Abstract
Background
The specific treatment regimens of IgA nephropathy (IgAN) patients with moderate proteinuria (1.0–3.5 g/day) remain controversial. The purpose of this study was to explore the optimized therapeutic regimen for IgAN patients through analyzing the clinical data.
Methods
A retrospective study was conducted, 449 patients with biopsy-proven IgAN were enrolled. Patients were divided into three groups according to proteinuria levels: urine protein 1.0–1.5 g/day (UP1, n = 111), urine protein 1.5–2.5 g/day (UP2, n = 213), urine protein 2.5–3.5 g/day (UP3, n = 125). Clinical pathological features, treatment regimens and renal outcome were compared. Responses to therapy included complete remission (CR), partial remission (PR), no response (NR) and end-stage renal disease (ESRD). The composite endpoints of renal outcome were defined as 50% decline in eGFR and/or progressing into end-stage renal disease.
Results
During the average follow-up of 44.27 months, 71 (63.9%), 150 (70.4%) and 68 (54.4%) patients achieved CR + PR among three groups, respectively. Whereas 15 (13.5%), 28 (13.1%) and 39 (31.2%) patients progressed to the primary endpoint (P < 0.001). Patients who received corticosteroids (CS) treatment had better remission rate than those with supportive care (SC) or combined corticosteroid plus immunosuppressant (CS + IT) therapy (P < 0.05). Kaplan–Meier survival analysis revealed that patients received CS and CS + IT treatments had better renal prognosis compared with SC therapy in UP2 and UP3 groups (P < 0.05). However, no statistical difference was found among three treatment regimens in UP1 group (P = 0.358).
Conclusion
Corticosteroids therapy might better improve renal prognosis compared with supportive care alone or corticosteroids plus immunosuppressant in IgAN patients with moderate proteinuria (1.5–3.5 g/day).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Immunoglobulin A nephropathy (IgAN) is the most common primary glomerulonephritis manifested as IgA depositing in the glomerular mesangium [1]. The main clinical characteristics of IgAN are hematuria, proteinuria and renal function deterioration [2]. As is known, about 20–40% patients would develop end-stage renal disease (ESRD) gradually within 20–30 years after the diagnosis of IgAN [3].
Until now, considerably debates exist in the effectiveness of different treatment regimens. Considering that proteinuria is an independent risk factor of poor prognosis [4]. Corticosteroids (CS) have been recommended to patients with persistent urinary protein (≥ 1.0 g/day) after 3–6 month supportive care, but other immunosuppressant was not recommended [5]. However, controversial results about the effectiveness of corticosteroids and immunosuppressant were reported. Pozzi et al. reported that corticosteroids treatment was significantly better than supportive therapy in IgAN patients with urine protein 1.0–3.5 g/day [6]. The European Validation Study of the Oxford Classification of IgAN (VALIGA) demonstrated corticosteroids could improve renal outcomes regardless of baseline eGFR and level of urinary protein [7]. Besides, a recent study also showed that the treatment of CS alone or CS + IT is significantly effective in NS-IgAN patients [8]. Therefore, the main controversy focuses on patients with moderate level urine protein, whether glucocorticoids and immunosuppressant could improve the renal survive of IgAN patients has not yet been addressed. This study was carried out to investigate the optimized regimens of IgAN patients with urine protein between 1.0 and 3.5 g/day.
Methods
Patients
This was a single-center retrospective study, IgAN patients with biopsy-proven from the West China Hospital of Sichuan University between December 2008 and July 2016 were included in this study. The inclusive criteria were as follows: (A) patients are over the age of 14 and were followed for at least 3 months. (B) IgAN was confirmed by renal biopsy. (C) 24-h urine protein ranges between 1.0 and 3.5 g/day. The exclusive criteria were as follows: (A) patients with systemic lupus erythematosus, Henoch–Schönlein purpura, diabetes mellitus, liver cirrhosis and other secondary etiologies of IgAN were excluded. (B) Patients with insufficient clinical and pathologic data, and renal biopsy samples contained less than eight glomeruli were excluded. (C) Patients without complete information or clinical data were also excluded. Patients were divided into three groups according to proteinuria level at the time of biopsy, UP1 group (1.0–1.5 g/day), UP2 group (1.5–2.5 g/day), and UP3 group (2.5–3.5 g/day), based on the level of 24-h urine protein at biopsy. The research was in compliance with the Declaration of Helsinki and was approved by the ethical committees of West China Hospital of Sichuan University.
Clinical data and therapy
Demographic and clinical data focused on age, sex, and mean arterial pressure (MAP). Laboratory results included serum albumin (Alb), serum creatinine (sCr), estimated glomerular filtration rate (eGFR), 24-h urinary protein and kidney pathology findings. EGFR was calculated using the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation [9]. Renal biopsy was classified according to the updated Oxford Classification: mesangial hypercellularity (M), endocapillary hypercellularity (E), segmental glomerulosclerosis (S), tubular atrophy/interstitial fibrosis (T) and cellular or fibrocellular crescents (C) [10]. All renal biopsy samples were reviewed independently by two kidney pathologists.
Treatment regimens were also divided into three groups: supportive care (SC), corticosteroids (CS), corticosteroids combined with immunosuppressive therapy (CS + IT). Patients in SC group received optimized dose of renin–angiotensin system inhibitors (ACEI) and/or angiotensin receptor blockers (ARB) applied to achieve the goal blood pressure (BP < 140/90 mmHg). Patients in CS group were treated with optimal ACEI/ARB plus corticosteroids (0.5–1 mg/kg/day prednisone or equal dose of methylprednisolone, gradually decreased within 6–8 months). Patients in CS + IT group were treated with corticosteroids and immunosuppressant including cyclophosphamide (2 mg/kg/day for 3 months). Mycophenolate Mofetil (1–2 g/day for 6–8 months) or cyclosporine (3–5 mg/kg/day) or tacrolimus 0.03–0.05 mg/kg/day for 6–8 months). Treatment regimens were determined by doctors and patients. Patients refuse to take steroids or immunosuppressant was given optimal supportive therapy. Written informed consent was collected by all patients.
Measurements
Hypertension (HTN) was defined as blood pressure (BP) > 140/90 mmHg. End-stage renal disease (ESRD) was defined as eGFR < 15 mL/min/1.73 m2 or maintenance renal replacement treatment. The composite endpoints of renal outcome were defined by a renal function decline > 50% in eGFR and/or ESRD. Responses to therapy included complete remission (CR), partial remission (PR), no response (NR) and end-stage renal disease (ESRD). CR was defined as urinary protein excretion < 0.5 g/24 h, along with eGFR decrease less than 10% baseline. PR was defined as proteinuria decrease by > 50% baseline, with eGFR decrease less than 10% baseline. NR was defined by proteinuria decrease less than 50% baseline, or eGFR increase > 10% baseline [11].
Statistical analysis
Normally distributed variables were expressed as mean ± SD, non-normal distributed variables were presented as median with interquartile range (IQR), Analysis of variance (ANOVA) or Kruskal–Wallis H test were used in data analysis. Categorical variables were summarized as number and percentage, analyzed by Chi-square test or Fischer’s exact test. Kaplan–Meier method was applied in renal survival analysis. SPSS version 22.0 (IBM SPSS, Chicago, IL) was used to carry out statistical analysis. P value was generated for all variables and P < 0.05 was considered to be statistically significant.
Results
Baseline data of IgAN with moderate urinary protein
A total of 1194 patients were enrolled from a medical center and were diagnosed as IgAN by renal biopsy. According to the inclusion and exclusion criteria, 449 patients (215 male and 234 female) were enrolled and 745 patients were excluded, which was shown in Fig. 1. Based on the levels of urinary protein, patients were divided into three groups. Patients with proteinuria between 1.0 and 1.5 g/day were classified as urine protein 1 (UP1) group (n = 111), 1.5–2.5 g/day as urine protein 2 (UP2) group (n = 213), and 2.5–3.5 g/day as urine protein 3 (UP3) group (n = 125). Table 1shows the clinical and pathological manifestations of IgAN patients enrolled in this study. The average follow-up period was 44.27 months.
All the clinical indexes at baseline were markedly different except for ages. Significant differences were observed in gender, blood pressure, hypertension rate, eGFR level, serum albumin and sCr levels among three groups (P < 0.05). It was noticed that patients in the UP3 group tended to have the severest clinical presentations: highest blood pressure and serum creatinine levels, and lowest eGFR and serum albumin level. Although obvious statistical significance was found in clinical manifestations, no markedly difference in pathological changes such as M, E, S and C was noticed. However, much severer chronic changes (T, interstitial and tubules fibrosis and atrophy) were found in UP2 and UP3 group patients.
Treatment response and outcomes
It was found that significant differences existed in the treatments regimens of patients in three groups (Fig. 2). Patients in UP2 and UP3 groups received more aggressive treatment when comparing with patients in UP1 group (P < 0.001). During the follow-up period, 228 (50.8%) patients achieved CR, 61 (13.6%) patients achieved PR, 78 (17.4%) patients ended in NR, 82 (17.8%) patients progressed to ESRD, and no patient died. In terms of therapeutic response, the highest remission rate was found in UP2 group (CR + PR 70.4%), while the lowest was observed in UP3 group (54.4%) as shown in Fig. 3a (P = 0.012). We then analyzed therapy responses of different treatment regimens among three groups (Fig. 3b–d). It could noticed that the treatment response of patients who received corticosteroids (CS) were better than those received supportive treatment alone (SC) or corticosteroids plus immunosuppressant (CS + IT) despite of urine protein level (UP1, UP2 and UP3 groups). Further analysis found that the treatment responses of SC was significantly different from that of the other two groups in three groups (UP1, CR + PR: 51.7% vs 83.3% vs 64.7%; UP2, CR + PR: 46.5% vs 86.0% vs 64.6%; UP3, CR + PR: 11.7% vs 77.8% vs 59.4%). Especially in UP3 group, the majority of patients who received treatment of SC failed to achieve remission. These findings demonstrated that CS could be a better choice in terms of therapeutic effect than supportive care alone for IgAN patients with moderate level proteinuria.
Renal survival during follow-up periods
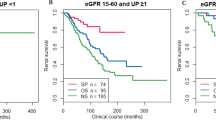
To evaluate the renal survival during follow-up period, Kaplan–Meier survival analysis was performed according to proteinuria level and different therapeutic measures. As shown in Fig. 4, renal survival during follow-up period was remarkably worse in UP3 group patients than UP1 and UP2 group patients. 33.6% patients in UP3 group reached composite renal endpoints during follow-up, while only 13.5% and 13.6% patients in UP1 and UP2 group reached (P < 0.001). No significant difference was observed between UP1 and UP2 groups (P = 0.870). Additionally, renal survival curves of different treatment regimens are displayed in Fig. 5a. It was found that patients received CS patients (9.1%) presented with the best renal survival rate than patients treated with SC (31.3%) or CS + IT (20.6%) patients (Fig. 5a, P < 0.001). In subgroup analysis, it was noticed that no statistical differences presented among three treatments regimens in UP1 group patients (Fig. 5b, P = 0.358). However, CS and CS + IT treatments could achieve remarkably better renal survival compared with SC therapy in UP2 (Fig. 5c) and UP3 (Fig. 5d) groups, while no significant difference between CS and CS + IT could be found.
Kaplan–Meier analysis for the probability of composite endpoint of IgAN patients with moderate level of proteinuria according to different regimens. The composite endpoint was 50% decline in eGFR and/or ESRD. SC, supportive care; CS, corticosteroids; CS + IT, corticosteroids combined with immunosuppressive therapy. a Renal survival of IgAN patients with moderate level of proteinuria according to different regimens. b Kidney survival rates showed SC, CS and CS + IT treatments in UP1 group. c Kidney survival rates showed SC, CS and CS + IT treatments in UP2 group. d Kidney survival rates showed SC, CS and CS + IT treatments in UP3 group
Discussion
To our knowledge, IgAN as one of the most common primary glomerulonephritis in the world is also the main cause of ESRD. Considering that there is not well-accepted specific treatment for IgAN, individualized therapy was decided usually according to clinical and pathological characteristics of IgAN patients in clinical practice. It was reported that proteinuria can reflect the deterioration of renal function of IgAN and patients with sustained proteinuria > 1.0 g/day is strongly associated with poorer renal outcomes [4]. Therefore, proteinuria has been considered as predictor of poor renal prognosis of patients. Previously, several studies have indicated that corticosteroids and immunosuppressant could reduce proteinuria and lower the risk of ESRD in IgAN patients [12,13,14]. However, other studies did not find benefit of corticosteroids or immunosuppressant in IgAN [15,16,17]. Due to the great heterogeneity among different studies such as races, geographical region, specific therapeutic strategies, experimental methods, sample size and follow-up duration, there is not well-accepted recommendation of optimal treatment regimens for IgAN patients with moderate proteinuria. Therefore, we performed this retrospective study to explore the efficacy of different regimens in treating IgAN patients with moderate proteinuria to provide more powerful evidence from actually daily practice.
Results of our study suggested that patients with more proteinuria tended to present with worse clinical manifestation, such as higher levels of BP and serum creatinine, lower levels of eGFR and serum albumin. Similar to our results, several studies have also suggested that proteinuria level along with eGFR and hypertension were risk index for disease progression in IgAN [18, 19]. Therefore, proteinuria level may even serve as predictor of a poor renal prognosis in IgAN patients. Furthermore, we also observed that patients with more proteinuria were characterized by severer chronic tubular and interstitial fibrosis (T) lesion. Considering that T lesion was predictor of disease progression in IgAN patients, this may be a reason of poor renal outcome in patients with more proteinuria, which was similar to previous report [20]. Based on our findings, it could speculated that proteinuria at biopsy combine with T lesion may be an important predictor for renal outcomes in IgAN patients just as reported by other study [21].
In this study, remarkable differences were found in renal survival among three groups. Patients with the highest level of proteinuria (UP3) tended to have the worst renal outcomes (P < 0.001). Although patients in UP3 group received much more aggressive therapy including corticosteroids and immunosuppressant, the proportion of patients in UP3 group was higher developed to ESRD during follow-up period compared with UP1 and UP2 groups (P < 0.05). This result suggested that proteinuria level in IgAN patients is strongly positively correlated with renal prognosis. Previous report also indicated similar result [4].
In view of the current research, we also found that patients received corticosteroids (CS) had better remission rate (CR + PR) and renal survival than those treated with supportive care alone (SC) (P < 0.001). Further analysis indicated that patients treated with CS and corticosteroids plus immunosuppressant (CS + IT) had better renal survival in UP2 and UP3 groups compared to those received SC alone. Moreover, no significant difference existed between CS and CS + IT groups. Given the risk of serious infection and other adverse effect of immunosuppressant, treatment with corticosteroids alone might be a better choice rather than combined with immunosuppressant. The present study showed the similar result with our previous and TESTING studies [8, 11, 16], suggesting that treatment with corticosteroids could delay renal deterioration at least in Asia or China adults with less proteinuria IgAN patients. It is worth noting that the result is different from the STOP-IgAN Trial. With careful analysis, we found that patients included in STOP-IgAN Trial had lower urine protein levels (about 1.0 ± 0.5 or 0.6 g/day), equivalent to the UP1 group in this study. In our cohort study, we also found no statistical significance for improving renal prognosis in UP1 group (Fig. 5B, P = 0.358), which is similar to the results of STOP-IgAN Trial. Combined with the previous results and several other important clinical studies, we speculated that treatment measures for IgAN patients should be determined according to the clinical manifestations. Patients with less proteinuria might not necessarily need the treatment with corticosteroids or immunosuppressant, while patients with more proteinuria level should recommend corticosteroids rather than merely supportive care or immunosuppressant.
The limitations of this study should be still recognized. First, the average follow-up in our cohort study was relatively short. Further study with longer follow-up period is needed. Second, this is a retrospective observational cohort study in Chinese population and the results might not necessarily representative of other countries and regions. Third, it difficult to extrapolate the results for coming from a single center study. Furthermore, some multicenter and multiracial IgAN studies with a large-scale, long-term follow-up are required to identify our results.
Conclusion
Corticosteroids therapy may be a better therapeutic choice for IgAN patients with moderate proteinuria (1.5–3.5 g/day). However, supportive care appears to be more appropriate for IgAN patients with less proteinuria (1.0–1.5 g/day).
References
Kim JK, Kim JH, Lee SC, Kang EW, Chang TI, Moon SJ et al (2012) Clinical features and outcomes of IgA nephropathy with nephrotic syndrome. CJASN 7(3):427–436
Rodrigues JC, Haas M, Reich HN (2017) IgA nephropathy. Clin J Am Soc Nephrol 12(4):677–686
Coppo R (2017) Corticosteroids in IgA nephropathy: lessons from recent studies. J Am Soc Nephrol 28:25–33
Reich HN, Troyanov S, Scholey JW, Cattran DC, Registry TG (2007) Remission of proteinuria improves prognosis in IgA nephropathy. J Am Soc Nephrol 18(12):3177–3183
Radhakrishnan J, Cattran DC (2012) The KDIGO practice guideline on glomerulonephritis: reading between the (guide)lines—application to the individual patient. Kidney Int 82(8):840–856
Pozzi C, Andrulli S, Del Vecchio L, Melis P, Fogazzi GB, Altieri P et al (2004) Corticosteroid effectiveness in IgA nephropathy: long-term results of a randomized, controlled trial. J Am Soc Nephrol 15(1):157–163
Tesar V, Troyanov S, Bellur S, Verhave JC, Cook HT, Feehally J et al (2015) Corticosteroids in IgA nephropathy: a retrospective analysis from the VALIGA study. J Am Soc Nephrol 26(9):2248–2258
Han X, Xiao Y, Tang Y, Zheng X, Anwar M, Qin W (2019) Clinical and pathological features of immunoglobulin A nephropathy patients with nephrotic syndrome. Clin Exp Med 19(4):479–486
Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF 3rd, Feldman HI et al (2009) A new equation to estimate glomerular filtration rate. Ann Intern Med 150(9):604–612
Working Group of the International IgA Nephropathy Network, and the Renal Pathology Society, Roberts IS, Cook HT, Troyanov S, Alpers CE, Amore A et al (2009) The Oxford classification of IgA nephropathy: rationale, clinicopathological correlations, and classification. Kidney Int 76(5):534–545
An L, Tang Y, Peng W, Mathew BS, Qin W (2018) Combined immunosuppressive treatment may improve short-term renal outcomes in Chinese patients with advanced IgA nephropathy. Kidney Blood Press Res 43(4):1333–1343
Lv J, Xu D, Perkovic V, Ma X, Johnson DW, Woodward M et al (2012) Corticosteroid therapy in IgA nephropathy. J Am Soc Nephrol 23:1108–1116
Zhang Y, Luo J, Hu B, Ma T (2018) Efficacy and safety of tacrolimus combined with glucocorticoid treatment for IgA nephropathy: a meta-analysis. J Int Med Res 46(8):3236–3250
Coppo R, Troyanov S, Bellur S, Cattran D, Cook HT, Feehally J et al (2014) Validation of the Oxford classification of IgA nephropathy in cohorts with different presentations and treatments. Kidney Int 86:828–836
Rauen T, Eitner F, Hertig A (2015) Intensive supportive care plus immunosuppression in IgA nephropathy. N ENGl JMED 373(23):2225–2236
Lv J, Zhang H, Wong MG, Jardine MJ, Hladunewich M, Jha V et al (2017) Effect of oral methylprednisolone on clinical outcomes in patients with IgA nephropathy: the TESTING randomized clinical trial. JAMA 318:432–442
Sarcina C, Tinelli C, Ferrario F, Pani A, De Silvestri A, Scaini P et al (2016) Changes in proteinuria and side effects of corticosteroids alone or in combination with azathioprine at different stages of IgA nephropathy. Clin J Am Soc Nephrol 11(6):973–981
Thompson A, Carroll K, Inker L, Floege J, Perkovic V, Boyer-Suavet S et al (2019) Proteinuria reduction as a surrogate end point in trials of IgA nephropathy. Clin J Am Soc Nephrol 14(3):469–481
Inker LA, Mondal H, Greene T, Masaschi T, Locatelli F, Schena FP et al (2016) Early change in urine protein as a surrogate end point in studies of IgA nephropathy: an individual-patient meta-analysis. Am J Kidney Dis 68(3):392–401
Ai Z, Xu R, Liu W, Zhou Q, Li B, Huang F et al (2016) Clinicopathologic features of IgA nephropathy patients with different levels of proteinuria. Clin Nephrol 86(7):35–41
Zhu X, Li H, Liu Y, You J, Qu Z, Yuan S et al (2017) Tubular atrophy/interstitial fibrosis scores of Oxford classification combinded with proteinuria level at biopsy provides earlier risk prediction in lgA nephropathy. Sci Rep 7(1):1100
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest with respect to the research.
Ethical approval
The research was in compliance with the Declaration of Helsinki and was approved by the ethical committees of West China Hospital of Sichuan University.
Informed consent
Written informed consents were signed by all the patients.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zhong, Z., Tang, Y., Tan, J. et al. Corticosteroids could improve the renal outcome of IgA nephropathy with moderate proteinuria. Int Urol Nephrol 53, 121–127 (2021). https://doi.org/10.1007/s11255-020-02644-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-020-02644-2