Abstract
In addition to their role in glycosylation reactions, UDP-sugars are released from cells and activate widely distributed cell surface P2Y14 receptors (P2Y14R). However, the physiological/pathophysiological consequences of UDP-sugar release are incompletely defined. Here, we report that UDP-glucose levels are abnormally elevated in lung secretions from patients with cystic fibrosis (CF) as well as in a mouse model of CF-like disease, the βENaC transgenic (Tg) mouse. Instillation of UDP-glucose into wild-type mouse tracheas resulted in enhanced neutrophil lung recruitment, and this effect was nearly abolished when UDP-glucose was co-instilled with the P2Y14R antagonist PPTN [4-(piperidin-4-yl)-phenyl)-7-(4-(trifluoromethyl)-phenyl-2-naphthoic acid]. Importantly, administration of PPTN to βENaC-Tg mice reduced neutrophil lung inflammation. These results suggest that UDP-glucose released into the airways acts as a local mediator of neutrophil inflammation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Nucleotides are released from cells in a regulated fashion, activate cell surface purinergic receptors, and promote a broad range of physiological processes [1, 2]. Purinergic receptors comprise three subfamilies. The G protein-coupled A1R, A2AR, A2BR, and A3R are activated by adenosine [3], the G protein-coupled P2Y receptors are activated by ATP (P2Y2R, P2Y11R), ADP (P2Y1R, P2Y12R, P2Y13R), UTP (P2Y2R, P2Y4R), UDP (P2Y6R, P2Y14R), or UDP-sugars (P2Y14R) [4], and the P2X receptors are ligand-gated ion channels activated by ATP [5].
Extracellular nucleotides and nucleosides regulate mucociliary clearance (MCC) activities, thereby promoting the primary innate defense mechanism that removes foreign particles and pathogens from airway surfaces. Purinergic regulation in the airways is mediated mainly by the P2Y2R and the A2BR [6]. Activation of the A2BR results in cyclic AMP-dependent activation of the cystic fibrosis transmembrane regulator (CFTR) Cl− channel and stimulation of ciliary beat frequency. Activation of the P2Y2R promotes inhibition of Na+ absorption as well as CFTR-dependent and CFTR-independent Cl− secretion, ciliary beating, and mucin secretion [6, 7]. In addition, nucleotides within the airway surface liquid (ASL) are potent pro-inflammatory signaling molecules acting on purinergic receptors expressed on immune/inflammatory cells or by promoting the release of cytokines and other chemoattractants from lung epithelial cells [8–11]. Thus, the rates of nucleotide release and metabolism in healthy airways are finely regulated to maintain effective MCC without promoting airway inflammation.
Mucus plugging, infection, and neutrophil inflammation in the lung are pathological features of chronic inflammatory lung diseases such as cystic fibrosis (CF) and chronic bronchitis [CB, a form of chronic obstructive lung disease (COPD)]. While polymorphonuclear neutrophils (PMN) are key players in fighting infections, they also are major contributors to the inflammatory response causing lung destruction in CF and COPD [12]. Failure to effectively manage lung inflammation in CF and COPD is due, in part, to a limited understanding of the processes responsible for neutrophil recruitment, activation, and clearance in diseased airways.
The P2Y14R is a Gi-coupled receptor that is activated by UDP-sugars with a relative potency order of UDP-glucose > UDP-galactose > UDP-glucuronic acid > UDP-N-acetylglucosamine [13, 14]. UDP also is an agonist of this receptor, but ATP, UTP, or other naturally occurring nucleoside 5′- di- or triphosphates have no P2Y14R activity [13–16]. P2Y14R mRNA expression has been reported in the brain and several peripheral tissues [13], including the lung, circulating neutrophils, and other immune/inflammatory cells [17–21].
Studies from our lab have illustrated the occurrence of regulated release of UDP-sugars from several cell types, including airway epithelial cells [22–28]. Notably, enhanced UDP-sugar release was observed in mucin-secreting cells. For example: (i) primary cultures of human bronchial epithelial (HBE) cells induced to develop goblet cell metaplasia by infection with respiratory syncytial virus or treatment with interleukin 13 (IL-13) exhibited enhanced release of UDP-glucose concomitantly with increased mucin secretion [22]; and (ii) goblet cell-like Calu-3 cells exhibited enhanced Ca2+-regulated exocytosis of mucin granules, which was accompanied by increased release of UDP-glucose [27]. Bronchoalveolar lavage fluids (BALF) from patients with CF and control diseases exhibit robust accumulation of UDP-sugars [24]. In spite of the apparent association between UDP-sugar levels in airway surface liquids and mucin hypersecretion and inflammation, the pathophysiological consequences of UDP-glucose release into the airways are not well understood.
Two lines of evidence suggest that UDP-sugars accumulating in the airway/alveolar space potentially trigger neutrophil infiltration in the lung. Müller and co-workers reported expression of P2Y14R mRNA in primary cultures of human alveolar epithelial type II cells, as well as in immortalized human lung epithelial cell lines [11]. They also showed that addition of UDP-glucose to these cells resulted in enhanced secretion of interleukin 8 (IL-8), a potent neutrophil chemoattractant [11]. In addition, we recently demonstrated that UDP-glucose promotes P2Y14R-mediated chemotaxis of freshly isolated human neutrophils. Enhanced PMN migration was observed in response to UDP-glucose gradients, and this activity was abolished when the P2Y14R antagonist PPTN [4-(piperidin-4-yl)-phenyl)-7-(4-(trifluoromethyl)-phenyl-2-naphthoic acid] was included in the cell suspension buffer [29, 30]. We also showed that UDP-glucose-promoted chemotaxis in neutrophil-like HL60 cells was absolutely dependent on the expression of P2Y14R in these cells and was abolished by PPTN [29, 30].
Whether UDP-glucose acts as a pro-inflammatory mediator in the lung is not known. To this end, we examined the effect of UDP-glucose administration on neutrophil lung infiltration in wild-type mice and used the mucin-hypersecreting βENaC transgenic mouse to further investigate the effect of PPTN on the spontaneous neutrophil lung inflammation associated with this mouse model.
Materials and methods
Materials
UDP-glucose (Fluka catalog # 94335) was purchased from Sigma-Aldrich (St. Louis, MO); high-performance liquid chromatography (HPLC) analysis indicated that UDP-glucose was not contaminated with ATP, UTP, or other nucleotide-signaling molecules [29]. PPTN was synthesized as previously described [30] and used as a dimethylsulfoxide (DMSO) stock solution (100 mM), which was stored at −20 °C. PPTN was freshly diluted in endotoxin-free PBS before its administration to mice and an equivalent dilution of DMSO in PBS was used as vehicle in control animals.
Subjects
Healthy (n = 10) and CF (n = 8) adults were recruited to provide sputum specimens. Healthy subjects were non-smokers without a history of asthma or allergy. CF subjects were at their baseline state of health and had not been treated for acute infection or exacerbation in the prior 4 weeks. Five of 8 CF subjects used cycling inhaled antibiotics chronically, but no samples were collected during an “on” treatment period. All but one CF subject were pancreatic insufficient, and all had moderate to severe lung disease. See Table 1 for additional demographic features. All subjects were studied at the University of North Carolina at Chapel Hill (Chapel Hill, NC, USA), and studies were approved by the Institutional Review Board.
Sputum collection and processing
Spontaneous sputum from CF patients and induced sputum from healthy control subjects were collected and processed as previously described [31, 32]. Briefly, mucus plug was selected and weighted. Aliquots were treated with Sputolysin (DTT) and 1 mM EDTA, filtered, and centrifuged, and the cell-free supernatant was stored at −80, until further nucleotide analysis.
Measurements of nucleotides in lung secretions
UDP-glucose concentration was measured using the UDP-glucose pyrophosphorylase-catalyzed conversion of UDP-glucose and 32PPi to [32P]UTP and glucose-1P; the resulting 32P-labeled species were quantified by HPLC, as described [28]; samples where supplemented with 25 mM 4-(2-hydroxyethyl)-1-piperazineethanesulfonic acid (HEPES) pH 7.4, 2 mM MgCl2, and 2 mM CaCl2 prior UDP-glucose measurements. ATP levels were quantified by the off-line luciferin-luciferase assay, using a GloMax luminometer (Promega, Madison, WI) equipped with an automated injector. Sample aliquots (20 μl) were transferred to a 96-well plate containing 150 μl H20/well and placed in the luminometer chamber. Seventy-five microliters of the luciferin-luciferase buffer [33] were subsequently injected, and luminescence was read and integrated every 4 s using the GloMax® Discover software. ATP calibration curves were performed in parallel to samples.
Metabolism of UDP-glucose and ATP in sputum
Sputum samples (50 μl) were incubated at 37 °C with 5 μM ATP or 5 μM UDP-Glc in the presence of 25 mM HEPES, 2 mM MgCl2 and 2 mM CaCl2. At the indicated times, samples were heat inactivated and cooled on ice, and ATP and UDP-Glc were quantified as indicated above.
Mice
All mice used in these studies were on C57BL/6 background. For intratracheal instillation studies, wild-type mice were purchased from Taconic (Hudson, NY). The airway specific βENaC transgenic (βENaC-Tg) mouse (overexpressing the β-subunit of the epithelial sodium channel ENaC encoded by the Scnn1b gene) [34] and littermate controls (wild type) were obtained from the UNC CF Center Mouse Model Core. Mice were housed in individually ventilated micro-isolator cages, in a specific pathogen-free facility maintained at the University of North Carolina at Chapel Hill, on a 12-h day/night cycle. They were fed a regular chow diet and given water ad libitum. Animal protocols were reviewed and approved by the Institutional Animal Care and Use Committee of the University of North Carolina at Chapel Hill.
Intratracheal instillation
Eight-week-old wild-type mice were treated with sterile, endotoxin-free PBS (2 μl/g body weight, 40–50 μl via intratracheal instillation) either alone or containing 10 mM UDP-glucose, 10 μM PPTN, or both [35]. Animals were sacrificed 12 h after treatment (unless specified otherwise) and bronchoalveolar lavage (BAL) obtained and analyzed as described below.
Bronchoalveolar lavage and differential cell counts
BAL was performed as previously described [36]. Briefly, mice were euthanized, the chest cavity opened, and PBS was gently injected (and retrieved) on the whole lung (800 μl in adult mice; 200 μl in 13–14-day-old pups). This procedure was conducted three times with an equal volume of PBS and fractions were pooled. Cells were pelleted and the cell-free supernatant (i.e., BALF) was stored at −80 °C for further analysis. Cells were resuspended, counted with a hemocytometer, and centrifuged (StatSpin CytoFuge 2) and the resulting cytospin was stained for differential cell counting (Wright staining). Cytospin images were obtained with a Nikon Microphot-SA microscope interfaced with a DXM 1200 camera.
PPTN treatment of newborn βENaC-Tg mice
Newborn βENaC-Tg mice were subjected to intranasal instillation [37] of PPTN (100 μM PPTN once a day, 1 μl/g body weight) or equal volume of vehicle for 12 days. Pulmonary deposition studies in newborn mice indicated that approximately 4 % of drug doses delivered by intranasal instillation were deposited into the lungs [37]. No differences in growth and survival were observed between control and PPTN-treated mice. Twelve hours after the last treatment, animals were sacrificed and BAL performed as described above.
Cytokine measurements
Mouse CXCL1/GRO alpha (keratinocyte-derived cytokine, KC) was measured in BALF by the UNC Immunotechnology Core (CGIBD Advanced Analytics Core), using the developing reagent 3,3′,5,5′-tetramethylbenzidine and the reader BioTek Synergy HT microplate spectrophotometer, BioTek’s Gen5.
Statistical analyses
Statistical analyses were performed using SigmaStat 3.1 or JMP 12.0.1. Comparisons between measurements from two groups with significant difference in variances were performed using the Student t test assuming non-equal variance, or non-parametric Wilcoxon rank-sum test. Comparison between multiple groups was performed using one-way analysis of variance (ANOVA) and differences among the group means were assessed by the Tukey-Kramer post-hoc test for multiple test correction. For inferential statistics, p < 0.05 was considered statistically significant. Where indicated, numeric values were log10-transformed with an offset of +1 before inferential statistical analyses.
Results
Increased levels of UDP-glucose in neutrophil-inflamed CF lung secretions
Previous studies indicated robust levels of UDP-sugars in in vivo airway surface liquid (BALF) from chronically diseased lungs (e.g., cystic fibrosis) [24], but the extent to which concentrations of UDP-sugars in CF airway secretions differ from healthy controls is not known. Therefore, we examined the nucleotide content in sputum samples (believed to reflect secretions from the large airways) [38] obtained from CF patients with moderate or severe lung disease and from healthy control subjects. As indicated in Table 1, CF patients exhibited decreased pulmonary function (assessed as forced expiratory volume, FEV1% predicted) and increased (but broadly spread) number of neutrophils in sputum. UDP-glucose concentrations in control sputa were in the low nanomolar range (UDP-glucose 9.5 ± 2.1 nM) but increased up to 11-fold in CF (Fig. 1a), i.e., reaching concentration values capable of promoting P2Y14R-mediated responses [29]. Although the small sample size prevented us from establishing a correlation between UDP-glucose levels and lung function or sputum neutrophils within the CF group (Suppl. Fig. 1), the data suggest an association between CF lung disease and ASL UDP-glucose.
Elevated UDP-glucose levels in CF sputa. Nucleotide levels (a) and nucleotide metabolism rates (b) were assessed in sputum samples obtained from ten control (CTL) subjects and eight CF patients. The data are expressed as mean ± SEM. An asterisk symbol indicates p < 0.05; a double-barred pipe symbol indicates p < 0.005 against CTL. UDP-Glc UDP-glucose
ATP levels seemed to increase in CF but were not significantly different between CF and control samples (Fig. 1). Ecto-nucleotidases expressed on (or secreted/shed from) epithelial cells and inflammatory cells [29, 39, 40] could have contributed to the pattern of nucleotide accumulation observed in control and CF sputum. To gain an insight into potential metabolism differences between ATP and UDP-glucose in lung secretions, rates of ATP and UDP-glucose hydrolysis were assessed in sputum supernatants. Incubation of control sputum with ATP resulted in 23 ± 5, 68 ± 9, and 78 ± 10 % hydrolysis after 10, 20, and 60 min, respectively (Fig. 1b). ATP hydrolysis increased considerably (to 61 ± 14, 89 ± 7, and 95 ± 4 % at 10, 20, and 60 min, respectively) in CF sputum. ATP half-life value in CF sputum (t 1/2 = 7.3 min) was 3-fold shorter than ATP t 1/2 value in control samples (23.2 min) (Fig. 1b). In contrast to ATP, UDP-glucose remained essentially unchanged in both control and CF sputa after 60 min (Fig. 1b).
CF/CB-like diseased mouse airways contain elevated levels of UDP-glucose
Overexpression of the epithelial Na+ channel β-subunit (Scnn1b gene, βENaC protein) in transgenic mouse airways (βENaC-Tg mice) results in epithelial Na+ hyperabsorption, airway dehydration, impaired mucus clearance, and airway inflammation [34, 41]. This phenotype recapitulates many features of CF and other chronic airway diseases [34, 41]. For example, βENaC-Tg mice exhibit signs of chronic bronchitis, with macrophage and neutrophil accumulation in the lumen of the conducting airways and elevated neutrophil counts in BAL [34, 41]. Our data indicate that the βENaC-Tg mouse exhibits enhanced levels of UDP-glucose in BALF. As shown in Fig. 2, UDP-glucose concentrations in BALF from wild-type mice were 17 ± 14 nM, but levels increased to 87 ± 15 nM in BALF from βENaC-Tg littermates. Taking into account the substantial ASL dilution occurring during BAL procedures, extracellular levels of UDP-glucose in βENaC-Tg mouse lungs likely reach concentrations capable of promoting robust activation of P2Y14R. ATP levels were not statistically elevated in βENaC-Tg BALF (Fig. 2), likely reflecting hydrolysis of released ATP.
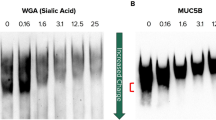
UDP-glucose promotes neutrophil lung inflammation
The observation that UDP-glucose concentrations are elevated in lung secretions from neutrophil-inflamed airways prompted us to investigate a potential pro-inflammatory action of UDP-glucose in the lung. UDP-glucose or PBS was administrated to the lungs of wild-type mice via tracheal instillation and BAL was performed after 12 h. BAL obtained from PBS-treated mice exhibited little or no neutrophils, and alveolar-resident macrophages were the predominant cells recovered in these lavages (Fig. 3a, b) [36]. In contrast, instillation of UDP-glucose resulted in a robust increase of neutrophils in BAL after 12 h (Fig. 3a, b). Similar effects of UDP-glucose were also observed after pre-treatment of UDP-glucose with apyrase to eliminate potential contamination with ATP/UTP [29] (not shown). Time-course experiments indicated that maximal PMN recruitment occurred within 12 h following UDP-glucose instillation; neutrophil levels declined considerably after 24 h (Fig. 3c).
UDP-glucose promotes neutrophil recruitment in mouse lungs. PBS or UDP-glucose was instilled into wild-type mouse trachea and BAL was performed after 12 h (a, b) or at the times indicated (c). a Representative photomicrograph of BAL cytospin preparations. Neutrophils are indicated with arrow heads; Wright staining (magnification = 40×). b Differential cell counting (mean ± SD, n = 4, *p < 0.05 against PBS). Mac macrophages, PMN neutrophils, Eos eosinophils, Lym lymphocytes. C Time-course of UDP-glucose-promoted neutrophil recruitment in the lung; the data are the mean ± difference to the mean from a representative experiment performed with duplicate samples; similar results were obtained in two separate experiments
We recently reported that the naphthoic acid derivative PPTN is a high-affinity competitive antagonist of the P2Y14R that does not interact with any of the other seven P2Y receptor subtypes [30]. UDP-glucose-stimulated neutrophil lung infiltration was almost completely blocked when the UDP-sugar was co-instilled with PPTN (Fig. 4). These results strongly suggest that UDP-glucose-stimulated neutrophil recruitment in mouse lungs involves activation of the P2Y14R.
The P2Y14R antagonist PPTN reduces neutrophil inflammation in the βENaC-Tg mouse
Having shown that administration of UDP-glucose resulted in P2Y14R-dependent neutrophil recruitment in wild-type mice, we asked whether the P2Y14R contributes to the spontaneous inflammatory phenotype associated with the βENaC-Tg mouse. Previous studies indicated that βENaC-Tg mouse lung inflammation is acquired over the perinatal period [34, 41, 42]. Therefore, we examined the effect of PPTN on neutrophil lung recruitment after daily intranasal instillation of the P2Y14R antagonist to neonatal mice for 12 days. BALs from βENaC-Tg mice treated with PBS displayed elevated neutrophils (and eosinophils) relative to wild-type mice (Fig. 5a and [36]). Levels of the neutrophil chemoattractant cytokine mKC also were elevated (Fig. 5b), consistent with the inflammatory phenotype described in 10-day-old βENaC-Tg mice [41, 42]. Notably, PMN infiltration and mKC levels were markedly reduced in βENaC-Tg mice treated with PPTN (Fig. 5a, b). PPTN had no effect on macrophage and eosinophil counts (Fig. 5a).
PPTN reduces neutrophil lung infiltration and BALF mKC levels in βENaC-Tg mice. Newborn βENaC-Tg mice were treated with PPTN (n = 17) or vehicle (n = 16) for 12 days, as indicated in the “Materials and methods” section. BAL was performed 24 h after the last treatment and a cells and b mKC were quantified. The data represent the mean ± SE; *p < 0.05 relative to vehicle
Discussion
Neutrophil infiltration and mucus plugs are a hallmark of lung diseases such as COPD and CF [12, 31, 43, 44], but the mechanism of neutrophil lung recruitment in mucus-obstructed lungs is incompletely understood. In the present study, we demonstrate that UDP-glucose levels are abnormally elevated in lung secretions from CF patients and from a mouse model of CF/chronic bronchitis, the βENaC-Tg transgenic mouse (Figs. 1 and 2). We also show that administration of UDP-glucose into mouse lung resulted in robust accumulation of neutrophils in BAL (Fig. 3).
Availability of PPTN provides an important molecular probe for interrogation of the functional role(s) played by the P2Y14R in lung physiology and pathophysiology. PPTN acts as a high-affinity competitive antagonist of the P2Y14R and does so without interacting with any of the other seven P2Y receptor subtypes [30]. Furthermore, PPTN blocks UDP-glucose-promoted chemotaxis of human neutrophils without affecting responses to bacterial peptides [30]. Here, we show that PPTN not only blocked the effect of exogenous UDP-glucose on neutrophil lung recruitment (Fig. 4) but also attenuated the spontaneous neutrophil inflammation that characterizes the βENaC-Tg mouse (Fig. 5). Collectively, these results strongly suggest that UDP-glucose released into CF-like diseased airways acts as a pro-inflammatory mediator, via stimulation of the P2Y14R.
P2Y14R mRNA is expressed in human [45] and murine [46] lungs [17, 46] and inflammatory cells [17–21], but the identity of the cell type(s) potentially sensing UDP-glucose in airway surface liquids is not known. We observed no P2Y14R mRNA amplification in well-differentiated primary cultures of bronchial epithelial cells (data not shown). However, relevant to this study, Müller and co-workers reported that P2Y14R mRNA is expressed in cultured human alveolar epithelial type II cells and also reported that addition of UDP-glucose to these cells resulted in enhanced secretion of IL-8 [11]. Our data indicating that PPTN decreased mKC levels in the βENaC-Tg mouse BAL (Fig. 5) could reflect a contribution of P2Y14R-promoted cytokine release from alveolar epithelial cells, upstream of neutrophil recruitment [47]. In addition to the above-discussed scenario, published gene expression analyses indicated high levels of P2Y14R mRNA in murine alveolar macrophages [48]. Therefore, activation of P2Y14R on lung resident macrophages also potentially results in production of pro-inflammatory cytokines leading to neutrophil recruitment.
We recently illustrated that the P2Y14R is functionally expressed in freshly isolated blood neutrophils, promoting cytoskeleton rearrangement, Rho activation, and cell migration [29, 30]. Therefore, an additional mechanism likely contributing to UDP-glucose-promoted neutrophil lung inflammation is via activation of the neutrophil P2Y14R. For example, UDP-glucose released into ASL could diffuse through the paracellular pathway generating trans-epithelial and trans-endothelial gradients that direct neutrophils from the vasculature to the airways. Alternatively, cytokines released from alveolar cells and/or macrophages could guide neutrophils out the blood vessels, and UDP-glucose could direct them into the airways. Furthermore, UDP-glucose-stimulated neutrophils may produce and release chemoattractants such as leukotriene B4 and IL-8, potentiating the recruitment of additional neutrophils at the inflammation site.
What is/are the cellular source(s) of extracellular UDP-glucose in the CF lung? UDP-sugars are synthesized in the cytosol and translocated into the lumen of the secretory pathway where they serve as substrates of glycosylation reactions. Thus, one mechanism potentially contributing to UDP-glucose accumulation in ASL is its release from vesicles as co-cargo with exported glycoconjugates. Indeed, we have shown that, by controlling the entry of UDP-sugars into the Golgi, SLC35 nucleotide-sugar transporters contribute to the vesicular release of UDP-sugars from cultured airway epithelial cells [24]. Furthermore, goblet cell-rich airway epithelial cell models exhibit enhanced release of UDP-glucose concomitantly with mucins, heavily glycosylated proteins. Thus, the mucin hypersecreting airway epithelia likely are an important source of UDP-glucose accumulation in CF sputa and βENaC-Tg mouse BALF. However, we cannot rule out that activated and/or necrotic/apoptotic inflammatory cells also contributed to the enhanced levels of UDP-glucose observed in these samples.
It is worth noting that, in most cases where regulated nucleotide release was assessed, rates of UDP-glucose release were markedly lower than ATP release rates, whereas steady-state levels of UDP-glucose were often higher than ATP levels [28]. Differences in rates of extracellular metabolism account for this apparent discrepancy. For example, ecto-nucleoside triphosphate diphosphohydrolases (E-NTPDases) sequentially dephosphorylate ATP to ADP and AMP (ATP → ADP → AMP + 2 phosphates) and are abundantly expressed on the surface of most cell types [49], including airway epithelial cells [39, 50] and neutrophils [51]. Alkaline phosphatase, which is expressed on airway epithelial cells [52], sequentially dephosphorylates ATP, ADP, and AMP. UDP-sugars are not metabolized by E-NTPDase or alkaline phosphatase activities [49]. An additional group of ecto-nucleotidases includes members of the ecto-nucleotide pyrophosphatase/phosphodiesterase (E-NPP) family. E-NPPs break down UDP-sugars (UDP-sugar → sugar-1P + pyrophosphate) as well as ATP (ATP → AMP + pyrophosphate) [49]. Our previous studies with primary cultures of HBE cells indicated that inorganic [32P]-phosphate, but not [32P]-pyrophosphate, was the product of [32γP]ATP hydrolysis on these cells [53], suggesting that E-NPP activities are not present on human airway epithelia. Consistent with this observation, we observed no hydrolysis of UDP-[3H]glucose after a 2-h incubation of this radiotracer on primary HBE cells, whereas [32γP]ATP was completely hydrolyzed (Lazarowski, unpublished). Our data with CF lung sputum (Fig. 1B) indicated that, unlike ATP, UDP-glucose was not hydrolyzed after 1 h, suggesting that secreted/shed E-NTPDases and/or phosphatases, but not E-NPPs, are present in the soluble phase of CF lung secretions.
Previous studies indicated that UDP-N-acetylglucosamine is present in BALF isolated from patients with CF and other inflammatory diseases at concentrations similar to UDP-glucose concentrations [24]. On a speculative basis, UDP-N-acetylglucosamine and potentially UDP-galactose and UDP-glucuronic acid may contribute to P2Y14R-dependent lung phenotypes. However, given the low P2Y14R agonist potency exhibited by these UDP-sugars, relative to UDP-glucose [13, 54], UDP-glucose predictably is the most important autocrine/paracrine regulator of P2Y14R-mediated lung inflammation. Recent studies examining P2Y14R-dependent second messenger formation in model cell lines revealed that UDP is a very potent agonist of this receptor [15]. However, since UDP serves as a substrate of most E-NTPDases [49], it is unlikely that the concentration of extracellular UDP approaches that of UDP-sugars under most physiological and pathological conditions. Collectively, our findings suggest that UDP-glucose is a highly stable pro-inflammatory mediator present in CF-like diseased airways.
In summary, this study indicates that UDP-glucose levels are elevated in CF and CF-like lung secretions and that administration of UDP-glucose into mouse lungs results in neutrophil inflammation. The hypothesis that nucleotide-sugars act as pro-inflammatory signaling molecules in the lung is further supported by the observation that a P2Y14R-selective antagonist reduces the spontaneous neutrophil lung inflammation associated with the CF-like βENaC mouse. The extent to which P2Y14R expressed on lung epithelial cells, alveolar macrophages, and neutrophils contribute to this phenotype remains to be elucidated.
References
Burnstock G (2006) Purinergic signalling. Br J Pharmacol 147(Suppl 1):S172–S181
Lazarowski ER (2012) Vesicular and conductive mechanisms of nucleotide release. Purinergic Signal 8:359–373
Fredholm BB, IJzerman AP, Jacobson KA, Klotz KN, Linden J (2001) International Union of Pharmacology. XXV. Nomenclature and classification of adenosine receptors. Pharmacol Rev 53:527–552
Abbracchio MP, Burnstock G, Boeynaems JM, Barnard EA, Boyer JL, Kennedy C, Knight GE, Fumagalli M, Gachet C, Jacobson KA, Weisman GA (2006) International Union of Pharmacology LVIII: update on the P2Y G protein-coupled nucleotide receptors: from molecular mechanisms and pathophysiology to therapy. Pharmacol Rev 58:281–341
Khakh BS, North RA (2006) P2X receptors as cell-surface ATP sensors in health and disease. Nature 442:527–532
Lazarowski ER, Boucher RC (2009) Purinergic receptors in airway epithelia. Curr Opin Pharmacol 9:262–267
Boucher RC (2003) Regulation of airway surface liquid volume by human airway epithelia. Pflugers Arch 445:495–498
Idzko M, Ferrari D, Eltzschig HK (2014) Nucleotide signalling during inflammation. Nature 509:310–317
Ribeiro CM, Paradiso AM, Carew MA, Shears SB, Boucher RC (2005) Cystic fibrosis airway epithelial Ca2+ i signaling: the mechanism for the larger agonist-mediated Ca2+ i signals in human cystic fibrosis airway epithelia. J Biol Chem 280:10202–10209
Douillet CD, Robinson WP III, Milano PM, Boucher RC, Rich PB (2006) Nucleotides induce IL-6 release from human airway epithelia via P2Y2 and p38 MAPK-dependent pathways. Am J Physiol Lung Cell Mol Physiol 291:L734–L746
Muller T, Bayer H, Myrtek D, Ferrari D, Sorichter S, Ziegenhagen MW, Zissel G, Virchow Jr JC, Luttmann W, Norgauer J, Di Virgilio F, Idzko M (2005) The P2Y14 receptor of airway epithelial cells: coupling to intracellular Ca2+ and IL-8 secretion. Am J Respir Cell Mol Biol 33:601–609
Downey DG, Bell SC, Elborn JS (2009) Neutrophils in cystic fibrosis. Thorax 64:81–88
Chambers JK, Macdonald LE, Sarau HM, Ames RS, Freeman K, Foley JJ, Zhu Y, McLaughlin MM, Murdock P, McMillan L, Trill J, Swift A, Aiyar N, Taylor P, Vawter L, Naheed S, Szekeres P, Hervieu G, Scott C, Watson JM, Murphy AJ, Duzic E, Klein C, Bergsma DJ, Wilson S, Livi GP (2000) A G protein-coupled receptor for UDP-glucose. J Biol Chem 275:10767–10771
Lazarowski ER, Harden TK (2015) UDP-sugars as extracellular signaling molecules: cellular and physiologic consequences of P2Y14 receptor activation. Mol Pharmacol 88:151–160
Carter RL, Fricks IP, Barrett MO, Burianek LE, Zhou Y, Ko H, Das A, Jacobson KA, Lazarowski ER, Harden TK (2009) Quantification of Gi-mediated inhibition of adenylyl cyclase activity reveals that UDP is a potent agonist of the human P2Y14 receptor. Mol Pharmacol 76:1341–1348
Harden TK, Sesma JI, Fricks IP, Lazarowski ER (2010) Signalling and pharmacological properties of the P2Y14 receptor. Acta Physiol (Oxford) 199:149–160
Moore DJ, Murdock PR, Watson JM, Faull RL, Waldvogel HJ, Szekeres PG, Wilson S, Freeman KB, Emson PC (2003) GPR105, a novel Gi/o-coupled UDP-glucose receptor expressed on brain glia and peripheral immune cells, is regulated by immunologic challenge: possible role in neuroimmune function. Brain Res Mol Brain Res 118:10–23
Skelton L, Cooper M, Murphy M, Platt A (2003) Human immature monocyte-derived dendritic cells express the G protein-coupled receptor GPR105 (KIAA0001, P2Y14) and increase intracellular calcium in response to its agonist, uridine diphosphoglucose. J Immunol 171:1941–1949
Lee BC, Cheng T, Adams GB, Attar EC, Miura N, Lee SB, Saito Y, Olszak I, Dombkowski D, Olson DP, Hancock J, Choi PS, Haber DA, Luster AD, Scadden DT (2003) P2Y-like receptor, GPR105 (P2Y14), identifies and mediates chemotaxis of bone-marrow hematopoietic stem cells. Genes Dev 17:1592–1604
Gao ZG, Ding Y, Jacobson KA (2010) UDP-glucose acting at P2Y14 receptors is a mediator of mast cell degranulation. Biochem Pharmacol 79:873–879
Scrivens M, Dickenson JM (2006) Functional expression of the P2Y(14) receptor in human neutrophils. Eur J Pharmacol 543:166–173
Okada SF, Zhang L, Kreda SM, Abdullah LH, Davis CW, Pickles RJ, Lazarowski ER, Boucher RC (2011) Coupled nucleotide and mucin hypersecretion from goblet cell metaplastic human airway epithelium. Am J Respir Cell Mol Biol 45:253–260
Lazarowski ER (2010) Quantification of extracellular UDP-galactose. Anal Biochem 396:23–29
Sesma JI, Esther CR Jr, Kreda SM, Jones L, O’Neal W, Nishihara S, Nicholas RA, Lazarowski ER (2009) ER/golgi nucleotide sugar transporters contribute to the cellular release of UDP-sugar signaling molecules. J Biol Chem 284:12572–12583
Kreda SM, Seminario-Vidal L, Heusden C, Lazarowski ER (2008) Thrombin-promoted release of UDP-glucose from human astrocytoma cells. Br J Pharmacol 153:1528–1537
Esther CR Jr, Sesma JI, Dohlman HG, Ault AD, Clas ML, Lazarowski ER, Boucher RC (2008) Similarities between UDP-glucose and adenine nucleotide release in yeast: involvement of the secretory pathway. Biochemistry 47:9269–9278
Kreda SM, Okada SF, van Heusden CA, O’Neal W, Gabriel S, Abdullah L, Davis CW, Boucher RC, Lazarowski ER (2007) Coordinated release of nucleotides and mucin from human airway epithelial Calu-3 cells. J Physiol 584:245–259
Lazarowski ER, Shea DA, Boucher RC, Harden TK (2003) Release of cellular UDP-glucose as a potential extracellular signaling molecule. Mol Pharmacol 63:1190–1197
Sesma JI, Kreda SM, Steinckwich-Besancon N, Dang H, Garcia-Mata R, Harden TK, Lazarowski ER (2012) The UDP-sugar-sensing P2Y14 receptor promotes Rho-mediated signaling and chemotaxis in human neutrophils. Am J Phys Cell Physiol 303:C490–C498
Barrett MO, Sesma JI, Ball CB, Jayasekara PS, Jacobson KA, Lazarowski ER, Harden TK (2013) A selective high-affinity antagonist of the P2Y14 receptor inhibits UDP-glucose-stimulated chemotaxis of human neutrophils. Mol Pharmacol 84:41–49
Loughlin CE, Esther CR Jr, Lazarowski ER, Alexis NE, Peden DB (2010) Neutrophilic inflammation is associated with altered airway hydration in stable asthmatics. Respir Med 104:29–33
Esther CR, Alexis NE, Clas ML, Lazarowski ER, Donaldson SH, Pedrosa Ribeiro CM, Moore CG, Davis SD, Boucher RC (2008) Extracellular purines are biomarkers of neutrophilic airway inflammation. Eur Respir J 31:949–956
Lazarowski ER, Boucher RC, Harden TK (2000) Constitutive release of ATP and evidence for major contribution of ecto-nucleotide pyrophosphatase and nucleoside diphosphokinase to extracellular nucleotide concentrations. J Biol Chem 275:31061–31068
Mall M, Grubb BR, Harkema JR, O’Neal WK, Boucher RC (2004) Increased airway epithelial Na + absorption produces cystic fibrosis-like lung disease in mice. Nat Med 10:487–493
Jones LC, Moussa L, Fulcher ML, Zhu Y, Hudson EJ, O’Neal WK, Randell SH, Lazarowski ER, Boucher RC, Kreda SM (2012) VAMP8 is a vesicle SNARE that regulates mucin secretion in airway goblet cells. J Physiol 590:545–562
Livraghi A, Grubb BR, Hudson EJ, Wilkinson KJ, Sheehan JK, Mall MA, O’Neal WK, Boucher RC, Randell SH (2009) Airway and lung pathology due to mucosal surface dehydration in {beta}-epithelial Na + channel-overexpressing mice: role of TNF-{alpha} and IL-4R{alpha} signaling, influence of neonatal development, and limited efficacy of glucocorticoid treatment. J Immunol 182:4357–4367
Zhou Z, Treis D, Schubert SC, Harm M, Schatterny J, Hirtz S, Duerr J, Boucher RC, Mall MA (2008) Preventive but not late amiloride therapy reduces morbidity and mortality of lung disease in betaENaC-overexpressing mice. Am J Respir Crit Care Med 178:1245–1256
Anderson WH, Coakley RD, Button B, Henderson AG, Zeman KL, Alexis NE, Peden DB, Lazarowski ER, Davis CW, Bailey S, Fuller F, Almond M, Qaqish B, Bordonali E, Rubinstein M, Bennett WD, Kesimer M, Boucher RC (2015) The relationship of mucus concentration (hydration) to mucus osmotic pressure and transport in chronic bronchitis. Am J Respir Crit Care Med 192:180–190
Picher M, Burch LH, Boucher RC (2004) Metabolism of P2 receptor agonists in human airways: implications for mucociliary clearance and cystic fibrosis. J Biol Chem 279:20234–20241
Fausther M, Pelletier J, Ribeiro CM, Sevigny J, Picher M (2010) Cystic fibrosis remodels the regulation of purinergic signaling by NTPDase1 (CD39) and NTPDase3. Am J Physiol Lung Cell Mol Physiol 298:L804–L818
Mall MA, Harkema JR, Trojanek JB, Treis D, Livraghi A, Schubert S, Zhou Z, Kreda SM, Tilley SL, Hudson EJ, O’Neal WK, Boucher RC (2008) Development of chronic bronchitis and emphysema in beta-epithelial Na + channel-overexpressing mice. Am J RespirCrit Care Med 177:730–742
Livraghi-Butrico A, Kelly EJ, Klem ER, Dang H, Wolfgang MC, Boucher RC, Randell SH, O’Neal WK (2012) Mucus clearance, MyD88-dependent and MyD88-independent immunity modulate lung susceptibility to spontaneous bacterial infection and inflammation. Mucosal Immunol 5:397–408
Evans CM, Koo JS (2009) Airway mucus: the good, the bad, the sticky. Pharmacol Ther 121:332–348
Yoshida T, Tuder RM (2007) Pathobiology of cigarette smoke-induced chronic obstructive pulmonary disease. Physiol Rev 87:1047–1082
Rollins BM, Burn M, Coakley RD, Chambers LA, Hirsh AJ, Clunes MT, Lethem MI, Donaldson SH, Tarran R (2008) A2B adenosine receptors regulate the mucus clearance component of the lung’s innate defense system. Am J Respir Cell Mol Biol 39:190–197
Freeman K, Tsui P, Moore D, Emson PC, Vawter L, Naheed S, Lane P, Bawagan H, Herrity N, Murphy K, Sarau HM, Ames RS, Wilson S, Livi GP, Chambers JK (2001) Cloning, pharmacology, and tissue distribution of G-protein-coupled receptor GPR105 (KIAA0001) rodent orthologs. Genomics 78:124–128
Arase T, Uchida H, Kajitani T, Ono M, Tamaki K, Oda H, Nishikawa S, Kagami M, Nagashima T, Masuda H, Asada H, Yoshimura Y, Maruyama T (2009) The UDP-glucose receptor P2RY14 triggers innate mucosal immunity in the female reproductive tract by inducing IL-8. J Immunol 182:7074–7084
Saini Y, Dang H, Livraghi-Butrico A, Kelly EJ, Jones LC, O’Neal WK, Boucher RC (2014) Gene expression in whole lung and pulmonary macrophages reflects the dynamic pathology associated with airway surface dehydration. BMC Genomics 15:726
Zimmermann H, Zebisch M, Strater N (2012) Cellular function and molecular structure of ecto-nucleotidases. Purinergic Signal 8:437–502
Zuo P, Picher M, Okada SF, Lazarowski ER, Button B, Boucher RC, Elston TC (2008) Mathematical model of nucleotide regulation on airway epithelia. Implications for airway homeostasis. J Biol Chem 283:26805–26819
Corriden R, Chen Y, Inoue Y, Beldi G, Robson SC, Insel PA, Junger WG (2008) Ecto-nucleoside triphosphate diphosphohydrolase 1 (E-NTPDase1/CD39) regulates neutrophil chemotaxis by hydrolyzing released ATP to adenosine. J Biol Chem 283:28480–28486
Picher M, Burch LH, Hirsh AJ, Spychala J, Boucher RC (2003) Ecto 5′-nucleotidase and non-specific alkaline phosphatase: two AMP-hydrolyzing ectoenzymes with distinct roles in human airways. J Biol Chem 278:13468–13479
Seminario-Vidal L, van Heusden C, Mugesh G, Lazarowski ER (2010) Ebselen is a potent non-competitive inhibitor of extracellular nucleoside diphosphokinase. Purinergic Signal 6:383–391
Fricks IP, Carter RL, Lazarowski ER, Harden TK (2009) Gi-dependent cell signaling responses of the human P2Y14-receptor in model cell systems. J Pharmacol Exp Ther 330:162–168
Acknowledgments
The authors are grateful to Dr. Silvia Kreda and Dr. Michael Chua (Histology/Microscopy Core) for the use of the Nikon Nicrophot-SA microscopy, Dr. Wanda O’Neal and Kristen Wilkinson (Mouse Core) for assisting with the βENaC-Tg mouse studies, and to Catharina van Heusden for technical assistance with the use of the HPLC.
This work was supported by the National Institutes of Health (NIH) National Institute of General Medical Sciences [R01-GM38213] (TKH), the NIH National Heart, Lung, and Blood Institute [P01-HL110873] (ERL), the National Institute of Diabetes and Digestive and Kidney Diseases Intramural Research Program (KAJ), the NIH Specialized Centers of Clinically Orientated Research [P50-HL084934] (SD), the US EPA cooperative agreement CR 833463015-35475 and NHLBI-RO1 HL080337 (NEA), and the American Cystic Fibrosis Foundation [SESMA1510] and North Carolina Translational & Clinical Science [NCTraCS 550KR101513] (JIS). The Histology/Microscopy and Mouse Cores were supported by NIH P30-DK065988.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All subjects were studied at the University of North Carolina at Chapel Hill (Chapel Hill, NC, USA), and studies were approved by the Institutional Review Board. Animal protocols were reviewed and approved by the Institutional Animal Care and Use Committee of the University of North Carolina at Chapel Hill.
Conflict of interest
The authors declare that they have no competing interests.
Electronic supplementary material
Supplemental Figure 1
(DOCX 34 kb)
Rights and permissions
About this article
Cite this article
Sesma, J.I., Weitzer, C.D., Livraghi-Butrico, A. et al. UDP-glucose promotes neutrophil recruitment in the lung. Purinergic Signalling 12, 627–635 (2016). https://doi.org/10.1007/s11302-016-9524-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11302-016-9524-5