Abstract
Purpose
Adequate and functional long-term vascular access (VA) is pivotal for the efficient hemodialysis (HD). It has been shown that the most reliable VA is autogenous arteriovenous fistulas (AVFs) as compared with arteriovenous grafts (AVGs) and vascular catheters (VCs). The vascular access register (VAR) has been established since 2010, and the 4-year trend of VA in Serbia is presented in this paper.
Methods
All HD centers in Serbia provided their data by fulfilling the questionnaire that included prevalent and incident HD patients on December 31, 2010–1013.
Results
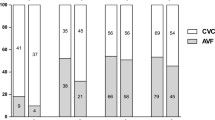
AVF is the most frequent prevalent VA (89.5–93.1 %) and also the most frequent newly created VA (87–89 %) during the observational period. The number of preemptive AVF is increasing, but it is still low (7.8 % in 2010 and 14.6 % in 2013). The percentage of incident AVG is constant (~3.4 %) as well as the number of permanent VC (8.2 % in 2010 and 7.8 % in 2013). The number of incident patients who started HD with AVF is decreasing (from 37 to 27 %), and the number of urgent start with VC is on the increase (from 63 to 73 %). In almost all relevant dialysis centers, vascular access is created by surgeons. Temporal VCs are placed by anesthesiologists (all centers), nephrologists (up to 25 % of centers) and vascular surgeons (up to 20 %). VCs are located mainly in jugular vein, but the number of femoral catheters remains high (up to 69 %).
Conclusion
Although we have favorable data, the VAR is of a great importance and ensures continuous quality improvement.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Effective chronic hemodialysis (HD) requires optimal long-term vascular access [1]. Autologous arteriovenous fistulas (AVFs) allow the best results as compared to prosthetic arteriovenous grafts (AVGs) and tunneled catheters. Patients with AVFs have less frequent vascular access-related complications including infections, thrombosis and surgical interventions and have better survival [2, 3]. Although there were no randomized comparisons between different vascular forms of access and patient outcome, observational studies revealed a superiority of native fistulas. Therefore, fistulas are considered the preferred form of hemodialysis access and are endorsed by local, national and international guidelines [4–6]. However, data from different regions revealed that a percentage of HD patients with native AVF is far from optimal. According to DOPPS V study, in most DOPPS countries, the frequency of native AVFs is usually less than 80 % ranging from 49 % in Canada up to 92 % in Russia [7]. There were some attempts to increase the percentage of native fistulas and reduce the percentage of vascular prosthesis and tunneled catheters. One of the most effective strategies was promoted by the initiative ‘fistula first catheter last’ [4]. It focuses on increasing the use of AVFs while decreasing the use of tunneled dialysis catheters as long-term vascular accesses for dialysis, toward goal of 68 % prevalent AVFs in all ESRD Networks. The work of the fistula first catheter last workgroup coalition is focused on supporting the renal community, the ESRD Networks, patients and authorities in efforts to improve vascular access outcomes and patients’ experience of care, as well as outcomes of the ESRD population while decreasing the cost of care. Over the last decade, the proportion of elderly frequently suffering from diabetes and hypertension increased and such population is unsuitable for successful AVF creation.
Chronic hemodialysis in Serbia dates back to 1969. Since then a significant attention has been paid to vascular access. As a part of a continuous quality improvement, we established a Vascular Access Registry in order to gain an insight into the current status of vascular access in all HD centers in Serbia and to follow the trend. The aim of this study was to present our experience concerning incident and prevalent vascular access during 4-year period.
Patients and methods
This multicenter observational study was based on a questionnaire sent to all HD centers in Serbia: 55 centers in 2010, 57 centers in 2011 and 2012 each and 62 centers in 2013. The questionnaire contains four groups of questions:
-
1.
The first set of questions relates to the data on the number and type of vascular access in prevalent hemodialysis patients in the current year at 31 December.
-
2.
The second set of questions includes the number and types of vascular accesses created in the current year, as well as information about who created them (vascular surgeon, urologist, nephrologist, general surgeon).
-
3.
The third group relates to data on temporary central venous catheters (by whom and in which vein were they placed).
-
4.
The last group of questions relates to the number of incident patients and their vascular access at the time of initiation of dialysis in the current year.
Data included all prevalent and incident patients in a given year and were expressed as percentages of all HD patients in Serbia. The response rate was 83.6 % in 2010, 94.7 % in 2011 and 100 % in 2012 and 2013 years. Given the high response rate, we believe that we present a realistic picture of vascular accesses at the national level.
Results
Table 1 shows the summary of data on prevalent patients who were treated by hemodialysis on December 31, 2010, 2011, 2012 and 2013. We followed data over the last 4 years, and it is evident that the native fistula remains a priority and the standard of vascular access care in Serbia. At the same time, the number of patients with vascular prosthesis remains low (2010, 2011, 2012 and 2013 = 3.8, 3.2, 3.3 and 2.8 %) as well as the number of patients with tunneled vascular catheter as a permanent vascular access (2010, 2011, 2012 and 2013 = 4.3, 4.1, 3.6 and 3.2 %). The most common localization of a tunneled vascular catheter was subclavian region, and the localization of vascular prosthesis in the arm was twice as much than in the leg.
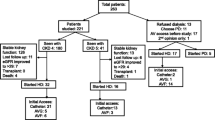
In most Serbian HD centers (77 %), vascular access is created by vascular surgeons, rarely general surgeon (9 %) and urologists (7 %). There is only one nephrologist who creates vascular access. The largest number of all vascular accesses in Serbia (49.6 %) is performed mainly in five major university dialysis centers. AVFs are the most commonly created vascular accesses which will certainly have the effect of maintaining a high number of prevalent AVF. The number of preemptive AVF increased from 7.8 % in 2010 to 14.6 % in 2013, which indicates that more attention is paid to this important aspect in the treatment of chronic kidney patients (Fig. 1).
The number of newly created AVG and tunneled vascular catheters is held constant during the period of observation.
The use of arteriovenous fistula and temporal vascular catheter in incidence hemodialysis patients is shown in Fig. 2. Some of these fistulas were preemptive ones (created more than 6 months before starting the dialysis), and some were urgent fistulas that were used within 1 month from the moment of creation. This is the figure we cannot be satisfied with and certainly needs improvement in the future.
Temporal vascular catheters were placed in 35 centers. During the 4-year period, the number of centers where nephrologists and vascular surgeons placed temporal catheters was reduced compared to the centers where anesthesiologists perform such activities (Fig. 3).
According to the questionnaire, temporal catheters are commonly placed in the jugular vein: (97–100 % of centers use this access rout). The number of centers placing femoral catheters is 60–69 %, which indicates a large number of patients who have exhausted other, more suitable locations for vascular catheters (Fig. 4).
Discussion
Renal replacement therapy (RRT) is available to all patients who need it in Serbia. According to The Annual Report on Renal Replacement Therapy in Serbia, during the last 4 years, the total number of patients with ESRD increased from 5546 in 2010 to 5651 in 2013 (137 new patients on million population) [8]. Out of the total number of patients treated with the methods of RRT in 2013, only 14.4 % of patients live with a transplanted kidney, and this percentage is substantially constant. This means that dialysis is the most common form of RRT; around 78 % of all ESRD patients are treated by chronic hemodialysis. Therefore, it is obvious why vascular access attracts a lot of attention of the Serbian nephrologists. The trend over the last 4 years shows that the native fistula remains a priority and dominant option in order to maintain a high standard in the vascular access care in Serbia despite the unfavorable structure of patients: Like the rest of the world we also register an increase in the incidence of the elderly population (>65 years), patients with hypertension (22–27 %) and diabetes (22–25 %) as the cause of ESRD [8]. Vascular accesses are mainly created by vascular surgeons. In some countries, nephrologists have taken over this responsibility, and according to literature data, the results are favorable [9–12].
Data presented in this paper are still significantly more favorable than those shown in the latest The Dialysis Outcomes and Practice Patterns Study—The DOPPS V study conducted by the USA and participating countries. In these countries, the frequency of AVFs varies from 49 % in Canada to 92 % in Russia. In addition to Russia, high percentage of AVFs (>80 %) have been established in Japan (91 %), China (87 %), Turkey (83 %), Australia and New Zealand (82 %), while in most European countries, this percentage is below 80 % [7]. A report from ERA-EDTA Registry pointed out that percentage of prevalent AVFs decreased from 66 to 62 % and the use of CVCs increased from 28 to 32 % [13]. The only data similar to those in Serbia are data from FYR of Macedonia with 89 % of prevalent patients with AVF [14].
The use of tunneled vascular catheters in Serbia is lower than in DOPPS countries where they are represented as chronic access in 4–18 % of patients, with the exception of Japan (1 % of patients). Representation grafts in DOPPS countries are diverse and range from 2 % (Russia) to 18 % (USA). Similarly to others [15], we have much better experience with vascular grafts than with tunneled vascular catheters but the number of patients with AVG is limited due to lack of proper products and financing due to their high price. Still, there is a positive trend in permanent vascular access in DOPPS countries which can be interpreted as initiative for the creation of AVF (fistula first catheter last). Based on the latest data, this initiative increased the prevalent AVFs in the USA to almost 63 %, while the percentage of CVCs is only about 9 % [16].
These differences between the countries may be explained not only by different patients’ characteristics but also by different treatment policies, availability of surgical support and access to interventional radiologists, health service structure and organization, and in our case, the (un)successful transplant program.
Although our results are displayed among the best, we cannot be satisfied with the number of preemptive fistulas: Over the last 4 years, the percentage of preemptive AVFs increased only by about 7 % (7.8–14.6 %). Consequently, 73 % of incident HD patients start their chronic HD program with temporal vascular catheter and they receive AVF later in the course of their treatment. Possible explanations are late referral of patients, small number of centers that create vascular accesses and their being overburdened with emergency vascular surgery. We share the similar reasons for the small number of preemptive AVFs like the other European countries (lack of dedicated and skilled surgeons, inadequate preoperative preparation) [17]. A report from the ERA-EDTA Registry has shown a significant decrease in the use of AVFs at the start of HD from 42 % in 2005 to 32 % in 2009, while the use of VCs increased from 58 to 68 % [13]. Catalan Renal Registry shows that 48 % of patients initiated HD with a fistula, 1.2 % with a graft and 15.9 % with tunneled and 35 % with untunneled catheters [18].
Number of incident catheters inserted in the jugular vein was two times higher than the number placed in the subclavian vein, which is in line with the recommendations of the official guidelines for vascular approaches. Namely, Vascular Access Society and European guidelines for hemodialysis (EBPG) recommend the right jugular vein whenever possible [19, 20]. However, the fact that the percentage of temporal femoral catheter is on the rise can be explained by unfavorable population structure.
Temporal vascular catheters were placed in 35 centers. The number of centers where nephrologists and vascular surgeons place temporary catheters is decreasing, while the number of anesthesiologists is increasing. The reason could be an insufficient number of trained nephrologists for this type of activity, while the placement of central line represents the everyday activities of anesthesiologists. The number of nephrologists should be higher given the fact that it falls within the scope of required activities of postgraduate education at our university. Although we are pleased with the outcome, we should consider including more nephrologists in the creation of vascular accesses due to the positive experience of some centers [9].
The VAR is a great success and significant contribution to the Serbian nephrology community because they encompass data from all hemodialysis centers in Serbia including incident and prevalent data. Even the DOPPS analyses included random samples of the HD patients in each dialysis center, and the database is limited to only several, mainly developed countries. However, this work has its limitations. Bearing in mind that it is based on a questionnaire, many details could not be taken into account as, for example, the patency of access, early and late complications, maturation time, the number of reinterventions and patients’ outcome. According to Goodkin et al. [21] after adjustment for vascular access, the hazard ratio for mortality in the USA significantly decreased from 1.56 to 1.06 as compared with Europe. Although we did not analyze likelihood to be treated with an AVF, we are aware that this analysis may be crucial for the further improvement of the incidence of native AVF, but we found very complicated to get such data from the questionnaire. This issue will certainly be the subject analysis of some of the following publications.
According to previous publications, female patients and patients older than 80 years were least likely to start HD with an AVF [13], and probability to use fistula was significantly higher in patients with polycystic kidney disease, predialysis nephrology care for more than 2 years and steady chronic kidney disease progression [18]. Still, we find this report very useful showing that even with limited resources favorable results could be achieved.
Conclusion
The Vascular Access Registry enables us to keep the standard of care of ESRD patients at high level and to prevent a negative trend by evaluating the following: preoperative diagnostics, continuous monitoring of vascular access, education of nephrovascular teams and postoperative care including adequate puncturing of vascular access. This goal can be achieved only through the interactive engagement of all members of the team including surgeons, nephrologists and dialysis nurses. Bearing in mind the inadequate number of renal transplants, the care for vascular access is the best way to ensure the longevity of our patients.
References
Ng Y-Y, We S-C, Hung Y-N, Ko P-J (2009) Effect of demographic characteristics and timing of vascular access maturation on patency in Chinese incident haemodialysis patients. Nephrol Dial Transplant 24(11):3447–3453
Vascular Access 2006 Work Group (2006) Clinical practice guidelines for vascular access. Am J Kidney Dis 48(Suppl 1):S176–S247
Zangan SM, Falk A (2009) Optimizing arteriovenous fistula maturation. Semin Interv Radiol 26(2):144–150
The AV fistula first breakthrough initiative coalition: arteriovenous fistula first website. http://www.fistulafirst.org. About fistula first, fistula first catheter last (FF/CL) data, July 2003–April 2012 graphs, graphs of prevalent AV fistula use rates, by network. Accessed 9 Sept 2013
Jindal K, Chan CT, Deziel C, Hirsch D, Soroka SD, Tonelli M, Culleton BF, Canadian Society of Nephrology Committee for Clinical Practice Guidelines (2006) Hemodialysis clinical practice guidelines for the Canadian Society of Nephrology. J Am Soc Nephrol 17(3 Suppl 1):S1–S27
National Kidney Foundation (2006) Clinical practice guidelines for vascular access. Am J Kidney Dis 48(Suppl 1):S176–S247
Pisoni RL, Zepel L, Port FK, Robinson BM (2015) Trends in US vascular access use, patient preferences, and related practices: an update from the US DOPPS practice monitor with international comparisons. Am J Kidney Dis 65(6):905–915
Yearly report on renal replacement therapy in Serbia, 2013: Annual report on vascular access for hemodialysis in Serbia, 2013. http://www.udruzenjenefrologa.com/en/registry-andrecommendations/. Accessed 13 Feb 2016
Malovrh M (2015) Vascular access creation and care should be provided by nephrologists. J Vasc Access 16(Suppl 9):S20–S23
Ravani P, Marcelli D, Malberti F (2002) Vascular access surgery managed by renal physicians: the choice of native arteriovenous fistulas for hemodialysis. Am J Kidney Dis 40(6):1264–1276
Konner K, Hulbert-Shearon TE, Roys EC, Port FK (2002) Tailoring the initial vascular access for dialysis patients. Kidney Int 62(1):329–338
Mishler R (2009) Autologous arteriovenous fistula creation by nephrologists. Adv Chronic Kidney Dis 16(5):321–328
Noordzij M, Jager K, van der Veer S, Kramar K, Collart F, Heaf JG, Stojceva-Taneva O, Leivestad T, Buturovic-Ponikvar J, Benitez Sanchez M, Moreso F, Prutc KG, Severn A, Wanner C, Vanholder R, Ravani P (2014) Use of vasculat access for hemodialysis in Europe: a report from the ERA EDTA registry. Nephrol Dial Transplant 29:1956–1964
Stojceva-Taneva O, Selim G (2014) Vascular access in hemodialysis patients—registry data. Hippokratia 18(3):209–211
Ravani P, Gillespie BW, Quinn RR, MacRae J, Manns B, Mendelssohn D, Tonelli M, Hemmelgarn B, James M, Pannu N, Robinson BM, Zhang X, Pisoni R et al (2013) Temporal risk profile for infectious and noninfectious complications of hemodialysis access. J Am Soc Nephrol 24:1668–1677
The AV Fistula first breakthrough initiative coalition: arteriovenous fistula first website, 2015. http://www.fistulafirst.org.FFCL-Dashboard-Jun2014.xlsx. Accessed 23 Dec 2015
van der Veer SN, Ravani P, Coentrão L, Fluck R, Kleophas W, Labriola L, Hoischen SH, Noordzij M, Jager KJ, van Biesen W (2015) Barriers to adopting a fistula-first policy in Europe: an international survey among national experts. J Vasc Access 16(2):113–119
Roca-Tey R, Arcos E, Comas J, Cao H, Tort J, Registre de Malalts Renals de Catalunya (RMRC), Organització Catalana de Trasplantaments (OCATT), Health Department of Catalonia, Catalonia—Spain (2015) Vascular access for incident hemodialysis patients in Catalonia: analysis of data from the Catalan renal registry (2000–2011). J Vasc Access 16(6):472–479
Vascular Access Society, home page, guidelines, 10. Central venous access, Guidelines 10.3. http://wwwvascularaccesssociety.com/intro/guidelines. Accessed 20 Aug 2015
Tordoir J, Canaud B, Haage P, Konner K, Basci A, Fouque D, Kooman J, Martin-Malo A, Pedrini L, co Pizzarelli F, Tattersall J, Vennegoor M, Wanner C, ter Wee P, Vanholder R (2007) EBPG on vascular access. Guideline 10.3 Central venous access. Nephrol Dial Transplant 22(Suppl 2):112–113
Goodkin DA, Pisoni RL, Locatelli F, Port FK, Saran R (2010) Hemodialysis vascular access training and practices are key to improved access outcomes. Am J Kidney Dis 56(6):1032–1042
Acknowledgments
We kindly acknowledge colleagues from the Serbian HD Centers contributing to the study (in alphabetical order): Andric Branislav, Antic Miodrag, Aracki Snezana, Arsenovic Aleksandra, Berto Sabo Anika, Bogdanovic Jasmina, Cekovic Biljana, Cuckovic Cedomir, Cukic Zoran, Cveticanin Anica, Djordjevic Verica, Dudic Svetlana, Gajic Snezana, Gojakovic Biljana, Golubovic Predrag, Gucic Ljubinka, Hadzibulic Edvin, Hadzifejzovic Mersada, Hamzagic Nedim, Haviza-Lilic Branimir, Ilic Mira, Ilic Nasta, Jelacic Rosa, Kostic Mirjana, Kovacevic Miodrag, Lazarevic Tatjana, Markovic Rodoljub, Micunovic Vesna, Milenkovic Olgica, Milenkovic Radomir, Milenkovic Srboljub, Milicevic Biserka, Milicevic Olivera, Nikolic Zora, Obrenovic Slavica, Orescanin Mira, Pavlovic Stevan, Pesic Snezana, Petkovic Dobrila, Pilipovic Dragana, Prokopovic Miomir, Radovanovic Zoran, Rakic Nenad, Rangelov Vanja, Sefer Kornelija, Sibalic Simin Marija, Stefanovic Nikola, Stojanovic Dragoslav, Stojanovic Stanojevic Marina, Tirmenstajn Jankovic Biserka, Vasic Jovanovic Vesna, Vasilic Kokotovic Olivera, Vojinovic Goran, Vuckovic Dragana, Vukelic Vesna, Vukic Jasmina, Zagorac Nikola, Zec Nenad. Work on the vascular access register was promoted by the Serbian Society of Nephrology, and it could never have been carried out without their support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Informed consent
Informed consent was not required for the purposes of this study as it was based upon anonymous patient data and did not involve patient intervention or the use of human tissue samples.
Additional information
An erratum to this article is available at http://dx.doi.org/10.1007/s11255-017-1511-4.
Rights and permissions
About this article
Cite this article
Jemcov, T., Dimkovic, N. Vascular access registry of Serbia: a 4-year experience. Int Urol Nephrol 49, 319–324 (2017). https://doi.org/10.1007/s11255-016-1378-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-016-1378-9