Abstract
Objectives
The aim of this study was to evaluate, using cone-beam computed tomography (CBCT), the relationship of persistent foramen tympanicum (PFT) with degenerative changes in the temporomandibular joint (TMJ) and the presence of pneumatized glenoid fossae and articular eminences.
Method
Two experienced oral and maxillofacial radiologists evaluated 510 CBCT scans, from which 94 patients were divided into two groups: G1—patients with PFT and G2—control group. The location of the PFT, presence, or absence of degenerative TMJ changes and morphology were evaluated. Similarly, all images were evaluated for the presence of pneumatized articular eminence and glenoid fossa. The Chi-square test and Fisher’s Exact test were used for the categorical variables. A multinomial logistic regression model was performed for subgroup analysis. To assess the estimation-chance occurrence of TMJ alterations the Odds Ratio analysis was used.
Results
Statistically significant results were found for erosion, planning, and subchondral cyst. Regarding TMJ morphology, significant results were found for: round, flat, and others. Moreover, it was possible to observe that patients who had the PFT were approximately 48 times more likely to manifest TMJ alterations and approximately 3 times more likely to manifest articular eminence pneumatization.
Conclusion
Since individuals who have FTP have a greater chance of having TMJ and PEA changes, it is important for the dental radiologist to be aware of these signs in CBCT scans for a correct diagnosis.
Trial registration number
CAAE: 34328214.3.0000.0104 (11/30/2014).
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The foramen tympanicum (FT), also known as the foramen of Huschke, described for the first time in 1889 by Emil Huschke, is an anatomic variation that affects adult individuals [1,2,3,4]. Usually, it is present in newborns and closes at around 5 years of age [5], but, in some cases, it may persist till adulthood, considered then an anatomic anomaly, particularly known as persistent foramen tympanicum (PFT) in adults [6,7,8].
This structure is found in the tympanic plaque of the temporal bone, in the anteroinferior region of the external acoustic meatus (EAM), posteromedial to the temporomandibular joint (TMJ), connecting the EAM with the glenoid fossa, where the TMJ is located [1, 2, 9].
The cause for PFT is uncertain, but some factors such as gender, age, ethnicity, and craniofacial discrepancies seem to be associated [3, 10,11,12]. Commonly, this anatomic variation is asymptomatic, hence neglected [9]. However, some authors attribute its persistence to the appearance of alterations like fistula and TMJ herniation, infectious arthritis, ear external, and medial inflammation [2]. Besides that, there is also the possibility of facilitating the propagation of infections and neoplastic cells from the EAM to the infratemporal fossa [4, 13].
It was observed in the scientific literature that the use of panoramic radiographs makes it impossible to identify the FT, since it is an examination that causes superimpositions in adjacent structures, such as the temporal bones [14]. That being said, when the visualization of EAM and medial ear structures is essential, CBCT scans are considered the best option [15]. For this reason, CBCT is an extremely valid option for FT analysis, seeing that, depending on the field of view (FOV) used, it allows the visualization of a greater area of the facial skeleton, beyond the limits of any radiograph, or even a small focused area of clinical interest, without the structures overlapping [6].
Given that the persistence of this foramen in adulthood may be related to various issues in adjacent structures [2, 4, 13], the acknowledgment of this anatomic anomaly is extremely important for doctors, dentists, and radiologists. The comprehension of this variation could help discover the origin of complications in the region, making it easier to diagnose and also direct the treatment, when necessary [4, 16].
There may be a possibility of changes in the bone structures in the TMJ region, due to recurring infections and local inflammations. Nevertheless, as analyzing the scientific literature, not many studies have been found evaluating the correlation between inflammation’s persistence because of regional morphologic alterations [17].
Therefore, the objective of this study is to evaluate the relationship between PFT with the TMJ degenerative alterations, the presence of pneumatization of the glenoid fossa and the articular eminence and the mandibular condyle’s morphology. The null hypothesis established is that PFT is not associated with the TMJ, degenerative alterations, the presence of pneumatized glenoid fossa (PGF) and pneumatized articular eminence (PAE) or the mandibular condyle’s morphology.
Materials and methods
Ethical approval
This project was sent and approved by the Standing Ethics Committee in Research Involving Human Beings of the State University of Maringa under the number CAAE: 34328214300000104.
Sample
The present study, of observational and retrospective character, used CBCT scans performed at the Clinical Research Image Laboratory (CRIL), of the Health Technology Centre (HTC), of the Complex of Research Support Centers (CRSC) of the State University of Maringa. The images were performed by a professional specialist in Oral and Maxillofacial Radiology. The images were obtained by the equipment i-CAT Next Generation® (Imaging Sciences International, Hatfield, PA, EUA), 300 µ of isometric voxel, FOV of 17 × 23 cm, tube tension of 120 kVp, and tube current of 3–8 mA.
The sample consists of 510 CBCT scans, performed from 2014 to 2019. The inclusion criteria were: patients with PFT, scans that included the ear and the TMJ region and scans where patients were in maximum intercuspation [16]. The exclusion criteria were: patients under 18, with history of TMJ surgical procedures, orthognathic surgery, facial traumas, craniofacial syndromes, orofacial pain, and other maxillofacial pathologies [16].
Database evaluation
Every evaluation was performed independently by two examiners, of the oral and maxillofacial radiology area, who registered the presence or absence of alteration in each TMJ. Previous to the analysis, 10% of the sample was used for randomized calibration. The evaluations were performed in duplicate with a 2-week pause and only 10 scans were examined each day to avoid eyestrain. In cases of divergence between the classifications, a third evaluator was consulted.
The evaluations were performed in a silent and low-light environment. The software CS 3D Suite Imaging (Carestream Dental LLC Atlanta, GA, USA), in a computer with Original Windows 11 Home Single Language (Microsoft Corp., Redmond, A, EUA), Intel® Core™ i5-10300H 10th generation (Intel Corporation, EUA), NVIDIA® GeForce® GTX 1650TI GPU (4 GB GDDR5) (NVIDIA Corporation, EUA) and a 15.6" Full HD 120 Hz 65% sRGB screen was used.
Tools such as contrast and brightness were adjusted as needed to guarantee an ideal visualization in the software. The data concerning gender (male and female) and age was collected. The CBCT scans were analyzed searching for the existence of FT, presence or absence of TMJ alterations and the alterations found [11]. Besides that, it evaluated the presence of PAE and PGF, uni or multilocular. The morphology of the mandibular condyle was also verified, being classified in convex, round, plain or angled.
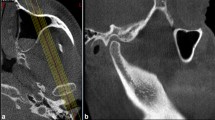
Evaluation of the presence of the foramen tympanicum
Out of 510 analyzed CBCT scans, 47 showed PFT and formed the first group (G1), next to it, 47 scans of patients who did not present PFT were randomly selected (Fig. 1), to form the control group (G2), making the total number of 94 CBCT scans. The identification of PFT was performed in the axial, coronal and sagittal reconstructions [11]. When the FT was present, the prevalence was calculated in relation to the degenerative alterations of the TMJ, the presence of PGF and PAE and the morphology of the mandibular condyle.
Evaluation of the mandibular condyle
The mandibular condyles were examined according to the criteria of diagnosis Research Diagnostic Criteria for Temporomandibular Disorders (RDC/TMD) published in 1992 by Samuel F. Dworkin and Linda LeResche [18]. That way, they were classified according to the following alterations and/or imaging findings (Fig. 2):
-
1.
flattening;
-
2.
formation of osteophytes or loose joint bodies;
-
3.
erosion, deviation in shape;
-
4.
subcortical sclerosis;
-
5.
generalized sclerosis;
-
6.
subcortical cysts;
-
7.
hyperplasia or hypoplasia of the condyle;
-
8.
bone ankylosis.
A Condylar flattening (parasagittal reconstruction); B Subchondral cyst (paracoronal reconstruction); C Condyle with osteophyte (parasagittal reconstruction); D Condylar subcortical sclerosis (parasagittal reconstruction); E Condylar erosion (parasagittal reconstruction); F Condylar hypoplasia (parasagittal reconstruction) and G Bifid head of the mandible (paracoronal reconstruction)
In case of condyle hyper or hypoplasia, the morphology is within normality, but its size is bigger or smaller, respectively [7]. The deviation in shape is defined as a shape alteration non attributable to flattening, such as erosive alterations, osteophytes, hyperplasia, or hypoplasia [7]. To ratify the presence of all these characteristics, hard-tissue alterations were observed in at least two consecutive sections.
The evaluation of the morphology of the mandibular condyle was performed from the coronal sections and classified as convex, round, plain, angled and other.
No examples of loose joint bodies, condylar hyperplasia, or bone ankylosis were found in this study.
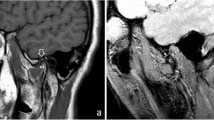
Evaluation of the presence of pneumatized articular eminence and roof of glenoid fossa
The presence and frequency of PAE and the roof of the glenoid fossa were also evaluated. For that, the analysis was performed in both the right and left TMJ of each patient. The axial, coronal, and sagittal reconstructions were used for visualization.
The diagnosis of PAE was made only when the following characteristics were found in the image [19, 20] a hypodense area in the zygomatic process of the temporal bone with an appearance similar to that of mastoid air cells, extending anteriorly to the articular eminence, but no further from the zygomatic-temporal suture, without augmentation or destruction of the zygoma cortices. The PGF was considered when the radiolucent defect was located in the roof of the glenoid fossa, above the condyle (Fig. 3).
A absence of pneumatization in the articular eminence and in the roof of the glenoid fossa (parasagittal reconstruction); B multilocular pneumatization of the roof of the glenoid fossa (parasagittal reconstruction); C unilocular pneumatization of the glenoid fossa (axial reconstruction); D unilocular pneumatization of the articular eminence (parasagittal reconstruction) and E unilocular pneumatization of the articular eminence (axial reconstruction)
The pneumatization was also classified as unilocular (a single oval and hypodense defect with well-defined limits) or multilocular (numerous minor-hypodense cavities) (Fig. 3).
Statistical analysis
A descriptive statistical analysis was initially performed to extract the initial data information. The Chi-squared test and the Fisher exact test were used for the categorical variables. A multinomial logistic regression model was used for the subgroup analysis. An occurrence Odds Ratio analysis of category of j answer in relation to the category r, pj (x)/pr (x), j = 1, 2, 3, 4 and r = 5, considering the PFT, was used to evaluate the estimative occurrence of TMJ alterations, PAE and PGF. The level of significance of 95% was established in P value ≤ 0.05.
Results
The age of the participants ranged from 18 to 65 years of age. The average age of the group with PFT was 41.21 (± 16.20) years. The age average of the control group was 40.10 (± 13.05) years. In the male group, 36 participants were allocated, with 12 (25.53%) belonging to the group with PFT and 24 (51.06%) belonging to the control group, totaling 38.30% of the sample. In the female group, 58 participants were included, with 35 (74.47%) in the PFT group and 23 (48.94%) in the control group, accounting for 61.70% of the total sample (Table 1).
In Table 2, it is noticeable the significant differences between the presence of TMJ alterations and PAE of individuals from groups G1 and G2 (P value < 0.0001). However, there was no significant difference related to PGF.
Table 3 shows there were significant differences between the type of TMJ alterations of individuals with PFT (G1) and control group (G2), being more frequent in the group with PFT. The alterations which had statistically significant results were: erosion (P < 0.0001), flattening (P < 0.0001), and subchondral cyst (P = 0.0007).
In Table 4, it is observed that there is a predominance of the convex type in both groups, with a statistically significant difference for morphology types round and plain (Table 5).
To obtain Odds Ratio estimates, both G1 and G2 individuals were considered (Table 6).
In Table 6, it is observed that there is a superior proportion of G1 patients presenting TMJ alteration and PAE, verifying (OR = 48.94 and OR = 3.25, respectively) the greater chance of presenting alterations (48 times more chance of presenting TMJ alterations and approximately 3 times more chances of presenting PAE). As to the PGF (Odds Ratio) occurring chances between G1 and G2 individuals, there were no statistically significant differences (OR = 0.679).
Discussion
The present study had as an objective the evaluation of CBCT scans for the relationship between PFT and TMJ degenerative changes (erosion, flattening, osteophyte, sclerosis, condylar hypoplasia, and subchondral cyst), presence of PAE, PGF, and mandibular condyle morphology.
Some authors suggest that individuals with facial skeletal patterns class II and III present with some degenerative joint diseases and/or signs and symptoms of temporomandibular disorder (TMD) with a significant major frequency [20, 21], making it necessary to perform TMJ procedures with major frequency in these individuals [22]. Alternatively, the presence of FT and pneumatized TMJ osseous components may be considered as potential complicating factors in clinical and surgical procedures in the temporal bone region, which reinforces the importance of acknowledging this alteration in imaging examination [16], as well as the pneumatized TMJ osseous components [8].
It is known that several studies have evaluated the presence of FT using dry skulls [16, 23,24,25]. These analyses were made visually, presenting a prevalence of 4% to 16% [16, 23,24,25]. Other studies, performed PFT evaluations from imaging scans [4, 11, 16, 26] Using helical computed tomography, it was found around 13% of prevalence of this alteration [4], but within CBCT studies, this number varied from 3 to 22% [11, 16, 26]. Recently, the research from Herreira-Ferreira et al. evaluated the PFT from CBCT scans and found a prevalence of 9.7% in a sample with over 500 patients [16].
Since the panoramic radiograph is not indicated for PFT evaluation [14], and is not the ideal examination for evaluation of the TMJ region, the present study used CBCT scans for analysis. This imaging exam provides high resolution, which permits evaluation of multiplanar reconstructions (axial, sagittal and coronal), it eliminates the superimposition of other anatomic structures and distortions. In comparison with helical tomography, CBCT presents a lower cost, less acquisition time and radiation doses [11, 26]. This technology is considered the gold standard for the TMJ and tympanic region osseous components [26].
In this study, it was observed that there was a predilection of PFT for females, which composed about 74% of the sample. This data agrees with the findings of scientific literature [3, 4, 11, 13, 16, 25, 26]. According to some authors, this prevalence to females may be explained due to the structural growth pattern being different between genders [1, 13].
No studies were found in the scientific literature that correlated PFT with TMJ alterations, ATM morphology, PAE and PGF from a pre-selected sample. This study performed all of these correlations. Statistically, this research has found a correlation between PFT and TMJ changes, in which 97.87% of individuals (n = 46) presented some kind of alteration, which is statistically significant (P < 0.0001) in comparison to group G2 (n = 23).
The findings of this work corroborate with Hasani et al. who found in a TMD patient a greater prevalence of FT (3.4%) in comparison to patients without TMD (0.8%). According to the author, this greater prevalence of FT in TMD patients may suggest a possible mechanism to TMJ disturbance development, which may be affected by the presence of FT [27]. In this work, by analyzing the chances of these individuals with PFT of presenting with TMJ changes, it was found that there is 48.94 times more chances (P = 0.0001) of occurrence than in group G2, according to this theory.
Among the found alterations, the flattening occurred in 45 TMJs (36.88%, P < 0.0001) followed by 43 TMJs with erosion (35.26%, P < 0.0001), it is statistically significant when compared to group G2 (n = 14 e n = 5, respectively). These results corroborate with the findings of Mathew et al., Shahab et al., Belgin et al. and disagree with Nah which related sclerosis to be the most common osseous alteration followed by erosion and according to Çakur et al. erosion followed by sclerosis [28,29,30,31,32].
Through the years, the causes and primary physiopathology of TMD has been a controversial subject [27]. It is suggested that besides PFT, a possible association between occlusal factors (bruxism and clenching), psychologic factors (depression and anxiety), hormonal factors (estrogen receptors in female TMJ), and trauma [33,34,35]. In the literature, there are reports of patients with existing TMJ symptoms without history of trauma or surgery, and in CBCT scans showing TMJ herniation from FT to EAM [36, 37]. According to some authors this herniation of the TMJ soft tissues to EAM may be associated with PFT and may be a predisposing factor to TMD [32, 38,39,40].
The pre-surgical detection of FT presence is of great importance to doctors and oral and maxillofacial surgeons who perform ear and TMJ surgery [27]. During TMJ arthroscopy, endoscopes smaller than 3 mm in diameter can penetrate the FT and cause a series of complications, including injury to the tympanic segment of the facial nerve [41].
It is noticeable that, even though this subject is of extreme importance, literature is short of studies about the presence of FT in TMD patients, the relations between TMJ abnormality is not clear, therefore, requiring more studies and awareness of the possible occurrence of TMD where FT is present [27].
As to the mandibular condyle morphology, it was found a great occurrence of the convex type for group G1 (58.51%, n = 55) as for group G2 (46.80%, n = 44). It is possible to speculate to the present moment that FT presence does not interfere with mandibular condyle morphology.
In CBCT studies, Miloglu et al., Rezende Barbosa et al. and Khojastepour et al. found varied prevalence rates of PAE (between 8% and 76.7%), without having compared PFT [20, 42, 43]. In this study, the G1 group individuals presented 46.80% (n = 22) of PAE, while group G2 presented 22.30% (n = 10), showing statistical significance (P = 0.009). As a consequence of the values found, it is possible to infer that the chances of an individual who has FT is 3.25 times (P = 0.016) greater than an individual without FT to have PAE. The found data corroborate with Koç et al. as they studied the FT prevalence and analyzed its association with pneumatization volume in the anterior part of the mastoid segment [20]. It was found that FT patients had a significantly greater pneumatization volume of the mastoid segment than the control group. If followed, this logic may explain the occurrence of pneumatization in PFT individuals.
When PAE was present, the similarity of some previous studies [8, 20, 22], the multilocular type mostly found in group G1 (23.41%, n = 22). This difference is statistically significant (P = 0.005) in group G2 (8.51%, n = 8). According to Tyndall and Matteson, a possible explanation for this major occurrence of pneumatized articular eminence is the fact that it is adjacent to the mastoid process, in which pneumatization is multilocular. This also explains the major occurrence of the multilocular type [19].
Furthermore, when it comes to PGF, it was only evaluated in the most recent studies, since it became possible due to the advent of CBCT [20]. Its major prevalence was reported in the study of Chicarelli et al. which found pneumatization in 62.9% of the cases [8]. In the present study, PGF prevalence was 44.7% (n = 21) in group G1 and 51.06% (n = 24) in group G2. No statistically significant difference was found. When present, in group G1 (36.18%, n = 34) and group G2 (28.72%, n = 2), the multilocular type was the most found, being compatible with the findings of other studies [8, 20]. The results show that the chances of an individual with PFT regardless PGF are the same as an individual without PFT (Odds Ratio = 0.77). These data reinforce the importance of knowing pneumatization can also occur in the glenoid fossa and present the same clinical implications [20].
These results found concerning the occurrence of pneumatization are important not only in cases of surgical necessity but also due to the fact that these anatomic variations may facilitate the propagation of tumors, inflammations, and increase the risk of fractures, because of the reduced resistance of these structures [20].
Finally, intra-articular inflammatory or non-inflammatory diseases can contribute to joint damage. In this sense, studies conducted with magnetic resonance imaging (MRI), may be able to reveal more details in hard and soft tissue.
The limitations of this study include its retrospective characteristics and clinical aspects. Hormonal disorders such as menopause and pregnant patients, osseous alterations such as osteopenia, osteoporosis, calcium metabolism abnormalities, which could not be screened in these patients can influence joint pathologies. Although every effort has been made to minimize or avoid any type of biases, prospective studies are needed to investigate these associations. Furthermore, the development of clinical studies is opportune to deepen the knowledge of the reason why these TMJ alterations and articular eminence pneumatization happen more frequently in patients with PFT.
Conclusion
From the results, it is possible to conclude that individuals with PFT have greater chance of developing TMJ alterations and PAE. Besides that, there does not seem to be a correlation between PFT and mandibular condyle morphology or PGF. Hence, it is important that the radiologist is attentive to these signs in CBCT exams to diagnose correctly.
References
Lacout A, Marsot-Dupuch K, Smoker WR, Lasjaunias P. Foramen tympanicum or foramen of Huschke: pathologic cases and anatomic CT study. Am J Neuroradiol. 2005;26:1317–23.
Akcam T, Hidir Y, Ilica AT, Kilic E, Sencimen M. Temporomandibular joint herniation into the external ear canal through foramen of Huschke. Auris Nasus Larynx. 2011;38:646–9.
Hashimoto T, Ojiri H, Kawai Y. The foramen of Huschke: age and gender specific features after childhood. Int J Oral Maxillofac Surg. 2011;40:743–6.
Ertugrul S, Keskin NK. Relationship of age to foramen of Huschke and investigation of the development of spontaneous temporomandibular joint herniation. Int J Oral Maxillofac Surg. 2019;48:534–9.
Williams PL, Warwick R, Dyson M, Bannister LH. GRAY Anatomy. Rio de Janeiro: Guanabara; 1995.
Ahmad M, Jenny J, Downieà M. Application of cone beam computed tomography in oral and maxillofacial surgery. Aust Dent J. 2012;57:82–94.
Ahmad L, Hollender Q, Anderson Q, Kartha K, Ohrbach R, Truelove ED, John MT, Schiffman EL. Research diagnostic criteria for temporomandibular disorders (RDC/TMD): development of image analysis criteria and examiner reliability for image analysis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;107:844–60.
Chicarelli M, França VTB, Walewski LA, Iwaki LCV, Tolentino ES. Temporal bone pneumatization in patients with dentofacial deformities: cone beam computed tomography study. Int J Oral Maxillofac Surg. 2019;48:1564–9.
Bhanu PS, Sankar KD. Incidence of Foramen of Huschke in South Andhra Population of India. J Clin Diagn Res. 2016;10:1–3.
Park YH, Kim HJ, Park MH. Temporomandibular joint herniation into the external auditory canal. Laryngoscope. 2010;120:2284–8.
Akbulut N, Kursun S, Aksoy S, Kurt H, Orhan K. Evaluation of foramen tympanicum using cone-beam computed tomography in orthodontic malocclusions. J Craniofac Surg. 2014;25:105–9.
Olarinoye-Akorede SA, Olanrewaju IS, Suleiman AO. Forame de Huschke (tímpano) em um homem nigeriano com herniação articular de partes moles no conduto auditivo externo. Ann Afr Med. 2014;13:226–8.
Deniz Y, Geduk G, Zengin AZ. Examination of foramen tympanicum: an anatomical study using cone-beam computed tomography. Folia Morphol (Warsz). 2018;77:335–9.
Hawke M, Kwok P, Mehta M, Wang RG. Bilateral spontaneous temporomandibular joint herniation into the external auditory canal. J Otolaryngol. 1987;16:387–9.
Greene MW, Hackney FL, Van Sickels JE. Arthroscopy of the temporomandibular joint: an anatomic perspective. J Oral Maxillofac Surg. 1989;47:386–9.
Herreira-Ferreira M, Tolentino ES, da Silva MC, Walewski LÂ, Iwaki LCV. Cone-beam computed tomographic study of the persistent foramen tympanicum according to age, sex, and skeletal patterns. Br J Oral Maxillofac Surg. 2020;58:57–61.
Meazzini MC, Brusati R, Caprioglio A, Diner P, Garattini G. True hemifacial microsomia and hemimandibular hypoplasia with condylar-coronoid collapse: Diagnostic and prognostic differences. AJO-DO. 2011;139(435):447.
Schiffman E, Ohrbach R, Truelove E, et al. Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) for Clinical and Research Applications: recommendations of the International RDC/TMD Consortium Network and Orofacial Pain Special Interest Group. J Oral Facial Pain Headache. 2014;28(1):6–27. https://doi.org/10.11607/jop.1151.
Tyndall SA, Matteson SR. Radiographic appearance and population distribution of the pneumatized articular eminence of the temporal bone. J Oral Maxillofac Surg. 1985;43:493–7.
Ladeira DB, Barbosa GL, Nascimento MC, Cruz AD, Freitas DQ, Almeida SM. Prevalence and characteristics of pneumatization of the temporal bone evaluated by cone beam computed tomography. Int J Oral Maxillofac Surg. 2013;42:771–5.
Manfredini D, Segù M, Arveda N, Lombardo L, Siciliani G, Rossi A, Guarda-Nardini L. Temporomandibular joint disorders in patients with different facial morphology A systematic review of the literature. J Oral Maxillofac Surg. 2016;74(29):46.
Orhan K, Oz U, Orhan AI, Ulker AE, Delibasi C, Akcam O. Investigation of pneumatized articular eminence in orthodontic malocclusions. Orthod Craniofacial Res. 2010;13:56–60.
Wang RG, Bingham B, Hawke M, Kwok P, Li JR. Persistence of the foramen of Huschke in the adult: an osteological study. J Otolaryngol. 1991;20:251–3.
Rezaian J, Namavar MR, VahdatiNasab V, Nobari ARH, Abedollahi A. Foramen tympanicum or foramen of huschke: a bioarchaeological study on human skeletons from an iron age cemetery at tabriz kabud mosque zone. Iran J Med Sci. 2015;40:367–71.
Ribeiro TMC, Freire AR, Junior ED, Botacin PR, Prado FB, Rossi AC. Foramen tympanicum prevalence in the population of Southeast Brazil: a morphological study in computed tomography scans. Folia Morphol. 2022;17:1042–6.
Lima AT, Leme TC, Barbieri AA, et al. Prevalence of tympanic foramen (or of Huschke) in a Brazilian population: study by cone beam computed tomography. Brazilian Dental Science. 2018;21:204–9.
Hasani M, Hadhnegahdar A, Khojastepour L, Haghighi MJG. Determining the existence of the foramen of Huschke in patients with temporomandibular joint disorders using cone beam computed tomography: retrospective cohort study. BMC Med Imaging. 2022;22:145.
Belgin CA, Serindere G, Aksoy S. Evaluation of the relationship between tympanic plate morphology and degenerative bone changes of condyle and articular eminence. J Stomatol Oral Maxillofac Surg. 2021;122:24–8.
Mathew AL, Sholapurkar AA, Pai KM. Condylar changes and its association with age, TMD, and dentition status: a cross-sectional study. Int J Dent. 2011;2011:413639.
Shahab S, Azizi Z, Damghani FT, Damghani FT. Prevalence of osseous changes of the temporomandibular joint in CBCT images of patients with and without temporomandibular disorders. Biosci Biotech Res Comm. 2017;10:518–24.
Nah KS. Condylar bony changes in patients with temporomandibular disorders: a CBCT study. Imaging Sci Dent. 2012;42:249–53.
Çakur B, Sümbüllü MA, Durna D, Akgül HM. Prevalência dos tipos de fissura petrotimpânica na disfunção da articulação temporomandibular. Acta radiol. 2011;52:562–5.
Gauer R, Semidey MJ. Diagnosis and treatment of temporomandibular disorders. Am Fam Physician. 2015;91(6):378–86.
Scrivani SJ, Keith DA, Kaban LB. Desordens temporomandibulares. N Engl J Med. 2008;359:2693.
Chisnoiu AM, Picos AM, Popa S, Chisnoiu PD, Lascu L, Picos A. Fatores envolvidos na etiologia das disfunções temporomandibulares uma revisão de literatura. Clujul Med. 2015;88:473.
Li W, Dai C. Spontaneous temporomandibular joint herniation into the external auditory canal. Braz J Otorhinolaryngol. 2015;81:3.
Lim K, Jung J, Rhee J, Choi J. Herniação da articulação temporomandibular através do forame de Huschke com zumbido estalante. Eur Ann Otorhinolaryngol Head Neck Dis. 2019;136:497–9.
Tasar M, Yetiser S, Saglam M, Tasar A. Deformidade congênita da cavidade comum dos seios frontal, etmoidal e esfenoidal. Fenda Palatina Craniofac J. 2003;40:639–41.
Langer J, Begall K. Otosialorréia-diagnóstico e terapia de uma fístula salivar do canal auditivo externo. Laringorrinotologie. 2004;83:606–9.
Miloglu O, Yilmaz AB, Yildirim E, Akgul HM. Pneumatization of the articular eminence on cone beam computed tomography: prevalence, characteristics and a review of the literature. Dentomaxillofac Radiol. 2011;40:110–4.
Rezende Barbosa GL, Nascimento V, Ladeira DB, Bomtorim VV, Cruz AD, Almeida SM. Accuracy of digital panoramic radiography in the diagnosis of temporal bone pneumatization: a study in vivo using cone-beam-computed tomography. J Craniomaxillofac Surg. 2014;42:477–81.
Khojastepour L, Paknahad M, Abdalipur V, Paknahad M. Prevalence and characteristics of articular eminence pneumatization: a cone-beam computed tomographic study. J Maxillofac Oral Surg. 2018;17:339–44.
Koç A, Kaya S. Prevalence of foramen Huschke: evaluation of the association between mastoid pneumatization volume and the existence of foramen Huschke using cone beam computed tomography. Eur Arch Otorhinolaryngol. 2021;278:791–6.
Acknowledgements
The authors would like to thank the State University of Maringa for investing and contributing to science through research and development.
Funding
No funding used in this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Ethical approval
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008 (5). Informed consent was obtained from all patients for being included in the study.
Informed consent
All authors consent the publication of this study as signed in the Certification Form.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Fagundes, R.J., Felipe, B.C., Couto, M.K. et al. The relation between persistent foramen tympanicum and degenerative bone alterations in temporomandibular joint region. Oral Radiol 40, 445–453 (2024). https://doi.org/10.1007/s11282-024-00749-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11282-024-00749-3