Abstract
Venous thrombosis (VT) is a complex multi-factorial disease and a major health concern worldwide. Its clinical implications include deep vein thrombosis (DVT) and pulmonary embolism (PE). VT pathogenesis involves intricate interplay of various coagulants and anti-coagulants. Growing evidences from epidemiological studies have shown that many non-coding microRNAs play significant regulatory role in VT pathogenesis by modulating expressions of large number of gene involved in blood coagulation. Present study aimed to investigate the effect of human micro RNA (hsa-miR)-320a antagonist on thrombus formation in VT. Surgery was performed on Sprague–Dawley (SD) rats, wherein the inferior vena cava (IVC) was ligated to introduce DVT. Animals were divided into four groups (n = 5 in each group); Sham controls (Sham), IVC ligated-DVT (DVT), IVC ligated-DVT + transfection reagent (DVT-NC) and IVC ligated-DVT + miR320a antagonist (DVT-miR-320a antagonist). IVC was dissected after 6 h and 24 h of surgery to estimate thrombus weight and coagulatory parameters such as levels of D-dimer, clotting time and bleeding time. Also, ELISA based biochemical assays were formed to assess toxicity of miRNA antagonist in animals. Our experimental analysis demonstrated that there was a marked reduction in size of thrombus in hsa-miR-320a antagonist treated animals, both at 6 h and 24 h. There was a marked reduction in D-dimer levels in hsa-miR-320a antagonist treated animals. Also, blood clotting time was delayed and bleeding time was increased significantly in hsa-miR-320a antagonist treated rats compared to the non-treated and Sham rats. There was no sign of toxicity in treated group compared to control animals. Hsa-miR-320a antagonist could be promising therapeutic target for management of VT.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Highlights
-
1.MicroRNAs regulate a large number of genes and thus play a major role in pathogenesis of complex diseases like venous thrombosis.
-
2.Ligation of inferior vena cava (IVC) introduces thrombus formation (DVT) in rat model.
-
3.Intravenous introduction of hsa-miR-320a antagonist into IVC ligated rats decrease the size and weight of thrombus significantly.
-
4.Hsa-miR-320a antagonist (1mg/kg body wt.) did not cause any lethality in rats and no visible signs of toxicity.
-
5.Hsa-miR-320a antagonist could be a promising therapeutic target for treatment of venous thrombosis.
Introduction
Venous thrombosis (VT) is the third most common cardiovascular disease with annual incidence rate of 1–2 individuals per 1000 and having chances of long term post thrombotic complications and recurrence [1,2,3]. It mainly comprises of two clinical manifestation including deep vein thrombosis (DVT) and pulmonary embolism (PE), the later one being potentially fatal. Sufficient epidemiological data has revealed that VT is a complex disease governed by several acquired and inherited risk factors [4, 5]. Apart from several predisposing factors such as cancer [6], cardiovascular diseases [7], trauma [8] and surgery [9], hypoxic conditions at high altitude (HA) have been regarded as independent risk factor to venous thrombosis, increasing risk of VT occurrence upto 30 times on exposure to HA [10,11,12]. Hypobaric hypoxic conditions prevailing at HA trigger various haematological changes including transient hypercoagulability and increased hematocrit volume and hemoglobin due to production of erythropoietin [12,13,14].
The disturbance in blood flow acts as triggering factor for deep vein thrombosis [15], however the sequence of molecular and cellular events resulting in formation of thrombus remains unclear. In humans, an event of VT is not essentially linked to endothelial injury [16, 17]. In animals, ligation of inferior vena cava, restricts blood flow through the vessels, without causing endothelial injury. Thus, DVT model of animals involving IVC stenosis-induced DVT, mimics human DVT in most appropriate manner [18, 19].
Small non-coding RNAs called MicroRNAs (miRNAs) modulate gene expression at post transcriptional level either by degradation of mRNA or by translational repression of targets [20]. MiRNA binds to the 3ʹ-untranslated region of target to form silencing complexes, thus inducing degradation [21, 22]. Each miRNA can potentially target a large number of genes and hence can modulate multiple biological pathways at the same time [23], Selbach et al. 2008). In the last one decade, number of studies has demonstrated that circulating miRNAs could serve as potential biomarkers in various diseases such as cancer, Myocardial infarction, liver diseases etc. [24,25,26]. Also, the critical role of specific miRNAs in vascular diseases such as atherosclerosis, vascular inflammation, coronary artery disease etc. has been highlighted [27,28,29]. Various bioinformatic approaches have been applied earlier to identify potential miRNAs involved in blood coagulation and VTE pathophysiology [30,31,32,33], however precise role of miRNAs in etiopathology of VTE is not elucidated.
Present study aims to identify potential miRNA target that can modulate genes involved in blood coagulation and could be used as therapeutic target for VTE treatment.
Materials and Methods
Bioinformatic approach to identify potential miRNA and its target genes it regulates
A through literature survey was done to identify the miRNAs associated with venous thrombosis, DVT and PE. Manual search was conducted on PubMed, Google Scholar and Science Direct using common key search terms. The search results were carefully analyzed to identify most suitable miRNA candidate that has been experimentally proven to play a significant role in VTE susceptibility.
Study groups
Experiments were conducted in accordance with the guidelines of Animal ethical norms laid by Committee for the Purpose of Control and Supervision of Experiments on Animals, Government of India. All experimental protocols were, including euthanasia were approved by Institutional animal ethical committee (IAEC) of Defence Institute of Physiology and Allied Sciences (DIPAS) (approval ID: IAEC/DIPAS/2021-22-Ext/06). For the present study, male Sprague–Dawley (SD) rats kept in standard laboratory conditions, weighing up to 250–300 g were selected. The study protocols were in accordance to the ARRIVE guidelines (https://arriveguidelines.org).
Animals used for the present study were divided into four groups randomly. Firstly, those who were operated for midline laprotomy and bowel manipulation without IVC ligation (Sham controls). Second set of animals were those who were operated to introduce thrombus formation by IVC ligation (DVT group). The third experimental group of animals were those in which only transfection reagent was injected (without miRNA), one hour prior to IVC ligation (DVT-NC). Lastly, fourth group of animals were injected with miR-320a antagonist after complexation with transfection reagent, invivofectamin 3.0 (Invitrogen) (DVT-miR-320a antagonist). Each experimental group comprised of five rats (n = 5). Two set of experiments were run and animals were sacrificed after 6 h and 24 h for performing thrombotic and biochemical assays (Table 1).
MiR-320a antagonist for in vivo delivery
MiRNA inhibitor (antagonist) of hsa-miR-320 (in vivo grade) was synthesized from Invitrogen, Thermo Fischer Scientific. It was suspended in transfection reagent, invivofectamine 3.0 (Invitrogen, Thermo Fischer Scientific) according to manufacturer’s instructions. Briefly, to prepare 1 ml of 0.1 mg/ml complex, 100 µl of 1.2 mg/ml miRNA solution was prepared by mixing miRNA duplex solution (2.4 mg/ml) and complexation buffer in a ratio of 1:1. Added this miRNA solution to 100 µl of Invivofectamine 3.0, at room temperature and vortex. Incubated Invivofectamine 3.0-miRNA duplex mixture for 30 min at 50 ºC. Centrifuged the tube briefly. Diluted the complex 6 folds by adding 1 ml of PBS (pH 7.4). Dose of miRNA angonist was standardized to 1 mg/kg of animals. This dose was equivalent to 200 µl of 0.1 mg/ml solution prepared, i.e., approx. 1 µl/g dose for 250 g rats. Each animal was administered 200 µl of solution (invivofectamine + DVT-miR-320a anatagonist/ or distill water in case of DVT-NC group) by tail vein one hour before IVC ligation (as described by [34, 35].
IVC ligation of rats to induce thrombus formation
Flow restriction animal model was used to for studying stasis induced thrombosis. Briefly, the animal was first allowed to acclimatize to the room environment to relieve stress. A small dose of Ketamine (100 mg/kg) and Xylazine (20 mg/kg) was injected into the animal according to its body weight to anesthetize the rats. Incision was made into a straight central body followed by opening of layer beneath and medial line of symmetry. Once the abdomen is open, the intestine and other organs were taken out and PBS was added from above to prevent its drying. To induce the thrombus in the animals, midline laprotomy was performed, blood flow was restricted by proximal ligation of the inferior vena cava (IVC) below the renal veins and lateral tributaries ligation as described by [36]. A prolene suture (non-reactive, 3.0) was used for IVC ligation below the renal veins on left and visible lateral branches [37]. The organs were then carefully placed back into the peritoneal cavity and the inner and outer layers of skin were stitched. Applied povidine-iodine ointment onto the suture to avoid post surgical infections and the animal was bandaged with adhesive tapes. Intra mascular Diclophenac (pain reliever) and Gentamycin injection (anti-biotic) was given to the animals after surgery. The animals were properly marked and kept in a separate cage with food and water. Animals were kept under close watch for their physical activity till it regained consciousness.
Animals were euthanized after 6 h and 24 h of surgery and the IVC was carefully dissected. Size and weight of thrombus was measured for each rat.
Coagulatory parameters
To calculate clotting time, a small sample of blood was collected in a micro-centrifuge tube (pre-incubated at 37 ºC) by retro-orbital puncture. The tube was kept in water bath set at 37 ºC and was checked every 20–30 s by tilting. The time taken for blood to clot was carefully noted.
To calculate bleeding time, animals were anesthetized and tail was transacted from the tip about ~ 2.0 mm using a surgical blade. The transacted tail was immediately dipped in 10 ml of isotonic saline solution (0.9% NaCl) in a falcon tube. The time from transaction till the bleeding completely stopped was noted.
Biochemical assays
Biochemical markers for heart, liver and kidneys were determined using Enzyme linked immunosorbent assay (ELISA) in serum samples. These included Gamma-glutamyltransferase (GGT), alkaline phosphatase (ALP), Lactate dehydrogenase (LDH), albumin deficiency marker (NAGase) and aspartate aminotransferases AST) for liver injury; Creatinine for kidney injury; N-terminal pro-brain natriuretic peptide (NT-proBNP), NT-pro-atrial natriuretic peptide (NT-pro-ANP), Cardiac muscle troponin T (cTnT) and Cardiac troponin I (cTnI) for heart failure.
Thrombotic markers
Levels of circulating Prothrombin fragment 1 + 2 and levels of D-dimer, a fibrin degradation product, were measured in rat plasma using commercially available ELISA kit (Elabscience, USA).
Target gene prediction of selected miRNA
In-silico tools were used to predict miRNA gene targets. In order to gain insights into the mechanism by which hsa-miR-320 mediates genes involved in VTE, a list of target genes of hsa-miR-320 was prepared using online databases. MiRNA target prediction was done using miRWalk (http://mirwalk.umm.uni-heidelberg.de/), which consolidates gene targets from three different databases, Targetscan, miRDB and mirTarbase. The gene list thus obtained was subjected to pathway analysis and gene enrichment analysis using online databases.
Results
Identification of target miRNA and its role in blood coagulation
Several studies have shown significant association of a number of miRNAs with venous thrombosis. These include miR-15b-5p, miR-197-3p, miR-27b-3p, and miR-30c-5p [38, 39], hsa-miR-126-3p, hsa-miR-885-5p, hsa-miR-194-5p, and hsa-miR-192-5p [40, 41], miR-191-5p, miR-320a, miR-21-5p, miR-23a-3p, and miR-451a [42] etc. Interestingly, many a number of studies commonly reported differential expression of hsa-miR-320 in VTE [42,43,44], (Xiao et al. 2011, Zhou et al. 2016). Significant up-regulation of hsa-miR-320a in VTE patients have been demonstrated in our previous studies [33], Srivastava et al. [32]. Thus after careful evaluation of existing data, we selected hsa-miR-320a for further study. Mature sequence of hsa-miR-320a (GCCUUCUCUUCCCGGUUCUUCC) is derived from its stem loop sequence CUCCCCUCCGCCUUCUCUUCCCGGUUCUUCCCGGAGUCGGGAAAAGCUGGGUUGAGAGGGCGAAAAAGGAUG, located on chromosome 8 from position 22,244,966 to 22,245,037,
on Build GRCh38. To silence the activity of hsa-miR-320a, the present study uses its antagonist (complementary to its mature miRNA sequence) in order to suppress thrombus growth.
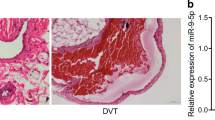
Thrombus weight and size measurement
In general, thrombus weight is proportional to thrombus length, i.e., weight of a thrombus decreases with thrombus length. In the present study, the thrombus weight was measured using laboratory weighing balance while the thrombus length was measured longitudinally using standard scaling method. Ex-vivo measurement of thrombus dimensions is a limitation of the study. Figure 1 shows the marked difference in thrombus size in different experimental groups. Animals treated with hsa-miR-320a antagonist showed marked reduction in weight and size of the thrombus. While no thrombus was formed in SHAM controls, thrombus was formed in other three groups of animals and the hsa-miR-320a antagonist treated animals had smallest thrombus in terms of size and average weight (~ 24 mg), significantly lower than the DVT (~ 38 mg) and DVT-NC (~ 41 mg) group, at both time points 6 h and 24 h. On the other hand, thrombus was of comparable size in experimental groups DVT and DVT-NC groups (Fig. 2).
Effect of systemic delivery of hsa-miR-320a antagonist
Introduction of miR-320a antagonist showed increased clotting and bleeding time in animals. Clotting time was significantly delayed in animals treated with hsa-miR-320a antagonist, both in case of 6 h and 24 h in comparison sham controls, DVT and DVT-NC groups. Another significant observation of the study was marked increase in bleeding time in hsa-miR-320a antagonist treated animals compared to other three study groups.
Toxicity of hsa-miR-320a antagonist
To study the suitability of hsa-miR-320a antagonist in in vivo delivery for VTE therapeutic potential, various toxicity assays were performed. Hsa-miR-320a antagonist did not cause lethality or any visible signs of injury in the animals. Markers indicative of liver injury such as AST, ALP, GGT and LDH did not show any significant difference in plasma levels between the different animal study groups. NAGase levels significantly changed between DVT-miR-320a antagonist treated rats and other three animal groups, both after 6 h and 24 h of introduction (Fig. 3A and B).
A and B Biochemical assays performed on four study groups. Markers for liver injury (a) Aspartate aminotransferases (AST), (b) alkaline phosphatase (ALP), (c) Gamma-glutamyltransferase (GGT), (d) Lactate dehydrogenase (LDH) and (e) albumin deficiency marker, N-acetyl-beta-d-glucosaminidase (NAGase); Kidney Injury, (f) Creatinine; and Heart injury, (g) N-terminal pro-brain natriuretic peptide (NT-proBNP), (h) NT-pro-atrial natriuretic peptide (NT-pro-ANP), (i) Cardiac troponin I (cTnI) and (j) Cardiac muscle troponin T (cTnT) were analyzed using ELISA. These 10 markers were evaluated in experimental sets, 6 h and 24 h. Significant differences were observed in plasma levels of NAGase, Creatinine, and NT-proANP
Levels of creatinine also changed significantly amongst the study groups, both at 6 h and at 24 h. There was a consistent increase in creatinine levels from sham to IVC ligated DVT rats and DVT-NC rats. Furthermore, there was a significant increase in creatinine levels in DVT-miR-320a antagonist treated rats in comparison to all other three study groups. Also, a Natriuretic peptide, NT-proANP, a marker of cardiac injury, was also significantly increased in DVT-miR-320a antagonist treated animals compared to the sham, DVT and DVT-NC rats, both at 6 h and 24 h. The significant increase in these biochemical markers could be due to physiological re-adjustments post introduction of hsa-miR-320a antagonist, however, the changes were non-lethal.
Measurement of thrombotic markers
Both D-dimer and prothrombin fragment 1 + 2 are well established markers of coagulation activation. Levels of these markers were estimated in plasma samples of rats in each study group. The average D-dimer level in sham controls was 336 ng/ml in 6 h and 356 ng/ml in 24 h. The levels of D-dimer increased beyond normal reference range in IVC ligated rats. In DVT rats, the average D-dimer levels were 788 ng/ml in 6 h and 797 ng/ml in 24 h. Similarly, for DVT-NC group D-dimer levels were 794 ng/ml and 812 ng/ml in 6 h and 24 h respectively. Interestingly, in DVT-miR-320a antagonist treated animal group, the levels of D-dimer were as low as that of sham group, i.e., 342 ng/ml in 6 h and 358 ng/ml in 24 h (Fig. 4A).
Estimation of A D-dimer and B prothrombin fragment 1 + 2 levels in Rat plasma amongst four study groups, both after 6 h and 24 h. Both D-dimer and prothrombin fragment 1 + 2 were higher than normal reference range in DVT and DVT-NC group of animals at both time points. The levels of these thrombotic indicators were within normal reference range for DVT-miR320a antagonist treated rats, close to that of sham controls, after 6 h and 24 h
Another thrombotic biomarker, prothrombin fragment 1 + 2 levels showed exactly similar pattern of expression as that of D-dimer. For sham controls, levels of prothrombin fragment 1 + 2 were 544 pg/ml and 564 pg/ml after 6 h and 24 h respectively. The average levels of this marker increased in DVT rats as well as DVT-NC rats ranging from 830 to 864 pg/ml at both time points. However in DVT-miR-320a antagonist treated rats, there was a marked decline in prothrombin fragment 1 + 2 levels. The average estimated levels were 582 pg/ml and 504 pg/ml after 6 h and 24 h respectively (Fig. 4B).
Target validation of miR-320
Target prediction by miRWalk enlisted 63,948 gene targets, with prediction score from 1 to 0.8. After removing the duplicates from this list, 16,456 unique targets were found, which were then subjected to pathway analysis using online tool, Panther [45]. The pathway analysis showed that hsa-miR-320 modulates several genes associated with blood coagulation pathway and fibrinolytic pathway. Several anti-coagulants as well as clot dissolution genes including endothelial protein C receptor (PROCR), vitamin K-dependent protein C (PROC), vitamin K-dependent protein S (PROS), antithrombin III (SERPINC1), thrombomodulin (THBD), Urokinase plasminogen activator surface receptor (PLAUR) and tissue-type plasminogen activator (PLAT) are regulated by hsa-miR-320. Besides these, pathway analysis also demonstrated that hsa-miR-320 targets coagulation factors such as factor XI (F11), factor XII (F12), factor III (Tissue factor), factor VII (F7), factor X (F10), factor II (prothrombin) etc.
Discussion
MicroRNAs are master regulators that play a pivotal role in several cellular and biochemical pathways and hence their dysregulation has been associated with several human diseases [46, 47]. MiRNAs serve as attractive targets for developing novel therapeutic approaches which primarily involves restoration of normal miRNA function, either by using miRNA mimics or by single-stranded antisense oligonucleotides, known as anti-miRs [48, 49]. Recently, several studies have been conducted to unravel the therapeutic potential of miRNA mimics and antagonists for treatment of venous thrombosis [34, 35], Sun et al. 2019, [50] as well as several other complex diseases such as renal fibrosis [51], epilepsy [52], several types of cancers (Fu et al. 2021) and even COVID-19 [53].
Predisposition to venous thromboembolism, a complex pathological condition is significantly linked to genetic factors. It induces development of thrombosis or embolism in both arteries and veins at multiple sites [54]. Previous studies have shown association of several miRNAs with VTE such as hsa-miR-126-3p, hsa-miR-885-5p, hsa-miR-194-5p, and hsa-miR-192-5p [40, 41]. Over past one decade, there have been several animal model studies which explore modulation of miRNAs for thrombus resolution in VTE. Intravenous injection of viral vector expressing miR-150, miR-126, let-7e-5p, miR-21 and miR-483-3p [55,56,57,58,59] and mimics of miR-145 and miR-150 [34, 35, 38, 39] in rat model of DVT by IVC ligation reportedly result in venous thrombus resolution in experimental DVT rats. Besides these, intravenous injection of viral vector expressing miR-103a-3p [60, 61] and mimics of miR-338-5p [62]in mouse model of DVT by IVC stenosis model have been demonstrated to reduce venous thrombus formation.
Selection of miRNA to be used in in-vivo studies conducted so far, have been done on the basis of either bioinformatic analysis or based on findings of previous studies on miRNA expression profile in DVT. Our research group has previously reported a significant increase in miR-320a levels in plasma of VTE patients in comparison to healthy controls [31,32,33]. In similar studies, significant over expression of miR-320a and miRNA-320b have reported in patients of DVT [43, 44]. Thus, miR-320 was selected to perform further in vivo experiments on rat model of DVT.
MiRNA-320 family comprising of miR-320a, miR-320b, miR-320, miR-320c and miR-320e is closely associated with several human diseases [63]. Previous reports have shown that miR-320 is a tumor suppressor and is significantly down-regulated in many cancers such as cervical cancer, colon cancer, gastric cancer and glioma [64,65,66,67]. These studies demonstrated that miR-320 could be used as diagnostic and prognostic biomarker in diverse range of cancers. In context of venous thrombosis, contradictory reports are available on expression of miR-320. There are evidences of hsa-miR-320 being up-regulated [32, 33, 43, 44] and down-regulated during VTE [68]. Experimental evidences in these reports establish that dysregulation of miR-320 levels are directly associated with VTE susceptibility.
MiRNA mimics and anti-miRs (antagonists) are used for miRNA modulation and thus reverse pathological miRNA expressions for variety of diseases [69]. However, integrity and stability of miRNAs in circulation is a major challenge for miRNA delivery. In the present study, invivofectamine (from Thermo Fischer Scientific) was used as transfection reagent to stabilize the miRNA-320a antagonist into living system. It is animal origin lipid based nanoparticle which facilitates in vivo delivery of miRNAs efficiently. We believe that, after intravenous introduction of miRNA-320a antagonist into rats through tail vein, it binds to mature circulatory miRNA-320 and thus inhibit their interaction with target gene.
The present study revealed therapeutic potential of hsa-miR-320a antagonist in treating venous thrombo-embolism. The findings of this study is a blend of network based bioinformatic tools that were used to identify potential miRNA target together with in vivo animal model, in which the efficacy of target miRNA as therapeutic target was validated. Our study explicitly demonstrated that intravenous administration of hsa-miR-320a antagonist reduces the size of thrombus formed due to coagulation of blood. Also, target prediction and pathway analysis of genes potentially modulated by miR-320, showed that a large number of genes were involved in blood coagulation and fibrinolysis pathway. These included several anti-coagulants and clot dissolution genes which might be down-regulated by over-expression of miR-320 in DVT rats. Interestingly, over-expression of miR-320 has also been associated with increased platelet activity as a result of interaction with WIPF1 gene encoding for WAS/WASL-interacting protein [70]. Thus is expression may increase susceptibility towards VTE. Introduction of hsa-miR-320a antagonist in DVT rats thus inhibit the activity of mature hsa-miR-320, thereby leading to reduction in blood clot (thrombus weight). Notably, pathway analysis revealed that besides targeting genes involved in blood coagulation and fibrinolysis, miR-320 also targets genes related to hypoxic response and endothelial dysfunction. Thus further studies may also be conducted to explore its therapeutic potential in hypoxia induced VTE.
Our results demonstrate that intravenous dose of hsa-miR-320a antagonist did not show any significant signs of toxicity. Significant alterations in injury markers NAGase, Creatinine and NT-proANP, amongst the miRNA antagonist treated animal group compared to others did not cause any lethality in these animals. The marked reduction in the size of the thrombus signifies that intravenous administration of hsa-miR-320a antagonist could be an effective strategy to manage the burden of venous thrombosis. The observations of the study are preliminary in nature and further detailed studies are required with different miRNA doses and duration to validate the current findings.
Conclusion
Several miRNAs have been characterized and validated to regulate physiological processes in development of venous thrombosis. It is important to identify specific miRNA that could mitigate the size of the growing thrombus and thus provide future therapeutic target for pulmonary embolism. In this regard, introduction of hsa-miR-320a antagonist could a novel therapeutic approach for treatment of venous thrombosis.
Limitations of the study
Due to technical reasons, we could perform experiments on limited number of animals.
Data availability
The datasets used and analyzed during the current study available from the corresponding author on reasonable request.
Abbreviations
- BT:
-
Bleeding time
- CT:
-
Clotting time
- DVT:
-
Deep vein thrombosis
- IVC:
-
Inferior vena cava
- PE:
-
Pulmonary embolism
- VT:
-
Venous thrombosis
References
ISTH Steering Committee for World Thrombosis Day (2014) Thrombosis: a major contributor to the global disease burden. J Thromb Haemost 12(10):1580–1590. https://doi.org/10.1111/jth.12698
Naess IA, Christiansen SC, Romundstad P, Cannegieter SC, Rosendaal FR, Hammerstrøm J (2007) Incidence and mortality of venous thrombosis: a population-based study. J Thromb Haemost 5(4):692–699. https://doi.org/10.1111/j.1538-7836.2007.02450.x
Schulman S, Lindmarker P, Holmström M, Lärfars G, Carlsson A, Nicol P, Svensson E, Ljungberg B, Viering S, Nordlander S, Leijd B, Jahed K, Hjorth M, Linder O, Beckman M (2006) Post-thrombotic syndrome, recurrence, and death 10 years after the first episode of venous thromboembolism treated with warfarin for 6 weeks or 6 months. J Thromb Haemost 4(4):734–742. https://doi.org/10.1111/j.1538-7836.2006.01795.x
Diaz JA, Obi A, Myers DD, Wrobleski SK, Henke PK, Mackman N, Wakefield TW (2012) Critical review of mouse models of venous thrombosis. Arterioscler Thromb Vasc Biol 32:556–562
Heit JA, O’Fallon WM, Petterson TM, Lohse CM, Silverstein MD, Mohr DN, Melton LJ (2002) Relative impact of risk factors for deep vein thrombosis and pulmonary embolism: a population-based study. Arch Intern Med 162:1245–1248
Zwicker I et al (2009) Tumor-derived tissue factor-bearing microparticles are associated with venous thromboembolic events in malignancy. Clin Cancer Res 15:6830–6840
Zhou X et al (2010) Incidence and risk factors of venous thromboembolic events in lymphoma. Am J Med 123:935–941
Demers C et al (1998) Incidence of venographically proved deep vein thrombosis after knee arthroscopy. Arch Intern Med 158:47–50
Chan MY, Andreotti F, Becker RC (2008) Hypercoagulable states in cardiovascular disease. Circulation 118:2286–2297
Anand AC, Jha SK, Saha A, Sharma V, Adya CM (2001) Thrombosis as a complication of extended stay at high altitude. Natl Med J India 14(4):197–201
Khalil KF, Saeed W (2010) Pulmonary embolism in soldiers serving at high altitude. J Coll Physicians Surg Pak 20:7
Kumar S (2006) High altitude induced deep venous thrombosis: a study of 28 cases. Indian J Surg 68:84–88
Rao KS (2006) Other medical illnesses aggravated by high altitude. In: Anand AC, Narula AS, Kakkar R, Kalra R (eds) Textbook of environmental emergencies. Department of Internal Medicine Armed Forces Medical College, Pune, pp 26–29
Singh I, Chohan IS (1972) Blood coagulation changes at high altitude predisposing to pulmonary hypertension. Br Heart J 34:611–617
Brill A, Fuchs TA, Chauhan AK et al (2011) von Willebrand factor-mediated platelet adhesion is critical for deep vein thrombosis in mouse models. Blood 117:1400–1407. https://doi.org/10.1182/blood-2010-05-287623
Mammen EF (1992) Pathogenesis of venous thrombosis. Chest. https://doi.org/10.1378/chest.102.6_supplement.640s
Sevitt S (1974) The structure and growth of valve-pocket thrombi in femoral veins. J Clin Pathol 27:517–528. https://doi.org/10.1136/jcp.27.7.517
Brühl MLV, Stark K, Steinhart A et al (2012) Monocytes, neutrophils, and platelets cooperate to initiate and propagate venous thrombosis in mice in vivo. J Exp Med 209:819–835. https://doi.org/10.1084/jem.20112322
Schönfelder T, Jäckel S, Wenzel P (2017) Mouse models of deep vein thrombosis. Gefasschirurgie 22:28–33. https://doi.org/10.1007/s00772-016-0227-6
Bartel DP (2004) MicroRNAs: genomics, biogenesis, mechanism, and function. Cell 116:281–297
Iwakawa HO, Tomari Y (2015) The functions of microRNAs: mRNA decay and translational repression. Trends Cell Biol 25(11):651–665
Zhu W, Qian J, Ma L, Ma P, Yang F, Shu Y (2017) MiR-346 suppresses cell proliferation through SMYD3 dependent approach in hepatocellular carcinoma. Oncotarget 8(39):65218–65229. https://doi.org/10.18632/oncotarget.18060
Bartel DP (2009) MicroRNAs: target recognition and regulatory functions. Cell 136:215–233
Armand-Labit V, Pradines A (2017) Circulating cell-free MicroRNAs as clinical cancer biomarkers. Biomol Concepts 8:61–81
Loosen SH, Schueller F, Trautwein C et al (2017) Role of circulating microRNAs in liver diseases. World J Hepatol 9:586–594
Rayner K, Dimmeler S, Calin GA et al (2014) Novel biomarkers for acute myocardial infarction: is microRNA the new kid on the block? ClinChem 60:812–817
Liu X, Cheng Y, Zhang S, Lin Y, Yang J, Zhang C (2009) A necessary role of miR-221 and miR-222 in vascular smooth muscle cell proliferation and neointimal hyperplasia. Circ Res 104:476–487
Tan M, Yan HB, Li JN et al (2016) Thrombin stimulated platelet-derived exosomes inhibit platelet-derived growth factor receptor-beta expression vascular smooth muscle cells. Cell Physiol Biochem 38:2348–2365
Weber C, Schober A, Zernecke A (2010) Micrornas in arterial remodelling, inflammation and atherosclerosis. Curr Drug Targets 11:950–956
Hembrom AA, Srivastava S, Garg I, Kumar B (2020) MicroRNAs in venous thrombo-embolism. Clin Chim Acta 504:66–72. https://doi.org/10.1016/j.cca.2020.01.034
Hembrom AA, Ghosh N, Kumar V, Garg I, Ganju L, Srivastava S (2022) Panel of regulatory miRNAs for blood coagulation under normoxic and hypoxic conditions. Def Life Sci J 7(1):17–26
Srivastava S, Garg I, Kumari B, Rai C, Singh Y, Kumar V, Yanamandra U, Singh J, Bansal A, Kumar B (2019) Diagnostic potential of circulating micro RNA hsa-miR-320 in patients of high altitude induced deep vein thrombosis: an Indian study. Gene Rep. 17:100550
Srivastava S, Garg I, Kumar B (2019) An In-Silico argument for Micro-RNAs showing pivotal role in susceptibility towards high altitude induced venous thrombo-embolism (HA-VTE). Int J Gen Sci 6(1):1–11
Sahu A, Jha PK, Prabhakar A, Singh HD, Gupta N, Chatterjee T, Tyagi T, Sharma S, Kumari B, Singh S, Nair V, Goel S, Ashraf MZ (2017) MicroRNA-145 impedes thrombus formation via targeting tissue factor in venous thrombosis. EBioMedicine 26:175–186
Sahu A, Jha PK, Prabhakar A, Singh HD, Gupta N, Chatterjee T, Tyagi T, Sharma S, Kumari B, Singh S et al (2017) MicroRNA-145 impedes thrombus formation via targeting tissue factor in venous thrombosis. EBioMedicine 26:175–186
Tyagi T, Ahmad S, Gupta N, Sahu A, Ahmad Y, Nair V, Chatterjee T, Bajaj N, Sengupta S, Ganju L, Singh SB, Ashraf MZ (2013) Altered expression of platelet proteins and calpain activity mediate hypoxia-induced prothrombotic phenotype. Blood. https://doi.org/10.1182/blood-2013-05-501924
Gupta N, Sahu A, Prabhakar A, Chatterjee T, Tyagi T, Kumari B, Khan N, Nair V, Bajaj N, Sharma M, Ashraf MZ (2017) Activation of NLRP3 inflammasome complex potentiates venous thrombosis in response to hypoxia. Proc Natl Acad Sci U S A 114(18):4763–4768. https://doi.org/10.1073/pnas.1620458114
Wang W, Zhu X, Du X, Xu A, Yuan X, Zhan Y, Liu M, Wang S (2019) MiR-150 promotes angiogensis and proliferation of endothelial progenitor cells in deep venous thrombosis by targeting SRCIN1. Microvasc Res 123:35–41
Wang X, Sundquist K, Svensson PJ et al (2019) Association of recurrent venous thromboembolism and circulating microRNAs. Clin Epigenet 11:28
Rodriguez-Rius A, Lopez S, Martinez-Perez A, Souto JC, Soria JM (2020) Identification of a plasma MicroRNA Profile associated with venous thrombosis. Arterioscler, Thromb, Vasc Biol 40:1392–1399
Rodriguez-Rius A, Lopez S, Martinez-Perez A, Souto JC, Soria JM (2020) Identification of a plasma MicroRNA profile associated with venous thrombosis. Arterioscler Thromb Vasc Biol 40(5):1392–1399. https://doi.org/10.1161/ATVBAHA.120.314092
Mussbacher M, Krammer TL, Heber S et al (2020) Impact of anticoagulation and sample processing on the quantification of human blood-derived microRNA signatures. Cells 9(8):E1915. https://doi.org/10.3390/cells9081915
Jiang Z, Ma J, Wang Q, Wu F, Ping J, Ming L (2018) Combination of circulating miRNA-320a/b and D-dimer improves diagnostic accuracy in deep vein thrombosis patients. Med Sci Monit 6(24):2031–2037
Starikova I, Jamaly S, Sorrentino A, Blondal T, Latysheva N, Sovershaev M, Hansen JB (2015) Differential expression of plasma miRNAs in patients with unprovoked venous thromboembolism and healthy control individuals. Thromb Res 136(3):566–572
Thomas PD, Ebert D, Muruganujan A, Mushayahama T, Albou L-P, Mi H (2022) PANTHER: making genome-scale phylogenetics accessible to all. Protein Soc 31(1):8–22. https://doi.org/10.1002/pro.421
Kloosterman WP, Plasterk RH (2006) The diverse functions of microRNAs in animal development and disease. Dev Cell 11:441–450. https://doi.org/10.1016/j.devcel.2006.09.009
Paul P, Chakraborty A, Sarkar D, Langthasa M, Rahman M, Bari M, Singha RS, Malakar AK, Chakraborty S (2018) Interplay between miRNAs and human diseases. J Cell Physiol 233:2007–2018. https://doi.org/10.1002/jcp.25854
Rupaimoole R, Slack FJ (2017) MicroRNA therapeutics: towards a new era for the management of cancer and other diseases. Nat Rev Drug Discov 16:203–222. https://doi.org/10.1038/nrd.2016.246
Van Rooij E, Kauppinen S (2014) Development of microRNA therapeutics is coming of age. EMBO Mol Med 6:851–864. https://doi.org/10.15252/emmm.201100899
Morelli VM, Brækkan SK, Hansen JB (2020) Role of microRNAs in venous thromboembolism. Int J Mol Sci 21(7):2602
Denby L, Ramdas V, Lu R, Conway BR, Grant JS, Dickinson B, Aurora AB, McClure JD, Kipgen D, Delles C, van Rooij E, Baker AH (2014) MicroRNA-214 antagonism protects against renal fibrosis. J Am Soc Nephrol 25(1):65–80
Zhang H, Qu Y, Wang A (2018) Antagonist targeting microRNA-146a protects against lithium-pilocarpine-induced status epilepticus in rats by nuclear factor-κB pathway. Mol Med Rep 17:5356–5361
Hum C, Loiselle J, Ahmed N, Shaw TA, Toudic C, Pezacki JP (2021) MicroRNA mimics or inhibitors as antiviral therapeutic approaches against COVID-19. Drugs 81(5):517–531
Sun L, Li X, Li Q, Wang L, Li J, Shu C (2021) Multiple arterial and venous thromboembolism in a male patient with hereditary protein C deficiency. Medicine (Baltimore) 100(15):e25575. https://doi.org/10.1097/MD.0000000000025575
Du X, Hong L, Sun L, Sang H, Qian A, Li W, Zhuang H, Liang H, Song D, Li C et al (2019) miR-21 induces endothelial progenitor cells proliferation and angiogenesis via targeting FASLG and is a potential prognostic marker in deep venous thrombosis. J Transl Med 17:270
Kong L, Du X, Hu N, Li W, Wang W, Wei S, Zhuang H, Li X, Li C (2016) Downregulation of let-7e-5p contributes to endothelial progenitor cell dysfunction in deep vein thrombosis via targeting FASLG. Thromb Res 138:30–36
Kong L, Hu N, Du X, Wang W, Chen H, Li W, Wei S, Zhuang H, Li X, Li C (2016) Upregulation of miR-483-3p contributes to endothelial progenitor cells dysfunction in deep vein thrombosis patients via SRF. J Transl Med 14:23
Meng Q, Wang W, Yu X, Li W, Kong L, Qian A, Li C, Li X (2015) Upregulation of MicroRNA-126 contributes to endothelial progenitor cell function in deep vein thrombosis via its target PIK3R2. J Cell Biochem 116:1613–1623. https://doi.org/10.1002/jcb.25115
Wang W, Li C, Li W, Kong L, Qian A, Hu N, Meng Q, Li X (2014) MiR-150 enhances the motility of EPCs in vitro and promotes EPCs homing and thrombus resolving in vivo. Thromb Res 133:590–598
Sun S, Chai S, Zhang F, Lu L (2020) Overexpressed microRNA-103a-3p inhibits acute lower-extremity deep venous thrombosis via inhibition of CXCL12. IUBMB Life 72(3):492–504. https://doi.org/10.1002/iub.2168
Sun S, Chai S, Zhang F, Lu L (2020) Overexpressed microRNA-103a-3p inhibits acute lower-extremity deep venous thrombosis via inhibition of CXCL12. IUBMB Life 72:492–504. https://doi.org/10.1002/iub.2168
Zhang Y, Zhang Z, Wei R, Miao X, Sun S, Liang G, Chu C, Zhao L, Zhu X, Guo Q et al (2020) IL (Interleukin)-6 contributes to deep vein thrombosis and is negatively regulated by miR-338-5p. Arterioscler Thromb Vasc Biol 40:323–334
McCreight J, Schneider S, Wilburn D, Swanson W (2017) Evolution of microRNA in primates. PLoS ONE 12:e0176596. https://doi.org/10.1371/journal.pone.0176596
Chen X, Gao S, Zhao Z, Liang G, Kong J, Feng X (2020) MicroRNA-320d regulates tumor growth and invasion by promoting FoxM1 and predicts poor outcome in gastric cardiac adenocarcinoma. Cell Biosci 10:80. https://doi.org/10.1186/s13578-020-00439-7
Fang Z, Tang J, Bai Y, Lin H, You H, Jin H, Lin L, You P, Li J, Dai Z et al (2015) Plasma levels of microRNA-24, microRNA-320a, and microRNA-423-5p are potential biomarkers for colorectal carcinoma. J Exp Clin Cancer Res 34:86. https://doi.org/10.1186/s13046-015-0198-6
Hong H, Zhu H, Zhao S, Wang K, Zhang N, Tian Y, Li Y, Wang Y, Lv X, Wei T et al (2019) The novel circCLK3/miR-320a/FoxM1 axis promotes cervical cancer progression. Cell Death Dis 10:950. https://doi.org/10.1038/s41419-019-2183-z
Lv Q, Du H, Liu Y, Huang Y, Wang G, Zhang X, Chen S, Zhou H (2017) Low expression of microRNA-320b correlates with tumorigenesis and unfavorable prognosis in glioma. Oncol Rep 38:959–966. https://doi.org/10.3892/or.2017.5762
Thibord F, Munsch G, Perret C, Suchon P, Roux M, Ibrahim-Kosta M, Goumidi L, Deleuze JF, Morange PE, Trégouët DA (2020) Bayesian network analysis of plasma microRNA sequencing data in patients with venous thrombosis. Eur Heart J Suppl 22(Suppl C):C34–C45
Diener C, Keller A, Meese E (2022) Emerging concepts of miRNA therapeutics: from cells to clinic. Trends Genet 38(6):613–626
Nagalla S, Shaw C, Kong X et al (2011) Platelet microRNA-mRNA coexpression profiles correlate with platelet reactivity. Blood 117(19):5189–5197. https://doi.org/10.1182/blood-2010-09-299719
Acknowledgements
The authors are extremely thankful to Animal house of DIPAS for providing healthy animals for the study. Authors also acknowledge efforts and cooperation of technical staff and research scholars during the experiments.
Funding
Defence Institute of Physiology and Allied Sciences (DIPAS), Defence Research and Development Organization (DRDO), S&T(A)/22-23/DIP-276.
Author information
Authors and Affiliations
Contributions
SS: experiment design, analysis and manuscript writing; IG and NG: experimental work and analysis; RV: review and editing of manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The manuscript has been read and approved for submission by all authors. No potential conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Srivastava, S., Garg, I., Ghosh, N. et al. Therapeutic implication of MicroRNA-320a antagonist in attenuating blood clots formed during venous thrombosis. J Thromb Thrombolysis 57, 699–709 (2024). https://doi.org/10.1007/s11239-024-02947-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11239-024-02947-6