Abstract
Purpose
Chemotherapy exerts adverse effects on physical, psychological and social functioning in women with breast cancer, which may trigger adaptive activities. For a better understanding of the experience of symptoms associated with chemotherapy and the development of targeted interventions, this study aimed to (a) explore the patient experience of chemotherapy, (b) identify patients’ strategies to cope with the side effects and distress and (c) explore the link between their experience and coping strategies.
Methods
Qualitative studies were included if they explored the experience or coping strategies of women with breast cancer receiving chemotherapy. Instruments from the Joanna Briggs Institute were used to critically appraise the methodological quality, extract data and aggregate findings from the included studies.
Results
Twelve studies presenting findings from 184 women with breast cancer who had received chemotherapy were included in this review. Three synthesized findings were identified from 8 categories based on 91 original findings: (1) Women living with chemotherapy experienced various stressful side effects, and their lives were changed. (2) Supportive care to address needs is essential to help women get through this difficult time. (3) They engaged in numerous types of coping strategies to deal with side effects and adapt to this difficult journey. Moreover, the link between experience of chemotherapy and coping strategies is based on the Lazarus’ stress and coping theory.
Conclusions
Although the experience of women with breast cancer undergoing chemotherapy is individualized, we concluded that the distressing experience related to chemotherapy as a stimulus was viewed as a stressor that demands coping or adaptation. Based on the Lazarus stress and coping theory, the ability of a woman to appraise how chemotherapy changed her life and how she appraises her resources to cope with chemotherapy are essential. The results highlight that pre-chemotherapy care programmes, information support systems, social support groups and individual effective coping strategies are helpful in reducing treatment-related distress levels and enhance self-care effects at home.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
The effects of breast cancer and chemotherapy
Breast cancer has the highest incidence of cancer in women worldwide and is the leading cause of cancer-related death. In 2018, 2,090,000 new cases and 626,000 deaths due to breast cancer occurred in women worldwide, accounting for 11.6% and 0.6% of all cancers, respectively [1]. Organized breast cancer screening and advances in adjuvant therapy have helped decrease breast cancer mortality rates and improve survival rates [2, 3]. Currently, the 5-year survival rate is greater than 90%, and the 10-year survival rate is greater than 80%. Clinically, the first five to ten years after breast cancer treatment represent a vulnerable period, during which some women face a multitude of physical and psychosocial problems [4].
Over half of patients with breast cancer are treated with chemotherapy that comprises chemical agents for both localized and metastatic cancer. For patients who present with localized cancer, the therapeutic goals are tumour eradication and recurrence prevention, while the therapeutic goals for patients who present with metastatic cancer are the prolongation of survival, maintenance of quality of life and palliation of symptoms [5, 6]. Chemotherapy helps reduce the 10-year mortality rate and achieve the greatest survival potential in the first 5 years for women with breast cancer [6, 7]. However, chemotherapy has some side effects, which can be immediate, short term or long term [8, 9]. Several quantitative studies have indicated that women with breast cancer undergoing chemotherapy experienced a cluster of symptoms associated with toxicity and side effects and experienced substantial changes in their psychological status, quality of life and social function [8,9,10]. According to most studies, women with breast cancer who received chemotherapy reported a poorer quality of life, physical functioning and psychological functioning (or psychological well-being) than women who did not receive chemotherapy [11, 12].
Qualitative systematic reviews on the experience of chemotherapy
Recently, researchers in related fields have shown considerable interest in exploring the adverse effects of chemotherapy, quality of life during chemotherapy and related interventions to cope with chemotherapy. However, the use of quantitative instruments to capture the unique features of individual experiences of patients with breast cancer related to chemotherapy is challenging, and this approach may omit important issues that would be analysed in a qualitative research study [13]. The perspective of patients on chemotherapy was much deeper than what an outsider would describe; thus, the best sources of information about their experience are the patients themselves. Qualitative studies are valuable because they enable patients to describe their experiences during chemotherapy treatment, facilitating a deeper understanding of the adaptive experiences that emerge. Some qualitative studies have described the lived experiences, social support and coping strategies of women receiving chemotherapy. These studies focussed on specific issues, such as different cycles of chemotherapy and diverse samples (e.g. patients with different stages of cancer, chemotherapy regimens, ages and cultures) [14,15,16,17].
Meta-aggregation is a process that identifies meanings from qualitative studies that may attributed to different methodologies and further abstracts those meanings into categories that are then synthesized [18]. In this review, we chose meta-aggregation as a suitable synthesis methodology to study the experience of chemotherapy among women with breast cancer because it has the advantages listed below [19,20,21]. First, because its philosophical foundation is pragmatic and influenced by transcendental phenomenology, a review focussing on qualitative research is philosophically congruent. Second, one of the special characteristics of a meta-aggregation is that it tries to provide practical implications for the synthesized findings. Third, meta-aggregation can be used to integrate the results of qualitative studies conducted using different designs (i.e. ethnography, grounded theory and phenomenology).
Rationale and objective of the review
An understanding of the current experience and coping strategies of women with breast cancer undergoing chemotherapy may help health-care professionals design self-care programmes or interventions to better prepare and manage the adverse effects of chemotherapy. Previous related qualitative reviews focussed on the symptoms experienced during chemotherapy [22], driving and disabling factors for chemotherapy [23, 24], experience and survivorship of patients with breast cancer [25], or the experience of patients with other types of cancer receiving chemotherapy [26]. Although research on the chemotherapy experience during different periods of cancer and treatment with different drugs and across different regions has increased, no qualitative reviews have focussed on the experience and coping strategies of women with breast cancer. By synthesizing the existing evidence, we hope to provide explicit and in-depth evidence of the experience of this population group while undergoing chemotherapy to guide future research. Therefore, we conducted a review focusing on the specific period of breast cancer treatment to understand women’s inner thoughts. Specifically, the objectives of this review were to analyse the following questions:
(i) What is the experience of women with breast cancer receiving chemotherapy?
(ii) How do they cope with distress during this process?
(iii) What is the link between their experience and coping strategies?
Methods
Inclusion criteria and exclusion criteria
Studies were included in this review if they were (1) original research, (2) qualitative studies, (3) studies focussed on the perspectives of women with breast cancer reporting their experiences, (4) studies focussed on the experience of chemotherapy and (5) studies written in English. Studies were excluded if they (1) analysed other types of cancer, (2) were not focussed on chemotherapy or (3) were mixed-method studies or quantitative studies.
Search strategy
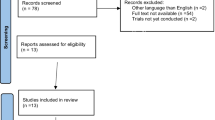
The search strategy (Table 1) aimed to identify published and unpublished qualitative research studies assisted by an evidence-based nursing expert. The search was limited to studies published in the English language. First, an initial unlimited search was performed in PubMed and CINAHL, and an analysis of the title, abstracts and index terms of the resulting articles was then performed. Second, a subsequent search was performed using identified index terms and keywords in the following databases: PubMed (1966–2018), CINAHL (1937–2018), the Cochrane Library (1985–2018), PsycINFO (1887–2018), EBSCO host (1944–2018), Scopus (1823–2018), Embase (1974–2018) and the Web of Science (1900–2018). Third, reference lists of identified articles were searched to find additional studies, including bibliographic searching, reference searching and citation backtracking. Finally, a search for unpublished studies, for example, in OpenSIGLE, Open Grey and the Grey Literature Report by the New York Academy of Medicine Library, was performed to minimize the influence of publication bias on the findings. The search results and process are illustrated in Fig. 1.
Assessment of methodological quality
Using the Johanna Briggs Institute Qualitative Assessment and Review Instrument (JBI-QARI), two independent raters (LPL and WLC) read and assessed the full texts of the included studies. A study that answered a minimum of six of ten prompt questions positively was included (or vice versa). Any disagreements that arose between the reviewers were decided through discussion or with the third reviewer. All studies included in the review met the inclusion and study quality criteria.
Data extraction
Qualitative data were extracted from studies included in the review by two reviewers (YNW and MYH). The extracted information included the bibliographic details, sample age and size, disease stages, numbered findings, data collection methodology, as well as data analysis methodology. Extracted findings together with “Quotations”, which form the first of the three-phased meta-aggregation process, are provided in Online Appendix 1.
Data synthesis
Qualitative research findings were summarized using the standardized data extraction tool from the Joanna Briggs Institute System for the Unified Management, Assessment and Review of Information (JBI-SUMARI). Meta-aggregation involves the synthesis or aggregation of findings to generate a set of statements that represent the aggregation through the assembly of the findings rated according to their quality and categorizing these findings based on similarity in meaning. These categories were then subjected to a meta-aggregation procedure to produce a single comprehensive set of synthesized findings that were used as a basis for evidence-based practice. These categories were then mapped according to the principles and framework of Lazarus’ Psychological Stress and Coping Theory (Fig. 1).
Two independent reviewers assigned a credibility level to each category based on whether the category was accompanied by a direct quote of a participant and how directly the quote(s) were related to the research question [27]. The credibility level was rated as unequivocal, credible, or not supported (see Table 4 footnotes).
Results
Study characteristics
Twelve studies were included in the review [14,15,16,17, 28,29,30,31,32,33,34,35]. These included studies were conducted internationally in the USA (n = 2), the UK (n = 2), Turkey (n = 2), Nigeria (n = 1), China (n = 2), Pakistan (n = 1), Sweden (n = 1),and Syria (n = 1). The sample size ranged from 7 to 30. The total sample of the studies included 184 women aged 22–70 years. The study settings were diverse because of the different countries and varying socioeconomic backgrounds of both the participants and locations. All studies used interviews (n = 11) and focus group discussions (n = 1) for data collection (Table 2).
The quality ratings of 2 studies were 6/10, of 3 studies were 7/10 and of 7 studies were 8/10 (Table 3). No study was excluded from this review.
Results of the synthesis
We included 12 studies in this review, representing 184 participants. Two independent raters identified 91 themes. These themes were clustered into 8 categories and 3 synthesized findings. A summary of each of these themes and associated studies is provided in Table 2. The three synthesized findings are listed below. (1) Women living with chemotherapy experienced various stressful side effects, and their lives were changed. (2) Supportive care to address needs is essential to help women get through this difficult time. (3) They engaged in numerous types of coping strategies to deal with side effects and adapted to this difficult journey.
In addition, the categories rated as having “unequivocal” credibility included physical problems, psychological discomfort, useful information and decision-making and desired social support. Other categories were rated as having “credible” credibility (Table 4).
Synthesized finding 1: women living with chemotherapy experienced various stressful side effects, and their lives were changed
A series of painful side effects accompany chemotherapy. Forty-five extracted findings identified that women undergoing chemotherapy experienced various distressful side effects and their lives were impaired. This synthesized finding included four categories: physical changes, emotional distress, cognitive changes and life changes (see Table 4 and Online Appendix 1).
Physical changes
Although reactions to symptoms and symptom experiences are very individualized, some common symptoms were reported as distressful by most women in this study [15,16,17, 30,31,32,33,34]. The long duration of the chemotherapy process may cause multiple symptoms, including chemotherapy-related fatigue, cognitive changes, hair loss, nausea, vomiting, insomnia, bone pain and peripheral neuropathy. Three physical symptoms were predominant in this study: fatigue, cognitive changes and hair loss. Fatigue included a constant sensation of tiredness, a lack of energy, lethargy and weakness that was not alleviated by resting or sleeping. Hair loss was not permanent but constituted a serious detriment to the women’s image of themselves. Interestingly, physical symptoms were dynamic; namely, the cycle of illness, recovery and illness as chemotherapy progressed was regarded as having a roller coaster effect.
Emotional distress
Fourteen findings extracted from eight studies indicated that women with breast cancer experienced a myriad of psychological burdens during the chemotherapy period, such as worry, fear, anxiety, anger, depression, uncertainty and isolation [14, 16, 17, 28, 30, 32, 34, 35]. Four psychological symptoms were predominant: fear, anxiety, depression and sadness. Women feared that the disease would be incurable and that they would be permanently separated from their family. They felt anxious about the changes in their bodies, the loss of independence and the possibility of recurrence in the future. Furthermore, they felt depressed and sad when they blamed themselves for not fulfilling their maternal responsibilities because of the adverse effects of chemotherapy. As they experienced strong psychological strain, they felt powerless and desperate, and some women had suicidal ideation or attempted suicide.
Cognitive changes
Although the symptoms were very subtle, the cognitive changes experienced affected their abilities to think clearly. Described as “chemo brain”, cognitive changes manifested as (1) difficulty finding words, (2) problems with memory, (3) difficulty in concentrating and paying attention, (4) difficulty organizing and prioritizing problems, (5) fatigue and (6) sensory changes, which created many daily struggles [29,30,31, 34].
Life changes
The symptoms of chemotherapy influence daily life and even the survival of these women [14, 15, 17, 29, 31, 32, 34, 35]. First, the side effects reduced the women’s abilities to perform daily activities and their activity levels. Second, as a wife, mother and daughter, women are the keepers of the family and maintain family functioning. Therefore, they experienced role failure when faced with the physical and emotional burdens of treatment. Third, after physical changes in body appearance and self-image, they became extremely sensitive and felt isolated, similar to stigmatization.
Synthesized finding 2: supportive care to address needs is essential to help women get through this difficult time
As described above, almost all types of patients undergoing chemotherapy face some similar major problems. Studies have focussed on needs for information and social support to assist women in overcoming a list of problems that tend to change and reoccur over time. Twenty-one findings were extracted from six studies that identified that supportive care needs are essential for women to go through this difficult time. This synthesized finding included two categories: the need for information and the need for social support (Table 4 and Online Appendix 1).
The need for information
The proactive dissemination of necessary information is important to equip these women with the abilities to better manage their lives, to provide stability and to relieve pressure [15, 28, 31, 32, 35]. The information they indeed needed was related to self-care practices, life-prolonging procedures and disease prognosis and treatment decisions. Most women concluded that the discomfort from chemotherapy was outweighed by the resulting improvement in survival chances, but few of them were allowed to make choices. Moreover, doctors were the major source of information. Other supplementary resources were received from other cancer survivors, books, the internet and friends with similar experiences.
The need for social support
Twelve of the extracted findings from five studies indicated that social support, particularly from family members and health-care providers, helped women get through this situation with comfort, safety and happiness [14,15,16, 28, 30, 31, 33, 34]. First, family, such as parents, children, husbands and siblings, played the most important role in their support systems. Families fulfilled all their needs and boosted their morale to overcome challenges. Furthermore, other support was received from health-care professionals, including pre-emptive information and health education on chemotherapy, encouragement to face chemotherapy bravely and with a positive attitude and the provision of regular physical care and emotional support. Finally, any source that improved mental energy might be considered a support system, such as encouragement from friends, shared experiences with other patients and spiritual comfort from religion.
Synthesized finding 3: they engaged in numerous types of coping strategies to deal with side effects and adapt to this difficult journey
Coping strategies often vary from person to person and evolve during chemotherapy. The coping strategies used depend on the patient’s personal coping style or nature, personal symptom experience, the need to control symptoms, the way they deal with challenges, how their life was affected by chemotherapy, their knowledge and beliefs, the way they manage their symptoms and their personal goals and different cultural backgrounds. Twenty-eight findings extracted from six studies indicated that women with breast cancer engaged in effective coping strategies to deal with chemotherapy. According to Lazarus’ Stress Adaptation Theory, coping is the cognitive and behavioural effort to understand, minimize or endure the inner and outer demands that develop as a result of stressful situations. This synthesized finding included three categories: problem-focussed coping strategies, behavioural coping strategies and emotion-focussed coping strategies. These strategies aimed to reduce distress and increase optimal coping strategies in women with breast cancer undergoing chemotherapy (Table 4 and Online Appendix 1).
Problem-focussed coping strategies
Twelve of the extracted findings from five studies indicated that many women with breast cancer engaged in problem-focussed coping strategies to control and address problems related to the side effects of chemotherapy [32,33,34,35]. The process may include identifying distressful events, making assessments, finding solutions and solving problems related to a particular scenario. During the chemotherapy process, the women identified strategies to prevent, manage, or eliminate side effects. For example, they adjusted their diet and monitored their nutrition and food intake to solve appetite problems.
Behavioural coping strategies
Seven of the extracted findings from six studies identified that behavioural coping strategies were an important part of coping strategies [15, 16, 28, 32, 35]. Behavioural coping strategies aimed to ensure that their mind remained sharp, mobilize them to cope with side effects, and maintain a normal life during the chemotherapy process. First, the abilities to maintain hope and bravely fight the disease helped them accept chemotherapy. Second, religion was an effective self-care strategy to boost physiological, emotional, social, or spiritual well-being in some cultures. Third, women tried to maintain their usual roles, such as a wife, mother and employee.
Emotion-focussed coping strategies
Emotion-focussed coping strategies are effective coping strategies aiming to reduce distress and minimize psychological discomfort from chemotherapy. Eleven of the extracted findings from seven studies showed that women with breast cancer described various emotion-focussed coping strategies during chemotherapy, including crying to release all heavy burdens, focusing on the positive, accepting reality, maintaining a sense of humour, being hopeful and faithful, trying to think less, denial, diverting attention to another thing and concealing their feelings, among others [14, 16, 28, 30, 31, 33, 34]. In addition, as the adverse effects of chemotherapy gradually subsided, the patients began to make an effort to maintain a normal and peaceful life, such as understanding the value of health, enjoying their life, planning for the future and going back to work.
Proposed model: patients’ experience of chemotherapy
The proposed model reveals the themes and subthemes arising from the thematic synthesis, as presented in Table 4. The themes that describe the nature of women’s experiences during chemotherapy and how these themes are related are shown in Fig. 2. These themes will be elaborated in more detail in the discussion.
Discussion
This study developed three synthesized findings reflecting the experience and coping strategies of women with breast cancer undergoing chemotherapy. The synthesized findings provide further evidence on the experience of side effects during chemotherapy, coping strategies to address these adverse effects and the need for information and social support to cope with distressful events.
Experience of women with breast cancer receiving chemotherapy
The first synthesized statement more generally overlapped with the stressful experiences of women with breast cancer receiving chemotherapy. The personal symptom experience was complex and dynamic, and each patient experienced different symptoms daily during the new treatment cycle. However, we identified some common symptoms based on our research. In our review, the common physical symptoms were fatigue, cognitive changes, hair loss, nausea, vomiting, insomnia, bone pain and peripheral neuropathy, which were slightly different from common side effects reported in a previous study conducted in a Southeast Asian setting [36]. In that study, the five most prevalent physical symptoms were fatigue, dry mouth, hair loss, drowsiness and a lack of appetite, and the most distressing symptoms were fatigue, loss of appetite and changes in food taste. However, the differences in the two results may be attributed to the analysis of patients from two countries with different stages of the disease, receiving different types of chemotherapy and different ages. A symptom has a range of physical, psychological, family and social effects. Thus, women with breast cancer may experience a series of physical symptoms resulting from chemotherapy. Any symptom may exert multidimensional effects; namely, a physical manifestation of side effects from chemotherapy may exert profound effects on other aspects of health. In addition, the impact of physical symptoms on daily life is not merely determined by the characteristics of the individual and their beliefs, knowledge and expectations of chemotherapy but also by their identity, roles in family and social networks, future perspectives and the support received in this phase [37].
The second synthesized statement showed that a support network is essential for women to better cope with chemotherapy. In this review, the most important types of support were information and social support. In addition, social support is a type of practical support provided by family, friends, health-care professionals, or anyone in society that makes the individual feel safe and loved. Social support plays an important part in decision-making and survival/coping strategies, which exerts beneficial effects on social well-being and the quality of life in stressful situations [38, 39]. These findings are consistent with previous studies reporting that patients who undergo chemotherapy tend to emphasize common interpersonal stressors (e.g. providing and caring for family, and distance from family) and social/structural stressors (e.g. economic problems, and lack of information) [40].
Coping strategies are stated to be effective if they lead to good adaptation and a new pattern of life, while ineffective strategies may lead to health problems. In the present study, problem-focussed coping strategies, behavioural coping strategies and emotion-focussed coping strategies were effective strategies that reduced the severity of symptom-related distress and enabled the patients to gain control of their lives [41,42,43]. Problem-focussed coping strategies aim to analyse and explore the causes of stressful events, seek relevant information and social support, eliminate or solve problems, set goals and change personal expectations. Emotion-focussed coping strategy responses are not aimed at solving problems directly but at changing a person’s thoughts, such as crying, denial, acceptance, hopeful thinking, a sense of humour, attention diversion and avoidance. Behavioural coping strategies, such as remaining hopeful, understanding and following the instructions for self-care, always checking in with themselves to ensure good health and trying to maintain one’s normal role in life, are strategies that may improve patient quality of life and help them cope with adverse symptoms [44].
The link between experience of chemotherapy and coping strategies
This systematic review has highlighted the link between the chemotherapy experience and coping strategies (see Fig. 2). Chemotherapy is an external stressor for women with breast cancer, which leads to various physiological and psychological side effects (fear, stress, anxiety, and depression). This stress motivates individuals to seek coping strategies that will prevent further psychological disorders and maintain psychological well-being. This finding is consistent with the views of previous studies [41, 43, 45]. A quantitative study by Sari [41] showed that adequate social support and effective coping strategies significantly reduce the symptom-related distress of patients undergoing chemotherapy. In addition, another study by Chirico [46] found an inverse relationship between self-efficacy for coping and distress from chemotherapy and a positive relationship between self-efficacy for coping and quality of life.
Moreover, we found that the results of this review matched the Contextual Model of Lazarus’ Stress and Coping Theory, which was helpful in describing and organizing the results. This theory is a system for assessing the process of coping with stressful experiences. Stressful encounters are interpreted as individual-environment transactions, which depend on the impact of the external stressor [47, 48]. All individuals have resources and skills known as coping mechanisms that are used to relieve stress. Anything that causes stress endangers life, unless it is met by adequate adaptive responses; conversely, anything that endangers life causes stress and adaptive responses [49]. The application of this theory would allow nurse practitioners to include a plan to relieve patient stress and to incorporate this plan into short-term goals with the aim of ensuring safety. The ability of patients to successfully complete chemotherapy depends on their coping skills, which will decrease stressors and allow the patient to move towards a more positive outlook and lifestyle.
Implications for practice
The synthesized findings from this meta-aggregation the Lazarus stress and coping theory provide some clear recommendations for intervention development and practice for patients to cope with chemotherapy. First, health-care professionals must scientifically and systematically assess real supportive care needs for woman with breast cancer undergoing chemotherapy and proactively provide specific information about the disease prognosis, chemotherapy regimen and potential side effects. Second, information support system and social support groups integrated in the routine procedures offered by nurses and other health-care providers should be established. For example, continuity of care by breast cancer nurses is needed throughout the duration of chemotherapy. Third, the development of pre-chemotherapy care programmes that include specific and focussed preparatory material to reduce the treatment distress level and increase adaptive coping are needed.
Strengths and limitations of the study
This systematic review and meta-aggregation of qualitative studies is the first to describe the experience and coping strategies of women with breast cancer undergoing chemotherapy. This study developed a comprehensive search strategy and an explicit and clearly reported quality assessment of the included studies and data extraction and synthesis process. The studies included in this review were conducted in eight countries, and these international studies make the results more convincing. In addition, the meta-aggregation also provides valuable insights into the work of nursing researchers and nursing administrators in related areas and identifies many potential areas for the development of further interventions and future research.
However, there are some limitations that should also be noted: First, because of the language limitations, a number of high-quality non-English studies might have been missed. Second, the systematic review protocol used in this study was not registered in Prospero prior to the study. Third, meta-aggregation is an interpretative process in which different teams studying the literature may produce different interpretations. Fourth, the experiences and coping strategies among women of different races and cultures, treated with different chemotherapy regimens and with stages of breast cancer may vary, but we were unable to conduct the analysis separately in this review because of the failure to obtain complete related data from most of the original studies. Therefore, the results from this study are relevant for some but not all patients.
Conclusions
This review is among the first to synthesize the literature of the experience and coping strategies of women with breast cancer undergoing chemotherapy based on the Contextual Model of Lazarus’ Stress and Coping Theory. According to the existing literature, we concluded that when women experienced various stressful side effects, supportive care to address needs and effective coping strategies are essential to help them adapt to this difficult journey. We recognized the need to develop pre-chemotherapy care programmes, information support systems, social support groups and individual effective coping strategies to reduce chemotherapy-related distress levels and enhance self-care at home.
Data availability
Data sharing is not applicable to this article, as no datasets were generated or analysed during the current study.
Abbreviations
- JBI-QARI:
-
Johanna Briggs Institute Qualitative Assessment and Review Instrument
- JBI-SUMARI:
-
Joanna Briggs Institute System for the Unified Management Assessment and Review of Information
References
Bray, F., Ferlay, J., Soerjomataram, I., Siegel, R. L., Torre, L. A., & Jemal, A. (2018). Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA-Cancer J Clin., 68, 394–424.
Plevritis, S. K., Munoz, D., Kurian, A. W., Stout, N. K., Alagoz, O., Near, A. M., et al. (2018). Association of Screening and Treatment With Breast Cancer Mortality by Molecular Subtype in US Women, 2000–2012. JAMA, 319(2), 154.
Zielonke, N., Gini, A., Jansen, E., Anttila, A., Segnan, N., Ponti, A., et al. (2020). Evidence for reducing cancer-specific mortality due to screening for breast cancer in Europe: A systematic review. European Journal of Cancer, 127, 191–206.
Montazeri, A. (2008). Health-related quality of life in breast cancer patients: a bibliographic review of the literature from 1974 to 2007. J Exp Clin Cancer Res., 27(1), 32.
Harbeck, N., & Gnant, M. (2017). Breast cancer. Lancet, 389(10074), 1134–1150.
Waks, A. G., & Winer, E. P. (2019). Breast Cancer Treatment: A Review. JAMA, 321(3), 288–300.
Peto, R., Davies, C., Godwin, J., Gray, R., Pan, H. C., Clarke, M., et al. (2012). Comparisons between different polychemotherapy regimens for early breast cancer: meta-analyses of long-term outcome among 100,000 women in 123 randomised trials. Lancet, 379(9814), 432–444.
Marino, J. L., Saunders, C. M., Emery, L. I., Green, H., Doherty, D. A., & Hickey, M. (2016). How does adjuvant chemotherapy affect menopausal symptoms, sexual function, and quality of life after breast cancer? Menopause., 23(9), 1000–1008.
Tao, J. J., Visvanathan, K., & Wolff, A. C. (2015). Long term side effects of adjuvant chemotherapy in patients with early breast cancer. The Breast., 24, S149–S153.
Neugut, A. I., Hillyer, G. C., Kushi, L. H., Lamerato, L., Buono, D. L., Nathanson, S. D., et al. (2016). A prospective cohort study of early discontinuation of adjuvant chemotherapy in women with breast cancer: the breast cancer quality of care study (BQUAL). Breast Cancer Res Tr., 158(1), 127–138.
Quinten, C., Kenis, C., Hamaker, M., Coolbrandt, A., Brouwers, B., Dal Lago, L., et al. (2018). The effect of adjuvant chemotherapy on symptom burden and quality of life over time; a preliminary prospective observational study using individual data of patients aged ≥70 with early stage invasive breast cancer. J Geriatr Oncol., 9(2), 152–162.
Sultan, A., Choudhary, V., & Parganiha, A. (2017). Worsening of rest-activity circadian rhythm and quality of life in female breast cancer patients along progression of chemotherapy cycles. Chronobiology International, 34(5), 609–623.
Sawatsky, A. P., Ratelle, J. T., & Beckman, T. J. (2019). Qualitative Research Methods in Medical Education. Anesthesiology, 131(1), 14–22.
Banning, M., Hafeez, H., Faisal, S., Hassan, M., & Zafar, A. (2009). The impact of culture and sociological and psychological issues on Muslim patients with breast cancer in Pakistan. Cancer Nursing, 32(4), 317–324.
Beaver, K., Williamson, S., & Briggs, J. (2016). Exploring patient experiences of neo-adjuvant chemotherapy for breast cancer. Eur J Oncol Nurs., 20, 77–86.
Chen, Y., Huang, H., Kao, C., Sun, C., Chiang, C., & Sun, F. (2016). The Psychological Process of Breast Cancer Patients Receiving Initial Chemotherapy. Cancer Nursing, 39(6), E36–E44.
Nizamli, F., Anoosheh, M., & Mohammadi, E. (2011). Experiences of Syrian women with breast cancer regarding chemotherapy: A qualitative study. Nurs Health Sci., 13(4), 481–487.
Florczak, K. L. (2018). Meta-Aggregation: Just What Is It? Nurs Sci Quart., 32(1), 11.
Hannes, K., & Lockwood, C. (2011). Pragmatism as the philosophical foundation for the Joanna Briggs meta-aggregative approach to qualitative evidence synthesis. Journal of Advanced Nursing, 67(7), 1632–1642.
Lockwood, C., Munn, Z., & Porritt, K. (2015). Qualitative research synthesis: methodological guidance for systematic reviewers utilizing meta-aggregation. Int J Evid Based Healthc., 13(3), 179–187.
Zuzelo, P. (2007). Evidence-based nursing and qualitative research: A partnership imperative for real-world practice. Nursing Research: A Qualitative Perspective., 13, 481–499.
Tanay, M. A. L., Armes, J., & Ream, E. (2017). The experience of chemotherapy-induced peripheral neuropathy in adult cancer patients: a qualitative thematic synthesis. Eur J Cancer Care., 26(5), e12443.
Johnson, M. (2012). Chemotherapy treatment decision making by professionals and older patients with cancer: a narrative review of the literature. Eur J Cancer Care., 21(1), 3–9.
Dowling, M., Hunter, A., Biesty, L., Meskell, P., Conway, A., O’Boyle, G., et al. (2019). Driving and Disabling Factors of Noncurative Oral Chemotherapy Adherence: A Qualitative Evidence Synthesis. Oncology Nursing Forum, 46(1), 16–28.
Howard, A. F., Balneaves, L. G., & Bottorff, J. L. (2007). Ethnocultural women’s experiences of breast cancer: a qualitative meta-study. Cancer Nursing, 30(4), E27–E35.
Manning, N., & Gyi, A. A. (2008). Experience of informal caregivers looking after people receiving chemotherapy to treat lung cancer: A systematic review. JBI Libr Syst Rev., 6(17 Suppl), 1–10.
Munn, Z., Porritt, K., Lockwood, C., Aromataris, E., & Pearson, A. (2014). Establishing confidence in the output of qualitative research synthesis: the ConQual approach. BMC Medical Research Methodology, 14, 108.
Anarado, A. N., Ezeome, E. R., Ofi, O. B., Nwaneri, A. C., & Ogbolu, Y. (2017). Experiences and desired nursing assistance of women on out-patient breast cancer chemotherapy in Southeastern Nigeria. Psycho-Oncology., 26(3), 385–391.
Boehmke, M. M., & Dickerson, S. S. (2005). Symptom, symptom experiences, and symptom distress encountered by women with breast cancer undergoing current treatment modalities. Cancer Nursing, 28(5), 382–389.
Browall, M., Gaston-Johansson, F., & Danielson, E. (2006). Postmenopausal women with breast cancer: their experiences of the chemotherapy treatment period. Cancer Nursing, 29(1), 34–42.
Cebeci, F., Yangin, H. B., & Tekeli, A. (2012). Life experiences of women with breast cancer in south western Turkey: a qualitative study. Eur J Oncol Nurs., 16(4), 406–412.
Cowley, L., Heyman, B., Stanton, M., & Milner, S. J. (2000). How women receiving adjuvant chemotherapy for breast cancer cope with their treatment: a risk management perspective. Journal of Advanced Nursing, 31(2), 314–321.
Gunusen, N. P., Inan, F. S., & Ustun, B. (2013). Experiences of Turkish Women with Breast Cancer During the Treatment Process and Facilitating Coping Factors. Asian Pacific Journal of Cancer Prevention, 14(5), 3143–3149.
Kanaskie, M. L., & Loeb, S. J. (2015). The experience of cognitive change in women with breast cancer following chemotherapy. Journal of Cancer Survivorship, 9(3), 375–387.
Lai, X. B., Ching, S. S. Y., & Wong, F. K. Y. (2017). A qualitative exploration of the experiences of patients with breast cancer receiving outpatient-based chemotherapy. Journal of Advanced Nursing, 73(10), 2339–2350.
Thiagarajan, M., Chan, C. M., Fuang, H. G., Beng, T. S., Atiliyana, M. A., & Yahaya, N. A. (2016). Symptom Prevalence and Related Distress in Cancer Patients Undergoing Chemotherapy. Asian Pacific Journal of Cancer Prevention, 17(1), 171–176.
Coolbrandt, A., Casterlé, B. D., Wildiers, H., Aertgeerts, B., Elst, E. V. D., van Achterberg, T., & Milisen, K. (2016). Dealing with chemotherapy-related symptoms at home: a qualitative study in adult patients with cancer. Eur J Cancer Care., 25(1), 79–92.
Gaston-Johansson, F., Haisfield-Wolfe, M. E., Reddick, B., Goldstein, N., & Lawal, T. A. (2013). The relationships among coping strategies, religious coping, and spirituality in African American women with breast cancer receiving chemotherapy. Oncology Nursing Forum, 40(2), 120–131.
Genc, F., & Tan, M. (2011). Symptoms of patients with lung cancer undergoing chemotherapy and coping strategies. Cancer Nursing, 34(6), 503–509.
Tan, M. (2007). Social support and coping in Turkish patients with cancer. Cancer Nursing, 30(6), 498–504.
Sari, D. K., Dewi, R., & Daulay, W. (2019). Association Between Family Support, Coping Strategies and Anxiety in Cancer Patients Undergoing Chemotherapy at General Hospital in Medan, North Sumatera. Indonesia. Asian Pac J Cancer Prev., 20(10), 3015–3019.
Muusses, L. D., Weert, J. C. M., Dulmen, S., & Jansen, J. (2012). Chemotherapy and information-seeking behaviour: characteristics of patients using mass-media information sources. Psycho-Oncology., 21(9), 993–1002.
Yahaya, N. A., Subramanian, P., Bustam, A. Z., & Taib, N. A. (2015). Symptom experiences and coping strategies among multi- ethnic solid tumor patients undergoing chemotherapy in Malaysia. Asian Pacific Journal of Cancer Prevention, 16(2), 723–730.
Martinez, T. D., Jacobsen, P., & Meade, C. D. (2016). Understanding the Stress Management Needs and Preferences of Latinas Undergoing Chemotherapy. Journal of Cancer Education, 31(4), 633–639.
Thiagarajan, M., Chan, C. M. H., Fuang, H. G., Beng, T. S., Atiliyana, M. A., & Yahaya, N. A. (2016). Symptom Prevalence and Related Distress in Cancer Patients Undergoing Chemotherapy. Asian Pacific Journal of Cancer Prevention., 17(1), 171–176.
Chirico, A., Lucidi, F., Merluzzi, T., Alivernini, F., Laurentiis, M., Botti, G., & Giordano, A. (2017). A meta-analytic review of the relationship of cancer coping self-efficacy with distress and quality of life. Oncotarget., 8(22), 36800–36811.
Biggs, A., Brough, P., & Drummond, S. (2017). Lazarus and Folkman’s psychological stress and coping theory. The handbook of stress and health: A guide to research and practice (pp. 351–364). Chickster, UK: Wiley-Blackwell.
Lazarus, R. S. (1974). Psychological Stress and Coping in Adaptation and Illness. Int J Psychiat Med., 5(4), 321–333.
Lazarus, R., & Folkman, S. (1984). Stress Appraisal and Coping. New York: Springer Publishing Company.
Funding
This study was funded by Guangdong Medical Research Foundation (CN). The Grant Number is A2018090. The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declared that there is no conflict of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Liu, L., Wu, Y., Cong, W. et al. Experience of women with breast cancer undergoing chemotherapy: a systematic review of qualitative research. Qual Life Res 30, 1249–1265 (2021). https://doi.org/10.1007/s11136-020-02754-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-020-02754-5