Abstract
Objective
To comprehensively identify components of the physical limitation concept in knee osteoarthritis (OA) and to rate the clinical importance of these using perspectives of both patients and health professionals.
Design
Concept mapping, a structured group process, was used to identify and organize data in focus groups (patients) and via a global web-based survey (professionals). Ideas were elicited through a nominal group technique and then organized using multidimensional scaling, cluster analysis, participant validation, rating of clinical importance, and thematic analyses to generate a conceptual model of physical limitations in knee OA.
Results
Fifteen Danish patients and 200 international professionals contributed to generating the conceptual model. Five clusters emerged: ‘Limitations/physical deficits’; ‘Everyday hurdles’; ‘You’re not the person you used to be’; ‘Need to adjust way of living’; and ‘External limitations,’ each with sub-clusters. Patients generally found their limitations more important than the professionals did.
Conclusion
Patients and professionals agreed largely on the physical limitation concept in knee OA. Some limitations of high importance to patients were lower rated by the professionals, highlighting the importance of including patients when conceptualizing patient outcomes. These data offer new knowledge to guide selection of clinically relevant outcomes and development of outcome measures in knee OA.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The predominant impact of knee osteoarthritis (OA) is generally regarded to be related to pain and physical function; these are recommended core outcomes in clinical trials on OA (Outcome Measures in Rheumatology, OMERACT [1], International Classification of Functioning, Disability and Health, ICF [2]) and chronic pain (Initiative on Methods, Measurement, and Pain Assessment in Clinical Trials, IMMPACT [3]). The guidelines do not offer formal definitions of these outcomes, which may result in false assumptions and inconsistency among researchers, clinicians, and health consumers. Asking simply about pain or physical function in an outcome measure will evoke different responses from different individuals with different problems. Such responses may be highly ambiguous and difficult to interpret. Consequently, careful elaborations of these key concepts are necessary for translation into precise and clinically meaningful constructs for use in outcome measures [4, 5].
While there is a widely used definition of pain—‘an unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage’ [6]—there is no equivalent definition of physical function, despite its high rank in the outcome hierarchy. Judging from the recommended outcome measures for physical function, the concept encompasses a broad range of constructs which all reflect some kind of physical limitation (walking, stair-climbing, shopping, sleeping, exercise tolerance, and muscle strength).
In the process of operationalizing concepts for use as outcome measures, it is important to involve patients alongside health professionals. This ensures clinical relevance by capturing the full range of the patient experience which may not only yield more relevant outcomes measures, but also aid in development and optimization of treatment strategies [7].
It has been reported that patients and professionals do not share points of view on treatment outcomes for chronic pain conditions [8, 9]. This illustrates the importance of a patient informed data-driven approach to define outcomes and guide development of measures. Such an approach was applied by Busija et al. [10] who developed a conceptual model identifying dimensions of the individual burden of OA, and the impact on the broader society. ‘Physical limitations’ was found to be a major dimension.
The specific components of the ‘physical limitation’ concept still need to be elaborated in order to operationalize it into measurable constructs. This adheres to the OMERACT (Outcome Measures in Rheumatology) filter 2.0 that recommends further specification of domains, categorized within a core area [11]. This is done in order to develop and validate new instruments. Accordingly, the objective of this study was to comprehensively identify components of the ‘physical limitation’ concept in knee OA and to rate the clinical importance of these using the perspective of both patients and health professionals.
Methods
Participants
A purposeful sampling of adults with knee OA was recruited through the OA outpatient clinic of Copenhagen University Hospital at Frederiksberg, Denmark, and invited to participate in a group workshop. Patients eligible for participation had a clinical diagnosis of knee OA confirmed by radiography. We did not include patients who were unable to speak, write, or understand Danish. Patients gave informed consent before enrolling in the project and received a copy of their consent.
A wide range of international OA health professionals were invited via email to participate in a web-based survey. Potential participants were identified through our networks and departmental websites. The health professionals were asked to pass on the survey invitation within their professional networks to expand the reach of the consultation. Furthermore, all European physiotherapy organizations were asked to place a link to the survey on their website. The organizations in Denmark, Norway, Sweden, Ireland, Finland, and Germany agreed to do so. The study was approved by the Deakin University Human Research Ethics Committee where the voluntary return of the survey was regarded as implied consent to participate in the project.
A concept mapping method [12] was applied. The method is highly effective in development of outcome measures and is described in detail elsewhere [10]. In short, concept mapping is a formal group process with a structured approach to identify ideas on a topic of interest and organize them into cogent domains. Patients were asked to provide responses to an initial task; ‘Thinking as broadly as you can, please list all the things that you cannot do in your everyday life because of your knee OA.’ Professionals were given a slightly modified initial task: ‘Thinking as broadly as possible, please list all the characteristics of the physical limitations of knee OA.’
Three patient workshops were planned, aiming for four to eight patients participating in each. At each workshop, the concept mapping process was introduced and conducted as follows: (1) individual brainstorming on the initial task, generating statements; (2) in a nominal group process, sharing statements with the group and clarifying the meaning, if necessary; (3) sorting of all statements by each participant in any way that made sense to them; (4) cluster analysis and multidimensional scaling of the sorted statements by use of specialized software (ConceptSystems) [13, 14]; (5) a concept map of the statements, organized into clusters, was presented and discussed with participants; (6) revision of the concept map by participants, including labeling each cluster, drawing associations, and causal relations between clusters and identifying sub- or super-clusters.
A similar approach was applied in the web-based survey for health professionals, using SurveyMonkey® software. The survey was administered in a two-step approach; (1) statement gathering and (2) statement sorting. In the first step, participants were asked to provide up to 20 brief narrative statements responding to the initial task (see above). Further, participants were asked to provide demographic data including their country of residence, profession, number of years in the OA field, academic qualifications, and current work role. Statements were collated and duplicates removed using standardized content analysis [15]. In the second step, the statement pool was sent back to the professionals for sorting and then analyzed as described above.
Further, all participants (patients and health professionals) were asked to rate the importance of each statement on a five-point scale; 1: ‘Not characteristic for knee OA at all,’ 2: ‘Rarely occurring with knee OA,’ 3: ‘Sometimes occurring with knee OA,’ 4: ‘Very frequently occurring with knee OA,’ and 5: ‘Essential (it wouldn’t be knee OA without it).’
Data analysis
Data from the patient and professional concept maps were consolidated by removing identical statements. The reduced statement pool was independently thematically analyzed by two of the authors (LK and EB), preserving fine distinctions in the wording across statements. The exact wording of the statements and cluster labels from the participants were kept, and sub-clusters were given labels derived from specific statements. The mean and median rating of statement importance within each sub-cluster was calculated for both groups separately and compared between groups with a Wilcoxon two-sample test at the p < 0.05 level.
Results
A total of 50 patients were invited to take part and 15 (9 women) participated in one of three workshops and completed the sorting and rating tasks. More than 250 initial e-mail invitations were sent to health professionals with encouragement to pass the invitation to colleagues. A total of 200 people from 15 different countries responded to the survey. Danish was the most frequent nationality (62 %), 70 % were clinicians, and among the clinicians, 67 % were physical therapists. The professionals had a mean of 17 years of experience with OA. A total of 122 respondents (61 %) provided their e-mail addresses and were invited to participate in the second step; sorting and rating of the statements. Of these, 22 (18 %) completed the sorting and rating tasks. Participants’ characteristics are shown in Table 1.
A total of 1739 statements were generated, broadly covering the physical limitations of knee OA (184 from patients, 1552 from professionals). Omitting redundancies within each participant group, the number of statements was reduced to a total of 361 (124 from patients, 104 from professionals). Pooling the two groups, a total of 228 individual statements remained (124 from patients, 104 from professionals). In the thematic analysis, two authors (LK and EB) initially agreed on 62 % of the sorting of statements in terms of location in clusters. The remaining statements were grouped through consensus between LK and EB. In this process, the content of the statements was discussed, placing most emphasis on the patient input; i.e., the concept maps from the patient workshops guided the final location of statements. Figure 1 illustrates the process of data collection and analysis. An example of a concept map from one of the patient groups is given in Fig. 2.
Example of a concept map from one of the patient groups (translated from Danish), based on 61 statements (small numbers) grouped in 10 clusters (large numbers). The grouping of statements is driven by multidimensional scaling in which statements that are frequently sorted together by the participants are placed closer together on the map and thereby interpreted as being closer conceptually related. Gray boxes contain the cluster labels provided by the patient group. Broken lines represent statements (marked with gray background) that are moved from one sub-cluster to another during group discussion. The broken circle indicates that statements and sub-clusters within are related. In this example, cluster number 7 is dissolved, as the participants decided to move all statements to other clusters
The physical limitation conceptual model is shown in Table 2. Overall, five clusters emerged. Within the five clusters, a total of 54 sub-clusters were present: Limitations/physical deficits (14 sub-clusters: ‘pain with load’ was the most important for patients, ‘limited movement’ most important for professionals); Everyday hurdles (19 sub-clusters: ‘hard to walk on stairs’ and ‘difficulty bicycling’ were the most important for patients, ‘cannot squat’ most important for professionals); You’re not the person you used to be (12 sub-clusters: ‘psychological impact’ was the most important for patients, ‘reduced quality of life’ and ‘loss of physical freedom’ most important for professionals); Need to adjust way of living (seven sub-clusters: ‘getting used to another way of living,’ was the most important for patients, ‘impact of pain’ most important for professionals); and External limitations (two sub-clusters: ‘other people thoughts’ were the most important for patients, and this was the only sub-cluster for professionals). The names of the clusters and sub-clusters were primarily derived from labels provided by the patient groups, but also reflected labels from the professional group.
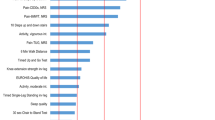
The importance of each statement was identified based on patients’ and professionals’ ratings of all the statements on a scale from one to five (five being most important). A Wilcoxon two-sample test showed group differences (patients vs. professionals) for statements in sub-clusters for 12 of the 54 sub-clusters. Eleven statements were rated significantly higher by patients than by professionals, and one statement was rated significantly higher by professionals than by patients as shown in Fig. 3.
Discussion
This is the first clear, comprehensive, and empirically grounded picture of the impact of knee OA in terms of physical limitations. Based on consultations with patients and professionals from 15 countries, our conceptual model of physical limitations in knee OA brings new knowledge and has the potential to guide selection of outcomes in research and clinical practice. The physical limitation conceptual model is sorted by patient-rated importance and thus provides a hierarchy for choosing components of physical limitation in the development of outcome measures.
Patients and professionals largely agreed on what encompass the physical limitation concept in knee OA. This suggests that the professionals had an appropriate, though not exhaustive, idea of the impact of physical limitations in knee OA as experienced by patients. On the other hand, professionals may impart personal subjects that patients are reluctant to talk about in focus groups, for example, sexual health that was mentioned by professionals but not patients. This is in line with reports on other chronic pain conditions mentioned in the introduction [8, 16] and highlights the importance of involving both patients and professionals in the identification and elaboration of relevant outcome components. Our conceptual model corresponds with the findings of Busija et al. [10] but elaborates more on the components on physical limitations, whereas Busija’s model provides a broader perspective on the individual and societal burden of knee OA.
The patients rated some knee-related problems higher on importance than the professionals did, and for eleven statements, this difference was statistically significant. The exception was ‘cannot squat,’ which was rated more relevant by professionals. Some of these differences may be initiated by the different terminology of patients and professionals. Even though the patients also had statements about deep knee bends which in the analysis were regarded as equivalent to the professionals’ squatting, they did not perceive this as relevant as some of the other statements that require deep knee bends, such as reaching the floor and getting up or down from low seating. This suggests that the two groups use different words and context settings to describe the same phenomenon. Thus, many of the same limitations are recognized by both groups, but the different perceptions may cause misunderstandings. The point is that from the patients’ perspective their knee-related limitations integrate components from theoretically separated constructs, as seen in the widely used International Classification of Functioning, Disability, and Health (ICF) with the categories ‘Body Functions and Structure’, ‘Activities of Daily Living’, and ‘Participation'. Our interpretation of this is that even though a theoretical framework is useful to obtain a common understanding between professionals, the same framework does not necessarily translate to patients, who experience their physical limitations through the activities they cannot do or participate in. This need for contextual framing of physical limitations should be considered, both in clinical settings and in relation to outcome evaluation. It is especially important in the development of outcome measures, for example, choosing items for a questionnaire, where the content validity relies very strongly on the respondent’s understanding of the question.
Many professional participants suggested a cluster for pain exclusively, where detailed aspects of pain were stated (e.g., pain at rest, pain with movement, pain with fatigue, and pain relief with movement). In general, pain was strongly represented in all groups, but interestingly only one of the three patient groups had a cluster with the label ‘pain’. Rather, the patients reflected on pain in conjunction with movements, activities, and participation, emphasizing the intimate association between pain and function. Surprisingly, there was no mentioning of constant or intermittent pain, which is the main theme of the Intermittent and Constant OsteoArthritis Pain score (ICOAP), a questionnaire based on extensive interviews with patients [9]. Sudden pain, which could correspond to intermittent pain, was stated by professionals, but not patients in this sample. However, the element of the pain being unpredictable is possibly implied in some of the sub-clusters of the concept (‘Planning is essential’ and ‘getting used to another way of living’) but did not come out as an individual construct among the patients.
The patients did not specifically mention overall difficulties with walking, as the professionals did. This was a general observation—the professionals tended to provide general statements, as opposed to the patients’ more detailed and contextually specified statements. For example, the professional group generated statements such as ‘general functional disability’ which comprises several poorly defined physical limitations. Not mentioning overall walking difficulties, patients did highlight fast walking, walking long distances, or walking on uneven surfaces. This last statement was rated significantly more relevant by patients than by professionals. In line with this, it is worth noting that the item ‘difficulties walking on even surfaces’, but not uneven surfaces, is included in two commonly used questionnaires in knee OA research, the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) [17] and the Knee Injury and Osteoarthritis Outcome Score (KOOS) [18]. The importance of walking disability was highlighted in a recent cohort study by Hawker et al. [19] showing that worse self-reported baseline WOMAC function scores and walking disability were independently associated with higher all-cause mortality for people with hip and knee OA.
Limitations of this study
We chose not to apply restrictive inclusion- and exclusion criteria, resulting in a heterogenic sample as specified in Table 1. It could be argued that a more restricted sample excluding co-morbidities and other potential influencing factors would have been a better strategy to obtain a more homogenous and ‘clean’ sample, which would represent people with knee OA only. However, in the real world, people with knee OA often have co-morbidities and other ‘disturbing’ factors; with this naturalistic sample, we aimed to reflect this circumstance.
For data collection, we used the term ‘physical limitations’ in the initial task to the professionals and ‘limitations in everyday life’ to the patients. This choice to differentiate between patients and professionals may have influenced our results and inflated the observed differences between the two groups. We did this because we expected to elicit all potential physical limitations from both groups with this approach. We suspected that the term ‘physical limitation’ would be somewhat unfamiliar for the patient groups and therefore chose a term that they could relate to. Regarding the professionals, we suspected that use of the term ‘everyday life’ would prompt associations to the ICF category ‘Activities of Daily Living,’ and did not want to limit the responses to that specific term commonly used by health professionals. ‘Physical limitations’ is a broad term not encompassed by the ICF. Thereby, we hoped to help the professionals to set aside their presumptions and assumed tendency to theorize concepts, which is a limiting factor in a data-driven approach.
Still, the structure of the physical limitation conceptual model, as illustrated in Table 2, is similar to that of the ICF with the main categories ‘Body Function and Structure,’ ‘Activity,’ and ‘Participation.’ We assume that this similarity is brought about by an inherent ‘health professional way of thinking,’ and primarily generated by the professional participants who also largely used the ICF terminology. However, the methods we used systematically ensured that participants’ contributions were preserved throughout the process where no unique statements were lost. The views of the patients were also preserved as we used the patients’ clusters and sub-clusters as the initial template for organizing the resulting model.
Implications
These results offer relevant knowledge in order to operationalize the recommended outcome of physical function and in the choice or development of outcome measures. From the patients’ perspective, the concept of physical limitations in knee OA is broadly encompassing constructs across the widely used ICF model. This should give raise to considerations about aiming knee OA treatment at improving physical function as broadly as the patients define it. Importantly, our data were generated using a grounded approach, and the derived framework emerged from distinct separate clusters—providing clear guidance for the development of a multi-dimensional outcome measure that has high construct validity and is capable to measuring clearly defined independent and important concepts. This process has been used to develop several multidimensional tools with very high construct validity across settings and cultures [7, 20, 21]. Moreover, the model provides strong guidance for interventions aimed at improving knee OA outcomes, particularly improving physical function, even as broadly as patients define it. This is consistent with Hawker et al. [22] call for clearly defined outcomes concerning participation, and treatments targeting participation.
With the concept mapping approach, the results are simply the participants’ statements organized into clusters, and these can reveal simple associations and also implied causal paths between the derived concepts. As the original statements still exist within each cluster, these data can be organized into an item pool, with conceptually sound constructs ready for use in the development of a new outcome measure in knee OA. This work is ongoing.
Conclusion
Patients and professionals agreed largely on the physical limitation concept in knee OA, although they had different ways of describing the components. The patients rated some knee-related physical limitations significantly higher on importance than the professionals, highlighting the importance of patient involvement in developing outcome recommendations and measures. These data offer new detailed knowledge about physical limitations in knee OA which can guide selection and innovation of clinically relevant outcomes and outcome measures.
References
Bellamy, N., Kirwan, J., Boers, M., Brooks, P., Strand, V., Tugwell, P., et al. (1997). Recommendations for a core set of outcome measures for future phase III clinical trials in knee, hip, and hand osteoarthritis. Consensus development at OMERACT III. Journal of Rheumatology, 24(4), 799–802.
Dreinhofer, K., Stucki, G., Ewert, T., Huber, E., Ebenbichler, G., Gutenbrunner, C., et al. (2004). ICF core sets for osteoarthritis. Journal of Rehabilitation Medicine, 44(Suppl), 75–80.
Dworkin, R. H., Turk, D. C., Farrar, J. T., Haythornthwaite, J. A., Jensen, M. P., Katz, N. P., et al. (2005). Core outcome measures for chronic pain clinical trials: IMMPACT recommendations. Pain, 113(1–2), 9–19.
Pollard, B., Johnston, M., & Dieppe, P. (2006). What do osteoarthritis health outcome instruments measure? Impairment, activity limitation, or participation restriction? Journal of Rheumatology, 33(4), 757–763.
Buchbinder, R., Batterham, R., Elsworth, G., Dionne, C. E., Irvin, E., & Osborne, R. H. (2011). A validity-driven approach to the understanding of the personal and societal burden of low back pain: Development of a conceptual and measurement model. Arthritis Res Ther, 13(5), R152.
Merskey, H., Bonica, J. J., Carmon, A., Dubner, R., Kerr, F. W. L., Lindblom, U., et al. (1979). Pain terms: A list with definitions and notes on usage. Recommended by the IASP subcommittee on Taxonomy. Pain, 6(3), 249.
Osborne, R. H., Batterham, R. W., Elsworth, G. R., Hawkins, M., & Buchbinder, R. (2013). The grounded psychometric development and initial validation of the Health Literacy Questionnaire (HLQ). BMC Public Health, 13, 658.
Turk, D. C., Dworkin, R. H., Revicki, D., Harding, G., Burke, L. B., Cella, D., et al. (2008). Identifying important outcome domains for chronic pain clinical trials: An IMMPACT survey of people with pain. Pain, 137(2), 276–285.
Hawker, G. A., Davis, A. M., French, M. R., Cibere, J., Jordan, J. M., March, L., et al. (2008). Development and preliminary psychometric testing of a new OA pain measure—An OARSI/OMERACT initiative. Osteoarthritis Cartilage, 16(4), 409–414.
Busija, L., Buchbinder, R., & Osborne, R. H. (2013). A grounded patient-centered approach generated the personal and societal burden of osteoarthritis model. Journal of Clinical Epidemiology, 66(9), 994–1005.
Boers, M., Kirwan, J. R., Wells, G., Beaton, D., Gossec, L., d’Agostino, M. A., et al. (2014). Developing core outcome measurement sets for clinical trials: OMERACT filter 2.0. Journal of Clinical Epidemiology, 67(7), 745–753.
Trochim, W., & Kane, M. (2005). Concept Mapping: An introduction to structured conceptualization in health care. International Journal for Quality in Health Care, 17(3), 187–191.
Trochim, W. M., Cook, J. A., & Setze, R. J. (1994). Using concept mapping to develop a conceptual framework of staff’s views of a supported employment program for individuals with severe mental illness. Journal of Consulting and Clinical Psychology, 62(4), 766–775.
Trochim, W. M., & Linton, R. (1986). Conceptualization for planning and evaluation. Evolution Program of Planning, 9(4), 289–308.
Crabtree, B. F., & Miller, W. L. (1999). Using codes and code manuals—a template organizing style of interpretation. In B. F. Crabtree & W. L. Miller (Eds.), Doing qualitative research (2nd ed., pp. 163–177). Thousand Oaks: Sage.
Beale, M., Cella, M., & Williams, A. C. C. (2011). Comparing patients’ and clinician-researchers’ outcome choice for psychological treatment of chronic pain. Pain, 152(10), 2283–2286.
Bellamy, N., Buchanan, W. W., Goldsmith, C. H., Campbell, J., & Stitt, L. W. (1988). Validation study of WOMAC: A health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. Journal of Rheumatology, 15(12), 1833–1840.
Roos, E. M., Roos, H. P., Lohmander, L. S., Ekdahl, C., & Beynnon, B. D. (1998). Knee Injury and Osteoarthritis Outcome Score (KOOS)—Development of a self-administered outcome measure. Journal of Orthopaedic and Sports Physical Therapy, 28(2), 88–96.
Hawker, G. A., Croxford, R., Bierman, A. S., Harvey, P. J., Ravi, B., Stanaitis, I., et al. (2014). All-cause mortality and serious cardiovascular events in people with hip and knee osteoarthritis: A population based cohort study. PLoS ONE, 9(3), e91286.
Osborne, R. H., Elsworth, G. R., & Whitfield, K. (2007). The Health Education Impact Questionnaire (heiQ): An outcomes and evaluation measure for patient education and self-management interventions for people with chronic conditions. Patient Education and Counseling, 66(2), 192–201.
Osborne, R. H., Norquist, J. M., Elsworth, G. R., Busija, L., Mehta, V., Herring, T., et al. (2011). Development and validation of the Influenza Intensity and Impact Questionnaire (FluiiQ). Value Health, 14(5), 687–699.
Hawker, G. A., & Gignac, M. A. (2006). How meaningful is our evaluation of meaningful change in osteoarthritis? Journal of Rheumatology, 33(4), 639–641.
Acknowledgments
We would like to thank the patients and health professionals who participated in this study. This study was supported by grants from The Oak Foundation, The Danish Physiotherapy Association, and The Danish Rheumatism Association. Financial support was provided from The Parker Institute and Deakin University.
Conflict of interest
The authors declare that they have no conflict of interests that could influence their work and conclusions in relation to this manuscript.
Informed consent
Informed consent was obtained from all individual patients included in the study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Klokker, L., Osborne, R., Wæhrens, E.E. et al. The concept of physical limitations in knee osteoarthritis: as viewed by patients and health professionals. Qual Life Res 24, 2423–2432 (2015). https://doi.org/10.1007/s11136-015-0976-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-015-0976-9