Abstract
Background
Responsiveness to erythropoietin-stimulating agent (ESA) may be associated with mortality risk in hemodialysis (HD) patients. The aim of the present study was to assess the relationship between responsiveness to ESA and long-term outcome in chronic HD patients.
Methods
Patients on HD therapy for more than 6 months were enrolled in this cohort study. The first year was used to assess the longitudinal dialysis status of patients; the subsequent years were used to assess the time-dependent risk of all-cause mortality. Hazard ratios were estimated using a Cox proportional model for the association between ESA dose and hemoglobin (Hb) level and mortality, adjusting for potential confounders. The ESA resistance index (ERI) was determined as the weekly weight-adjusted dose of ESA divided by Hb concentration. Patients were divided into three groups by tertiles of ERI.
Results
Of the 320 subjects enrolled, 105 died during the follow-up period of 70.4 ± 29.0 months. When subjects were stratified by epoetin dose and Hb level into four groups, those who had low Hb despite a high dose of epoetin were associated with the highest risk of mortality among the four groups (adjusted hazard ratio 1.86; 95 % confidence interval 1.25–2.75). These highest risk subjects had older age, lower body mass index, and lower serum levels of albumin, triglyceride, and transferring saturation. The impact of serum albumin and serum ferritin on mortality risk in an adjusted Cox proportional hazards model was in accordance with low Hb and higher ESA. There was no significant difference between the mortality risk and tertile of ERI.
Conclusions
High ESA dose and low Hb level were associated with an increased risk of all-cause mortality. However, the responsiveness to ESA estimated by ERI was not related to mortality risk. These findings suggest that the responsiveness to ESA should be evaluated by different methods in HD patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The development of erythropoiesis-stimulating agent (ESA) has resulted in substantial health benefits for patients with end-stage renal disease (ESRD), including improved quality of life, reduced blood transfusion requirements, and enhanced exercise capacity [1]. Unfortunately, a considerable proportion of ESRD patients exhibit a suboptimal hematologic response to ESA, as evidenced by the persistence of anemia despite adequate dosing, or the requirement of high-dose ESA to achieve recommended hemoglobin (Hb) targets [2]. Erythropoiesis-stimulating agent (ESA) dose and achieved Hb levels have been found to be associated with mortality in hemodialysis (HD) patients [3], and hyporesponsiveness to ESA therapy is known to predict poorer outcomes [4]. Both high-dose ESA therapy and low Hb levels may contribute to poorer outcomes in HD patients with hyporesponse to ESA [5–7].
Many factors causing a dose-response to ESA are known to be associated with an increased risk of mortality in dialysis patients [8, 9]. However, the impact of ESA dose–hemoglobin level interaction on mortality is not precisely understood. ESA responsiveness is generally assessed with ESA dose and Hb level, and physicians commonly adjust ESA dosage according to Hb level. The Kidney Disease Outcomes Quality Initiative (KDOQI) guidelines [10] and European Best Practice guidelines [11] define ESA hyporesponsiveness as a continued need for greater than 300 IU/kg/week epoetin or 1.5 μg/kg/week darbepoetin administered by the subcutaneous route. However, given that the mean ESA dosage in Japan is less than one third that in the United States [12], whether the association between ESA responsiveness and all-cause mortality is similar for lower ESA dosages is uncertain.
The aim of the present study was to clarify the relationship between responsiveness to ESA and long-term outcome in chronic HD patients.
Subjects and methods
Study design and subjects
The present study was a retrospective, observational cohort study conducted in a single center in Japan. The study subjects were recruited from patients who had been routinely treated in the dialysis unit of the Hidaka Hospital for at least 6 months. HD patients, who were suffering from septicemia and severe illness, were excluded and transferred to another dialysis unit for intensive care. The enrolled patients (n = 320) underwent stable regular HD using bicarbonate dialysate. The underlying diseases of ESRD were diabetic nephropathy (n = 109), chronic glomerulonephritis (n = 108), nephrosclerosis (n = 69), chronic pyelonephritis (n = 12), and unknown origin (n = 22). Autosomal dominant polycystic kidney disease with often higher Hb level and lower ESA requirement were excluded. The study was divided into two study periods to evaluate the time-dependent risk of mortality based on subjects’ longitudinal dialysis status. The first phase (12 months) was used to collect laboratory data to evaluate longitudinal dialysis status. The second phase (the subsequent 5 years) was used to evaluate the time-dependent risk of mortality. In order to use longitudinal dialysis status as a predictive value, laboratory data were not measured during the second phase. The ESA resistance index (ERI) was determined as the weekly weight-adjusted dose of epoetin (IU/kg/week) divided by Hb concentration (g/dL), as previously described [13]. Patients were divided into three groups by tertiles of ERI as follows: Tertile 1, ERI = 0–6.04; Tertile 2, ERI = 6.04–12.21; and Tertile 3, ERI = 12.21 IU/kg/week/g/dL.
Blood pressure was recorded three times with a brachial sphygmomanometer after the subject had rested in the supine position for at least 10 min, and the average value of the three measurements was adopted. Blood was collected at entry to measure routine laboratory parameters, including hemoglobin concentration, serum levels of urea nitrogen, albumin, calcium, phosphorus, intact parathyroid hormone, total cholesterol, high-density-lipoprotein (HDL) cholesterol, triglyceride, low-density-lipoprotein (LDL) cholesterol, and C-reactive protein (CRP). With regard to urea kinetics, we measured a blood-based dialysis parameter, Kt/V [14]. Mean values of 3 measurements during the 12 months before the start of this study were used for analysis. Information on antihypertensive agents including angiotensin-converting enzyme inhibitors, angiotensin receptor blockers, calcium channel blockers, and beta-blockers was collected from medical records.
The subjects included in the study were in census for 12 consecutive months from January 1, 2005 to December 31, 2005. During this period, laboratory data were measured monthly before the first dialysis session of the week and the data were averaged. Those who failed to complete the study or died during the first phase were excluded. Subjects’ baseline characteristics consisted of their age, sex, presence of diabetes mellitus (diabetes), and period on dialysis. The Institutional Review Board of the Hidaka Hospital approved all study protocols, which were performed in accordance with the Declaration of Helsinki guidelines regarding ethical principles for medical research involving human subjects. Informed consent was obtained from all study subjects after information about the study.
Anemia treatment strategy
Subjects’ anemia was treated according to the guidelines published in 2004 by the Japanese Society of Dialysis Therapy (JSDT) [15]. The target Hb level was 10–11 g/dL; epoetin beta was administered to achieve the target Hb level. Intravenous iron was administered if a subject’s transferrin saturation was <20 % or serum ferritin level was <100 ng/mL.
Statistical analysis
A normally distributed, unpaired continuous value was expressed as mean ± SD and compared using analysis of covariance (ANOVA) or Student’s t test. Nonparametric values were expressed as medians and interquartile ranges and compared using the Mann–Whitney test. Categorical values were expressed as percentages and compared using the chi-squared test. A p value <0.05 was considered to be statistically significant. Survival analysis was based on the Kaplan–Meier curve with subjects censored for death. A log-rank test was used to compare the survival rate between two groups. A univariate or multivariate Cox proportional hazards model was used to evaluate the mortality risk, adjusting for multivariate factors. Results were expressed as a hazard ratio (HR) with 95 % confidence intervals (CIs). All statistical analyses were performed by using the JMP version 9.0 software program (SAS Institute Inc., Cary, NC, USA) for Windows personal computers.
Results
Baseline characteristics of the study subjects
Baseline characteristics are shown in Table 1. Subjects had a mean age of 62.52 years, 33.9 % had diabetes, and the average dialysis vintage was 8.12 years. The mean Kt/V was 1.12 ± 0.22. Antihypertensive agents were prescribed in 42.7 % of the subjects.
Follow-up
The mean follow-up period was 70.4 ± 29.0 months. Of the 320 enrolled subjects, 105 died during the follow-up period. The causes of death were cardiovascular disease in 44 (41.9 %) subjects and non-cardiovascular diseases including infection and malignancy in 61 (58.1 %) subjects.
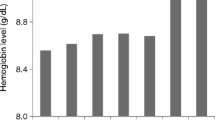
Average Hb Level and all-cause mortality risk
In order to assess the all-cause mortality risk in association with average Hb level, subjects were divided into three categories according to Hb level (<10, ≥10 and <11, and ≥11 g/dL), which were based on the recommended range of Hb level according to the 2004 JSDT renal anemia guidelines. In this analysis, subjects with the lowest Hb had the worst outcome compared with subjects with the highest Hb level: Hb < 10 versus Hb > 11 g/dL: HR 0.58, 95 % CI 0.34–0.95 (p = 0.0303); Hb < 10 versus Hb > 10 and <11 g/dL: HR 0.54, 95 % CI 0.35–0.82 (p = 0.0034). A Kaplan–Meier curve of survival probability according to average Hb level is shown in Fig. 1.
Epoetin dose and all-cause mortality risk
In order to assess the association between epoetin dose and all-cause mortality rate, subjects were divided into three categories according to the tertile of their epoetin dose (T1:<60; T2: ≥60 and <120; T3: ≥120 IU/kg/week). Time-dependent analyses of time of death revealed that there was no significant association between epoetin dose and mortality risk (p = 0.9946). The results are shown in Fig. 2.
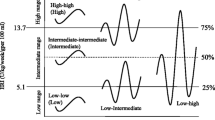
Relation of epoetin dose and Hb level to all-cause mortality risk
To assess the all-cause mortality risk of responsiveness to epoetin, subjects were divided into four categories according to average Hb level and epoetin dose. Low Hb was defined as an average Hb level<10 g/dL, and a high epoetin dose was defined as the highest tertile of epoetin. The groups were as follows—Group 1: ESA > 120 IU/kg/week and Hb < 10 g/dL, n = 43; Group 2: ESA < 60 and Hb < 10, n = 101; Group 3: ESA > 120 and Hb > 10, n = 37; Group 4: ESA < 60 and Hb > 10, n = 140. Age at entry was significantly higher (p = 0.001), and body mass index (p = 0.001) and serum albumin (p < 0.001) were significantly lower in Group 1 compared to the other groups (Table 2). Serum triglyceride was also significantly lower in Group 1 compared to the other groups (p = 0.02). The average CRP level tended to be higher in Group 1 compared to the other groups, but did not reach the statistical significance.
A Kaplan–Meier survival analysis showed the worst outcome for Group 1 (Fig. 3). A log-rank test confirmed a significantly worse outcome for Group 1 compared to the other groups—Group 1 versus Group 4: HR 0.51, 95 % CI 0.33–0.77 (p = 0.0015); Group 1 versus Group 3: HR 0.57, 95 % CI 0.29–1.04 (p = 0.0704); Group 1 versus Group 2 (p = 0.4068). A Cox proportional hazards model showed that patients with low Hb receiving high ESA (Group 1) have a significantly higher risk of all-cause mortality even after adjusting for the demographic factors of age, sex, dialysis vintage, body mass index, and serum albumin (unadjusted HR 1.77, 95 % CI 1.21–2.55; adjusted HR 1.86, 95 % CI 1.25–2.75) (Table 3). In addition, the presence of diabetes (unadjusted HR 1.72, 95 % CI 1.18–2.48; adjusted HR 2.12, 95 % CI 1.34–3.34), older age (unadjusted HR 1.05, 95 % CI 1.03–1.07; adjusted HR 1.06, 95 % CI 1.04–1.08), lower serum albumin (unadjusted HR 0.36, 95 % CI 0.25–0.53; adjusted HR 0.62, 95 % CI 0.41–0.98), and higher serum ferritin (unadjusted HR 1.00, 95 % CI 1.00–1.00; adjusted HR 1.00, 95 % CI 1.00–1.00) were significant variables associated with all-cause mortality risk.
Association between ERI and mortality risk
During the mean follow-up period was 70.4 ± 29.0 months, 44 (41.9 %) of the 320 enrolled subjects had cardiovascular events. Figure 4 shows the Kaplan–Meier curve for the cumulative events-free survival according to the tertile of ERI. There was no significant difference in the mortality risk among the three groups (p = 0.5243).
Discussion
In the present study, we found that ESA responsiveness, defined based on ESA dose and Hb level, was associated with long-term mortality risk after adjustment for potential confounding factors. In particular, the worst outcomes were noted in hyporesponsive patients with low Hb levels receiving high-dose ESA therapy. In a Cox proportional hazards model, the significantly increased all-cause mortality risk associated with higher epoetin dose and lower Hb level was not attenuated by adjustment for age, presence of diabetes, serum levels of albumin, and serum ferritin. However, the responsiveness to ESA estimated by ERI was not related to mortality risk. These findings suggest that both ESA dose and Hb level should be considered simultaneously when evaluating the relationship between renal anemia and mortality risk, and ESA responsiveness estimated by different methods has prognostic importance in anemia management.
Regidor et al. [16] conducted a 2-year-observational cohort study. When subjects were stratified into four categories according to weekly dose of ESA, there was an inverse relationship between ESA dose and risk of mortality. However, there was also an inverse relationship between ESA dose and Hb level. Since the percentage of patients who achieved target Hb was lower in the higher ESA dose group, their poor outcomes may have been due to lower responsiveness to ESA. Szczech et al. [17] examined data from a secondary analysis of the CHOIR study and also reported that the inability to achieve a target Hb level and a high-dose epoetin alfa were associated with an increased risk of primary endpoints including death, myocardial infarction, congestive heart disease, or stroke, supporting the hypothesis that lower responsiveness to ESA is associated with increased risk of mortality.
In our present study, poor prognosis was seen among subjects receiving higher doses of epoetin. However, when subjects were categorized into four groups according to epoetin dose and average Hb level, it was only the subjects with higher epoetin dose and lower Hb level who had a poor prognosis. These findings are similar to the results from a Japanese cohort study [18]. Fukuma et al. [18] found that low Hb level and high-dose ESA therapy were both associated with all-cause mortality. Adjusted HRs for high-dose ESA with low Hb level were 1.94 for all-cause mortality and 2.02 for cardiovascular mortality. They also noted the interaction between ESA dosage and Hb level on all-cause mortality (p = 0.002). Taken together, they concluded that mortality can be affected by ESA responsiveness, which may include independent and interactive effects of ESA dose and Hb level.
ESA responsiveness is relative, not absolute; the 2 determinants of responsiveness are ESA dose and Hb level. Previous studies have demonstrated that the resistance to ESA was associated with both the all-cause mortality and cardiovascular mortality in patients with ESRD [3, 16, 19]. The ERI has been considered useful to assess the ESA resistance. However, the follow-up period of the previous studies was relatively short (i.e., 1 or 2 years). In the present study, we showed that the ERI was not associated with mortality risk during the mean follow-up period of 70.4 ± 29.0 months. Because ERI was calculated based on baseline data, the ERI may be changed during a long-term follow-up period.
ESA responsiveness varies widely depending on a number of clinical factors [5–7]. In a Cox proportional hazards model, older age, diabetes, low serum albumin level, and high serum ferritin level were found to be associated with all-cause mortality in the present study. These findings suggest that older diabetic patients with malnutrition and inflammation have higher mortality risk. Chronic inflammation is a common feature of ESRD as a major cause of morbidity and mortality and link to the development of the malnutrition–inflammation–atherosclerosis (MIA) syndrome [20]. Anemia appears to be an important element linking the MIA syndrome with elevated proinflammatory cytokines with poor patient outcomes. Moreover, the MIA syndrome has found to be associated with hyporesponsiveness to ESA [21]. Abe et al. [22] has recently reported that diabetic HD patients with MIA syndrome have a lower response ESA. Taken together, hyporesponsiveness to ESA in accordance with MIA syndrome can be associated with higher mortality risk in chronic HD patients. Further, prospective investigation is needed to confirm these hypotheses.
Our present study has several limitations. First, baseline data were used to define exposure categories in this cohort, and we were unable to examine the effect of changes from the baseline category during follow-up as previously described [23]. Second, since this was a single-center cohort study, data and results may not be representative of HD patients in other countries, particularly given that ESA dose and Hb level generally are lower in Japan than in other countries. However, the mortality rate and other baseline characteristics in our present cohort are similar to those for general Japanese dialysis patients [24]. Third, due to the reimbursement policy in Japan, the average dose of epoetin is less than those used in other countries [25]. Until April 2006, the maximum dose of epoetin had been limited to 9,000 U/week of epoetin alfa or epoetin beta. Fourth, the present cohort size is small. However, the follow-up period of our cohort (70.4 ± 29.0 months) was longer than that of previous studies [9, 13, 18].
In summary, we examined HD patients in a single center and assessed the risk of all-cause mortality associated with the responsiveness to ESA, defined based on ESA dose and Hb levels and ERI. Low Hb level despite a high-dose epoetin was associated with higher mortality risk. However, ERI was not related to mortality risk. These findings suggest that combination of ESA dose and Hb level may have independent and interactive effects on all-cause mortality. The responsiveness to ESA should be evaluated by different methods. In the future study, more attention should be focused on background factors that cause responsiveness to ESA in addition to the effort to achieve a target Hb level.
References
Eschbach JW, Egrie JC, Downing MR et al (1987) Correction of the anemia of end-stage renal disease with recombinant human erythropoietin. Results of a combined phase I and II clinical trial. N Engl J Med 316:73–78
Macdougall IC, Cooper A (2002) The inflammatory response and epoetin sensitivity. Nephrol Dial Transplant 17(Suppl 1):48–52
Zhang Y, Thamer M, Stefanik K et al (2004) Epoetin requirements predict mortality in hemodialysis patients. Am J Kidney Dis 44:866–876
Kilpatrick R, Critchlow C, Fishbane S et al (2008) Greater epoetin alfa responsiveness is associated with improved survival in hemodialysis patients. Clin J Am Soc Nephrol 3:1077–1083
Locatelli F, Pisoni R, Combe C, Bommer J, Andreucci VE, Piera L, Greenwood R, Feldman HI, Port FK, Held PJ et al (2004) Anaemia in haemodialysis patients of five European countries: association with morbidity and mortality in the Dialysis Outcomes and Practice Patterns Study (DOPPS). Nephrol Dial Transplant 19:121–132
Robinson BM, Joffe MM, Berns JS et al (2005) Anemia and mortality in hemodialysis patients: accounting for morbidity and treatment variables updated over time. Kidney Int 68:2323–2330
Szczech LA, Barnhart HX, Inrig JK et al (2008) Secondary analysis of the CHOIR trial epoetin-alpha dose and achieved hemoglobin outcomes. Kidney Int 74:791–798
Johnson DW, Pollock CA, Macdougall IC (2007) Erythropoiesis-stimulating agent hyporesponsiveness. Nephrology (Carlton) 12:321–330
Kalantar-Zadeh K, Lee GH, Miller JE et al (2009) Predictors of hyporesponsiveness to erythropoiesis-stimulating agents in hemodialysis patients. Am J Kidney Dis 53:823–834
KDOQI Clinical practice guidelines and clinical practice recommendations for anemia in chronic kidney disease (2006) Am J Kidney Dis 47 (5 Suppl 3): S16–S145
Locatelli F, Aljama P, Bárány P (2004) European best practice guidelines working group: Revised European best practice guidelines for the management of anaemia in patients with chronic renal failure. Nephrol Dial Transplant 19 (Suppl 2): ii1-ii47
Akizawa T, Pisoni RL, Akiba T (2008) Japanese haemodialysis anaemia management practices and outcomes (1999–2006): results from the DOPPS. Nephrol Dail Transplant 23:3643–3653
Chung S, Song HC, Shin SJ et al (2012) Relationship between erythropoietin resistance index and left ventricular mass and function and cardiovascular events in patients on chronic hemodialysis. Hemodial Int 16:181–187
Daugirdas JT (1993) Second generation logarithmic estimates of single-pool variable volume Kt/V: an analysis of error. J Am Soc Nephrol 4:1205–1213
Gejyo F, Saito A, Akizawa T et al (2004) Japanese society for dialysis therapy. Ther Apher Dial 8:443–459
Regidor D, Kopple J, Kovesdy C (2006) Associations between changes in hemoglobin and administered erythropoiesis-stimulating agent and survival in hemodialysis patients. J Am Soc Nephrol 17:1181–1191
Szczech LA, Barnhart HX, Sapp S et al (2010) A secondary analysis of the CHOIR trial shows that comorbid conditions differentially affect outcomes during anemia treatment. Kidney Int 77:239–246
Fukuma S, Yamaguchi T, Hashimoto S et al (2012) Erythropoiesis-stimulating agent responsiveness and mortality in hemodialysis patients: results from a cohort study from the dialysis registry in Japan. Am J Kidney Dis 59:108–116
Kalantar-Zadeh K, McAllister CJ, Lehn RS et al (2003) Effect of malnutrition-inflammation complex syndrome on EPO hyporesponsiveness in maintenance hemodialysis patients. Am J Kidney Dis 42:761–773
Stenvinkel P (2001) The role of inflammation in the anaemia of end-stage renal disease. Nephrol Dial Transplant 16(Suppl 7):36–40
Smrzova Jm Balla J, Barany P (2005) Inflammation and resistance to erythropoiesis-stimulating agents-What do we know and what needs to be clarified? Nephrol Dial Transplant 20 (Suppl 8): viii2–viii7
Abe M, Okada K, Maruyama T, Maruyama N, Matsumoto K, Soma M et al (2011) Relationship between erythropoietin responsiveness, insulin resistance, and malnutrition-inflammation-atherosclerosis (MIA) syndrome in hemodialysis patients with diabetes. Int J Artif Organs 34:16–25
Kaysen GA, Muller HG, Ding J, Chertow GM (2006) Challenging the validity of the EPO index. Am J Kidney Dis 47:157–166
Nakai S, Iseki K, Itami N et al (2012) An overview of regular dialysis treatment in Japan (as of 31 December 2010). Ther Apher Dial 16:483–521
Hasegawa T, Bragg-Gresham JL, Pisoni RL et al (2011) Changes in anemia management and hemoglobin levels following revision of a bundling policy to incorporate recombinant human erythropoietin. Kidney Int 79:340–346
Acknowledgments
The authors are very grateful to dialysis staff who understood the clinical importance of this study and who provided high-quality data in Hidaka Hospital. This study was in part supported by a grant from Japan Promotion Society for Cardiovascular Disease.
Conflict of interest
The authors have no conflicts of interest to declare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ogawa, T., Shimizu, H., Kyono, A. et al. Relationship between responsiveness to erythropoiesis-stimulating agent and long-term outcomes in chronic hemodialysis patients: a single-center cohort study. Int Urol Nephrol 46, 151–159 (2014). https://doi.org/10.1007/s11255-013-0494-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-013-0494-z