinine (see Eq. 2, 0.57 ± 1.35, B)
Interestingly the coefficients of variability for the metabolites identified in the guinea pig population were similar, or in some cases greater, when compared to the human control population. Many studies choose to use animal models because many of the extraneous factors identified as possible sources of error in human studies can be controlled, but our study demonstrates that similar variation is possible in a control guinea pig population. For example, control rat urine metabolites have varied during estrus cycles (Bollard et al. 2001), animal species (Bollard et al. 2005; Ebbels et al. 2004), diet (Phipps et al. 1998), and even metabolic variation within similar species (Tate et al. 2001; Holmes et al. 2000).
The time from the administration of anesthesia to collection of urine in the guinea pigs was roughly the same within minutes for all animals. NMR analysis of the guinea pig urine revealed resonant peaks from urethane; the concentration of which was statistically similar among all the animals (data not shown). This should remove the influence of anesthesia on metabolic variation within the guinea pig population because the level of sedation was consistent within the group (similar urethane concentrations in the urine).
Our data support the conclusions of some human urine studies indicating that there is a significant difference in metabolite excretion between male and female subjects. Our data shows that half of the metabolites examined demonstrated a statistically significant difference between sex groups. It is important that investigators choose the appropriate gender to compare between test and control populations (i.e., both populations of same sex, or equal mixture of gender) since we have shown that differences in metabolite excretion as a result of gender may confuse metabolic conclusions.
Although studies for urine metabolites in human control subjects are limited, there are studies which attempt to find correlation of urinary metabolites with age and diet (Guneral and Bachmann 1994), variation within large populations (Dyer et al. 1997; Symanski and Greeson 2002), and variation of metabolites over time (Lenz et al. 2003; Zuppi et al. 1997). Investigators have identified high inter-individual variations in urine metabolites, while intra-individual variation was low (Zuppi et al. 1997). These investigators concluded that most subjects had a characteristic profile that did not change with time and was independent of diet. Those results are not consistent with the degree of metabolite variation observed in this study. Although the average metabolite concentrations and standard deviations were strikingly similar for our normal population compared with Zuppi et al. (1997), the large degree of variability was not reduced when we followed single individuals over time. Since Zuppi et al. collected urine only once a month for 4 months the difference in collection frequency may explain the discrepancy. In addition, the larger population sampled in our study did not reduce the degree of variability. This suggests a unique population distribution that should be considered when performing the most basic statistical analysis. Other investigators have found that although there was high inter-individual variability, the intra-individual variability remained small (Lenz et al. 2003). Of the 24 metabolites measured in our study we found high inter- and intra-individual variability, and the different findings may be the result of the limited diet and short duration of the Lenz study. Unfortunately, they do not report actual metabolite concentrations making comparison to our study difficult.
Despite the intra-individual variability between our study and Zuppi et al., the population averages for three of the four metabolites (i.e., hippurate and citrate) reported in their study were strikingly similar to the population averages found in our study. Given the geographic difference (Rome, Italy for Zuppi (Zuppi et al., 1997) versus Edmonton, Canada for this study), and the probable genetic and diet differences between subjects in our study and those from Italy, the similarity in population averages between four metabolites from the two studies is very intriguing.
4 Concluding remarks
Urine is not a fluid in constant circulation throughout the body that requires monitoring like the blood. Rather, urine is a collection of waste and biological by-products that are reflective of a larger mixture of metabolic processes that may have occurred over a long time period. The large variability in metabolite concentrations within control subjects may be a reflection of the overall biological function of urine. However, the ease of urine sample collection has lead to its widespread use .as the biofluid for metabolomic studies of many different human disease states. Our study has highlighted important factors such as metabolite excretion differences due to sampling time, gender, and inter- and intra-individual variability; each of which impacts the growing use of urine in metabolomic and future clinical diagnostic studies. This investigation demonstrates the great care that must be taken when establishing normal metabolite baselines for comparison in basic research or clinical investigations.
References
Aspevall, O., Hallander, H., Gant, V., & Kouri, T. (2001). European guidelines for urinalysis: a collaborative document produced by European clinical microbiologists and clinical chemists under ECLM in collaboration with ESCMID. Clinical Microbiology and Infection, 7, 173–178.
Assadi, F. K. (2002). Quantitation of microalbuminuria using random urine samples. Pediatric Nephrology, 17, 107–110.
Bollard, M. E., Holmes, E., Lindon, J. C., Mitchell, S. C., Branstetter, D., Zhang, W., & Nicholson, J. K. (2001). Investigations into biochemical changes due to diurnal variation and estrus cycle in female rats using high-resolution (1)H NMR spectroscopy of urine and pattern recognition. Analytical Biochemistry, 295, 194–202.
Bollard, M. E., Stanley, E. G., Lindon, J. C., Nicholson, J. K., & Holmes, E. (2005). NMR-based metabonomic approaches for evaluating physiological influences on biofluid composition. NMR in Biomedicine, 18, 143–162.
Brindle, J. T., Antti, H., Holmes, E., Tranter, G., Nicholson, J. K., Bethell, H. W., Clarke, S., Schofield, P. M., Mckilligin, E., Mosedale, D. E., & Grainger, D. J. (2002). Rapid and noninvasive diagnosis of the presence and severity of coronary heart disease using 1H-NMR-based metabonomics. Nature Medicine, 8, 1439–1244.
Cavaluzzi, M. J., Kerwood, D. J., & Borer, P. N. (2002). Accurate nucleic acid concentrations by nuclear magnetic resonance. Analytical Biochemistry, 308, 373–380.
Chadha, V., Garg, U., & Alon, U. S. (2001). Measurement of urinary concentration: A critical appraisal of methodologies. Pediatric Nephrology, 16, 374–382.
Chung, Y. L., Rider, L. G., Bell, J. D., Summers, R. M., Zemel, L. S., Rennebohm, R. M., Passo, M. H., Hicks, J., Miller, F. W., & Scott, D. L. (2005). Muscle metabolites, detected in urine by proton spectroscopy, correlate with disease damage in juvenile idiopathic inflammatory myopathies. Arthritis and Rheumatism, 53, 565–570.
Coen, M., O’Sullivan, M., Bubb, W. A., Kuchel, P. W., & Sorrell, T. (2005). Proton nuclear magnetic resonance-based metabonomics for rapid diagnosis of meningitis and ventriculitis. Clinical Infectious Diseases, 41, 1582–1590.
Crockford, D. J., Keun, H. C., Smith, L. M., Holmes, E., & Nicholson, J. K. (2005). Curve-fitting method for direct quantitation of compounds in complex biological mixtures using 1H NMR: Application in metabonomic toxicology studies. Analytical Chemistry, 77, 4556–4562.
De Jongste, J. C. (2000). Surrogate markers of airway inflammation: Inflammometry in paediatric respiratory medicine. Paediatric Respiratory Reviews, 1, 354–360.
Duarte, I. F., Stanley, E. G., Holmes, E., Lindon, J. C., Gil, A. M., Tang, H., Ferdinand, R., Mckee, C. G., Nicholson, J. K., Vilca-Melendez, H., Heaton, N., & Murphy, G. M. (2005). Metabolic assessment of human liver transplants from biopsy samples at the donor and recipient stages using high-resolution magic angle spinning 1H NMR spectroscopy. Analytical Chemistry, 77, 5570–5578.
Dunn, W. B., Bailey, N. J., & Johnson, H. E. (2005). Measuring the metabolome: Current analytical technologies. The Analyst, 130, 606–625.
Dyer, A., Elliott, P., Chee, D., & Stamler, J. (1997). Urinary biochemical markers of dietary intake in the INTERSALT study. The American Journal of Clinical Nutrition, 65, 1246S–1253S.
Ebbels, T. M., Holmes, E., Lindon, J. C., & Nicholson, J. K. (2004). Evaluation of metabolic variation in normal rat strains from a statistical analysis of 1H NMR spectra of urine. Journal of Pharmaceutical and Biomedical Analysis, 36, 823–833.
Ekins, S., Nikolsky, Y., & Nikolskaya, T. (2005). Techniques: Application of systems biology to absorption, distribution, metabolism, excretion and toxicity. Trends in Pharmacological Sciences, 26, 202–209.
Gavaghan, C. L., Wilson, I. D., & Nicholson, J. K. (2002). Physiological variation in metabolic phenotyping and functional genomic studies: Use of orthogonal signal correction and PLS-DA. FEBS Letters, 530, 191–196.
Geigy, A. L. (1981–1992). Geigy scientific tables. West Cadwell, NJ: Ciba-Geigy Corp.
Green, R. H., Brightling, C. E., Mckenna, S., Hargadon, B., Parker, D., Bradding, P., Wardlaw, A. J., & Pavord, I. D. (2002). Asthma exacerbations and sputum eosinophil counts: A randomised controlled trial. Lancet, 360, 1715–1721.
Guneral, F., & Bachmann, C. (1994). Age-related reference values for urinary organic acids in a healthy Turkish pediatric population. Clinical Chemistry, 40, 862–866.
Holmes, E., Nicholls, A. W., Lindon, J. C., Connor, S. C., Connelly, J. C., Haselden, J. N., Damment, S. J., Spraul, M., Neidig, P., & Nicholson, J. K. (2000). Chemometric models for toxicity classification based on NMR spectra of biofluids. Chemical Research in Toxicology, 13, 471–478.
Keller, N. P., Turner, G., & Bennett, J. W. (2005). Fungal secondary metabolism—from biochemistry to genomics. Nature Reviews. Microbiology, 3, 937–947.
Keun, H. C., Ebbels, T. M., Antti, H., Bollard, M. E., Beckonert, O., Schlotterbeck, G., Senn, H., Niederhauser, U., Holmes, E., Lindon, J. C., & Nicholson, J. K. (2002). Analytical reproducibility in (1)H NMR-based metabonomic urinalysis. Chemical Research in Toxicology, 15, 1380–1386.
Kraut, J. A., & Kurtz, I. (2005). Metabolic acidosis of CKD: Diagnosis, clinical characteristics, and treatment. American Journal of Kidney Diseases, 45, 978–993.
Kubitz, R., Keitel, V., & Haussinger, D. (2005). Inborn errors of biliary canalicular transport systems. Methods in Enzymology, 400, 558–569.
Kumar, A., Ernst, R. R., & Wuthrich, K. (1980). A two-dimensional nuclear overhauser enhancement (2D NOE) experiment for the elucidation of complete proton–proton cross-relaxation networks in biological macromolecules. Biochemical and Biophysical Research Communications, 95, 1–6.
Lenz, E. M., Bright, J., Wilson, I. D., Morgan, S. R., & Nash, A. F. (2003). A 1H NMR-based metabonomic study of urine and plasma samples obtained from healthy human subjects. Journal of Pharmaceutical and Biomedical Analysis, 33, 1103–1115.
Lenz, E. M., Bright, J., Wilson, I. D., Hughes, A., Morrisson, J., Lindberg, H., & Lockton, A. (2004). Metabonomics, dietary influences and cultural differences: A 1H NMR-based study of urine samples obtained from healthy British and Swedish subjects. Journal of Pharmaceutical and Biomedical Analysis, 36, 841–849.
Lindon, J. C., Holmes, E., Bollard, M. E., Stanley, E. G., & Nicholson, J. K. (2004). Metabonomics technologies and their applications in physiological monitoring, drug safety assessment and disease diagnosis. Biomarkers, 9, 1–31.
Moolenaar, S. H., Engelke, U. F., & Wevers, R. A. (2003). Proton nuclear magnetic resonance spectroscopy of body fluids in the field of inborn errors of metabolism. Annals of Clinical Biochemistry, 40, 16–24.
Phipps, A. N., Stewart, J., Wright, B., & Wilson, I. D. (1998). Effect of diet on the urinary excretion of hippuric acid and other dietary-derived aromatics in rat. A complex interaction between diet, gut microflora and substrate specificity. Xenobiotica, 28, 527–537.
Rastall, R. A., Gibson, G. R., Gill, H. S., Guarner, F., Klaenhammer, T. R., Pot, B., Reid, G., Rowland, I. R., & Sanders, M. E. (2005). Modulation of the microbial ecology of the human colon by probiotics, prebiotics and synbiotics to enhance human health: An overview of enabling science and potential applications. FEMS Microbiology Ecology, 52, 145–152.
Sabatine, M. S., Liu, E., Morrow, D. A., Heller, E., Mccarroll, R., Wiegand, R., Berriz, G. F., Roth, F. P., & Gerszten, R. E. (2005). Metabolomic identification of novel biomarkers of myocardial ischemia. Circulation, 112, 3868–3875.
Sardari, S., & Sardari, D. (2002). Applications of artificial neural network in AIDS research and therapy. Current Pharmaceutical Design, 8, 659–670.
Saude, E. J., Slupsky, C. M., & Sykes, B. D. (2006). Optimization of NMR analysis of biological fluids for quantitative accuracy. Metabolomics, 2, 113–123.
Saude, E. J., Sykes, B. D. (2007). Urine stability for metabolomic studies: Effects of preparation and storage. Metabolomics, 3, 19–27.
Shockcor, J. P., & Holmes, E. (2002). Metabonomic applications in toxicity screening and disease diagnosis. Current Topics in Medicinal Chemistry, 2, 35–51.
Singer, M. (2005). Metabolic failure. Critical Care Medicine, 33, S539–s542.
Slupsky, C. M., Rankin, K., Wagner, J., Fu, H., Chang, D., Weljie, A. M., Saude, E. J., Lix, B., Adamko, D. J., Shah, S., Greiner, R., Sykes, B. D., Marrie, T. J. (2007). Investigations of the effects of gender, diurnal variation, and age in human urinary metabolomic profiles. Analytical Chemistry, 79, in press.
Somorjai, R. L., Dolenko, B., Demko, A., Mandelzweig, M., Nikulin, A. E., Baumgartner, R., & Pizzi, N. J. (2004). Mapping high-dimensional data onto a relative distance plane—an exact method for visualizing and characterizing high-dimensional patterns. Journal of Biomedical Informatics, 37, 366–379.
Stanley, E. G., Bailey, N. J., Bollard, M. E., Haselden, J. N., Waterfield, C. J., Holmes, E., & Nicholson, J. K. (2005). Sexual dimorphism in urinary metabolite profiles of Han Wistar rats revealed by nuclear-magnetic-resonance-based metabonomics. Analytical Biochemistry, 343, 195–202.
Stoyanova, R., & Brown, T. R. (2001). NMR spectral quantitation by principal component analysis. NMR in Biomedicine, 14, 271–277.
Symanski, E., & Greeson, N. M. (2002). Assessment of variability in biomonitoring data using a large database of biological measures of exposure. AIHA Journal (Fairfax, Va), 63, 390–401.
Tate, A. R., Damment, S. J., & Lindon, J. C. (2001). Investigation of the metabolite variation in control rat urine using (1)H NMR spectroscopy. Analytical Biochemistry, 291, 17–26.
Trachtenbarg, D. E. (2005). Diabetic ketoacidosis. American Family Physician, 71, 1705–1714.
Van Rhijn, B. W., Van Der Poel, H. G., & Van Der Kwast, T. H. (2005). Urine markers for bladder cancer surveillance: A systematic review. European Urology, 47, 736–748.
Weckwerth, W. (2003). Metabolomics in systems biology. Annual Review of Plant Biology, 54, 669–689.
Wennergren, G. (2000). Inflammatory mediators in blood and urine. Paediatric Respiratory Review, 1, 259–265.
Zuppi, C., Messana, I., Forni, F., Rossi, C., Pennacchietti, L., Ferrari, F., & Giardina, B. (1997). 1H NMR spectra of normal urines: Reference ranges of the major metabolites. Clinica Chimica Acta, 265, 85–97.
Acknowledgments
The authors would like to thank the volunteers for their participation in the study, Bruce Lix for his assistance with organization, Shana Regush for her assistance with sample preparation and data acquisition, Carol Mangan for her logistical management of the study, Dr. Edward Akhmetshin for his expertise in statistical analysis, and Ryan McKay for his thorough reviews of the manuscript. This research was supported by the Canadian Institutes of Health Research (CIHR), Genome Prairie, and Genome Canada, and by an establishment grant from the Alberta Heritage Foundation for Medical Research (AHFMR) to T. Marrie. We would like to thank the Canadian National High Field NMR Centre (NANUC) for their assistance and use of the facilities. CIHR, the Natural Science and Engineering Research Council of Canada and the University of Alberta fund the operation of NANUC. Drs. Rowe and Sykes are supported by Canada Research Chairs. Dr. Adamko is supported by AHFMR as a Clinical Investigator. Magnetic Resonance Diagnostic Centre (MRDC) is supported by establishment grants from the Alberta Science and Research Authority (ASRA), and Western Economic Development (WED). All of the authors are members of the Medical Resonance Diagnostics Centre (MRDC) at the University of Alberta, Edmonton, Alberta, Canada.
Support: Canadian Institutes of Health Research (CIHR), Genome Prairie, Genome Canada, an establishment grant from the Alberta Heritage Foundation for Medical Research (AHFMR), the Canadian National High Field NMR Centre (NANUC), the Natural Science and Engineering Research Council of Canada (NSERC), the University of Alberta fund, the Magnetic Resonance Diagnostic Centre (MRDC), the Alberta Science and Research Authority (ASRA), and Western Economic Development (WED).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Saude, E.J., Adamko, D., Rowe, B.H. et al. Variation of metabolites in normal human urine. Metabolomics 3, 439–451 (2007). https://doi.org/10.1007/s11306-007-0091-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11306-007-0091-1