Abstract
Cancer is a known hypercoagulable state that leads to an increased risk of venous thromboembolism (VTE). Low molecular weight heparin remains the preferred anticoagulant for VTE in patients with cancer over vitamin K antagonist. However, the preferred anticoagulant in prevention of stroke and systemic embolism in atrial fibrillation (AF) in patients with cancer has yet to be determined. The direct oral anticoagulants (DOACs) are increasingly being utilized; however their role in cancer has only recently been investigated. The objective of this retrospective cohort was to describe real-world anticoagulation prescribing patterns in cancer patients at a large academic medical center between January 1, 2013 and October 31, 2016. We sought to assess the safety, tolerability, and efficacy of DOACs in patients with cancer for either VTE and/or AF. Patient demographic, clinical characteristics, as well as bleeding and thrombotic events were collected. There were 214 patients in our analysis, of which 71 patients (33%) received a DOAC [apixaban (n = 22), dabigatran (n = 17), and rivaroxaban (n = 32)]. There were fewer bleeding events and/or discontinuations in the DOAC group compared to enoxaparin (13 vs. 27, p = 0.022). There was no difference in major or minor bleeds or thromboembolic events in comparing DOAC to enoxaparin or DOAC to warfarin. This was a retrospective, single-institution study assessing the safety and efficacy of DOACs compared to warfarin or enoxaparin in patients with cancer. DOACs may represent an alternative to warfarin or enoxaparin in patients with cancer for VTE and/or stroke reduction in AF.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cancer is a well-established hypercoagulable state that is associated with a 4–7 fold increased risk of venous thromboembolism (VTE) [1, 2]. It has been estimated that 18% of the total number of VTE cases are attributed to cancer with an annual VTE incidence of 1–2 for every 1000 people [1]. This high rate of cancer-associated VTE has been associated with a direct 5-year health cost per patient of $49,351 for cancer patients with VTE compared to $26,529 for cancer patients without VTE [3]. Therefore, optimal therapeutic anticoagulation is necessary to prevent further thromboembolic events and reduce cost associated with VTE in cancer patients.
The current standard of care for treatment of VTE in patients with cancer is low-molecular-weight heparin (LMWH) over warfarin, a vitamin K antagonist (VKA) [4,5,6,7]. Enoxaparin, a LMWH, has predictable pharmacokinetics, fixed weight-based dosing and minimal laboratory monitoring compared to warfarin. However, challenges with enoxaparin therapy include cost and subcutaneous (subQ) administration. Thus, there remains a large interest in utilizing the direct oral anticoagulants (DOACs) in patients with cancer due to the fixed oral dosing schedule, predictable pharmacokinetics, and minimal drug interactions. Data regarding the safety and efficacy of apixaban, a factor Xa inhibitor, and dabigatran, a direct thrombin inhibitor, in cancer, is extrapolated from larger data registries resulting in small heterogeneous sample size. The AMPLIFY trial, comparing apixaban to VKA in patients with VTE, only had 2.7% of patients with cancer while the RECOVER and RECOVER-II trials, studying dabigatran against initial parental anticoagulation followed by VKA, only had 7% of patients with active cancer [8,9,10,11].
There has been recent emerging data specifically utilizing rivaroxaban, a factor Xa inhibitor, for VTE in patients with cancer. Rivaroxaban was initially shown to be non-inferior to conventional therapy in the EINSTEIN-DVT and PE trials for acute VTE [12, 13]. A subgroup analysis of patients with active cancer enrolled in EINSTEIN-DVT and PE trials demonstrated that rivaroxaban was as efficacious to conventional therapy and reduced the number of bleed events [14]. Subsequently, three single center retrospective cohort studies concluded that rivaroxaban may be a viable option for cancer associated VTE [15,16,17].
In addition, there is limited data evaluating the tolerability and efficacy of the DOACs for stroke and/or systemic embolism prevention in patients with cancer and atrial fibrillation (AF). Although the association between AF and cancer is not as well defined, AF remains the most common cardiac arrhythmia and affects more than 33 million people across the world [18, 19]. The DOACs have shown comparable efficacy and safety to VKA for stroke prevention in non-valvular AF [20,21,22]. However, these trials excluded patients at high risk for bleeding complications or with life expectancies of less than 1–3 years, therefore potentially discounting a number of patients with active cancer [23]. A recent Danish population based cohort study found similar rates of thromboembolic events and bleeding in patients with and without cancer with AF when comparing VKA or DOAC therapy [24]. Although an attractive option, data to support utilization of the DOACs preferentially for this particular patient population remains limited.
The DOACs may be convenient alternatives for patients with cancer, especially those with better prognoses and longer life expectancy [8]. This retrospective cohort study uniquely focuses on the safety, tolerability, and efficacy of the DOACs in VTE and /or AF in cancer patients in our institution.
Methods
We conducted a single-centered, institutional review board approved, retrospective cohort study at New York University Langone Health (NYULH), an 800 bed tertiary academic medical center. Patients admitted to NYULH, with active cancer between January 2013 and October 2016, were eligible for inclusion. Active cancer was defined by the diagnosis of cancer, other than basal-cell or squamous-cell carcinoma of the skin and excision of melanoma, and receiving any treatment within the previous year, or recurrent or metastatic cancer. These patients were included if they were at least 18 years of age, and received therapeutic anticoagulation with enoxaparin, warfarin or a DOAC including dabigatran, apixaban, or rivaroxaban. Edoxaban use had not been adopted into our healthcare system during this time. Patients receiving prophylactic dosed anticoagulation were excluded.
Data collection was obtained through a retrospective medical record review of baseline demographics and past medical history including hypertension, cardiac abnormalities, hyperlipidemia, diabetes, history of smoking status within the past year, renal disease, chronic obstructive pulmonary disease, gastrointestinal bleed, coagulopathy, recent major surgery or trauma in past 6 months, cirrhosis, or factor V Leiden gene mutation. Other data collected included dosing of anticoagulation, concomitant antiplatelet therapy, cancer history, chemotherapy regimen, bleeding events, and thromboembolic events. For the patients with a past medical history of AF, CHA2DS2-VASc scores were calculated. Data was managed utilizing Research Electronic Data Capture (REDCap) which is a secure informatics system designed to support data collection across various research disciplines [25].
The primary outcome was a composite of safety and tolerability. Safety was determined by the number of major and minor bleeds. Major bleeding events was defined using the International Society of Thrombosis and Hemostasis criteria: fatal bleeding, and/or symptomatic bleeding in a critical area or organ (including intracranial, intraspinal, intraocular, retroperitoneal, intra-articular, pericardial or intramuscular bleeding with compartment syndrome), and/or a greater than 2 g/dl decrease in hemoglobin or bleeding necessitating 2 or 3 units of whole blood or packed red blood cells [26]. Clinically relevant minor bleeding was defined as overt bleeding noted by a physician that was not attributed to an alternative source. Tolerability was determined by the number of discontinuations of anticoagulation therapy. Reasons for discontinuations included major or minor bleed event, thrombocytopenia, subQ administration, international normalized ratio (INR) testing, cost of therapy, acute kidney injury (AKI), other and unclear documented reason in the patient’s chart. Acute kidney injury (AKI) was defined by RIFLE criteria [27]. Secondary outcomes included safety, tolerability, and efficacy. Efficacy was determined by the incidence of thromboembolic events including DVT, PE, and/or ischemic stroke.
Statistical analysis was performed using SPSS version 23 to compare two groups: DOAC versus enoxaparin and DOAC versus warfarin. Descriptive variables were reported as medians and percentages. Chi square test and Fisher’s exact test were used for categorical variables. Mann–Whitney U test was used for continuous variables. A univariate analysis was performed on the primary and secondary outcomes. A p value < 0.05 was considered statistically significant.
Results
We identified a total of 1470 patients based on ICD-9 and 10 codes for cancer who also received at least one dose of therapeutic anticoagulation during the study period. SAS was utilized to select random cases. In total 335 patients were screened and 214 were included for analysis. The screening methods are summarized in Fig. 1. There were 77 (36%) patients that received enoxaparin, 66 (31%) patients that received warfarin and 71 (33%) patients that received a DOAC. Of the patients who received a DOAC, 22 received apixaban, 17 received dabigatran and 32 received rivaroxaban. The median age in this cohort was 69 years (IQR 59, 79), 76% of patients were Caucasian, and 44% of patients were male. The most common past medical history was hypertension (115, 54%) followed by cardiac abnormalities (96, 45%). There was a statistically significant difference between the DOAC versus enoxaparin group in median age (74 vs. 61 years, p = 0.001), cardiac abnormalities (41 vs. 11, p = 0.001), AF (37 vs. 5, p = 0.001), coronary artery disease (17 vs. 6, p = 0.007), hypertension (40 vs. 30, p = 0.034), hyperlipidemia (39 vs. 23, p = 0.002) and stroke (10 vs. 1, p = 0.003). There was a statistically significant difference between the DOAC versus warfarin group in hyperlipidemia (39 vs. 23, p = 0.025). The majority of the patients in the cohort had solid tumor disease (187, 87%) with lung and breast cancer as the most common malignancies. A small percentage had hematologic cancers (27, 13%) as well as current treatment with an immunomodulator (4, 2%) or vascular endothelial growth factor (VEGF) inhibitor (4, 2%). All other baseline characteristics were similar across treatment groups. Patients were more likely to receive enoxaparin for DVT or PE, 44 (57%) and 34 (44.2%) respectively (p = 0.001). In contrast, warfarin and DOACs were more likely used for stroke reduction with AF, 32 (49%) and 44 (62%) respectively (p = 0.112). Warfarin was also used in valvular AF and mechanical valve in a small number of patients, 5 (8%) and 3 (5%) respectively. The baseline demographics and past medical histories are described in Table 1, oncologic history in Table 2, and anticoagulation indication in Table 3.
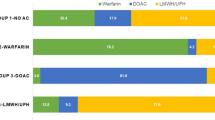
Of the 214 patients receiving anticoagulation, 60 (28%) patients had a bleed event and/or discontinued anticoagulation therapy (Fig. 2). Among the patients who had a bleed event or discontinued therapy 13 (18%) patients received a DOAC, 27 (35%) patients received enoxaparin, and 20 (30%) patients received warfarin. As a composite, there were fewer discontinuations and/or bleed events in the DOAC group compared to enoxaparin (13 vs. 27, p = 0.022), and fewer discontinuations and/or bleed events in the DOAC group compared to warfarin, though not significant (13 vs. 20, p = 0.101).
Safety
There were 25 (12%) patients that experienced a bleed event in this cohort (Table 4). There were 9 episodes of major bleeds and 16 episodes of minor bleeds. Among the patients who had a major bleed event, 2 (3%) received a DOAC, 3 (4%) received enoxaparin, and 4 (6%) received warfarin. There was no difference found in major bleed episodes between the DOAC versus enoxaparin group or the DOAC versus warfarin group (p = 0.683, 0.672). Within the 9 patients who experienced a major bled, each individual’s anticoagulation therapy was dosed appropriately accounting for indication, body weight, renal function, and drug interactions. The two major bleeds that occurred in the DOAC group occurred in patients with AKI at the time of the bleed, 1 bleed on dabigatran and 1 bleed on rivaroxaban. For the major bleeds that occurred on warfarin therapy, the median INR at time bleed was 4 (IQR 2.7, 5.5) and one patient was initiated on a macrolide antibiotic within 2 weeks of the major bleed episode. The median time on anticoagulation before a major bleed episode was 13 months (IQR 2, 20.5).
Of the patients who experienced a minor bleed event, 5 (7%) received enoxaparin, 5 (8%) received warfarin, and 6 (9%) received a DOAC (2 on apixaban, 3 on dabigatran, and 1on rivaroxaban). There was no difference found in minor bleed events between the DOAC versus enoxaparin group or the DOAC versus warfarin group (p = 0.650, 0.851). For the minor bleeds, 1 individual on enoxaparin and 1on dabigatran were on suboptimal dosing (incorrect renal adjustment and concomitant interacting medication) at the time of the bleed. The median time on anticoagulation before a minor bleed episode was 16 months (IQR 1, 36).
Tolerability
We observed 53 (25%) patients discontinue anticoagulation therapy in this cohort. Of those patients who discontinued therapy, 11 (15%) discontinued a DOAC, 26 (34%) discontinued enoxaparin and 16 (24%) discontinued warfarin. There were fewer discontinuations in the DOAC group versus enoxaparin (11 vs. 26, p = 0.010) and there were fewer discontinuations in the DOAC group versus warfarin (11 vs. 16, p = 0.19). Discontinuation of therapy due to a bleeding event occurred in 5 patients on enoxaparin, 4 patients on warfarin, and 5 patients on a DOAC. The most common reason for enoxaparin discontinuations was intolerance due to subQ administration which was observed in 8 patients (31%). The most common reasons for warfarin discontinuations was unclear documented reason (6, 38%), inconvenience of INR testing (4, 25%) and bleed event (4, 25%). Of the11 patients who discontinued DOAC therapy, 3 were on apixaban, 3 were on dabigatran, and 5 were on rivaroxaban. There were 11 patients on warfarin who switched anticoagulation therapies (1 switch to enoxaparin, 4 to apixaban, and 6 to rivaroxaban). Of the 27 patients on enoxaparin, 12 patients switched anticoagulation therapies (4 to warfarin, 1 to apixaban, and 7 to rivaroxaban). Only 1 patient on a DOAC switched therapy from dabigatran to apixaban.
Efficacy
There were 23 patients (11%) that experienced a thromboembolic event in this cohort. There were 4 (5.6%) patients within the DOAC cohort, 9 (11.7%) within the enoxaparin cohort, and 10 (15.2%) within the warfarin cohort. There was no difference found between the DOAC versus enoxaparin group (4 vs. 9, p = 0.110) or DOAC versus warfarin group (4 vs. 10, p = 0.185) for thromboembolic events. We found that there were less recurrent DVTs in the DOAC group versus enoxaparin (0 vs. 6, p = 0.005) and the DOAC group versus warfarin (0 vs. 7, p = 0.029). Out of the 9 patients on enoxaparin, there were 6 recurrent DVT episodes, 2 recurrent PE episodes, and 1 episode of ischemic stroke. One of the patients that had a PE in this cohort was not on therapeutic enoxaparin at the time of event. Compliance for all other patients to anticoagulation was assumed based on documentation, at the time of thromboembolic event. Of the patients on warfarin, 7 experienced a recurrent DVT and 3 experienced PE. Of note, one patient within the warfarin group experienced both a DVT and PE which accounted as two separate events. The median INR at the time of thromboembolic event was 1.3 (IQR 1.1, 1.5) and two patients reported nonadherence with warfarin. For those on a DOAC, there were 3 episodes of ischemic stroke, 1 PE event, and 0 DVT events. Of the 3 ischemic stroke episodes, 2 occurred in the rivaroxaban subgroup and 1 in the dabigatran subgroup. Notably the patient in the dabigatran group was not taking dabigatran at the time of thromboembolic event. The only PE event occurred on rivaroxaban. For the rivaroxaban subgroup, compliance to anticoagulation was assumed based on documentation, at the time of thromboembolic event. There was no thromboembolic events found with apixaban. The median time to any thromboembolic event was 9.4 months (IQR 1.5, 41.7) in the total patient population. The median time, within the total patient population, to DVT, PE, or ischemic stroke was 20.8 months (IQR 1.3, 55.4), 7.6 months (IQR 1.4, 19.4), and 5.1 months (IQR 0.9, 35.5), respectively. Detailed characteristics for each DOAC can be found in the supplemental material (Online Resource 1).
Discussion
Our study describes real-world anticoagulation prescribing patterns in patients with cancer at a large academic medical center. Although LMWH is considered the preferred anticoagulant in patients with cancer, its clinical use may be limited by patient preference, inconvenience of subcutaneous administration, or cost. Furthermore, there is limited evidence looking at discontinuation rates of VKA due to inconvenience of INR testing. The availability of fixed-dose DOACs has an appealing option for patients with cancer, to improve adherence and provide sustainable anticoagulation without the need for routine laboratory monitoring. However, there remains limited data supporting the safety and efficacy of these agents in patients with cancer for VTE due to small percentages of patients with cancer in trials [9].
Despite limited data evaluating the safety and efficacy of DOACs in patients with cancer, these agents are being utilized in clinical practice at NYULH, as 33% of patients in our cohort were prescribed a DOAC. Of note, majority of DOAC use was in patients with solid tumors. For the DOACs, we noted rivaroxaban used most frequently, followed by apixaban, then dabigatran. This could be due to the available evidence thus far for rivaroxaban for treatment of VTE in patients with cancer. A subgroup analysis of patients with active cancer in the EINSTEIN-DVT and EINSTEIN PE trial demonstrated recurrent venous thromboembolism occurred in 5% with rivaroxaban and 7% with enoxaparin and vitamin K antagonist [14]. There were 2% of patients in the rivaroxaban group and 5% in the enoxaparin and vitamin K antagonist group who experienced a major bleed [14]. Subsequent single center retrospective studies have demonstrated similar safety and efficacy with rivaroxaban for VTE in patients with cancer [15, 16]. Bott-Kitslaar et al. specifically studied rivaroxaban for VTE in patients with cancer compared to patients with no cancer. Rates of VTE recurrence in patients with cancer were 4 (3.3%) out of 118 with a major bleed occurrence of 3 (2.5%) [16]. Pignataro et al. observed that 3.25% of their study population had a VTE reoccurrence with 5.5% having a major bleed [15]. A recent single centered prospective study assessed rivaroxaban in treatment of cancer associated VTE compared to enoxaparin and saw 4.4% cumulative incidence rate of new or recurrent VTE in 6 months [28].
Our study found similar rates of thromboembolic events and major bleeds among the entire DOAC group, 5.6 and 2.8% respectively. Two meta-analyses looking at DOACs against heparin bridge to VKA, LMWH, or placebo therapy in patients with cancer also described low rates of recurrence VTE [29, 30]. However, one meta-analysis saw an increased rate of clinical relevant bleeding in the DOAC group (8.6 vs. 5.8%). Although we observed more recurrent DVTs in the enoxaparin group (n = 6) and warfarin group (n = 7) compared to DOACs (n = 0), upon univariate analysis, this was not statistically significant and may have been due to chance given the heterogeneous patient population. In our study, rivaroxaban was more routinely used for VTE or history of VTE (38% DVT, 16% PE, and 19% history of VTE) while apixaban and dabigatran were mainly used for AF (68 and 100%) suggesting clinician preference for rivaroxaban for VTE compared to the other agents in patients with cancer. In addition, there were low rates of discontinuations of DOAC agents (15%) compared to enoxaparin or warfarin suggesting that DOACs are tolerable and convenient medications. An interesting finding was that of the patients on warfarin and enoxaparin who switched therapies, the majority were switched to rivaroxaban, further suggesting clinician preference for rivaroxaban in patients with cancer.
Although LMWH is preferred over VKA for the treatment of VTE in patients with cancer, there is no ‘gold-standard’ recommendation for the preferred anticoagulation for the reduction of stroke and systemic embolism in patients with AF and cancer. In our study, DOACs were chosen in older patients with cardiac abnormalities such as AF. Interestingly, dabigatran was solely used for AF within our study cohort. In the RELY trial, studying dabigatran against warfarin, 1.11% patients per year experienced a stroke or systemic embolism, 3.11% patients per year experienced a major bleed, and 14.84% patients per year experienced a minor bleed within the dabigatran 150 mg twice daily group [20]. In our study, only 1 (5.8%) patient experienced an episode of ischemic stroke, 1 (5.8%) patient experienced a major bleed on dabigatran who had AKI at the time and 3 (17.6%) patients experienced a minor bleed on dabigatran. Although there were only 17 patients on dabigatran in our cohort, the percentage of bleeding events were relatively similar.
Our study is limited by its retrospective nature and small sample size. The patient population was heterogeneous; however this study highlights a real-life application of the DOACs in patients with cancer. The patients within the oral anticoagulant population had significantly more cardiovascular disease compared to enoxaparin. In addition, there was a significant difference in the number of patients with metastatic disease when comparing DOAC versus enoxaparin suggesting potentially avoidance of utilizing DOAC in advanced cancer patients at higher risk of developing VTE. However, there was no significance in pancreatic, hematologic, brain, gynecologic, and lung cancers which are cancers thought to be at higher risk for VTE [1]. Lastly, clinician prescribing bias could not be controlled; therefore patients may have not had the opportunity to fail a particular anticoagulation therapy if the clinician purposely avoided therapy due to insurance cost etc.
In conclusion, anticoagulation therapy is frequently warranted in patients with cancer due to hypercoagulability. In our study, we found DOACs to be a safe and effective alternative to LMWH or VKA in patients with cancer. While DOACs are increasingly being utilized in patients with AF or VTE, research regarding the safety and efficacy in cancer patients is still investigational. Based on our findings, DOACs may represent an attractive alternative to warfarin or enoxaparin in patients with cancer for VTE and/or stroke reduction in AF. Future prospective studies are needed to confirm the safety and efficacy of DOACs in cancer patients. In addition, although newer literature primarily focuses on rivaroxaban, whether a preferred DOAC agent exists in cancer patients remains unknown.
References
Ay C, Pabinger I, Cohen AT (2017) Cancer-associated venous thromboembolism: burden, mechanisms, and management. Thromb Haemost 117(2):219–230. doi:10.1160/TH16-08-0615
Linkins LA (2008) Management of venous thromboembolism in patients with cancer: role of dalteparin. Vasc Health Risk Manag 4(2):279–287
Cohoon KP, Ransom JE, Leibson CL, Ashrani AA, Petterson TM, Long KH, Bailey KR, Heit JA (2016) Direct medical costs attributable to cancer-associated venous thromboembolism: a population-based longitudinal study. Am J Med 129(9):1000 e1015–1000 e1025. doi:10.1016/j.amjmed.2016.02.030
Lee AY, Levine MN, Baker RI, Bowden C, Kakkar AK, Prins M, Rickles FR, Julian JA, Haley S, Kovacs MJ, Gent M, Randomized Comparison of Low-Molecular-Weight Heparin versus Oral Anticoagulant Therapy for the Prevention of Recurrent Venous Thromboembolism in Patients with Cancer I (2003) Low-molecular-weight heparin versus a coumarin for the prevention of recurrent venous thromboembolism in patients with cancer. N Engl J Med 349 (2):146–153. doi:10.1056/NEJMoa025313
Hull RD, Pineo GF, Brant RF, Mah AF, Burke N, Dear R, Wong T, Cook R, Solymoss S, Poon MC, Raskob G, Investigators LT (2006) Long-term low-molecular-weight heparin versus usual care in proximal-vein thrombosis patients with cancer. Am J Med 119(12):1062–1072. doi:10.1016/j.amjmed.2006.02.022
Kearon C, Akl EA, Ornelas J, Blaivas A, Jimenez D, Bounameaux H, Huisman M, King CS, Morris TA, Sood N, Stevens SM, Vintch JR, Wells P, Woller SC, Moores L (2016) Antithrombotic therapy for VTE disease: CHEST guideline and expert panel report. Chest 149(2):315–352. doi:10.1016/j.chest.2015.11.026
Streiff MB, Holmstrom B, Ashrani A, Bockenstedt PL, Chesney C, Eby C, Fanikos J, Fenninger RB, Fogerty AE, Gao S, Goldhaber SZ, Hendrie P, Kuderer N, Lee A, Lee JT, Lovrincevic M, Millenson MM, Neff AT, Ortel TL, Paschal R, Shattil S, Siddiqi T, Smock KJ, Soff G, Wang TF, Yee GC, Zakarija A, McMillian N, Engh AM (2015) Cancer-associted venous thromoembolic disease, Version 1. 2015. J Natl Compr Canc Netw 13(9):1079–1095
Franchini M, Bonfanti C, Lippi G (2015) Cancer-associated thrombosis: investigating the role of new oral anticoagulants. Thromb Res 135(5):777–781. doi:10.1016/j.thromres.2015.02.024
van der Hulle T, Kooiman J, den Exter PL, Dekkers OM, Klok FA, Huisman MV (2014) Effectiveness and safety of novel oral anticoagulants as compared with vitamin K antagonists in the treatment of acute symptomatic venous thromboembolism: a systematic review and meta-analysis. J Thromb Haemost 12(3):320–328. doi:10.1111/jth.12485
Agnelli G, Buller HR, Cohen A, Curto M, Gallus AS, Johnson M, Masiukiewicz U, Pak R, Thompson J, Raskob GE, Weitz JI, Investigators A (2013) Oral apixaban for the treatment of acute venous thromboembolism. N Engl J Med 369(9):799–808. doi:10.1056/NEJMoa1302507
Schulman S, Kearon C, Kakkar AK, Mismetti P, Schellong S, Eriksson H, Baanstra D, Schnee J, Goldhaber SZ, Group R-CS (2009) Dabigatran versus warfarin in the treatment of acute venous thromboembolism. N Engl J Med 361(24):2342–2352. doi:10.1056/NEJMoa0906598
Investigators E, Bauersachs R, Berkowitz SD, Brenner B, Buller HR, Decousus H, Gallus AS, Lensing AW, Misselwitz F, Prins MH, Raskob GE, Segers A, Verhamme P, Wells P, Agnelli G, Bounameaux H, Cohen A, Davidson BL, Piovella F, Schellong S (2010) Oral rivaroxaban for symptomatic venous thromboembolism. N Engl J Med 363(26):2499–2510. doi:10.1056/NEJMoa1007903
Investigators E-P, Buller HR, Prins MH, Lensin AW, Decousus H, Jacobson BF, Minar E, Chlumsky J, Verhamme P, Wells P, Agnelli G, Cohen A, Berkowitz SD, Bounameaux H, Davidson BL, Misselwitz F, Gallus AS, Raskob GE, Schellong S, Segers A (2012) Oral rivaroxaban for the treatment of symptomatic pulmonary embolism. N Engl J Med 366(14):1287–1297. doi:10.1056/NEJMoa1113572
Prins MH, Lensing AW, Brighton TA, Lyons RM, Rehm J, Trajanovic M, Davidson BL, Beyer-Westendorf J, Pap AF, Berkowitz SD, Cohen AT, Kovacs MJ, Wells PS, Prandoni P (2014) Oral rivaroxaban versus enoxaparin with vitamin K antagonist for the treatment of symptomatic venous thromboembolism in patients with cancer (EINSTEIN-DVT and EINSTEIN-PE): a pooled subgroup analysis of two randomised controlled trials. Lancet Haematol 1(1):e37–e46. doi:10.1016/S2352-3026(14)70018-3
Pignataro BS, Nishinari K, Cavalcante RN, Centofanti G, Yazbek G, Krutman M, Bomfim GA, Fonseca IY, Teivelis MP, Wolosker N, Sanches SM, Ramacciotti E (2016) Oral rivaroxaban for the treatment of symptomatic venous thromboembolism in 400 patients with active cancer. Clin Appl Thromb Hemost. doi:10.1177/1076029616677800
Bott-Kitslaar DM, Saadiq RA, McBane RD, Loprinzi CL, Ashrani AA, Ransone TR, Wolfgram AA, Berentsen MM, Wysokinski WE (2016) Efficacy and safety of rivaroxaban in patients with venous thromboembolism and active malignancy: a single-center registry. Am J Med 129(6):615–619. doi:10.1016/j.amjmed.2015.12.025
Nicklaus MD, Ludwig SL, Kettle JK (2017) Recurrence of malignancy-associated venous thromboembolism among patients treated with rivaroxaban compared to enoxaparin. J Oncol Pharm Pract. doi:10.1177/1078155217690922
Rahman F, Ko D, Benjamin EJ (2016) Association of atrial fibrillation and cancer. JAMA Cardiol 1(4):384–386. doi:10.1001/jamacardio.2016.0582
Chugh SS, Havmoeller R, Narayanan K, Singh D, Rienstra M, Benjamin EJ, Gillum RF, Kim YH, McAnulty JH, Zheng ZJ, Forouzanfar MH, Naghavi M, Mensah GA, Ezzati M, Murray CJL (2014) Worldwide epidemiology of atrial fibrillation a global burden of disease 2010 study. Circulation 129(8):837–847. doi:10.1161/Circulationaha.113.005119
Connolly SJ, Ezekowitz MD, Yusuf S, Eikelboom J, Oldgren J, Parekh A, Pogue J, Reilly PA, Themeles E, Varrone J, Wang S, Alings M, Xavier D, Zhu J, Diaz R, Lewis BS, Darius H, Diener HC, Joyner CD, Wallentin L, Committee R-LS, Investigators (2009) Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med 361(12):1139–1151. doi:10.1056/NEJMoa0905561
Patel MR, Mahaffey KW, Garg J, Pan G, Singer DE, Hacke W, Breithardt G, Halperin JL, Hankey GJ, Piccini JP, Becker RC, Nessel CC, Paolini JF, Berkowitz SD, Fox KA, Califf RM, Investigators RA (2011) Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med 365(10):883–891. doi:10.1056/NEJMoa1009638
Granger CB, Alexander JH, McMurray JJ, Lopes RD, Hylek EM, Hanna M, Al-Khalidi HR, Ansell J, Atar D, Avezum A, Bahit MC, Diaz R, Easton JD, Ezekowitz JA, Flaker G, Garcia D, Geraldes M, Gersh BJ, Golitsyn S, Goto S, Hermosillo AG, Hohnloser SH, Horowitz J, Mohan P, Jansky P, Lewis BS, Lopez-Sendon JL, Pais P, Parkhomenko A, Verheugt FW, Zhu J, Wallentin L, Committees A, Investigators (2011) Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med 365(11):981–992. doi:10.1056/NEJMoa1107039
Short NJ, Connors JM (2014) New oral anticoagulants and the cancer patient. Oncologist 19(1):82–93. doi:10.1634/theoncologist.2013-0239
Ording AG, Horvath-Puho E, Adelborg K, Pedersen L, Prandoni P, Sorensen HT (2017) Thromboembolic and bleeding complications during oral anticoagulation therapy in cancer patients with atrial fibrillation: a Danish nationwide population-based cohort study. Cancer Med 6(6):1165–1172. doi:10.1002/cam4.1054
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG (2009) Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 42(2):377–381. doi:10.1016/j.jbi.2008.08.010
Schulman S, Kearon C, Subcommittee on Control of Anticoagulation of the S, Standardization Committee of the International Society on T, Haemostasis (2005) Definition of major bleeding in clinical investigations of antihemostatic medicinal products in non-surgical patients. J Thromb Haemost 3(4):692–694. doi:10.1111/j.1538-7836.2005.01204.x
Bellomo R, Ronco C, Kellum JA, Mehta RL, Palevsky P, Acute Dialysis Quality Initiative w (2004) Acute renal failure—definition, outcome measures, animal models, fluid therapy and information technology needs: the Second International Consensus Conference of the Acute Dialysis Quality Initiative (ADQI) Group. Crit Care 8 (4):R204–R212. doi:10.1186/cc2872
Mantha S, Laube E, Miao Y, Sarasohn DM, Parameswaran R, Stefanik S, Brar G, Samedy P, Wills J, Harnicar S, Soff GA (2017) Safe and effective use of rivaroxaban for treatment of cancer-associated venous thromboembolic disease: a prospective cohort study. J Thromb Thrombolysis 43(2):166–171. doi:10.1007/s11239-016-1429-1
Vedovati MC, Germini F, Agnelli G, Becattini C (2015) Direct oral anticoagulants in patients with VTE and cancer: a systematic review and meta-analysis. Chest 147(2):475–483. doi:10.1378/chest.14-0402
Sardar P, Chatterjee S, Herzog E, Pekler G, Mushiyev S, Pastori LJ, Visco F, Aronow WS (2015) New oral anticoagulants in patients with cancer: current state of evidence. Am J Ther 22(6):460–468. doi:10.1097/MJT.0000000000000055
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Xiang, E., Ahuja, T., Raco, V. et al. Anticoagulation prescribing patterns in patients with cancer. J Thromb Thrombolysis 45, 89–98 (2018). https://doi.org/10.1007/s11239-017-1558-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11239-017-1558-1