Abstract
Purpose
It is not completely clear whether and how medication adherence, asthma control, and quality of life (QOL) predict each other over time. Therefore, the aim of the present study was to examine the longitudinal associations between asthma control, medication adherence, and quality of life among adolescents.
Methods
In this 3-wave longitudinal study, adolescents (N = 139, Mean age = 11.8) completed questionnaires about their medication adherence (Medication Adherence Report Scale for Asthma), asthma control (Asthma Control Questionnaire), and QOL (Adolescent Asthma Quality of Life Questionnaire) during home visits in the spring/summer of 2011, 2012, and 2013. Cross-lagged analyses examined temporal interrelations between the three variables over the course of 3 years.
Results
Higher QOL at baseline predicted increased medication adherence at follow-up (T2), but did not predict changes in asthma control over time. Medication adherence and asthma control did not predict changes in QOL over time. There were no associations between asthma control and medication adherence over time.
Conclusions
Interventions could focus on increasing QOL to increase medication adherence in adolescents with asthma.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Asthma is the most common chronic disease in childhood [1], with a reported lifetime prevalence of 12.9 % in the Netherlands, which is higher compared to other Western European countries [2]. Asthma is characterized by recurrent episodes of wheezing, breathlessness, tightness of the chest, and coughing, particularly in the morning or at night [3]. Adolescents with poorly controlled asthma show more of these symptoms, and more frequently, than well-controlled teens. To control asthma most effectively, daily adherence to preventer asthma medication is necessary. With non-adherence, not taking asthma medication as recommended by the health-care provider, the effect of asthma medication is reduced [4]. Moreover, adolescents with asthma experience increased psychosocial problems [e.g., lower quality of life (QOL)] compared to their healthy peers.
Cross-sectional studies on the relations between asthma control and medication adherence are inconsistent. One study found a positive relation between asthma control and medication adherence in adults [5], while another study did not find a correlation between the two variables in young adults [6]. Longitudinal studies, for both children and adolescents with asthma, found that good medication adherence predicted increased asthma control at each follow-up (after 4, 8, and 12 months) [7, 8]. However, no studies examined whether asthma control could predict changes in medication adherence. Studies on other chronic diseases than asthma, like on adults with HIV [9], showed that better control over the disease increased adherence to HIV medication at 6 months. However, this result based on adults with HIV could not be generalized to adolescents with asthma. Medication for HIV has much more side effects than asthma medication, and medication regimes differ between HIV and asthma. Moreover, results based on adult patients could differ from adolescents. Adolescence is a phase where many changes occur and where it is very important for the adolescents not to be ‘different’ than their peers because they need medication. Therefore, we do not base the hypothesis of the present study on studies with other chronic diseases than asthma or adults. For adolescents with asthma, one could hypothesize that if adolescents have more control over asthma, medication adherence could decrease over time. When adolescents experience less or no symptoms of asthma (good control), they could think that their medication is no longer necessary. However, it could also be expected that more control over asthma could predict an increase in medication adherence because adolescents experience that their medication is effective; therefore, they adhere to it. This study aimed to test the bidirectional relation between asthma control and medication adherence.
Cross-sectional studies have not yielded significant correlations between medication adherence and QOL [7, 10, 11]. Most intervention studies that aimed to increase medication adherence in adults with asthma found that better medication adherence predicted increases in QOL from baseline to follow-up at 2 to 4 weeks [12], and even over longer periods of time, like 3 months [13]. However, some studies did not show improvement in QOL as a result of better medication adherence at 3 or 6 months after the intervention [14]. To our knowledge, no studies have yet examined whether QOL predicts changes in medication adherence. The hypothesis on this relation is twofold. It could be expected that good QOL could lead to decreases in adherence because adolescents feel good and do not think they need their medication. It is also possible that medication adherence increases when adolescents have a good QOL, because they do not feel barriers to take their asthma medication. The literature seems to support the second hypothesis in that better emotional well-being is related to increased medication adherence [15, 16]. Because of inconsistencies in the results on the relation between medication adherence and QOL in the previous literature and the lack in results on the relation between medication adherence and QOL in adolescents with asthma, it is important to examine the temporal interrelations between these two variables in this population.
Finally, positive associations have been found between asthma control and QOL. Cross-sectional studies showed that more asthma control is related to better QOL in adolescents with asthma [17–20]. One longitudinal study showed that in children (1–14 years old), more control over asthma predicted improvement in QOL at 2- and 6-week follow-up and at 6-month follow-up [21]. No studies yet examined whether QOL could predict changes in asthma control. We expected that based on the previous hypothesis for the relation between QOL and medication adherence, better QOL could increase or decrease asthma control because of increased or decreased medication adherence.
In sum, the aim of the present study was to examine the temporal relations between asthma control, medication adherence, and QOL in adolescents with asthma using a cross-lagged model. Given the focus of this study on adherence to preventive asthma medication, this study only included adolescents who were prescribed daily preventive asthma medication during the 3 years of this study. With the cross-lagged analyses, the temporal nature of the relations between the three variables could be examined. Longitudinal research has the advantage of examining the temporal relations between variables, and using a cross-lagged design, all variables are included within one model.
Methods
Procedure
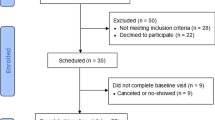
This study was approved by the ethics committee of the Faculty of Social Sciences of the Radboud University Nijmegen. Participants were recruited through schools and an announcement of the study in the magazine of the Lung Foundation Netherlands. Information on the recruitment procedure can be found elsewhere [22].
Families were included if (1) the adolescent received an asthma diagnosis by a physician, (2) the adolescent used asthma medication or experienced asthma-related symptoms at least once in the last 12 months, and (3) parents had adequate Dutch language skills. Of the 311 families that responded to the invitation letter, 261 (83.9 %) met the inclusion criteria at baseline (T1). In total, 257 (98.5 %) families participated at follow-up (T2) 1 year later and 253 (96.9 %) 2 years later (T3). Given the focus of this study on preventive asthma medication adherence, we selected 139 families where the adolescents have prescribed daily preventive asthma medication at T1, T2, and T3.
All participating families were visited at home three times, in March–September of 2011, 2012, and 2013. During the home visits, after brief instructions and the guarantee of anonymity, adolescents filled out the informed consent forms and completed questionnaires about, among other variables, medication adherence, QOL, and asthma control. Additionally, adolescents performed a lung function test. Participating families received a 20-Euro voucher for participating the first two years and a 35-Euro voucher for participating the third year.
Measures
Medication adherence
A Dutch translation of the Medication Adherence Report Scale for Asthma (MARS-A) [23] was used to measure adherence to asthma preventive medication. The MARS-A has been reliably used for (early)adolescents with a chronic lung disease before [24]. Adolescents were asked to describe their typical patterns of medication adherence by rating 10 items (e.g., ‘I alter the dose of my medication’) on a five-point Likert scale ranging from 1 = ‘very often’ to 5 = ‘never’. A mean score was calculated for the 10 items, with a lower score indicating low medication adherence.
Quality of life
The Adolescent Asthma Quality of Life questionnaire (AAQOL) was used to measure adolescents’ asthma-specific QOL [25]. The AAQOL was uniquely developed for and reported by adolescents with asthma and contained six subscales that cover the most important aspects in the lives of adolescents with asthma: the symptoms domain (six items; e.g., How bothered have you been by wheezing?, the medication domain (five items; e.g., How bothered or concerned have you been about taking medication for your asthma?), the physical activities domain (six items; e.g., How often have you been restricted in sports, hobbies, or other recreational activities because of your asthma?), the emotions domain (five items; e.g., How often did you feel frustrated because of your asthma?), the social interaction domain (five items; e.g., How often did you feel worried or embarrassed when taking asthma medication in front of other people?), and the positive effects domain (five items; e.g., With regard to your asthma, how often have your friends been helpful and understanding?). Responses were given on a seven-point Likert scale that ranged from 1 = ‘often’ to 7 = ‘never.’ The symptom domain had too much overlap with asthma control; therefore, it was not included in the QOL score. As recommended by the authors of the scale, the positive effects domain was not included in the total QOL score, because this is the only domain that focusses on the positive effects of asthma on the QOL of the adolescents, while the other domains assess the negative effects. Therefore, the positive effects domain could not be added to the total score meaningfully [25]. The other four subscales (medication, physical activities, emotions, and social interaction domains) together formed the QOL variable. A mean score was calculated for the total QOL including the medical, physical activity, emotions, and social interaction domains, with a higher score on the total QOL indicating better QOL of the adolescents.
Asthma Control Questionnaire
The Dutch translation of the Asthma Control Questionnaire (ACQ) consists of seven items, and answers are given by the adolescents with respect to experiences in the previous week [26]. Answers are given on a seven-point scale that ranged from 0 = ‘complete control’ to 6 = ‘very little control.’ Five items are about the five most common symptoms of asthma (e.g., ‘During the past week, how often were you woken by your asthma during the night?’) and one on daily rescue bronchodilator use. The ACQ is not a fully self-reported questionnaire. One item is based on the FEV1 % predicted, which is assessed with the lung function test. The result of the lung function test relate directly to a score on the ACQ. For example, a test result of >.95 % predicted FEV1 gives a score 0, a test result between .89 and .80 % predicted FEV1 gives a score 2, and a test result between .69 and .60 predicted FEV1 gives a score 4. This scale has reliably been used to measure asthma control in (early)adolescents before [27]. The mean score of all seven items formed the asthma control variable, with a higher score on the ACQ indicating a better control over asthma.
Covariates
Adolescents’ gender, age, and time since diagnosis of asthma, as well as mothers’ countries of birth were included as control variables in the analyses. These variables were included as confounders, because they were found to be associated in this sample with one or more of the main variables (medication adherence, asthma control, and QOL). Other variables, like adolescent education, or if parents (have) had asthma, did not associate with the main variables and were therefore not included as covariates.
Analyses
SPSS19 was used to calculate the mean, standard deviation, and intercorrelations of the variables. Paired sample t tests were conducted to examine changes in adherence, QOL, and asthma control (ACQ). Mplus6 was used to test the cross-lagged relations between medication adherence, QOL, and asthma control (ACQ), controlled for the covariates at T1. In the cross-lagged analysis at each time point (i.e., T1, T2, T3), medication adherence, QOL, and asthma control were allowed to correlate. To examine the mediating effect of medication adherence on the relation between QOL and asthma control, we included an indirect model in the analysis, where QOL at T1 related with asthma control at T3 through medication adherence at T2. Model fit was evaluated by the way of the (a) root-mean-square error of approximation (RMSEA) and (b) comparative fit index (CFI). Preferably, RMSEA values should be ≤.05, and CFI values should be >.90 [28]. Additionally, the Chi-square value, degrees of freedom, and the p value of the model are reported. Associations between variables were evaluated based on standardized path coefficients and p values (p < .05). Full-information maximum likelihood (FIML) estimation was applied to make use of all available data.
Results
Sample characteristics
Demographic characteristics are presented in Table 1. Mean age of the adolescents (N = 139) at T1 was 11.8, at T2 12.8, and at T3 13.8. Male adolescents (57.6 %) were slightly overrepresented, and most adolescents were born in the Netherlands (97.8 %). Most adolescents had asthma for an average of 7.4 years; during this study, most adolescents (61.9 %) reported partly controlled asthma according to the global initiative for asthma (GINA) guidelines [29]. At T2, asthma control, regarding these GINA guidelines [29], was divided into 18.0 % of the adolescents with controlled, 59.0 % partly controlled, and 23.0 % uncontrolled asthma. At T3, 21.6 % of the adolescents had controlled, 54.0 % partly controlled, and 24.5 % uncontrolled asthma.
Reliability scores
The internal consistency as measured by the Cronbach’s Alpha was acceptable to good for all variables (Table 2).
Correlations
In Table 3, intercorrelations between the model variables are represented. Pearson’s correlations showed strong positive associations between adherence at T1–T2–T3, asthma control at T1-T2-T3, and QOL at T1–T2–T3. Positive associations were also found between medication adherence T1 and QOLT1, and between medication adherence T2 and QOLT1, T2, and T3. Furthermore, positive correlations were found between asthma control and QOL at all time points.
Paired sample t tests showed that medication adherence at T2 did not significantly differ from T1 (t = 1.10, df = 136, p = .28). However, medication adherence at T3 was significantly lower compared to T1 (t = 2.96, df = 136, p = .004). Asthma control did not change over time. Compared to QOL at T1, QOL at T2 (t = −3.50, df = 138, p = .001) and T3 (t = −3.41, df = 138, p = .001) significantly increased over time.
Cross-lagged model
The cross-lagged model showed a satisfactory fit (Fig. 1). Results showed strong positive autocorrelations for medication adherence, QOL, and asthma control measures over time (Fig. 1). Furthermore, QOL at T1 predicted an increase in medication adherence at T2, but QOL did not predict changes in asthma control over time. Medication adherence and asthma control did not predict changes in QOL over time, and there were no associations between medication adherence and asthma control over time. Regarding the indirect effect of medication adherence on the relation between QOL and asthma control, the results showed that the relation between QOL and asthma control was not mediated by medication adherence (β = −.00, SE = −.10, p = .92).
Cross-lagged relations between adherence, asthma control, and QOL. Note QOL Quality of life, C covariates (adolescents’ gender, age, time since diagnosis of asthma, mothers’ country of birth). Fit indices: N = 139, χ2 [72] = 656.51, p < .001, CFI = .99, RMSEA = .04. 90 % CI of the RMSEA estimate = .00 .057, SRMR = .04. *p < .05, **p < .01, ***p < .001
Discussion
This study examined the temporal interrelations of self-reported medication adherence, asthma control, and QOL in adolescents with asthma. Results showed that better QOL at baseline predicted an increase in medication adherence at follow-up 1 year later. Other associations over time were not found in the present study.
The finding of the present study showed that medication adherence decreased over time, which is in line with previous studies [30]. Asthma control remained high, despite the drop in medication adherence. A possible explanation is that adolescent with asthma can experience a symptom-free period [31]. In this period, asthma medication is not necessary to control asthma. Thus, with lower medication adherence, no changes are expected in asthma control. QOL of the adolescents increased over time, which is in line with Sawyer et al. [32]. They suggest that this could be explained by the illness perceptions of the adolescents. Over time, adolescents perceived their illness as less concerning. With that, adolescents report less interference of asthma reflected in their QOL.
This study showed that medication adherence did not predict changes in asthma control, and asthma control did not predict changes in medication adherence over time. This finding is in contrast to previous studies in which medication adherence did predict changes in asthma control [7, 8]. A possible explanation for not finding such relations could be differences in study designs. Previous studies used intensive interventions to increase medication adherence [7, 8], while the present study did not use an intervention design, but used a cross-lagged observational study design; here medication adherence decreased instead of increased. Another explanation could be that adolescents had ‘outgrown’ their asthma [20]. Symptoms of asthma can disappear in puberty (although symptom can return at later ages) [33], and with that, asthma medication is no longer needed to control [33, 34]. This could explain why low medication adherence did not predict a decrease in asthma control over time. Further, asthma control did not predict changes in medication adherence over time. It is possible that asthma control predicts medication adherence only for a certain group of adolescents. In other words, the relation between asthma control and medication adherence could be moderated by, for example, the knowledge or beliefs that adolescents have about their medications [35]. When asthma is well controlled, adolescents do not experience symptoms. For example, if adolescents do not know or believe that asthma medication should be taken continuously, even when they do not experience symptoms, well-controlled asthma could lead to medication non-adherence.
For the temporal interrelations between QOL and medication adherence, the results were in contrast to previous studies [11, 13]. Specifically, good medication adherence did not predict an increase in QOL over time. An explanation for this finding could be that there is no room for QOL to increase. Adolescents in this study already had a relatively high score on QOL at baseline; mean scores were around six on a scale from 1 (bad QOL) to 7 (very good QOL). Perhaps medication adherence would predict an increase in QOL only in populations with low baseline scores. However, this study did show that better QOL at baseline predicted increased medication adherence at follow-up 1 year later. No previous studies have examined this relation in adolescents with asthma. Nevertheless, the research has shown in adolescents and adults with asthma that other negative psychosocial factors related to decreased medication adherence [17, 36]. Thus, it could be that when adolescents feel good (have a good QOL), they are better able to overcome the barriers to take asthma medication. It could also be that when adolescents feel good, they attribute this feeling to the effectiveness of their medication and with the adherence to their medication.
Finally, considering the temporal interrelations between asthma control and QOL, the present study showed that, in contrast to a previous study [21], asthma control did not predict changes in QOL. Moreover, we did not find that QOL predicted changes in asthma control over time. A possible explanation could be that asthma control did not change over time in the present study. With no change over time in asthma control and only a small increase in QOL, it is hard to detect significant changes over time in QOL predicted by asthma control, and changes in asthma control predicted by QOL. Another explanation could be the time-intervals between T1, T2, and T3. There was 1 year between each follow-up. In the study of Benito-Férnandez [21], relations between asthma control and QOL were examined with time-intervals of 2 and 6 weeks and 6 months. These time-intervals are much shorter than our 1-year interval. Therefore, perhaps using shorter time-intervals would have given us more opportunity to find relations over time between QOL and asthma control.
This study has several strengths and limitations. Strength is the use of cross-lagged analyses; this study could test all temporal interrelations between the variables. Limitation is that medication adherence was measured with self-report, rather than more objective measures such as electronic devices. Measuring medication adherence with an electronic device could give a more accurate view of adolescents’ medication adherence [37]. Further, the sample was rather homogeneous regarding ethnicity, and most adolescents had partly controlled asthma. Thus, the results of this study cannot be generalized to all adolescents with asthma. Another limitation of this study was the exclusion of families because of language barriers. Families would be excluded if the parents and/or adolescent were not able to complete the Dutch questionnaires. This is a limitation in the present study, because the persons who would not understand the questionnaires possibly would have a limited health literacy [38], which could have affected the results. Therefore, it is advised for future studies to include these families as well and assist them in completing the questionnaires. A last limitation was that the variables (medication adherence, QOL, and asthma control) were relatively stable across time. With only small changes over time in the variables, it is hard to detect whether the variables could predict changes in each other over time.
In conclusion, this study adds important information about the relevance of QOL for medication adherence in adolescents with asthma. It is the first study to show positive effects of QOL on medication adherence. Results suggest that increasing QOL in intervention or prevention programs is beneficial to increasing medication adherence of adolescents with asthma. To increase QOL, several interventions could be implemented. For instance, one study showed that creating an asthma-friendly school environment could enhance QOL of adolescents with asthma [39]. Furthermore, group sessions guided by health-care professionals have shown beneficial for adolescent QOL [40].
References
World Health Organization. (2013). Asthma Fact Sheet. http://www.who.int/mediacentre/factsheets/fs307/en/index.html
van de Ven, M. O. M., van den Eijnden, R. J., & Engels, R. M. C. E. (2006). Atopic diseases and related risk factors among Dutch adolescents. European Journal of Public Health, 16, 549–558. doi:10.1093/eurpub/ckl022.
Lung Foundation Netherlands. https://www.longfonds.nl/over-longen/longziekten-overzicht/astma
Milgrom, H., Bender, B., Ackerson, L., Bowry, P., Smith, B., & Rand, C. (1996). Noncompliance and treatment failure in children with asthma. Journal of Allergy and Clinical Immunology, 98, 1051–1057.
Murphy, A. C., Proeschal, A., Brightling, C. E., Wardlaw, A. J., Pavord, I., Bradding, P., & Green, R. H. (2012). The relationship between clinical outcomes and medication adherence in difficult-to-control asthma. Thorax, 67, 751–753. doi:10.1136/thoraxjnl-2011-201096.
Axelsson, M., Emilsson, M., Brink, E., Lundgren, J., Torén, K., & Lötvall, J. (2009). Personality, adherence, asthma control and health-related quality of life in young adult asthmatics. Respiratory Medicine, 103, 1033–1040. doi:10.1016/j.rmed.2009.01.013.
Jentzsch, N. S., Camargos, P., Sarinho, E. S. C., & Bousquet, J. (2012). Adherence rate to beclomethasone dipropionate and the level of asthma control. Respiratory Medicine, 106, 338–343. doi:10.1016/j.rmed.2011.12.001.
Lasmar, L., Camargos, P., Champs, N. S., Fonseca, F. T., Fontes, M. J., Ibiapina, C., & Moura, J. A. R. (2009). Adherence rate to inhaled corticosteroids and their impact on asthma control. Allergy, 64, 784–789. doi:10.1111/j.1398-9995.2008.01877.x.
Howard, A. A., Arnsten, J. H., Lo, Y., Vlahov, D., Rich, J. D., Schuman, P., & Schoenbaum, E. E. (2002). A prospective study of adherence and viral load in a large multi-center cohort of HIV-infected women. AIDS, 16, 2175–2182.
Clerisme-Beaty, E. M., Bartlett, S. J., Teague, W. G., Lima, J., Irvin, C. G., Cohen, R., & Wise, R. A. (2011). The Madison avenue effect: How drug presentation style influences adherence and outcome in patients with asthma. Journal of Allergy and Clinical Immunology, 127, 406–411. doi:10.1016/j.jaci.2010.11.038.
Leroyer, C., Lebrun, T., Proust, A., Lenne, X., Lucas, E., Rio, G., & Clavier, J. (1998). Knowledge, self-management, compliance and quality of life in asthma: A cross-sectional study of the French version of the asthma quality of life questionnaire. Quality of Life Research, 7, 267-272. http://www.jstor.org/stable/4035807
Choi, J. Y., & Chung, H. C. (2010). Effect of an individualized education programme on asthma control, inhaler use skill, asthma knowledge and health-related quality of life among poorly compliant Korean adult patients with asthma. Journal of Clinical Nursing, 2010(20), 119–126. doi:10.1111/j.1365-2702.2010.03420.x.
Kaya, Z., Erkan, F., Ozkan, M., Ozkan, S., Kocaman, N., Ertekin, B. A., & Direk, N. (2009). Self-management plans for asthma control and predictors of patient compliance. Journal of Asthma, 46, 270–275. doi:10.1080/02770900802647565.
Wang, K., Chian, C., Lai, H., Tarn, Y., & Wu, C. (2010). Clinical pharmacist counseling improves outcomes for Taiwanese asthma patients. Pharmacy World & Science, 32, 721–729. doi:10.1007/s11096-010-9427-4.
Simoni, J., Asarnow, J., Munford, P., Koprowski, C., Belin, T., & Saluskky, I. (1997). Psychological distress and treatment adherence among children on dialysis. Pediatric Nephrology, 11, 604–606. doi:10.1007/s004670050346.
Van de Ven, M. O. M., Witteman, C. L. M., & Tiggelman, D. (2013). Effect of Type D personality on medication adherence in early adolescents with asthma. Journal of Psychosomatic Research, 75, 572–576. doi:10.1016/j.jpsychores.2013.09.001.
Everhart, R. S., & Fiese, B. H. (2009). Asthma severity and child quality of life in pediatric asthma: A systematic review. Patient Education and Counseling, 75, 162–168. doi:10.1016/j.pec.2008.10.001.
Chan, K. S., Mangione-Smith, R., Burwinkle, T. M., Rosen, M., & Varni, J. W. (2005). The PedsQL™: Reliability and validity of the short-form generic core scales and asthma module. Medical Care, 43, 256-65. http://www.jstor.org/stable/3768224
Sawyer, M. G., Spurrier, N., Whaites, L., Kennedy, D., Martin, A. J., & Baghurst, P. (2001). The relationship between asthma severity, family functioning, and the health related quality of life of children with asthma. Quality of Life Research, 9, 1105–1115.
Van de Ven, M. O. M., Engels, R. C. M. E., Sawyer, S. M., Otten, R., & van den Eijnden, R. J. J. M. (2007). The role of coping strategies in quality of life of adolescents with asthma. Quality of Life Research, 16, 625–634. doi:10.1007/s11136-006-9146-4.
Benito-Fernández, J., Mojica-Moñoz, E., Andrés-Olaizola, A., González-Balenciaga, M., Urrutia-Adan, M., Martinez-Indart, L., & Mintegi, S. (2013). Impact on quality of life by improving asthma control medication in patients with persistent asthma in a paediatric emergency department. European Journal for Emergency Medicine, 20, 350–355. doi:10.1097/MEJ.0b013e32835ad5c8.
Tiggelman, D., van de Ven, M. O. M., van Schayck, O. C. P., & Engels, R. C. M. E. (2014). Moderating effect of gender on the prospective relation of physical activity with psychosocial outcomes and asthma control in adolescents: A longitudinal study. Journal of Asthma. Doi 10.3109/02770903.2014.941475
Cohen, J. L., Mann, D. M., Wisnivesky, J. P., Horne, R., Leventhal, H., Musumeci-Szabó, T. J., & Halm, E. A. (2009). Assessing the validity of self-reported medication adherence among inner-city asthmatic adults: The Medication Adherence Report Scale for Asthma. Annals of Allergy, Asthma & Immunology, 103, 325–331. doi:10.1016/S1081-1206(10)60532-7.
Buck, R. S., Hawkins, K., Skinner, T. C., Horn, S., Seddon, P., & Horne, R. (2009). Adherence to treatment in adolescents with cystic fibrosis: The role of illness perceptions and treatment beliefs. Journal of Pediatric Psychology, 34, 893–902. doi:10.1093/jpepsy/jsn135.
Rutishauser, C., Sawyer, S. M., Bond, L., Coffey, C., & Bowes, G. (2001). Development and validation of the Adolescent Asthma Quality of Life Questionnaire (AAQOL). The European Respiratory Journal, 17, 52–58.
Juniper, E. F., O’Byrne, P. M., Guyatt, G. H., Ferrie, P. J., & King, D. R. (1999). Development and validation of a questionnaire to measure asthma control. The European Respiratory Journal, 14, 902–907. doi:10.1034/j.1399-3003.1999.14d29.x.
Juniper, E. F., Gruffydd-Jones, K., Ward, S., & Svensson, K. (2010). Asthma Control Questionnaire in children: Validation, measurement properties, interpretation. European Respiratory Journal, 36, 1410–1416. doi:10.1183/09031936.00117509.
Bentler, P. M., & Bonett, D. G. (1980). Significance test and goodness-of-fit in the analysis of covariance structures. Psychological Bulletin, 88, 588–600. doi:10.1037/0033-2909.88.3.588.
Global Strategy for Asthma Management and Prevention. From the Global Strategy for Asthma Management and Prevention, Global Initiative for Asthma (GINA) 2012. http://www.ginasthma.org
McQuaid, E. L., Kopel, S. J., Klein, R. B., & Fritz, G. K. (2003). Medication adherence in pediatric asthma: Reasoning, responsibility, and behavior. Journal of Pediatric Psychology, 28, 323–333.
Nicolai, T., Illi, S., Tenborg, J., Kiess, W., & Mutius, E. (2001). Puberty and prognosis of asthma and bronchial hyper-reactivity. Pediatric Allergy and Immunology, 12, 142–148.
Sawyer, M. G., Reynolds, K. E., Couper, J. J., French, D. J., Kennedy, D., Martin, J., & Baghurst, P. A. (2004). Health-related quality of life of children and adolescents with chronic illness: A two year prospective study. Quality of Life Research, 13, 1309–1319.
Stern, D. A., Morgan, W. J., Wright, A. L., Guerra, S., & Martinez, F. D. (2007). Poor airway function in early infancy and lung function by age 22 years: A non-selective longitudinal cohort study. Lancet, 370, 758–764. doi:10.1016/S0140-6736(07)61379-8.
Bender-Benz, J., Carter, A. S., Wagiller, R. L., Horwitz, S. M., Klein-Murdock, K., & Briggs-Gowan, M. (2007). Prevalance and correlates of early onset asthma and wheezing in a healthy birth cohort of 2- to 3- year olds. Journal of Pediatric Psychology, 32, 154–166. doi:10.1093/jpepsy/jsj123.
Mosnaim, G., Hong, L., Martin, M., De Juran, R., Belice, P. J., Avery, E., & Powell, L. (2014). Factors associated with levels of adherence to inhaled corticosteroids in minority adolescents with asthma. Annals of Allergy, Asthma & Immunology, 112, 116–120. doi:10.1016/j.anai.2013.11.021.
Bosley, C. M., Fosbury, J. A., & Cochrane, G. M. (1995). The psychological factors associated with poor compliance with treatment in asthma. European Respiratory Journal, 8, 899–904. doi:10.1183/09031936.95.08060899.
Bender, B., Wamboldt, F. S., O’Connor, S. L., Rand, C., Szefler, S., Milgom, H., & Wamboldt, M. Z. (2000). Measurement of children’s asthma medication adherence by self report, mother report, canister weight, and Doser CT. Annals of Allergy, Asthma & Immunology, 85, 416–421. doi:10.1016/S1081-1206(10)62557-4.
Williams, M. V., Baker, D. W., Honig, E. G., Lee, T. M., & Nowlan, A. (1998). Inadequate health literacy is a barrier to asthma knowledge and self-care. Chest, 114, 1008–1015. doi:10.1378/chest.114.4.1008.
Cicutto, L., To, T., & Murphy, S. (2013). A randomized controlled trial of a public health nurse-delivered asthma program to elementary schools. Journal of School Health, 83(12), 876–884. doi:10.1111/josh.12106.
Broquet Ducret, C., Verga, M. E., Stoky-Hess, A., Verga, J., & Gehri, M. (2013). Impact of a small-group educational intervention for 4-to 12-year-old asthmatic children and their parents on the number of healthcare visits and quality of life. Archives de Pediatrie, 20(11), 1201–1205. doi:10.1016/j.arcped.2013.08.021.
Acknowledgments
We would like to thank all of the families who were willing to participate in this study and the Lung Foundation Netherlands who supported this study (Grant Number 3.4.09.012).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tiggelman, D., van de Ven, M.O.M., van Schayck, O.C.P. et al. Longitudinal associations between asthma control, medication adherence, and quality of life among adolescents: results from a cross-lagged analysis. Qual Life Res 24, 2067–2074 (2015). https://doi.org/10.1007/s11136-015-0945-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-015-0945-3