Abstract
This study aim to investigate if remote intensive coaching for the first 6 months post-AMI will improve adherence to the twice-a-day antiplatelet medication, ticagrelor. Between July 8, 2015, to March 29, 2019, AMI patients were randomly assigned to remote intensive management (RIM) or standard care (SC). RIM participants underwent 6 months of weekly then two-weekly consultations to review medication side effects and medication adherence coaching by a centralized nurse practitioner team, whereas SC participants received usual cardiologist face-to-face consultations. Adherence to ticagrelor were determined using pill counting and serial platelet reactivity measurements for 12 months. A total of 149 (49.5%) of participants were randomized to RIM and 152 (50.5%) to SC. Adherence to ticagrelor was similar between RIM and SC group at 1 month (94.4 ± 0.7% vs. 93.6±14.7%, p = 0.537), 6 months (91.0±14.6% vs. 90.6±14.8%, p = 0.832) and 12 months (87.4±17.0% vs. 89.8±12.5%, p = 0.688). There was also no significant difference in platelet reactivity between the RIM and SC groups at 1 month (251AU*min [212–328] vs. 267AU*min [208–351], p = 0.399), 6 months (239AU*min [165–308] vs. 235AU*min [171–346], p = 0.610) and 12 months (249AU*min [177–432] vs. 259AU*min [182–360], p = 0.678). Sensitivity analysis did not demonstrate any association of ticagrelor adherence with bleeding events and major adverse cardiovascular events. RIM, comprising 6 months of intensive coaching by nurse practitioners, did not improve adherence to the twice-a-day medication ticagrelor compared with SC among patients with AMI. A gradual decline in ticagrelor adherence over 12 months was observed despite 6 months of intensive coaching.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute myocardial infarction (AMI) is a major cause of mortality and morbidity worldwide [1]. Dual antiplatelet therapy (DAPT) has been the cornerstone of treatment for patients with AMI. Data from previous randomized controlled trials demonstrated that treatment with ticagrelor-based DAPT in acute coronary syndrome reduced the occurrence of major adverse cardiovascular events (MACE) as compared to clopidogrel or placebo [2, 3]. Ticagrelor exerts its antiplatelet activity by reversibly binding to the P2Y12 receptor and results in a non-competitive inhibition of the adenosine diphosphate-induced signalling pathway [4]. The reversible binding property of ticagrelor and plasma half-life of 7-8.5-hour mandate twice daily dosing, which may reduce adherence rate as compared to other P2Y12 inhibitors with once daily dosing [5, 6] Despite the remarkable success of therapeutic interventions and secondary prevention during the post-MI period, non-adherence to medication is a common problem and is associated with increased future ischemic events [7,8,9].
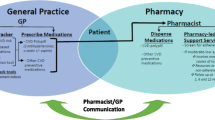
Telemedicine is an important advance in modern medicine that allow for the exchange of health information remotely using electronic means of communication. In patients with chronic disease such as diabetes and hypertension, better medication adherence was seen in those who were on telemedicine as compared to those who were on conventional face-to-face consultation [10]. In this study, we aim to evaluate the impact of post-discharge, telehealth-enabled, nurse-led remote intensive management (RIM) on adherence to ticagrelor with pill counting and platelet reactivity measurements as the outcomes in a population of high-risk MI patients who successfully underwent percutaneous coronary intervention (PCI).
Methods
Study design
The IMMACULATE randomized trial was a prospective, multicentre randomized controlled trial conducted at 3 tertiary cardiac hospitals in Singapore to compare 6-month RIM compared with standard care (SC) among patients discharged with revascularized AMI (https://clinicaltrials.gov/ct2/show/NCT02468349). From July 8, 2015, to March 29, 2019, 301 eligible participants were randomized 1:1 to RIM or SC using block randomization as previously described [11]. The primary IMMACULATE study was designed to compare the outcomes of ventricular remodeling and hemodynamic stress among patients with AMI and elevated N-terminal pro–b type natriuretic peptide (NT-pro-BNP) receiving RIM versus SC. In this study, there were no significant differences in safety events (a composite of hypotension, bradycardia, hyperkalemia, or acute kidney injury requiring hospitalization), or left ventricular reverse remodeling outcomes [6 months indexed left ventricular end systolic volume (LVESV) adjusted for baseline LVESV] in patients treated for 6 months after discharged by a centralized nurse practitioner -led telehealth program compared with standard in-person care by a cardiologist. This present study was a sub study of the IMMACULATE trial, designed to assess the efficacy of telemedicine-based coaching program in improving adherence to antiplatelet therapy. We hypothesize that RIM will improve adherence to ticagrelor leading to superior platelet reactivity outcomes, as compared with SC. This secondary analysis was pre-specific in the original trial protocol prior to the start of recruitment. The study was performed in accordance with ethical principles that have their origin in the Declaration of Helsinki and are consistent with Good Clinical Practice. Informed consents were signed and obtained from all participants. The National Healthcare Group Domain Specific Review Board approved the study for all 3 hospitals (National University Heart Centre, National Heart Centre, and Tan Tock Seng Hospital in Singapore).
Patient population
Individuals who were admitted for AMI were considered eligible if they had (i) ST elevation myocardial infarction or non-ST elevation myocardial infarction within the last 7 days, (ii) predischarge whole-blood NT-pro-BNP concentration more than 300pg/mL, (iii) undergone PCI for the index event, (iv) age ≥ 21 years and ≤ 85 years. Patients with hypersensitivity to ticagrelor, high bleeding risk, active malignancy, severe liver or renal impairment, psychosocial barrier to telemedicine adoption, and patients who declined consent were excluded from the trial. Patients who needed combination of antiplatelet and anticoagulation therapy after enrolment due to left ventricular thrombus or atrial fibrillation were excluded from the ticagrelor sub study. Information on demographics, co-morbidities, history of coronary revascularization, clinical presentation, inpatient laboratory values, left ventricular ejection fraction (LVEF) and pharmacotherapy on discharge were prospectively collected by trained study coordinators according to a standardized case report form.
Intervention
All participants received DAPT with (i) aspirin 300 mg loading dose followed by 100 mg daily and (ii) ticagrelor 180 mg loading dose followed by 90 mg twice a day. Ticagrelor was provided free-of-charge for 12 months to all study participants. If they were on another P2Y12 antagonist, the preceding P2Y12 antagonist were stopped, and they were started on ticagrelor. Participants randomized to the RIM arm were scheduled to have weekly consultations via telephone for the first 2 months and fortnightly consultation for the subsequent 4 months. During these consultations, trained nurse practitioners provided medication adherence coaching and monitoring trial participants for bleeding and other adverse events, according to a standardized algorithm. Participants randomized to SC received regular face-to-face consultations with their cardiologists as per usual practice.
Adherence measures
Ticagrelor pill count
Adherence to ticagrelor was measured using pill counting method at 1 month, 6 months and 12 months. Study participants were instructed to return all used and unused ticagrelor medication blister during every study visit. Thereafter, a new batch of ticagrelor will be dispensed to them until the next study visit. Adherence rate was calculated as the percentage of the number of prescribed pills corrected for the number of returned pills divided by the period (in days) multiplied by 100%. Following previous studies, participants were considered having good adherence to ticagrelor if their adherence rate was ≥ 80% [12], [13].
Platelet reactivity testing
Platelet activity was measured by longitudinal profiles of adenosine diphosphate-induced impedance aggregometry (Multiplate®- multiple platelet function analyser; Roche Diagnostics AG) at 1 week, 1 month, 6 months and 12 months. Results were expressed as arbitrary Aggregation Units (AU) and plotted against time, defining platelet function as the area under curve (AUC or AU*min). High platelet reactivity was considered for test value > 468 AU*min (46 AU), linking this cut off value to occurrence of stent thrombosis after PCI [14, 15].
Safety outcomes
The primary safety event was cumulative bleeding events at 12 months according to the BARC (Bleeding Academic Research Consortium) definitions [16]. Major bleeding was defined as BARC ≥ 3b. Having early bleeding event may have been a result of earlier prasugrel or clopidogrel use before switching to ticagrelor, or anti-thrombotics use such as unfractionated heparin or glycoprotein IIb/IIIa during primary angioplasty. As such, we added another analysis of cumulative bleeding events that excluded bleeding events that occurred within the first 7 days.
Clinical outcomes
The primary clinical outcome was MACE, defined as a composite outcome of recurrent MI, repeat revascularization, or all-cause mortality. The diagnosis of MI was based on the Third Universal Definition of MI [17]. Repeat revascularization included any type of percutaneous of surgical revascularization on any vessels. Clinical outcomes were tracked at 1 month, 6 months, 12 months, and 24 months.
Statistical analysis
The baseline sample characteristics were presented in mean±standard deviations or frequency (%), and exploratory analyses between RIM and SC were performed with Mann-Whitney test and Chi-square test. Clinical outcomes were compared using Chi Square test, Fisher Exact test and Mann-Whitney test. Analyses was done based on intention-to-treat (ITT) method. The sensitivity analysis concerning ticagrelor adherence, BARC ≥ 2 bleeding at 12 months and MACE at 24 months were performed with generalized structural equation model (gSEM) in view of the multi-level data structures, inter-correlations among predictors and multiple outcomes of mixed types. This was essentially a network of three equations with shared predictors for different but related outcomes, thus allowing direct and indirect effects of the predictors be ascertained. Ticagrelor adherence, bleeding at 12 months and MACE at 24 months were analyzed with an underlying Binomial distribution and Beta distribution with a logit link. The final model was chosen based on interpretability and relevance to the research questions. Analyzed with Stata MP V16 (Stata Corporations, Texas, USA), all statistical tests were conducted at 5% level of significance.
Results
Baseline characteristics
A total of 301 participants were recruited from July 8, 2015, to March 29, 2019, and randomized to either RIM (n = 149 [49.5%]; mean [SD] age, 55.8 [8.5] years) or SC (n = 152 [50.5%; mean [SD] age, 54.7 [9.1] years). There was no crossover of trial subjects. Only participants who were on ticagrelor (268 out of 301 participants) were included in the IMMACULATE Ticagrelor Adherence sub study. (Fig. 1) Baseline characteristics were balanced between both groups with 285 (94.7%) male participants, 249 (82.7%) were married, 12 (4.0%) who live alone and 217 (72.1%) with secondary school education or higher. Majority of participants presented with ST elevation myocardial infarction (STEMI, 86.7%) and received guideline directed medical therapy on discharge (DAPT 100%, beta blocker 86.0%, statin 99.0% and ACE-I/ARB 76.7%). Heamoglobin level was 15.1g/dL in the RIM group and 14.6g/dL in the standard care group (p<0.001). There were 32.9% in the RIM group and 30.3% in the control group who switched from prasugrel or clopidogrel to ticagrelor (p = 0.622). (See Table 1).
Ticagrelor pill count data were available for 130 participants in the RIM group and 138 participants in the SC group. (Fig. 1) Adherence rate to ticagrelor was similar between RIM and SC group 1 month (94.4 ± 0.7% vs. 93.6 ± 14.7%, p = 0.537), 6 months (91.0 ±14.6% vs. 90.6 ± 14.8%, p = 0.832) and 12 months (87.4 ± 17.0% vs. 89.8 ±12.5%, p = 0.688). (Table 2) Proportion of participants with good ticagrelor adherence rate ≥ 80% was also similar between both groups at 1 month (91.5% vs. 93.7%, p = 0.508), 6 months (84.3% vs. 86.3%, p = 0.648) and 12 months (80.0% vs. 84.7%, p = 0.348). Over time, a gradual decline in adherence was observed in the overall study participants (94.0 ± 12.8% at 1 month, 90.8 ± 14.7% at 6 months and 88.5 ± 15.1% at 12 months). At 1 month, 92.6% had high ticagrelor adherence rate of ≥ 80% as compared to only 82.2% at 12 months follow up.
Next, there was also no significant difference in platelet reactivity between the RIM and SC groups at 1 week (285AU*min [222–368] vs. 281AU*min [229–381], p = 0.669), 1 months (25 AU*min [212–328] vs. 267AU*min [208–351], p = 0.399), 6 months (239AU*min [165–308] vs. 235AU*min [171–346], p = 0.610) and 12 months (249AU*min [177–432] vs. 259AU*min [182–360], p = 0.678) (Table 2). Similarly, there was no significant difference in the proportion of participants with high platelet reactivity between RIM and SC group at 1 week (12.9% vs. 14.7%, p = 0.656) 1 month (11.1% vs. 10.5%, p = 0.861), 6 months (6.7% vs. 6.9%, p = 0.947) and 12 months (22.5% vs. 14.1%, p = 0.086), although numerically there were more participants with high platelet reactivity in the RIM group. Overall, the number of participants with high platelet reactivity was found to be lowest at 6 months (6.8%) and highest at 12 months (18.4%).
Cumulative bleeding events at 12 months were reported in 44 (33.3%) in the RIM group and 46 (36.2%) in the SC group, with no significant difference detected between the two groups (p = 0.626). (Table 3) Of these events, only 4 patients in the RIM group and 5 patients in the SC group were ≥ BARC 2 bleeding. Between 8 days to 12 months, there was no statistical difference in the bleeding events between RIM (23.5%) and SC group (23.7%, p = 0.695). The cumulative clinical outcomes of MACE and the individual components of all-cause death, MI and revascularization were also similar between the RIM and SC group at 1 month, 6 months, 12 months and 24 months follow up. A total of 2 patients died during follow up (RIM: 1; SC: 1, p = 0.973), and this occurred between 12-24 months of follow up. (Table 3)
The sensitivity analysis did not demonstrate any association between ticagrelor adherence with bleeding events and major adverse cardiovascular events. (Table 4). The analysis concerning ticagrelor adherence was conducted with demographics (age, sex, gender, ethnicity, and marital status) and STEMI included as adjusting covariates.
Discussion
The IMMACULATE ticagrelor sub study is, to our knowledge, the first randomized controlled trial designed to determine the effectiveness of six months of intensive remote coaching by nurse practitioners in improving ticagrelor adherence among patients discharged with high-risk AMI. Our findings showed adherence to ticagrelor post-MI did not improve with post-discharge, telehealth-enabled, nurse-led RIM as compared to SC. However, we did show a gradual declined in adherence rate over time in the overall study population. Further sensitivity analysis, there were no significant impact of ticagrelor adherence on platelet reactivity, bleeding events and MACE.
To date, interventions to improve adherence to cardiovascular medications have yielded modest effect sizes. Ho et al. randomized patients with acute coronary syndrome to pharmacist-led medication reconciliation and tailoring, patient education, collaborative care between pharmacist and physician and voice messaging refill reminders versus usual care. These multifaceted interventions resulted in better adherence to clopidogrel, statin and ACEI/ARB although it did not translate into better blood pressure and LDL-cholesterol level control [12]. On the other hand, monthly personalized educational reminders in the DERLA-STEMI and weekly motivational and supportive text messages TEXTMEDS trial did not improve adherence to cardiovascular drugs after acute coronary syndrome [18, 19]. Another patient focused enhanced in-hospital counselling with attention to adherence barriers, communication of discharge medication to community pharmacist and physician as well as ongoing assessment of adherence by community pharmacist also failed to increase medication adherence in the intervention arm [19, 20].
While we cannot be certain about why 6 months of remote intensive coaching failed to improve adherence ticagrelor in this trial, we would like to put for several potential explanations its neutral result. First, this is a cohort of trial participants who were young (mean age 55.0 ± 8.8 years) with good social support and education background (82.7% were married and 72.1% obtained secondary school education or higher). Second, there are already routine comprehensive pre-discharge education by speciality nurses and post discharge cardiac rehabilitation programme in place for post-MI patients in the local hospitals that may influence the behaviour of medication taking in participants of both treatment arm. Third, it would be reasonable to assume that the patients who agreed to be enrolled in clinical trials are highly motivated individuals. Fourth, participants in clinical trials commonly practise better behaviour and adherence due to the presence of Hawthorne effect, or the awareness of being studied [21]. In fact, like our study, the PLATO trial (Study of Platelet Inhibition and Patient Outcomes) reported a relatively high adherence rate of 82.8% to study drugs in their trial subjects [3]. Fifth, secondary analysis can be inadequately powered to detect significant differences in results for several reasons. The original study may not have included enough participants to provide sufficient statistical power for the secondary analysis. Additionally, certain relevant variables may be missing, poorly measured, or not granular enough, limiting the ability to detect significant differences. Finally, participants in the RIM group only received intensive remote consultation for 6 months. This intervention period may be too short to effect any significant change in behaviour towards medication adherence for the longer term.
A couple of findings in our study require elaboration. Regardless of treatment arm, we noticed a gradual decline in ticagrelor adherence rate over time. This is despite all participants receiving ticagrelor directly from the study team and at no cost to the participant, which eliminate potential logistic and cost issue as reasons for non-adherence. Medication non-adherence is a common and undertreated problem in the healthcare setting [22, 23]. Besides twice daily dosing that can reduce adherence, patient who are on ticagrelor has higher risk of discontinuation due to higher cost and adverse events such as dyspnoea and bleeding as compared to clopidogrel or aspirin [24, 25]. After AMI, DAPT is generally recommended for at least 12 months unless there is excessive bleeding risk [26, 27]. However, reported adherence to antiplatelet therapy post-MI were at most moderate and tend to worsen over time [7, 28, 29]. A study by Latry et al. found at discontinuation of DAPT for at least 1 month was 18.6% during the first 3 months and 49.1% at 12 months after PCI for MI [30]. In another study, only 54.3% of patients had good adherence to clopidogrel at 12 months post-MI [13]. The barriers to medication adherence are a complex interplay of patient, healthcare providers, treatment, and healthcare system related factors. Telemedicine may address certain patient related factors, such as motivation, beliefs, perceptions about the need for medication, forgetfulness, and health literacy during the intervention period, but there are also other barriers to medication adherence like such as side effects, cost and system issues that cannot be addressed by telemedicine and may cause adherence to deteriorate over time [31].
This study highlights the difficulties in managing medication non-adherence and the need for an innovative solution that is easily replicated, cost effective and sustainable in the long run. Interventions to improve medication adherence were often complex and require a combination of education, counselling, repeated reminders, and supervisions, with at most modest effects and are difficult to sustain long-term. With the emergence of COVID-19 pandemic recently and the increased need for social distancing, telemedicine present as an alternative to face to face contact when ‘high-touch’ management such as patient coaching is needed. Patients should also be an active participant in this process and work together with their healthcare providers to improve medication adherence. Patients who are unable to adhere to ticagrelor due to side effects or cost should be identified early and offered help such as financial assistance or consider switching to clopidogrel.
Limitation
This study has several limitations. First, the results are only applicable to the type of intervention that we used in this study and cannot be generalized to other types of telemedicine design. Second, adherence rate by pill counting can potentially be inaccurate, as patients may not bring all their remaining medication and may discard pills before study visits (“pill dumping”) [22]. For this reason, a complementary indicator using direct measure method such as platelet reactivity test to detect biological marker administered with the drug can be used. Platelet reactivity can be widely variable in clopidogrel, but ticagrelor exert a more uniformed platelet response, making it a reasonable test to measure drug activity in this study [32]. It is noteworthy that direct measure may also introduce bias if participants only take the medication nearer to their study visits and were still able to demonstrate platelet inhibition. Besides that, platelet reactivity can be affected by age, body mass index and smoking status during ticagrelor maintenance therapy [33]. Medication events monitoring system may be the gold standard in measuring adherence, but these equipment are expensive and we are unable to employ it in ticagrelor that comes in blister packs rather than drug containers. Third, we did not record the reason for non-adherence for individual participants, thus limiting the findings. Finally, we did not study the adherence of other cardiovascular medications that were prescribed along with ticagrelor for post-MI.
Conclusion
In this randomized trial comparing six months of remote intensive coaching versus SC, we observed no significant difference in adherence to ticagrelor between treatment groups. Ticagrelor adherence declined significantly over 12 months despite an initial 6 months of intensive coaching. Medication non-adherence remains an unmet clinical need for innovative solutions that are easily replicated, cost effective and sustainable in the long run.
References
Roth GA, Johnson C, Abajobir A, Abd-Allah F, Abera SF, Abyu G et al (2017) Global, Regional, and National Burden of Cardiovascular Diseases for 10 causes, 1990 to 2015. J Am Coll Cardiol 70(1):1–25
Bonaca MP, Braunwald E, Sabatine MS (2015) Long-term use of Ticagrelor in patients with prior Myocardial Infarction. N Engl J Med 373(13):1274–1275
Wallentin L, Becker RC, Budaj A, Cannon CP, Emanuelsson H, Held C et al (2009) Ticagrelor versus clopidogrel in patients with acute coronary syndromes. N Engl J Med 361(11):1045–1057
Van Giezen JJJ, Nilsson L, Berntsson P, Wissing B-M, Giordanetto F, Tomlinson W et al (2009) Ticagrelor binds to human P2Y12 independently from ADP but antagonizes ADP-induced receptor signaling and platelet aggregation. J Thromb Haemost 7(9):1556–1565
Bae JP, Dobesh PP, Klepser DG, Anderson JD, Zagar AJ, McCollam PL et al (2012) Adherence and dosing frequency of common medications for cardiovascular patients. Am J Manag Care 18(3):139–146
Saini SD, Schoenfeld P, Kaulback K, Dubinsky MC (2009) Effect of medication dosing frequency on adherence in chronic Diseases. Am J Manag Care 15(6):e22–33
Huber CA, Meyer MR, Steffel J, Blozik E, Reich O, Rosemann T (2019) Post-myocardial infarction (MI) care: Medication Adherence for secondary Prevention after MI in a large real-world Population. Clin Ther 41(1):107–117
Mehran R, Baber U, Steg PG, Ariti C, Weisz G, Witzenbichler B et al (2013) Cessation of dual antiplatelet treatment and cardiac events after percutaneous coronary intervention (PARIS): 2 year results from a prospective observational study. Lancet 382(9906):1714–1722
Rasmussen JN, Chong A, Alter DA (2007) Relationship between adherence to evidence-based pharmacotherapy and long-term mortality after acute Myocardial Infarction. JAMA 297(2):177–186
Bingham JM, Black M, Anderson EJ, Li Y, Toselli N, Fox S et al (2021) Impact of Telehealth interventions on Medication Adherence for patients with type 2 Diabetes, Hypertension, and/or dyslipidemia: a systematic review. Ann Pharmacother 55(5):637–649
Chan MY, Koh KWL, Poh S-C, Marchesseau S, Singh D, Han Y et al (2021) Remote Postdischarge treatment of patients with Acute Myocardial Infarction by Allied Health Care Practitioners vs Standard Care: the IMMACULATE Randomized Clinical Trial. JAMA Cardiol 6(7):830–835
Ho PM, Lambert-Kerzner A, Carey EP, Fahdi IE, Bryson CL, Melnyk SD et al (2014) Multifaceted intervention to improve medication adherence and secondary prevention measures after acute coronary syndrome hospital discharge: a randomized clinical trial. JAMA Intern Med 174(2):186–193
Kubica A, Kasprzak M, Obonska K, Fabiszak T, Laskowska E, Navarese EP et al (2015) Discrepancies in assessment of adherence to antiplatelet treatment after Myocardial Infarction. Pharmacology 95(1–2):50–58
Sibbing D, Braun S, Morath T, Mehilli J, Vogt W, Schömig A et al (2009) Platelet reactivity after clopidogrel treatment assessed with point-of-care analysis and early drug-eluting stent Thrombosis. J Am Coll Cardiol 53(10):849–856
Bonello L, Tantry US, Marcucci R, Blindt R, Angiolillo DJ, Becker R et al (2010) Consensus and future directions on the definition of high on-treatment platelet reactivity to adenosine diphosphate. J Am Coll Cardiol 56(12):919–933
Ndrepepa G, Schuster T, Hadamitzky M, Byrne RA, Mehilli J, Neumann FJ et al (2012) Validation of the Bleeding Academic Research Consortium definition of bleeding in patients with coronary artery Disease undergoing percutaneous coronary intervention. Circulation 125(11):1424–1431
Thygesen K, Alpert JS, Jaffe AS, Simoons ML, Chaitman BR, White HD et al (2012) Third universal definition of Myocardial Infarction. J Am Coll Cardiol 60(16):1581–1598
Chow CK, Klimis H, Thiagalingam A, Redfern J, Hillis GS, Brieger D et al (2022) Text messages to improve Medication Adherence and secondary Prevention after Acute Coronary Syndrome: the TEXTMEDS Randomized Clinical Trial. Circulation 145(19):1443–1455
Schwalm JD, Ivers NM, Natarajan MK, Taljaard M, Rao-Melacini P, Witteman HO et al (2015) Cluster randomized controlled trial of delayed Educational Reminders for Long-Term Medication Adherence in ST-Elevation Myocardial Infarction (DERLA-STEMI). Am Heart J 170(5):903–913
Calvert SB, Kramer JM, Anstrom KJ, Kaltenbach LA, Stafford JA, Allen LaPointe NM (2012) Patient-focused intervention to improve long-term adherence to evidence-based medications: a randomized trial. Am Heart J 163(4):657–665 e1
Parsons HM (1974) What happened at Hawthorne? New evidence suggests the Hawthorne effect resulted from operant reinforcement contingencies. Science 183(4128):922–932
Osterberg L, Blaschke T (2005) Adherence to medication. N Engl J Med 353(5):487–497
Marcum ZA, Sevick MA, Handler SM (2013) Medication nonadherence: a diagnosable and treatable medical condition. JAMA 309(20):2105–2106
Arora S, Shemisa K, Vaduganathan M, Qamar A, Gupta A, Garg SK et al (2019) Premature Ticagrelor discontinuation in Secondary Prevention of Atherosclerotic CVD: JACC Review topic of the Week. J Am Coll Cardiol 73(19):2454–2464
Bonaca MP, Bhatt DL, Oude Ophuis T, Steg PG, Storey R, Cohen M et al (2016) Long-term tolerability of Ticagrelor for the Secondary Prevention of Major Adverse Cardiovascular Events: a secondary analysis of the PEGASUS-TIMI 54 Trial. JAMA Cardiol 1(4):425–432
Lawton JS, Tamis-Holland JE, Bangalore S, Bates ER, Beckie TM, Bischoff JM et al (2022) 2021 ACC/AHA/SCAI Guideline for Coronary Artery revascularization: executive summary: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice guidelines. Circulation 145(3):e4–e17
Collet JP, Thiele H, Barbato E, Barthelemy O, Bauersachs J, Bhatt DL et al (2021) 2020 ESC guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Rev Esp Cardiol (Engl Ed) 74(6):544
Pietrzykowski L, Michalski P, Kosobucka A, Kasprzak M, Fabiszak T, Stolarek W et al (2020) Medication adherence and its determinants in patients after Myocardial Infarction. Sci Rep 10(1):12028
Thim T, Johansen MB, Chisholm GE, Schmidt M, Kaltoft A, Sørensen HT et al (2014) Clopidogrel discontinuation within the first year after coronary drug-eluting stent implantation: an observational study. BMC Cardiovasc Disord 14:100
Latry P, Martin-Latry K, Lafitte M, Peter C, Couffinhal T (2012) Dual antiplatelet therapy after Myocardial Infarction and percutaneous coronary intervention: analysis of patient adherence using a French health insurance reimbursement database. EuroIntervention: journal of EuroPCR in collaboration with the Working Group on Interventional Cardiology of the European Society of Cardiology. 7(12):1413–1419
Lauffenburger JC, Choudhry NK (2018) A call for a systems-thinking Approach to Medication Adherence: stop blaming the patient. JAMA Intern Med 178(7):950–951
Alexopoulos D, Galati A, Xanthopoulou I, Mavronasiou E, Kassimis G, Theodoropoulos KC et al (2012) Ticagrelor versus prasugrel in acute coronary syndrome patients with high on-clopidogrel platelet reactivity following percutaneous coronary intervention: a pharmacodynamic study. J Am Coll Cardiol 60(3):193–199
Alexopoulos D, Xanthopoulou I, Stavrou K, Hahalis G, Davlouros P (2013) Platelet reactivity measurements reveal patient noncompliance during ticagrelor maintenance therapy. Can J Cardiol 29(12):1743e13–1743e14
Acknowledgements
Not applicable.
Funding
This work was supported by the National Medical Research Council, Singapore, (grants NMRC/CSA-INV/0006/2016 [principal investigator, Dr Chan] and NMRC/STaR/0022/2014 [principal investigator, Dr Richards]), National Medical Research Council Collaborative Centre Grant (grant NMRC/CGAug16C006), and AstraZeneca (grant ESR-14-10490). Dr Hausenloy was supported by the National Institute for Health Research University College London Hospitals Biomedical Research Centre, Duke–National University Singapore Medical School, and Singapore Ministry of Health’s National Medical Research Council under its Clinician Scientist-Senior Investigator scheme (grant NMRC/CSA-SI/0011/2017).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
Drs Chan, Chin, J. Tan, Ho, Loh: receive consultation honoraria from AstraZeneca. Drs Chan, Richards and Hausenloy receive research grant funding from AstraZeneca. Dr J. Tan reports grants from Medtronic and honorarium from Bayer, Roche Diagnostics, and Philips outside the submitted work. No other disclosures were reported.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sim, H.W., Koh, K.W.L., Poh, SC. et al. Remote intensive management to improve antiplatelet adherence in acute myocardial infarction: a secondary analysis of the randomized controlled IMMACULATE trial. J Thromb Thrombolysis 57, 408–417 (2024). https://doi.org/10.1007/s11239-023-02931-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11239-023-02931-6