Abstract
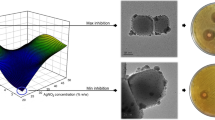
The combination of antimicrobial agents has been proposed as a therapeutic strategy to control bacterial diseases and to reduce the emergence of antibiotic-resistant strains in clinical environments. In this study, the interaction between the lantibiotic bovicin HC5 with chloramphenicol, gentamicin, nisin, lysostaphin and hydrogen peroxide against Staphylococcus aureus O46 was evaluated by MIC assays. The central composite rotatable design (CCRD), a robust and economic statistical design, was used to combine concentration levels of different antimicrobials agents with distinct mechanisms of action and the presence of significant interactions among the antimicrobials was determined by regression analysis. According to the adjusted model, there were no significant interactions between bovicin HC5 and gentamicin, lysostaphin, nisin or hydrogen peroxide. However, bovicin HC5 showed a significant interaction (P < 0.02) with chloramphenicol. This is the first study applying the CCRD approach to evaluate the combined effect of antimicrobials against S. aureus. Based on our results, this approach is an effective strategy to determine synergistic interactions between antimicrobial agents applied in human and veterinary medicine against bacterial pathogens.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The emergence of resistant bacteria to antibiotics is a leading public health concern (CDC 2013). In recent years, bacteria isolated from hospital-acquired infections often show resistance to at least one of the drugs most commonly used in the clinical treatment (Indrawattana et al. 2013). In this context, the combination of antimicrobial agents with different mechanisms of action has been proposed to reduce the emergence of human and livestock antibiotic-resistant strains and improve their efficacy against microbial pathogens by targeting multiple sites in the cell (Branen and Davidson 2004; Laxminarayan et al. 2006; del Pozo and Patel 2007; Lacasse et al. 2008; Dosler and Mataraci 2013).
Most studies evaluating the combined effect among antimicrobials use a complete factorial design to assess the activity of such inhibitors (Aaron et al. 2002; Nazer et al. 2005; Desbois and Coote 2011). Although these approaches allow the evaluation of several combined treatments, a large number of experimental units are often required to assess the interactions between treatments, with a remarkable increase in workload and experimental costs. Additionally, in many cases, the interpretation of the results does not always allow a clear interpretation of the interactions between antimicrobials being tested (Chou 2006; Tallarida 2011).
In this scenario, the central composite design (CCD) offers a robust regression analysis that can be used to design experiments with a lower number of treatments without losing discrimination power and maintaining its sensitivity to the occurrence of outliers in the experimental design (Chou 2006; Ukaegbu and Chigbu 2014). Among the different types of CCD, the central composite rotatable design (CCRD) has shown great potential to target the stability region of the design around a central point determined by its properties of rotatability and orthogonality (Hader and Park 1978). The CCRD approach has several applications, especially in studies aiming the optimization of experimental conditions or containing several treatments or variables. Although the CCRD has been applied to optimize the concentrations and exposure times of antimicrobials against the target bacteria (de Oliveira et al. 2012), the use of this approach to study the combined effects of different antimicrobial agents against pathogenic organism has been largely overlooked until now.
In this study we aimed to evaluate if the interaction between an antimicrobial peptide (bovicin HC5) and other antimicrobial agents could improve the inhibitory activity of bacteriocins against the pathogenic bacterium Staphylococcus aureus. The use of bacteriocins for therapeutic purposes has been considered an attractive alternative to control bacterial infections and to avoid the development of resistant strains (Hoffmann et al. 2002; Cao et al. 2007; Wu et al. 2007; Field et al. 2008). Bovicin HC5, a lantibiotic produced by Streptococcus equinus HC5, is highly effective against several bacterial pathogens, including S. aureus (de Carvalho et al. 2007; Pimentel-Filho et al. 2013, 2014). To test our hypothesis, a statistical approach using CCRD was applied to combine concentration levels of each antimicrobial and regression analysis was used to determine the interactions between these factors.
Materials and methods
Microorganisms and culture conditions
Streptococcus bovis HC5 was cultivated under anaerobic conditions, at 39 °C, in basal medium containing, per liter: 0.292 g K2HPO4, 0.292 g KH2PO4, 0.48 g (NH4)2SO4, 0.48 g NaCl, 0.1 g MgSO4·7H2O, 0.064 g CaCl2·2H2O, 0.6 g cystein hydrochloride, 0.1 g trypticase®, 0.5 g yeast extract, 4 g Na2CO3 and 16 g glucose.
The reference strain S. aureus O46 used in this study was kindly provided by the Institut National de la Recherche Agronomique (INRA)—UMR1253, Science et Technologie du Lait et de l’Oeuf, Rennes, France. S. aureus O46 was isolated from a ewe diagnosed with mild mastitis (Le Marechal et al. 2011) and was cultivated overnight under microaerophilic conditions, at 37 °C, in Mueller–Hinton (MH) media.
Preparation of the antimicrobial agents
Bovicin HC5 extracts were prepared and purified by reversed phase cromatography as previously described (Mantovani et al. 2002; Paiva et al. 2012). Purified bovicin HC5 was resuspended in phosphate buffer (PB, 30 µmol l−1, pH 7.0) and stored at −20 °C until use. Nisin stock solution was prepared by dissolving the appropriate amounts of commercial nisin (Sigma, N5764, 2.5 %) in 0.85 % NaCl prepared in 0.2 N HCl (pH 2.0). The other antimicrobials combined with bovicin HC5 were chloramphenicol (Fluka, 23275), gentamicin sulfate (Sigma, G3632) and lysostaphin (Sigma, L0761). These antimicrobials were prepared by dissolving the appropriate amounts of powder from commercial products into sterile deionized water with the exception of hydrogen peroxide (Synth, d 1.130), in which the stock solution was prepared by direct dilution in distilled water. Stock solutions of all antimicrobial agents were stored at −20 °C until use.
Minimum inhibitory concentration (MIC) assays
The MIC assay for different antimicrobials was performed using standard broth microdilution methods (CLSI 2013). Incubations were performed using MH media and the concentration range of each antimicrobial agent was (in μmol l−1): 1.0–125.0 for bovicin HC5, 16.2–130 for chloramphenicol, 0.2–25.0 for gentamicin, 373.1–5970.0 for hydrogen peroxide, 1.0–140 for lysostaphin 0.8–100 for nisin. The MIC values were used to determinate the concentration range of each antimicrobial tested in the combined treatment.
Combined effects of antimicrobial agents
Overnight cultures of S. aureus O46 (105 CFU ml−1) were inoculated into 96-well plates containing MH media added with combined concentrations of antimicrobials. The concentrations of each antimicrobial agent were determined using the CCRD approach. The maximum concentrations corresponded to ½ MIC values and the minimum concentrations were ten times lower than the MIC. When necessary, distilled water was added to adjust the final volume in each well to 200 µl. The optical densities (OD600nm) were monitored every 30 min for up to 12 h of incubation.
Data analysis
Each antimicrobial concentration used in this study was coded according to the standardization and principles of analysis of the CCRD approach. Levels of bovicin HC5 (factor A) were combined with five levels of each antimicrobial (factor B), generating nine treatments (Table 1). Three technical replicates were used for each treatment, yielding a total of 135 experimental units for each biological replication.
The final OD600nm values (obtained after 12 h of growth) were subjected to regression analysis to assess the combined effect of the antimicrobials on bacterial growth. The following first-order model considering the interaction of each antimicrobial with bovicin HC5 was used:
where, \(a_{i}\) is the level i of the factor A (bovicin HC5), if \({-}1.4142 \le a_{i} \le 1.4142\) and \(b_{j}\) is the level j of the factor B (each antimicrobial that was combined with bovicin HC5), if \(- 1.4142 \le b_{j} \le 1.4142.\)
Depending on the model, non-significant coefficients (P > 0.02) were removed one at a time, based first on the interaction between factors, and subsequently, based on the interaction that had a higher P value according to the Student’s t test.
Results
The MIC values for each antimicrobial agent tested against S. aureus O46 are summarized in Table 2. The concentration range for each antimicrobial agent was determined using the CCRD approach and tested in the treatments combined with bovicin HC5. The concentration range of each antimicrobial agent was (in μmol l−1): 0.1–1000 for bovicin HC5, 1.61–16.13 for chloramphenicol, 0.01–18 for gentamicin, 37.30–373.05 for hydrogen peroxide, 0.12–1.25 for lysostaphin and 0.07–0.78 for nisin (Table 3). The growth kinetics of S. aureus was always influenced by the presence of antimicrobials in the MH media. In general, the lag phases were prolonged and the growth rate and final OD600nm were lower compared to the control treatments (Fig. 1).
Growth of S. aureus O46 in presence of bovicin HC5 combined with different antimicrobials. Panels a through e represent each antimicrobial agent combined with bovicin HC5: a chloramphenicol, b gentamicin, c lysostaphin, d nisin and e hydrogen peroxide. Control treatments without antimicrobials (open circles) are also shown in each panel. Levels 1 through 9 represent the coded levels of each antimicrobial agent determined by the CCRD approach. Results are the mean OD600nm obtained from three independent experiments performed in triplicate. Bars represent the standard deviation of the mean
The regression analysis of the first-order interactions observed in our study allowed the evaluation of the combined effects between bovicin HC5 and other antimicrobials. The estimated equations, used for the interpretation of the combined effects of the antimicrobials on microbial growth were composed only by significant terms and are described in Table 4, as well as their respective coefficients of determination (R2). The mean value of R2 for the estimated equations was 0.744. When bovicin HC5 was combined with different antimicrobial agents, positive interactions in inhibitory activity were observed only between bovicin HC5 and chloramphenicol (P < 0.02), an antibiotic that inhibit peptide bond formation by 70S bacterial ribosomes. However, our results did not show interaction (P > 0.02) between bovicin HC5 and antimicrobial agents that target other structural or biochemical cellular components (e.g. 30S ribosomal subunits, peptidoglycan, lipid II, membrane lipids and macromolecules). Therefore, the decrease in bacterial growth shown in Fig. 1b–e is explained mainly by the inhibitory activity of bovicin HC5 against S. aureus.
Discussion
Staphylococcus aureus is an opportunistic pathogen frequently isolated from chronic infections (Indrawattana et al. 2013). Diseases caused by S. aureus are often difficult to treat and cure, and the raise of methicillin-resistant S. aureus strains (MRSA) emphasizes the need for more effective therapeutic strategies to control S. aureus infections (Römling and Balsalobre 2012; Otto 2013). Therefore, the combination of antimicrobials with distinct mechanisms of action could enhance their efficacy and therapeutic effects, reducing the time or the concentration required during clinical treatment (Dosler and Mataraci 2013).
In this study, the utilization of the CCRD approach to define the combined effects of different antimicrobial agents resulted in a regression analysis with significant interaction for the combination of bovicin HC5 and chloramphenicol (P < 0.02). This synergistic effect could be partially related with the mechanisms of action of these antimicrobial molecules. Chloramphenicol is a broad-spectrum antibiotic that diffuses through the cytoplasmic membrane and specifically prevents protein chain elongation in the 50S ribosomal subunit by reversibly inhibiting the transfer of amino acids to the growing peptide (Lin et al. 1997). Bovicin HC5 binds with high affinity to lipid II (Ka = 3.4 × 106 mol l−1) and is able to form a pre-pore-like structure (Paiva et al. 2011, 2012). Our previous results suggested that bovicin HC5 is too short to permeabilize lipid bilayers composed of phospholipids with C18 or longer acyl chains. Nonetheless, the antibacterial activity of bovicin HC5 is often more persistent than the activity of other lantibiotics that also target lipid II (e.g. nisin) and potassium efflux if often observed only if the bacteriocin is allowed to interact with sensitive cells for longer periods of time (Mantovani and Russell 2008; Paiva et al. 2011, 2012).
Based on these results, molecules acting against the cell membrane could facilitate other molecules to access the cell interior and reach its primary target (Park et al. 2004). This could be the case for the interaction between bovicin HC5 and chloramphenicol, in which, the latter could inhibit anabolic reactions in the cytoplasm and prevent a stress response in S. aureus cells. Additionally, bovicin HC5 is capable to cause efflux of cations that are relevant to maintain cell homeostasis (e.g. potassium). Therefore, a decrease in intracellular ATP pools and an increase in respiratory activity might be expected in these combined treatments (Mantovani and Russell 2008).
The regression analysis of the first-order interactions observed in our study also allowed the evaluation of the combined effects between bovicin HC5 and other antimicrobial agents. According to the adjusted models, there was no significant interaction between bovicin HC5 and gentamicin, hydrogen peroxide, lysostaphin or nisin, indicating that these antimicrobials neither act synergistically with bovicin HC5 nor interfere (P > 0.02) with the inhibitory activity of the peptide against S. aureus. The absence of synergism and the antagonism between antimicrobial agents has been previously described. When the antimicrobial activity of nisin and ramoplanin were evaluated against methicillin-resistant S. aureus (MRSA) and vancomycin-resistant enterococci (VRE) strains, an antagonistic effect was observed if the antimicrobials were added simultaneously to BHI media (Brumfitt et al. 2002).
In the case of gentamicin, lysostaphin and nisin, which showed much lower MIC values compared to chloramphenicol, the interaction with bovicin HC5 was probably not required to improve the antimicrobial activity of these molecules used alone. Gentamicin is an aminoglycoside that irreversibly binds to ribosomal proteins and 16S rRNA found in the 30S ribosomal subunit, inhibiting the initiation complex required for protein synthesis in the cell (Yoshizawa et al. 1998). The MIC values for gentamicin were approximately 85-fold lower than those observed for S. aureus cultures treated with chloramphenicol, indicating that this antibiotic can reach its target in the cytoplasm successfully without other “auxiliary” compounds.
Nisin is also a lantibiotic that target lipid II and in our assays the MIC values for nisin and bovicin HC5 were comparable to both bacteriocins (1.56 and 2.0 µmol l−1, respectively). The interactions between nisin and bovicin HC5 was not synergistic at the concentrations tested, and the regression analysis parameters further indicated that nisin did not reduce the inhibitory activity of bovicin HC5. These results could be explained by the greater affinity of bovicin HC5 for lipid II compared to nisin (Paiva et al. 2011, 2012).
In the case of lysostaphin, a glycylglycine endopeptidase that can hydrolyse the crosslink bridges in the peptidoglycan of staphylococci, it was initially expected that its mechanism of action could facilitate the activity of molecules that target the cell membrane, such as bovicin HC5. Previous work demonstrated a synergistic antibacterial activity between cell wall hydrolases (e.g. lysozyme, muramidases) and nisin and the authors postulated that these enzymes could enable the antimicrobial peptide to cross the cell wall and reach the cell membrane (Prado-Acosta et al. 2010). However, such synergistic effects were not observed in the present study when S. aureus was grown in the presence of bovicin HC5 and lysostaphin. These differences might be due to the smaller size of bovicin HC5 (23 amino acids) compared to nisin (34 amino acids), facilitating the diffusion through the cell envelope to reach its target site (cytoplasm membrane).
Hydrogen peroxide causes chemical oxidation of cellular components, including lipids and proteins (Cabiscol et al. 2010). Because these effects generally induces an oxidative stress response, the cell often respond with several changes in gene expression and can become adapted to the stimulus if the concentration of H2O2 is not lethal. Our results suggested that hydrogen peroxide does not affect the activity of bovicin HC5 (P < 0.02) and even 0.550 µmol l−1 of bovicin HC5 could cause complete inhibition of S. aureus growth when the bacteriocin was combined with the lowest dose of H2O2 (Fig. 1).
Although chloramphenicol was the antimicrobial agent showing greater interaction with bovicin HC5 against S. aureus, it should be noted that the clinical use of chloramphenicol is restricted due to its effect inhibiting mitochondrial protein synthesis and associated collateral effects, such as plastic anemia (Barnhill et al. 2012). Nonetheless, studies reporting the use of chloramphenicol in clinical practice and its ability to enhance the inhibitory activity of other antimicrobials or to control microbial pathogens are not rare (Laporte et al. 1998; Zuberbuhler et al. 2014; Maaland et al. 2015; Kiruthika et al. 2015).
Based on our results, it was possible to discriminate the significant interactions between bovicin HC5 and other antimicrobials with distinct mechanisms of action using the CCRD approach to determine the concentration levels and the interactions between the factors being evaluated. The CCRD approach could potentially be used to study the effect of combined antimicrobial agents with greater discriminatory efficiency. Our results shown that even at concentrations below MIC values, bovicin HC5 combined with other antimicrobial agents could prevent the growth of S. aureus cultures, and this effect persisted even if the incubation time was as long as 48 h. These results emphasize the potential of bovicin HC5 to inhibit S. aureus growth and prevent bacterial infections in vivo and highlight opportunities for improving therapeutic strategies by combining effective antimicrobial agents against microbial pathogens.
References
Aaron SD, Ferris W, Ramotar K, Vandemheen K, Chan F, Saginur R (2002) Single and combination antibiotic susceptibilities of planktonic, adherent, and biofilm-grown Pseudomonas aeruginosa isolates cultured from sputa of adults with cystic fibrosis. J Clin Microbiol 40:4172–4179
Barnhill AE, Brewer MT, Carlson SA (2012) Adverse effects of antimicrobials via predictable or idiosyncratic inhibition of host mitochondrial components. Antimicrob Agents Chemother 56:4046–4051
Branen JK, Davidson PM (2004) Enhancement of nisin, lysozyme, and monolaurin antimicrobial activities by ethylenediaminetetraacetic acid and lactoferrin. Int J Food Microbiol 90:63–74
Brumfitt W, Salton MR, Hamilton-Miller JM (2002) Nisin alone and combined with peptidoglycan-modulating antibiotics: activity against methicillin-resistant Staphylococcus aureus and vancomycin-resistant enterococci. J Antimicrob Chemother 50:731–734
Cabiscol E, Tamarit J, Ros J (2010) Oxidative stress in bacteria and protein damage by reactive oxygen species. Int Microbiol 3:3–8
Cao LT, Wu JQ, Xie F, Hu SH, Mo Y (2007) Efficacy of nisin in treatment of clinical mastitis in lactating dairy cows. J Dairy Sci 90:3980–3985
CDC (2013) Antibiotic resistance threats in the United States, 2013. US Department of Health and Public Services, Centre for Disease Control and Prevention, pp 14–28. http://www.cdc.gov/drugresistance/threat-report-2013/pdf/ar-threats-2013-508.pdf. Accessed 24 July 2014
Chou TC (2006) Theoretical basis, experimental design, and computerized simulation of synergism and antagonism in drug combination studies. Pharmacol Rev 58:621–681
Clinical and Laboratory Standards Insitute (CLSI) (ed) (2013) Performance standards for antimicrobial susceptebility testing: twenty-third informational supplement M100-S23. CLSI, Wayne, PA
de Carvalho AA, Costa ED, Mantovani HC, Vanetti MC (2007) Effect of bovicin HC5 on growth and spore germination of Bacillus cereus and Bacillus thuringiensis isolated from spoiled mango pulp. J Appl Microbiol 102:1000–1009
de Oliveira MMM, Brugnera DF, do Nascimento JA, Batista NN, Piccoli RH (2012) Cinnamon essential oil and cinnamaldehyde in the control of bacterial biofilms formed on stainless steel surfaces. Eur Food Res Technol 234:821–832
del Pozo JL, Patel R (2007) The challenge of treating biofilm-associated bacterial infections. Clin Pharmacol Ther 82:204–209
Desbois AP, Coote PJ (2011) Bactericidal synergy of lysostaphin in combination with antimicrobial peptides. EJCMID 30:1015–1021
Dosler S, Mataraci E (2013) In vitro pharmacokinetics of antimicrobial cationic peptides alone and in combination with antibiotics against methicillin resistant Staphylococcus aureus biofilms. Peptides 49:53–58
Field D, Connor PMO, Cotter PD, Hill C, Ross RP (2008) The generation of nisin variants with enhanced activity against specific gram-positive pathogens. Mol Microbiol 69:218–230
Hader R, Park SH (1978) Slope-rotatable central composite designs. Technometrics 20:413–417
Hoffmann A, Pag U, Wiedemann I, Sahl HG (2002) Combination of antibiotic mechanisms in lantibiotics. Il Farm 57:685–691
Indrawattana N, Sungkhachat O, Sookrung N, Chongsa-nguan M, Tungtrongchitr A, Voravuthikunchai SP, Kong-ngoen T, Kurazono H, Chaicumpa W (2013) Staphylococcus aureus clinical isolates: antibiotic susceptibility, molecular characteristics, and ability to form biofilm. BioMed Res Int. Article ID 314654. doi:10.1155/2013/314654
Kiruthika V, Maya S, Suresh MK, Anil Kumar V, Jayakumar R, Biswas R (2015) Comparative efficacy of chloramphenicol loaded chondroitin sulfate and dextran sulfate nanoparticles to treat intracellular Salmonella infections. Colloids Surf B Biointerfaces 127C:33–40
Lacasse P, Lauzon K, Diarra MS, Petitclerc D (2008) Utilization of lactoferrin to fight antibiotic-resistant mammary gland pathogens. J Anim Sci 86:66–71
Laporte JR, Vidal X, Ballarín E, Ibáñez L (1998) Possible association between ocular chloramphenicol and aplastic anaemia—the absolute risk is very low. Br J Clin Pharmacol 46:181–184
Laxminarayan R, Bhutta Z, Duse A, Jenkins P, O’Brien T, Okeke IN, Pablo-Mendez A, Klugman KP (2006) Drug resistance. In: Jamison DT, Breman JG, Measham AR, Alleyne G, Claeson M, Evans DB, Jha P, Mills A, Musgrove P (eds) Disease control priorities in developing countries, 2nd edn, Chapter 55. World Bank, Washington (DC). http://www.ncbi.nlm.nih.gov/books/NBK11774/. Acessed 27 June 2014
Le Marechal C, Hernandez D, Schrenzel J, Even S, Berkova N, Thiery R, Vautor E, Fitzgerald JR, Francois P, Le Loir Y (2011) Genome sequences of two Staphylococcus aureus ovine strains that induce severe (strain O11) and mild (strain O46) mastitis. J Bacteriol 193:2353–2354
Lin AH, Murray RW, Vidmar TJ, Marotti KR (1997) The oxazolidinone eperezolid binds to the 50S ribosomal subunit and competes with binding of chloramphenicol and lincomycin. Antimicrob Agents Chemother 41:2127–2131
Maaland MG, Mo SS, Schwarz S, Guardabassi L (2015) In vitro assessment of chloramphenicol and florfenicol as second-line antimicrobial agents in dogs. J Vet Pharmacol Ther. doi:10.1111/jvp.12204
Mantovani HC, Russell JB (2008) Bovicin HC5, a lantibiotic produced by Streptococcus bovis HC5, catalyzes the efflux of intracellular potassium but not ATP. Antimicrob Agents Chemother 52:2247–2249
Mantovani HC, Hu H, Worobo RW, Russell JB (2002) Bovicin HC5, a bacteriocin from Streptococcus bovis HC5. Microbiology 148:3347–3352
Nazer A, Kobilinsky A, Tholozan JL, Dubois-Brissonnet F (2005) Combinations of food antimicrobials at low levels to inhibit the growth of Salmonella sv. Typhimurium: a synergistic effect? Food Microbiol 22:391–398
Otto M (2013) Staphylococcal infections: mechanisms of biofilm maturation and detachment as critical determinants of pathogenicity. Annu Rev Med 64:175–188
Paiva AD, Breukink E, Mantovani HC (2011) Role of lipid II and membrane thickness in the mechanism of action of the lantibiotic bovicin HC5. Antimicrob Agents Chemother 55:5284–5293
Paiva AD, Irving N, Breukink E, Mantovani HC (2012) Interaction with lipid II induces conformational changes in bovicin HC5 structure. Antimicrob Agents Chemother 56:4586–4593
Park Y, Kim HJ, Hahm KS (2004) Antibacterial synergism of novel antibiotic peptides with chloramphenicol. Biochem Biophys Res Commun 321:109–115
Pimentel-Filho NJ, Mantovani HC, Diez-Gonzalez F, Vanetti MCD (2013) Inhibition of Listeria and Staphylococcus aureus by bovicin HC5 and nisin combination in milk. J Agric Sci 5:188–196
Pimentel-Filho NJ, Mantovani HC, de Carvalho AF, Dias RS, Vanetti MCD (2014) Efficacy of bovicin HC5 and nisin combination against Listeria monocytogenes and Staphylococcus aureus in fresh cheese. Int J Food Sci Technol 49:416–422
Prado-Acosta M, Ruzal SM, Allievi MC, Palomino MM, Rivas CS (2010) Synergistic effects of the Lactobacillus acidophilus surface layer and nisin on bacterial growth. Appl Environ Microbiol 76:974–977
Römling U, Balsalobre C (2012) Biofilm infections, their resilience to therapy and innovative treatment strategies. J Intern Med 272:541–561
Tallarida RJ (2011) Quantitative methods for assessing drug synergism. Genes Cancer 2:1003–1008
Ukaegbu EC, Chigbu PE (2014) Graphical evaluation of the prediction capabilities of partially replicated orthogonal central composite designs. Qual Reliab Eng Int. doi:10.1002/qre.1630
Wu J, Hu S, Cao L (2007) Therapeutic effect of nisin Z on subclinical mastitis in lactating cows. Antimicrob Agents Chemother 51:3131–3135
Yoshizawa S, Fourmy D, Puglisi JD (1998) Structural origins of gentamicin antibiotic action. EMBO J 17:6437–6448
Zuberbuhler B, Abedin A, Roudsari A (2014) A novel case of chronic conjunctivitis in a 58-year-old woman caused by Raoultella. Infection 42:927–929
Acknowledgments
Authors gratefully acknowledge Dr. Yves Le Loir (Institut National de la Recherche Agronomique—Rennes) for kindly providing reference strains and Dr. Maria Cristina Baracat-Pereira (Departamento de Bioquímica e Biologia Molecular at the Universidade Federal de Viçosa) for technical support in the purification of bovicin HC5. This research was supported by the Fundação de Amparo à Pesquisa do Estado de Minas Gerais (FAPEMIG, Belo Horizonte, Brazil). F.G.S. received a doctoral fellowship from the Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq, Brasília, Brazil) and Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES, Brasília, Brazil).
Conflict of interest
The authors declare that there are no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Santos, F.G., Mendonça, L.A. & Mantovani, H.C. A central composite rotatable design (CCRD) approach to study the combined effect of antimicrobial agents against bacterial pathogens. World J Microbiol Biotechnol 31, 1361–1367 (2015). https://doi.org/10.1007/s11274-015-1884-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11274-015-1884-4