Abstract
Purpose
Gastrointestinal (GI) symptoms pose a significant burden to patients receiving chemoradiation therapy (CRT) for anal cancer; however, the impact of symptoms from the patient perspective has not been quantified. This retrospective study examined and compared patient and clinician reports of acute GI toxicity during CRT.
Materials and methods
Patients treated with definitive RT using intensity-modulated radiation therapy for anal cancer between 9/09 and 11/12 were reviewed. Median RT dose was 56 Gy (range 45–56), and 76 patients (97%) received concurrent 5-fluorouracil-based chemotherapy. During RT, patients completed the 7-item Bowel Problem Scale (BPS) weekly. Clinicians assessed toxicity separately using CTCAE v. 3.0. Scores of BPS ≥ 3 and CTCAE ≥ 1 were considered to be clinically meaningful. Agreement of the two assessments was evaluated by Cohen’s kappa coefficient.
Results
Seventy-eight patients completed at least one BPS and had a corresponding clinician assessment. Patients reporting scores of ≥3 was highest at week 5 (n = 68) for diarrhea (44.1%), proctitis (57.4%), and mucus (48.4%), while urgency (47.6%), tenesmus (31.7%), and cramping (27%) were highest at week 4 (n = 63). Baseline bleeding scores (26.7%; score ≥3) improved during treatment (13.4% at week 5). “Poor” agreement was observed between patient- and clinician-reported proctitis (Cohen’s k = 0.11; n = 58); however, there was “good” agreement for diarrhea (Cohen’s k = 0.68; n = 58).
Conclusions
Acute GI toxicity during definitive CRT for anal cancer was most significant during weeks 4–5, while rectal bleeding improved during treatment. Discrepancies in patient- and clinician-reported symptoms demonstrate the potential for patient-reported outcomes to be useful tools for anal cancer clinical assessments.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Definitive radiation therapy (RT) with concurrent 5-fluorouracil (5-FU)-based chemotherapy is the current standard of care in treatment of anal carcinomas. Although chemoradiation therapy has demonstrated good local control with preservation of sphincter and bowel function, it is also associated with a high rate of acute treatment-related toxicities [1,2,3]. With the use of intensity-modulated radiation therapy (IMRT), when compared to conventional techniques, reductions of radiation doses to normal tissue have helped to reduce acute toxicity [4]. However, toxicity still poses a significant burden to patients receiving IMRT for anal cancer and the extent of symptoms from the patient perspective has not been quantified.
Patient-reported outcomes (PROs) have become an important tool in capturing and measuring patient health concepts and determining the extent of symptoms. The field is quickly evolving, with the National Cancer Institute recently designating PRO measures in clinical trials to further assist in documentation of adverse event reporting [5]. This reflects the increasing importance associated with incorporating the patient’s voice during treatment. Collection of PROs may contribute to improved communication between patients and physicians, which could enhance patient quality of life, improve patient management, and assist in early detection of adverse events [6,7,8,9].
Utilizing PROs integrated in clinical practice, this retrospective study examined their agreement with clinician-reported symptoms and also analyzed the trajectory of patient-reported symptoms and clinician reports of acute GI toxicity during chemoradiation therapy for anal cancer.
Materials and methods
Patients and radiation therapy
After obtaining a waiver of authorization from the Institutional Review Board, the medical records of patients treated with definitive RT using IMRT for anal cancer from September 2009 through November 2012 at Memorial Sloan Kettering Cancer Center (MSKCC) were reviewed. Patients were included in the analysis if they had completed at least one bowel problem scale (BPS) questionnaire and had a corresponding physician toxicity assessment to be included in this study. All patients had either a confirmed diagnosis of squamous cell carcinoma (94%) or adenocarcinoma (6%) and nearly all patients (97%) received concurrent 5-FU-based chemotherapy with or without mitomycin C (Table 1).
Patients were simulated in the prone position and immobilized in a thermoplastic body mold on a PET-CT simulator (GE Discovery ST, GE Healthcare, Waukesha, WI) to obtain fused PET images with the treatment-planning CT scan. Oral contrast (Gastroview) and intravenous contrast was administered to delineate the small bowel and blood vessels. Information from the clinical examination, pretreatment diagnostic imaging, and PET scan was combined to delineate the gross tumor volume (GTV). If inguinal or pelvic nodes were clinically or radiographically involved, these were identified as separate GTVs. The clinical target volume (CTV) consisted of the GTV with 1- to 1.5-cm margin and the draining lymph nodes as designated by the RTOG anorectal atlas [10]. The CTVA was contoured to include the mesorectal, internal iliac, and superior hemorrhoidal lymph node regions. The CTVB included the external iliac lymph nodes and the CTVC was delineated to include the inguinal nodal basins. A planning target volume (PTV) margin of 5 mm was created around the CTVA + B + C.
All patients were treated with IMRT, which was delivered over 5–6 weeks, 1.8–2 Gy five times a week. IMRT treatment planning was performed using custom in-house software. Radiation dose was stage dependent. Clinically uninvolved pelvic and inguinal nodes were treated to 45 Gy at 1.8 Gy per fraction. For T1 tumors, the primary tumor dose was brought to 50 Gy in 2 Gy fractions using an integrated boost. For tumors ≥2 cm, an additional 6 Gy in three fractions was added as a sequential boost to bring the primary tumor and any >2 cm nodes to 56 Gy. The median dose was 56 Gy (range 45–56). 75% of patients received a boost to primary nodes. Normal tissue structures of interest in IMRT planning were routinely contoured on each CT slice [10]. We attempted to use the following constraints for normal tissue doses: 95% of the small bowel to receive <45 Gy; mean bladder dose 30–33 Gy; maximum dose to the femoral head 50 Gy; and maximum dose to cauda equina <50 Gy. Treatment was delivered using mixed 6 and 15 MV energies and a median of 7 coplanar beams.
Chemotherapy
The majority of patients (97%) received concurrent 5-FU-based chemotherapy; 52 pts (67%) of patients received a combination of mitomycin (10 mg/m2) and 5-FU (1000 mg/m2 over 96 h), 13 pts (17%) received a combination of mitomycin and capecitabine (875 mg/m2 BID daily M-F), 5 pts (6%) received 5-FU alone, and 6 pts (8%) received capecitabine alone. Two patients (3%) did not receive concurrent chemotherapy.
Five patients (6%) also received induction chemotherapy prior to concurrent chemoradiation therapy, with three patients receiving a combination of cisplatin and 5-FU and two patients receiving folinic acid, 5-FU, and oxaliplatin (FOLFOX).
Assessment of toxicity
Patients were followed up weekly in clinic to assess toxicities and to complete the 7-item Bowel Problem Scale (BPS) [11]. Patients were given the BPS form by a nurse prior to the clinician’s assessment. Clinicians assessed symptoms separately using a standardized assessment form during weekly clinic visits, which documented symptoms including fatigue, nausea, vomiting, diarrhea, dermatitis, mucositis, cystitis, and proctitis. These toxicities were graded using common terminology for clinical adverse events (CTCAE) version 3.0 [12]. All patients in the study except for one were treated and assessed by the same physician, reducing any interobserver variability in patient assessments.
The BPS questionnaire, which was developed by Clark and Talcott, has been validated and used in prior studies for prostate cancer patients receiving radiation therapy and in rectal cancer patients receiving 5-FU-based chemoradiation [13, 14]. The questionnaire contains questions about symptoms that reflect some of the toxicities assessed in the clinician’s assessment and asks patients to report the frequency of diarrhea, urgency, pain, bleeding, cramping, mucus, and tenesmus on a 5-point Likert-type scale ranging from 1, “not at all,” to 5, “very frequently” (≥3 times/day).
Analysis
Clinician-reported symptoms assessed weekly using a standardized acute toxicity assessment and graded using CTCAE version 3.0 were collected into a gastrointestinal database. Toxicities with a grade 1 or more were considered clinically meaningful and prevalent. The proportion of patients reporting symptoms, those with grade 1 or more, were indicated at each week and their prevalence was plotted over the course of treatment. This allowed the trajectory of symptom prevalence to be demonstrated.
The prevalence of symptoms experienced at each weekly status check was compared to patient-reported symptoms. A symptom score ≥3 on the BPS indicated that a symptom was expressed “fairly frequently” (3–4 times/week) to “very frequently” (≥3 times/day) and indicated prevalence. Clinician CTCAE assessment scores of grades ≥1 indicated that there was a mild adverse reaction and thus the symptom was considered prevalent. Thus, scores of BPS ≥ 3 and CTCAE ≥ 1 were considered to be clinically meaningful. Agreement of the two assessments was evaluated by Cohen’s kappa coefficient.
Symptoms of diarrhea and proctitis were the only symptoms which were assessed by both patient and clinician. All other symptoms, such as cramping, urgency, and tenesmus, assessed by the patient were not symptoms included on the standardized acute toxicity assessment used by the physician. Thus, these symptoms had no comparable corresponding clinician assessment. The agreement of patient reporting and clinician assessment of diarrhea and proctitis (present or not present) at week 5 was evaluated by Cohen’s kappa coefficient [15]. Kappa values of 0.6–0.8 suggested good agreement and kappa values of less than 0.2 demonstrated poor agreement, per the guidelines of Landis and Koch [16].
Results
Patient characteristics
Between September 2009 and November 2012, seventy-eight patients were identified who had completed at least one BPS and had a corresponding clinician toxicity assessment. The median age was 59 years (range 36–95). As reflected in the incidence of the disease, a majority (74%) of patients were female. Most patients presented with either stage II (23%) or stage III (60%) disease. Karnofsky Performance Status Scale (KPS) was assessed at baseline. This scale assigns scores from 0 to 100 and correlates to the patient’s level of physical functioning. 100 indicates that the patient is fully active and able to function at a normal level [17]. At baseline, 68% of patients had a KPS of 90, with 24% of patients with a KPS of 80 (Table 1). All patients treated definitively had a KPS ≥ 70. Less than a third of patients required treatment breaks (29%).
Completion of questionnaires
Patients were treated with radiation over 5–6 weeks, and thus had the opportunity to complete a maximum of 5–6 questionnaires with a corresponding physician assessment. Completion of at least one BPS questionnaire with a corresponding physician assessment was required for inclusion in this analysis. This inclusion criterion was used by a previous study assessing patient-reported outcomes for rectal cancer [14].
Prior longitudinal patient-reported outcome studies for rectal cancer therapy have defined a “participant” as having completed at least four or more assessments [13, 14]. In our cohort of seventy-eight patients, we had a relatively high completion rate. A majority, 74% of patients, completed at least four assessments, demonstrating that implementation of the questionnaire in clinic appeared feasible, with no significant burden to patients.
Trajectory of clinician-reported toxicity
Figure 1 illustrates the trajectory of non-hematologic toxicity as assessed by clinicians. Sharp increases in clinician-reported prevalence of symptoms appeared between week 1 (n = 70) and week 2 (n = 70) for symptoms of nausea (5.7–22.9%), diarrhea (14–45%), oral mucositis (0–37.1%), and fatigue (8.6–40%).
The number of patients reporting fatigue appeared to gradually progress over treatment with a vast majority of patients (85.4%) reporting fatigue by the end of treatment. A similar trajectory was seen with symptoms of dermatitis, which appeared prevalent in a majority of patients with 82% of patients reporting symptoms at week 5 (n = 66).
Gradual progression of symptoms occurred with cystitis and proctitis. In symptoms of cystitis, almost a fifth of patients (18.2%) reported symptoms by the end of treatment and nearly half (45.5%) of patients reporting symptoms of proctitis by treatment end.
Symptoms of nausea and vomiting appeared to increase in prevalence by week 2 with 22.9% reporting nausea and 5.7% reporting vomiting. Symptoms seemed to gradually improve halfway through treatment, with 9.9% reporting nausea and 1.4% reporting vomiting at week 4 (n = 71). However, a late progression appeared toward the end of treatment with 25.5% reporting nausea and 9.1% reporting vomiting by treatment end.
Other symptoms demonstrated gradual decreases or plateaus in prevalence of clinician-reported symptoms. Reported symptoms of oral mucositis increased at week 2 (37.1%) but its prevalence gradually decreased over the course of treatment with 11.1% of patients reporting symptoms by treatment end. Over half of patients (53.6%) reported diarrhea symptoms by week 3 (n = 69), and this percentage remained relatively stable until the end of treatment with 54.5% reporting symptoms of diarrhea by week 6 (n = 54).
Trajectory of patient-reported toxicity
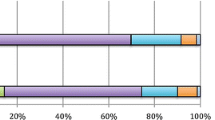
Figure 2 illustrates the trajectory of acute toxicity as reported by patients. The proportion of patients reporting scores of ≥3 was highest at week 5 (n = 68) for diarrhea (44.1%), proctitis (57.4%), and mucus (48.4%). Prevalence of diarrhea and mucus appeared to sharply increase from weeks 4 through 5. Urgency (47.6%), tenesmus (31.7%), and cramping (27%) were highest at week 4 (n = 63) with a gradual decrease in prevalence of symptoms illustrated toward the end of treatment. Bleeding scores were higher at baseline (26.7%; score ≥3), and appeared to improve over the course of treatment (13.4% at week 5).
Agreement of patient and clinician assessment
Patient versus clinician-reported symptoms varied for diarrhea and proctitis, with patients more likely to report prevalence of symptoms than clinicians (Figs. 3, 4). The estimated agreement demonstrated “good” agreement between patient- and clinician-reported diarrhea (Cohen’s k = 0.68; n = 58). However, “poor” agreement was observed between patient- and clinician-reported proctitis (Cohen’s k = 0.11; n = 58) (Table 2). Eighty-six percent of completed patient assessments had a corresponding clinician assessment at week 5. Uncorrected agreement was 44.8 and 84.5%, respectively.
Discussion
Clinician reports demonstrate that symptoms of nausea, oral mucositis, fatigue, and diarrhea appear to sharply increase in prevalence within the first two weeks with the highest prevalence of symptoms by treatment end. The most prevalent clinician-reported symptoms were fatigue and dermatitis, with 85.4 and 82%, respectively, reporting symptoms by week 6. Patient-reported outcomes demonstrate a similar trajectory with acute GI symptoms being most significant during weeks 4–5. Anorectal pain was the most prevalent symptom by treatment end, with 61.4% reporting pain by week 6. Clinician-reported symptoms of oral mucositis and patient-reported symptoms of bleeding appeared to improve over the course of treatment. This decrease may be attributed to clinical intervention to manage the mucositis and tumor response to treatment.
While relatively “good” agreement was observed with patient- and clinician-reported symptoms of diarrhea, there appeared to be poor agreement with patient- and clinician-reported symptoms of proctitis. Discrepancies in patient- and clinician-reported symptoms of proctitis are consistent with studies in rectal cancer. In accordance with the study by Flores et al., it was also demonstrated that there was better observed agreement between clinician- and patient-reported diarrhea [14]. The discrepancy in reporting may be attributable to a number of factors. Previous studies evaluating adverse event reporting by clinicians in comparison to patients have shown that agreement tends to be higher for observable symptoms compared to non-observable symptoms, and that patients tend to report symptoms earlier and much more frequently than clinicians. It was suggested that the reason for this might be due to the fact that different criteria are considered based on the varying perspective of the individual assessing symptoms [6, 7]. The clinician report was more predictive of unfavorable clinical events, i.e., emergency department visits or death, while the patient report more closely reflected daily health status [7].
Others have confirmed that subjective symptoms are much more difficult to capture by clinicians, which contributes to a discrepancy [18, 19]. In addition, several studies have found disagreement on unobservable symptoms such as “nausea” and “pain” [18,19,20]. The BPS questionnaire was designed to capture the frequency of symptoms but does not assess severity, whereas the routine form used by clinicians assessed symptoms according to CTCAE version 3.0, which measures the severity of patient-reported events [12]. Although the response scales or rating scales for each were not directly comparable, patient reports of symptoms do provide information which is complementary to clinician grading. The BPS questionnaire was feasible for prospective use by clinicians and patients. This finding was consistent with other studies which found that the BPS questionnaire was not burdensome for patients and had a high rate of completion when administered in clinic [13, 14].
To our knowledge, this is the first study comparing patient-reported outcomes with physician reports throughout the course of treatment for anal cancer. Further, only one other study has evaluated patient-reported outcomes during IMRT for anal cancer [3]. The trajectory of symptoms identified in this study illustrates that acute GI toxicity during treatment was most significant during weeks 4–5, while rectal bleeding improved during treatment. This information is important for providing patients with accurate expectations and for identifying the need for symptom palliation. Patient-reported outcome data offer depth and further insight into the complex picture of patient symptoms and can be critical to understanding the impact of the disease throughout the course of treatment.
The methods and processes for incorporating patient-reported outcome assessments into clinical care are developing rapidly. A variety of platforms for internet-based assessment of patient-reported outcomes have been implemented at medical centers, and substantial guidance on the design of patient-reported outcome assessment for use in clinical care is available [21,22,23]. Current research is identifying optimal formats for presenting these data to clinicians, including how the data should be interpreted. In many disease areas, work is being conducted to identify scoring cutpoints (e.g., nausea greater than a score of x) where clinical intervention should be considered [24]. Further, approaches for integrating patient-reported outcome data collection into electronic health records are being developed to provide a centralized source of information for clinicians and to enhance patient care [25].
References
Devisetty, K., Mell, L. K., Salama, J. K., Schomas, D. A., Miller, R. C., Jani, A. B., et al. (2009). A multi-institutional acute gastrointestinal toxicity analysis of anal cancer patients treated with concurrent intensity-modulated radiation therapy (IMRT) and chemotherapy. Radiotherapy and Oncology, 93(2), 298–301.
Kachnic, L. A., Tsai, H. K., Coen, J. J., Blaszkowsky, L. S., Hartshorn, K., Kwak, E. L., et al. (2012). Dose-painted intensity-modulated radiation therapy for anal cancer: A multi-institutional report of acute toxicity and response to therapy. International Journal of Radiation Oncology Biology Physics, 82(1), 153–158.
Han, K., Cummings, B. J., Lindsay, P., Skliarenko, J., Craig, T., Le, L. W., et al. (2014). Prospective evaluation of acute toxicity and quality of life after IMRT and concurrent chemotherapy for anal canal and perianal cancer. International Journal of Radiation Oncology Biology Physics, 90(3), 587–594.
Bazan, J. G., Hara, W., Hsu, A., Kunz, P. A., Ford, J., Fisher, G. A., et al. (2011). Intensity-modulated radiation therapy versus conventional radiation therapy for squamous cell carcinoma of the anal canal. Cancer, 117(15), 3342–3351.
Quinten, C., Maringwa, J., Gotay, C. C., Martinelli, F., Coens, C., Reeve, B. B., et al. (2011). Patient self-reports of symptoms and clinician ratings as predictors of overall cancer survival. Journal of the National Cancer Institute, 103(24), 1851–1858.
Basch, E., Iasonos, A., McDonough, T., Barz, A., Culkin, A., Kris, M. G., et al. (2006). Patient versus clinician symptom reporting using the National Cancer Institute common terminology criteria for adverse events: Results of a questionnaire-based study. Lancet Oncology, 7(11), 903–909.
Basch, E., Jia, X., Heller, G., Barz, A., Sit, L., Fruscione, M., et al. (2009). Adverse symptom event reporting by patients versus clinicians: Relationships with clinical outcomes. Journal of the National Cancer Institute, 101(23), 1624–1632.
Basch, E. (2010). The missing voice of patients in drug-safety reporting. New England Journal of Medicine, 362(10), 865–869.
Trotti, A., Colevas, A. D., Setser, A., & Basch, E. (2007). Patient-reported outcomes and the evolution of adverse event reporting in oncology. Journal of Clinical Oncology, 25(32), 5121–5127.
Myerson, R. J., Garofalo, M. C., El Naqa, I., Abrams, R. A., Apte, A., Bosch, W. R., et al. (2009). Elective clinical target volumes for conformal therapy in anorectal cancer: a radiation therapy oncology group consensus panel contouring atlas. International Journal of Radiation Oncology Biology Physics., 74(3), 824–830.
Clark, J. A., & Talcott, J. A. (2001). Symptom indexes to assess outcomes of treatment for early prostate cancer. Medical Care, 39(10), 1118–1130.
National Cancer Institute (NCI) Cancer therapy program, common terminology criteria for adverse events, Version 3.0. August 9, 2006. Retrieved October 20, 2014, from http://ctep.cancer.gov/protocolDevelopment/electronic_applications/docs/ctcaev3.pdf
Chen, R. C., Mamon, H. J., Chen, Y. H., Gelman, R. S., Suh, W. W., Talcott, J. A., et al. (2010). Patient-reported acute gastrointestinal symptoms during concurrent chemoradiation treatment for rectal cancer. Cancer, 116(8), 1879–1886.
Flores, L. T., Bennett, A. V., Law, E. B., Hajj, C., Griffith, M. P., & Goodman, K. A. (2012). Patient-reported outcomes versus clinician symptom reporting during chemoradiation for rectal cancer. Gastrointestinal Cancer Research., 5(4), 119–124.
Cohen, Jacob. (1960). A coefficient of agreement for nominal scales. Educational and Psychological Measurement, 20(1), 37–46.
Landis, J. R., & Koch, G. G. (1977). The measurement of observer agreement for categorical data. Biometrics, 33(1), 159–174.
Karnofsky, D. A., & Burchenal, J. H. (1949). The clinical evaluation of chemotherapeutic agents in cancer. In C. M. MacLeod (Ed.), evaluation of chemotherapeutic agents (p. 196). New York: Columbia Univ Press.
Fromme, E. K., Eilers, K. M., Mori, M., Hsieh, Y. C., & Beer, T. M. (2004). How accurate is clinician reporting of chemotherapy adverse effects? A comparison with patient-reported symptoms from the Quality-of-Life Questionnaire C30. Journal of Clinical Oncology, 22(17), 3485–3490.
Xiao, C., Polomano, R., & Bruner, D. W. (2013). Comparison between patient-reported and clinician-observed symptoms in oncology. Cancer Nursing, 36(6), E1–E16.
Efficace, F., Rosti, G., Aaronson, N., Cottone, F., Angelucci, E., Molica, S., et al. (2014). Patient- versus physician-reporting of symptoms and health status in chronic myeloid leukemia. Haematologica, 99(4), 788–793.
Jensen, R. E., Rothrock, N. E., DeWitt, E. M., Spiegel, B., Tucker, C. A., Crane, H. M., et al. (2015). The role of technical advances in the adoption and integration of patient-reported outcomes in clinical care. Medical Care, 53(2), 153–159.
Bennett, A. V., Jensen, R. E., & Basch, E. (2012). Electronic patient-reported outcome systems in oncology clinical practice. CA: A Cancer Journal for Clinicians, 62(5), 336–347.
Snyder, C. F., Aaronson, N. K., Choucair, A. K., Elliott, T. E., Greenhalgh, J., Halyard, M. Y., et al. (2012). Implementing patient-reported outcomes assessment in clinical practice: a review of the options and considerations. Quality of Life Research, 21(8), 1305–1314.
Brundage, M. D., Smith, K. C., Little, E. A., Bantug, E. T., & Snyder, C. F. (2015). Communicating patient-reported outcome scores using graphic formats: results from a mixed-methods evaluation. Quality of Life Research, 24(10), 2457–2472.
Chung, A. E., & Basch, E. M. (2015). Incorporating the patient’s voice into electronic health records through patient-reported outcomes as the “review of systems”. Journal of the American Medical Informatics Association, 22(4), 914–916.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no financial disclosures or conflicts of interest to report.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors. A waiver of authorization was approved from the Institutional Review Board at Memorial Sloan Kettering Cancer Center for this retrospective analysis.
Rights and permissions
About this article
Cite this article
Tom, A., Bennett, A.V., Rothenstein, D. et al. Prevalence of patient-reported gastrointestinal symptoms and agreement with clinician toxicity assessments in radiation therapy for anal cancer. Qual Life Res 27, 97–103 (2018). https://doi.org/10.1007/s11136-017-1700-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-017-1700-8