Abstract
Purpose
Health-related quality of life (HRQoL) is important for long-term social functioning. It is considerably reduced in patients with depression. We studied the impact of HRQoL on treatment outcome in patients with unipolar depression. Furthermore, we analysed factors associated with HRQoL in inpatients with unipolar depression.
Methods
One hundred and eighty patients suffering from major depressive disorder were evaluated during their inpatient treatment by assessing admission and discharge depression severity and their HRQoL, using the Medical Outcomes Study 12-item Short Form (SF-12). Baseline and treatment variables associated with HRQoL were examined by regression analysis. Primary outcome measures were the Hamilton Rating Scale and the Beck Depression Inventory.
Results
HRQoL improved significantly during inpatient treatment. Lower HRQoL outcomes were strongly associated with higher age, somatic comorbidities, a recurrent depressive disorder and stronger depressive symptoms at admission. Additionally, patients with a complex treatment situation (high number of medications, antidepressant switch) showed stronger impairment of HRQoL. Personality disorders and additional psychotherapy did not predict HRQoL.
Conclusion
The inpatient treatment resulted in an increase of the SF-12 scores, although to a lower extent than depressive symptoms. Several factors negatively influence HRQoL, such as the presence of somatic and axis I psychiatric comorbiditites and a recurrent or severe depressive episode. Targeting somatic comorbidities in patients with unipolar depression seem to play an important role for HRQoL.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Major depressive disorder (MDD) with a lifetime prevalence of 15 % is one of the most frequent mental disorders [1]. It causes loss of life quality, disability and is related to early death [2]. Health-related quality of life (HRQoL) is an assessment of how the individual’s well-being may be affected over time by a disease, disability or disorder [3]. HRQoL and social functioning are considerably reduced in patients suffering from depression [4–6], especially compared to the general population and patients with other chronic diseases, such as diabetes, arthritis or cardiovascular disease [7]. If patients with unipolar depression suffer from further somatic disorders, the impairment of HRQoL is even worse [8].
Ravindran et al. [9] demonstrated in a sample of depressed patients that the severity of depression influences life quality. If remission of depressive symptoms after treatment can be reached within a period of 6 month, this results in a significant higher HRQoL [10]. Furthermore, HRQoL is a predictor of treatment response and can be used to assess chronicity and relapse [11]. For example, a high impairment of psychosocial functioning is related to a more severe course of disease and higher relapse rates [4]. Also, in remitted MDD patients, especially in women, HRQoL is lower than in the general population and is inversely correlated with the degree of depressive symptoms, which emphasizes its relevance also after the decline of acute symptoms and raises implications for the intensive treatment of residual symptoms [12]. However, depression inventories only explain a small variance of HRQoL. Therefore, additional assessment of HRQoL with specific tests is recommended [13].
One aspect of HRQoL is somatic symptoms which are often present in depressed patients [14]. Increased pain in patients with MDD is associated with higher severity of depression, impaired HRQoL and a negative impact on treatment response [15]. Additionally, somatic symptoms may influence outcome of treatment for depression, hinder the full remission of depression and increase the risk of relapse [16].
For example, Bair et al. [17] found that in primary care patients, severity of pain was a strong predictor of a poor treatment response and poor HRQoL outcome at 3 months after the initiation of antidepressant therapy.
Improvement of HRQoL after initiation of treatment is related to fewer somatic symptoms at baseline, antidepressant treatment and less switching of antidepressants. The course of the disease (number of previous depressive episodes and current episode duration) was also associated with worse HRQoL outcomes [18]. In several studies, treatment resulted in a significant improvement of the mental dimension of life quality combined with a decrease of depressive symptoms [19, 20]. However, at the same time, the physical dimension of life quality did not or only marginally change during treatment of depression [6]. Contradictory studies report no significant association between HRQoL and the improvement of depressive symptoms, however, in primary care [21].
Last but not least, there is an increasing demand that HRQoL should be considered in evaluation of drug agents, e.g. antidepressants [22]. Quality of life measures assess well-being across several domains, which is important because disease-specific measures of severity of illness may not accurately represent the overall treatment effect [23]. Trials reporting the parallel measurement of efficacy of antidepressant treatment and HRQoL demonstrate that although antidepressants improve social functioning compared to placebo over a short treatment period, the endpoint scores of HRQoL are still significantly below the average in the general population [18].
Summing up, HRQoL seems to be an important parameter in evaluating the treatment outcome of depression and is important for long-term social functioning. However, study results are heterogeneous and limited in their comparability due to the variability in tools to assess HRQoL (e.g. Nottingham Health Profile (NHP); the Life-5 Dimensions (EQ-5D), the health status index (HSI); [24]). Therefore, this is the first study that examines the influence of inpatient treatment on HRQoL in a severely depressed population, its relationship to treatment response, development of depressive symptoms and possible parameters influencing HRQoL.
Methods
Participants
Patients were recruited from the psychiatric unit of the ‘Theodor-Wenzel-Werk’ clinics in Berlin, Germany. Patients were included if they had (1) a major depressive episode or recurrent depression as the principal current diagnosis according to ICD-10, (2) an age ≥18 years and (3) a score ≥15 on the 17-item version of the Hamilton Rating Scale for Depression and/or a score ≥18 on the Beck Depression Inventory (BDI) at admission, indicating a clinically relevant severity of depression in an expert- and/or a self-rating scale [25]. The study has been conducted in accordance with the current version of the Declaration of Helsinki and was approved by the local Ethics Committee. Participants were excluded from the study if they had (1) a previous history of schizophrenia, schizoaffective disorder or bipolar I disorder, (2) an acute withdrawal syndrome induced by the use of psychoactive substances or (3) language as well as concentration and thinking deficits to an extent that they could not complete the questionnaires. Furthermore, patients were excluded from the study if the depressive episode was attributable to organic illness.
Treatment
Treatment was multidisciplinary. All patients were treated with psychopharmacological medication and clinical management according to the German national clinical practice guideline for unipolar depression [26]. If indicated, patients took part in occupational therapy (92 %), sports therapy (83 %), cognitive–behavioural group therapy for depression (69 %), individual cognitive–behavioural therapy (54 %), motion therapy (41 %), music therapy (25 %), cognitive–behavioural group therapy for anxiety disorders (19 %), progressive muscle relaxation training (20 %), addiction therapy (8 %), art therapy (5 %) and light therapy (2 %). The inpatient treatment lasted an average of 57.6 ± 28.4 days.
Assessment
The diagnosis of a major depressive episode or a recurrent depression was given by the attending psychiatrist using the International Diagnostic Checklist for ICD-10 and DSM-IV for Depressive Episodes (IDCL [27]). To measure depression severity, the 17-item version of the Hamilton Rating Scale for Depression (HRSD [28]; clinician-rated) and the BDI([29]; self rating, higher scores demonstrate higher depressive symptom severity) were used. Additionally, the Global Assessment of Functioning Scale (GAF [30]) and the Clinical Global Impression Scale (CGI [31]) were used. The HRSD was administered by an experienced clinical psychologist. The GAF and CGI were administered by the attending psychiatrist who received training in the use of the IDCL, GAF and CGI. The assessment of personality disorders was performed using the structured clinical interview for DSM-IV personality disorders (SCID II) and was conducted by trained and experienced clinical psychologists 3 weeks after admission [32]. All symptom ratings were performed within 4 days after admission and 4 days before discharge. All raters were given training and supervision to perform clinician-rated assessment procedures (HRSD, CGI, GAF, SCID II), which are collected routinely. The HRSD is a sum score, whereas the CGI is a 7-point scale, the GAF is a numeric scale (1 through 100) and the SCID II a structured diagnostic interview with self- and clinician-rated parts. Information about comorbid axis I disorders and treatments were gained by chart review post-treatment.
Measurement of HRQoL
We measured the HRQoL using the Medical Outcomes Study 12-item Short Form (SF-12). Derived from the SF-36, the SF-12 is a self-administered questionnaire and measures two components of life quality, physical health (the PCS-12 Scale) and mental health (the MCS-12 Scale) functioning, without substantial loss of information, compared to its longer form the SF-36 [33]. There are good experiences with the SF-12 for psychiatric patients [34]. The PCS-12 items include an assessment of the participant’s self report on the level of limitation experienced in performing moderate activities, climbing stairs, accomplishing less due to physical health impairments, the experience of bodily pain and a rating of general health. The MCS-12 items include questions on feeling calm and peaceful, downhearted and blue, accomplishing less and doing activities less carefully than usual because of one’s mental health. Higher scores in the respective summary scales represent higher levels of functioning [35].
Outcome measures
Outcome was operationalized as: (1) baseline-to-discharge change in symptom severity scores, (2) symptom severity scores at discharge and (3) percentage of patients meeting remission criteria. Remission was defined as a HRSD17 score <8 and a BDI score <11. For the CGI, remission was defined as a value of 2 in the subscale therapeutic effect. For the GAF, values with 70 were equated with a sufficient level of functional gain [36].
Statistical analysis
For parametric variables, analysis of variance (ANOVA) for repeated measures were used to analyse differences in changes in symptom severity (HRSD, BDI, CGI, GAF) and the HRQoL (PCS-12 and MCS-12) from admission to discharge for all patients. We also computed Cohen’s d as a measure of the pre–post effect size. According to the criteria of Cohen’s classification, .2 is small, .5 is medium and .8 is large effect size [37].
Backward regression analysis was performed to identify variables independently associated with HRQoL outcomes. Separate models were fitted for each of the following outcome variables: SF-12 mental component summary (MCS-12) and physical component summary (PCS-12) for discharge. Independent variables were removed from the full model until only statistically significant (p ≤ .05) variables remained.
Independent variables in the model included at baseline were: age, gender, education, occupational status, marital status (see Table 1), chronicity of depression (first vs. recurrent depressive episode), duration of treatment, HRDS, BDI, CGI, GAF at (1) admission and at (2) discharge, somatic comorbidities (yes/no), additional psychotherapy (yes/no), psychiatric comorbidities (yes/no), additional personality disorder, number of medications, class of antidepressant taken between baseline and discharge, switch of antidepressants during treatment. For all independent variables included in the analysis, relevance for HRQoL has been demonstrated in previous studies (e.g. [24]).
All statistical tests were two-tailed, with an alpha level of .05. All the data were examined using SPSS for Windows, version 16.0.
Results
Attrition
Two hundred and eighty-three patients were included in the study. A total of 103 patients (22 %) were not considered as completers, because their treatment duration was <21 days (3 weeks is considered to be the minimum time necessary for treatment response [26]), they did not fulfill inclusion criteria, or they did not complete the post-treatment evaluation. Hence, the following analyses are based on the 180 patients. χ 2 and t tests show no significant differences between included patients and patients that dropped out with regard to age, gender distribution, marital and educational status as well as symptom severity at intake (BDI, HRSD) or HRQoL (SF-12).
Subject characteristics
The mean age of the sample was 52.2 ± 13.3 years. 61.1 % (n = 110) were women, 47.2 % (n = 85) were married and 49.5 % (n = 94) had a university degree (Table 1). At admission, the mean HRSD score was 29.5 ± 7.9, and the mean BDI score was 27.2 ± 10.1. Furthermore, the GAF mean score was 46.3 ± 10.1, and the CGI mean score was 5.45 ± .7.
Data on the SF-12 were available from 180 patients. The mean PCS score was 41.8 ± 10.3, and the mean MCS score 26.4 ± 8.1. 43.3 % of patients reported their health was in general fair or poor (item one in SF-12). Pain interference was reported to be moderate to extreme by 53.3 %, mild by 28.9 % and absent by 17.8 % (item 8). In the past 4 weeks, physical or emotional problems interfering with social activities were present all or most of the time in 23.9 % of patients (item 12).
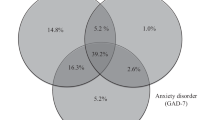
40.6 % (n = 73) had a recurrent depressive disorder, 38.9 % (n = 70) met criteria for at least one comorbid axis I disorder. The most frequent comorbid axis I disorders were ICD-10 F1 Mental and behavioural disorders due to psychoactive substance use (11.7 %, n = 21) and ICD-10 F4 Neurotic, stress-related and somatoform disorders (24.4 %, n = 44). 36.1 % (n = 65) of patients also met the criteria for at least one personality disorder (Table 1). The prescribed psychiatric medication is displayed in Table 2. A total of 108 patients (60.3 %) had at least one somatic comorbidity (Table 3).
Treatment outcome
For the inpatient treatment, there was a significant effect of time for the HRSD (F [1, 180] = 1,023.3, p < .001), the BDI (F [1, 180] = 361.72, p < .001), the GAF (F [1, 180] = 346.35, p < .001) and the CGI (F [1, 180] = 456.1, p < .001), pre–post means and effect sizes are displayed in Table 4). The response rates for the HRSD were 82.7 % and for the BDI 58.9 %. 61.1 % of the patients in the HRSD and 56.6 % in the BDI achieved remission criteria.
On the SF-12, the physical health (PCS; F [1, 180] = 113.7, p > .01) and mental health MCS, (F [1, 180] = 269.1, p < .001) scores showed a significant increase during inpatient treatment. Regarding effect sizes d for repeated measures from admission to discharge, all instruments demonstrated high effect sizes from admission to discharge (HRSD: d = 2.9; BDI: d = 1.4; GAF: d = 1.8). The effect sizes of the MCS improvement were greater than those of PCS (MCS: d = 1.6, PCS: d = .4).
Psychosocial factors and HRQoL
The results of the stepwise regression analysis are displayed in Table 5. Severity of depression (HRSD, BDI) at admission (t1) predicted HRQoL at discharge (t2). Higher symptom scores of the HRSD and the BDI at t1 predicted lower SF-12 scores at t2 [MCS estimate for HRSD of −1.49, 95 % CI (−4.27 to −.94), p = .03; MCS estimate for BDI of −.91, 95 % CI (−6.31 to −.64); p = .04; PCS estimate for HRSD −1.39, 95 % CI (−3.47 to −1.22), p = .04; PCS estimate for BDI −.83, 95 % CI (−7.81 to .80), p = .06]; however, there was only a statistic trend (p < .1) for the BDI predicting the PCS score.
Patients with higher impairment of overall functioning at t1 also had significantly lower MCS scores at t2 [MCS estimate for GAF −1.27, 95 % CI (−3.88 to −.17), p = .05; PCS estimate for GAF −1.01, 95 % CI (−3.24 to .49), p = .07]. Further variables related with depression severity, such as the recurrence of depressive episodes and the duration of the current depressive episode, were consistently associated with worse HRQoL at t2 (see Table 5): PCS score at t2 was inversely associated with the diagnosis of a recurrent depressive disorder [PCS estimate for recurrence −1.42, 95 % CI (−5.32 to −.89), p = .04]. Also, the recurrence of depression [MCS estimate for recurrence −1.31, 95 % CI (−5.27 to −.69), p = .04] as well as longer duration of the inpatient treatment [MCS estimate for duration −1.75, 95 % CI (−4.21 to −1.13), p = .04] were associated with a lower MCS score at t2. Also, somatic diseases predicted lower MCS and PCS scores at discharge [MCS estimate for somatic comorbidity −1.84, 95 % CI (−5.48 to −1.01), p = .03; PCS estimate for somatic comorbidity −1.93, 9 % CI (−6.14 to −1.11), p = .02]. Also, age predicted significantly a stronger impairment of the PCS [PCS estimate for age −1.58, 95 % CI (−4.82 to −.61), p = .04]. Patients with comorbid psychiatric axis I disorders had lower HRQoL in the MCS (tendency) and in the PCS compared to patients without psychiatric comorbidities [MCS estimate for psychiatric comorbidity −1.52, 95 % CI (−3.26 to −.57), p = .07; PCS estimate for psychiatric comorbidity −1.59, 95 % CI (−5.59 to −1.38), p = .03]. Comorbid personality disorders did not predict the HRQoL at discharge (Table 5).
Treatment factors and HRQoL
Results of the regression analysis show that patients receiving additional CBT did not differ regarding HRQoL at t2 compared to patients receiving only pharmacotherapy (see Table 5). Switching treatment within AD was consistently associated with a lower HRQoL at t2 [MCS estimate for switch −.76, 95 % CI (−4.57 to −.14), p = .05; PCS estimate for switch −.69, 95 % CI (−6.32 to −.43) p = .05], compared to the group that did not switch AD. There were no differences in HRQoL at t2 regarding the type of the antidepressant (see Table 5). Also, the number of medication at discharge was associated with a lower HRQoL [MCS estimate for number of medication −1.95; 95 % CI (−9.13 to −1.62), p = .04; PCS estimate for number of medication −1.87, 95 % CI (−8.89 to −.79), p = .02] at discharge.
Discussion
In this trial, we could verify that the multidisciplinary inpatient treatment of depression improves HRQoL, although to a lower extent than depressive symptoms.
Furthermore, several factors were negatively related to HRQoL, such as the presence of somatic and axis I psychiatric comorbidities and a recurrent or severe depressive episode.
Depression is often associated with reductions in HRQoL and disturbed social functioning. In this study, patients improved during inpatient treatment with regard to HRQoL as well as depression severity and global functioning. Overall response (HRSD: 84.4 %, BDI: 58.9 %) and remission rates (HRSD: 63.4 %, BDI: 54.4 %) were relatively high. The results are comparable to those of other effectiveness studies measuring the quality as well as effectiveness of inpatient treatment of depression [38].
Regarding HRQoL, measured by using the SF-12 and its subscales, we found comparable impairment of HRQoL to similar studies at admission (PCS: M = 41.8; MCS: M = 26.4 vs. PCS: M = 44.9; MCS: M = 22.0; Finder-trial, [20]). Furthermore, we could verify a moderate relationship of the severity of depression (HRSD, BDI) and the amount of impairment in the SF-12 at admission [39].
During inpatient treatment, HRQoL scores increased significantly in both subscales of the SF-12. Effect sizes were moderate to high (MCS: d = 1.6, PCS: d = .4). In the European observational study EUFINDER, the changes of HRQoL were observed in outpatients with a depressive episode receiving pharmacological treatment in routine primary care. Treatment with antidepressants was associated with large improvements in HRQoL, assessed by the SF-36 and the EQ-5D [18, 40, 41]. The overall improvement in HRQoL during treatment in our study is also in line with several other studies [18, 42, 43]. Although a considerable number of patients reached remission in the HRSD and the BDI, after inpatient treatment the impairment of HRQoL was still higher compared to non-depressed subjects, especially on the PCS. This indicates that impaired social functioning persists even after remission of depression [44], and that residual depressive symptoms are associated with enduring psychosocial impairment [45].
We could also demonstrate that high depression scores at baseline (HRDS, BDI) were significantly associated with a worse HRQoL outcome at discharge. This is comparable to several other studies [40, 46] also reporting a decline of life quality with increasing symptom severity in depressed patients.
In the reported regression analysis, several depression-related factors (longer duration of the current depressive episode and a recurrent depressive disorder) were associated with a poorer HRQoL outcome [39]. Age was specifically related to a reduced PCS score, which can be explained by an increasing number of disabling somatic comorbidities at higher ages.
What is notable is that the HRQoL impairment at baseline and the improvements during treatment were higher on the MCS subscale of the SF-12 than on the PCS subscale. This is comparable to the FINDER study [18] and is probably associated with a strong negative relationship of physical illnesses and HRQoL and specifically on the PCS score, a fact that can hardly be changed during psychiatric inpatient treatment. Accordingly, we could confirm that an increasing number of somatic comorbidities were associated with both poorer physical as well as mental functioning in the SF-12 at discharge. A recent study of Lim et al. [8] could prove that the individual effects of medical and psychiatric morbidity on functional status and quality of life were considerably worse when both were present in the same individual. Interestingly, the authors even report that physical and mental disorders in their combined presence were highly disabling, much more than the sum of their individual effects (non-additive interactive effects). These results emphasize the need of a careful treatment of somatic diseases in psychiatric patients.
In a recent study of Reed et al. (2009), switching antidepressants was also associated with low HRQoL, compared to not switching antidepressant treatment. We could also verify that the number of changes in medication (either switch, combination or augmentation strategies) were associated in a reduced HRQoL at discharge, compared to patients receiving a monotherapy without switching. However, we could not find differences of a change between an AD-class (e.g. SSRI → SSRI) or a non-between AD class switch (e.g. SSRI → SNRI) as Reed et al. (2009) could find (favouring a non-between-class switch). Nevertheless, we could also demonstrate that switching and combining antidepressants is related to a lower HRQoL at discharge, compared to the augmentation of antidepressants with lithium or antipsychotics [47], a finding that is in line with other controlled studies [48].
Our findings indicate the usefulness of the SF-12 in quantifying HRQoL. The SF-12 has proven to be an effective indicator of physical and mental health functioning. Nevertheless, the importance of assessing the relationship of depression severity and HRQoL has only recently been recognized. Social functioning has become of increasing importance regarding the treatment and outcome assessment of psychiatric disorders. Several authors argue that HRQoL should be included in the definitions of remission to emphasize that the improvement in psychosocial functioning is a relevant parameter ensuring remission [23]. Especially, the additional intensified treatment of somatic comorbidities may be helpful to further reduce depressive symptoms and achieve higher social functioning.
Further research is needed to evaluate the long-term meaning of HRQoL in patients with depression, for example, the relationship with relapse rates or social functioning. Additionally, it could be interesting to address HRQoL specifically in the inpatient treatment programme (e.g. psychoeducation). Altogether, HRQoL should be investigated as an explicit outcome parameter for treatment of unipolar depression in addition to the depressive symptom scores.
Methodological limitations
There are a number of limitations to this work that need to be acknowledged. In this study, we examined a depressed inpatient sample. Inpatients are generally more severely depressed than outpatients. Therefore, our results cannot be generalized to depressed outpatients. Regarding the generalizability of our results, it is also important to note restrictively that the patient group in our study was highly educated (53 % with a university degree) and that the average duration of inpatient treatment (59 days) was quite high. A further limitation concerns the naturalistic design of our study: Treatment was not standardized and depended on each patients´ needs in accordance with the German national clinical practice guideline for unipolar depression [26]. The multidisciplinary approach may have had unintended effects on the study variables. During the inpatient treatment, depressed patients have received different interventions (e.g. medication, different types of individual and group psychotherapy, physiotherapy). This can affect the interpretation of the results as it is very difficult to separate the specific effect of the different intervention approaches. Additionally, we only used the SF-12 to assess HRQoL and no further instruments, which is a major shortcoming. There are some relevant limitations of regression analysis, which also should be taken into consideration: First of all, logistic regression needs a huge sample size, especially if there is a large number of independent variables. Small sample sizes can lead to widely inaccurate estimates of parameters. There also several assumptions which have to be fulfilled that logistic regression can be used. And last but not least, correlations and regression do not allow making statements about causality.
Conclusion
Multiprofessional inpatient treatment improves HRQoL in patients with depression, although to a lower extent than depressive symptoms. Somatic and axis I psychiatric comorbidities negatively influence HRQoL. Targeting somatic comorbidities in patients with unipolar depression seems to play an important role for HRQoL and should be focussed during treatment. HRQoL measurement is a meaningful concept in addition to the concept of depressive symptom response and remission.
References
Kessler, R. C., Berglund, P., Demler, O., Jin, R., Merikangas, K. R., & Walters, E. E. (2005). Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry, 62(6), 593–602.
Lopez, A. D., Mathers, C. D., Ezzati, M., Jamison, D. T., & Murray, C. J. (2006). Global and regional burden of disease and risk factors, 2001: Systematic analysis of population health data. Lancet, 367(9524), 1747–1757.
Center for Control Disease and Prevention. (2014). Retrieved from http://www.cdc.gov/hrqol/concept.htm.
Hirschfeld, R. M., Montgomery, S. A., Keller, M. B., Kasper, S., Schatzberg, A. F., Moller, H. J., et al. (2000). Social functioning in depression: A review. Journal of Clinical Psychiatry, 61(4), 268–275.
Angermeyer, M. C., Holzinger, A., Matschinger, H., & Stengler-Wenzke, K. (2002). Depression and quality of life: Results of a follow-up study. International Journal of Social Psychiatry, 48(3), 189–199.
Berlim, M. T., Pargendler, J., Brenner, J., & Fleck, M. P. (2007). Significant improvement in the quality of life of Brazilian depressed outpatients 12 weeks following the start of antidepressants. Psychiatry Research, 153(3), 253–259.
Moussavi, S., Chatterji, S., Verdes, E., Tandon, A., Patel, V., & Ustun, B. (2007). Depression, chronic diseases, and decrements in health: Results from the World Health Surveys. Lancet, 370(9590), 851–858.
Lim, L., Jin, A. Z., & Ng, T. P. (2012). Anxiety and depression, chronic physical conditions, and quality of life in an urban population sample study. Social Psychiatry and Psychiatric Epidemiology, 47(7), 1047–1053.
Ravindran, A. V., Matheson, K., Griffiths, J., Merali, Z., & Anisman, H. (2002). Stress, coping, uplifts, and quality of life in subtypes of depression: A conceptual frame and emerging data. Journal of Affective Disorders, 71(1–3), 121–130.
Sobocki, P., Ekman, M., Agren, H., Runeson, B., & Jonsson, B. (2006). The mission is remission: Health economic consequences of achieving full remission with antidepressant treatment for depression. International Journal of Clinical Practice, 60(7), 791–798.
Pyne, J. M., Bullock, D., Kaplan, R. M., Smith, T. L., Gillin, J. C., Golshan, S., et al. (2001). Health-related quality-of-life measure enhances acute treatment response prediction in depressed inpatients. Journal of Clinical Psychiatry, 62(4), 261–268.
ten Doesschate, M. C., Koeter, M. W., Bockting, C. L., & Schene, A. H. (2010). Health related quality of life in recurrent depression: A comparison with a general population sample. Journal of Affective Disorders, 120(1–3), 126–132.
Rapaport, M. H., Clary, C., Fayyad, R., & Endicott, J. (2005). Quality-of-life impairment in depressive and anxiety disorders. American Journal of Psychiatry, 162(6), 1171–1178.
Kroenke, K. (2003). Patients presenting with somatic complaints: Epidemiology, psychiatric comorbidity and management. International Journal of Methods in Psychiatric Research, 12(1), 34–43.
Tylee, A., & Gandhi, P. (2005). The importance of somatic symptoms in depression in primary care. Primary Care Companion to the Journal of Clinical Psychiatry, 7(4), 167–176.
Judd, L. L., Akiskal, H. S., Maser, J. D., Zeller, P. J., Endicott, J., Coryell, W., et al. (1998). Major depressive disorder: A prospective study of residual subthreshold depressive symptoms as predictor of rapid relapse. Journal of Affective Disorders, 50(2–3), 97–108.
Bair, M. J., Robinson, R. L., Eckert, G. J., Stang, P. E., Croghan, T. W., & Kroenke, K. (2004). Impact of pain on depression treatment response in primary care. Psychosomatic Medicine, 66(1), 17–22.
Reed, C., Monz, B. U., Perahia, D. G., Gandhi, P., Bauer, M., Dantchev, N., et al. (2009). Quality of life outcomes among patients with depression after 6 months of starting treatment: Results from FINDER. Journal of Affective Disorders, 113(3), 296–302.
Matsunaga, M., Okamoto, Y., Suzuki, S., Kinoshita, A., Yoshimura, S., Yoshino, A., et al. (2010). Psychosocial functioning in patients with treatment-resistant depression after group cognitive behavioral therapy. BMC Psychiatry, 10, 22.
Caruso, R., Rossi, A., Barraco, A., Quail, D., & Grassi, L. (2010). The Factors Influencing Depression Endpoints Research (FINDER) study: Final results of Italian patients with depression. Annals of General Psychiatry, 9, 33.
Wells, K. B., Sherbourne, C., Schoenbaum, M., Duan, N., Meredith, L., Unutzer, J., et al. (2000). Impact of disseminating quality improvement programs for depression in managed primary care: A randomized controlled trial. JAMA, 283(2), 212–220.
Bech, P. (2005). Social functioning: Should it become an endpoint in trials of antidepressants? CNS Drugs, 19(4), 313–324.
Trivedi, M. H. (2001). Sensitizing clinicians and patients to the social and functional aspects of remission. Journal of Clinical Psychiatry, 62(Suppl 19), 32–35.
Wisniewski, S. R., Rush, A. J., Bryan, C., Shelton, R., Trivedi, M. H., Marcus, S., et al. (2007). Comparison of quality of life measures in a depressed population. The Journal of Nervous and Mental Disease, 195(3), 219–225.
Frank, E., Prien, R. F., Jarrett, R. B., Keller, M. B., Kupfer, D. J., Lavori, P. W., et al. (1991). Conceptualization and rationale for consensus definitions of terms in major depressive disorder. Remission, recovery, relapse, and recurrence. Archives of General Psychiatry, 48(9), 851–855.
Härter, M., Klesse, C., Bermejo, I., Schneider, F., & Berger, M. (2010). Unipolar depression: Diagnostic and therapeutic recommendations from the current S3/National Clinical Practice Guideline. Deutsches ärzteblatt International, 107(40), 700–708.
Hiller, W., Zaudig, M., & Mombour, W. (2005). IDCL: ICD-10 Checklists. Göttingen: Hogrefe.
Hamilton, M. (1960). A rating scale for depression. Journal of Neurology, Neurosurgery and Psychiatry, 23, 56–62.
Beck, A. T., Ward, C. H., Mendelson, M., Mock, J., & Erbaugh, J. (1961). An inventory for measuring depression. Archives of General Psychiatry, 4, 561–571.
Endicott, J., Spitzer, R. L., Fleiss, J. L., & Cohen, J. (1976). The global assessment scale. A procedure for measuring overall severity of psychiatric disturbance. Archives of General Psychiatry, 33(6), 766–771.
Guy, W. (1976). Clinical Global Impressions (CGI). In: ECDEU Assessment Manual for Psychopharmacology US Department of Health, Education, and Welfare Publication (ADM) 76–338 (pp. 218–222). Rockville, MD: National Institute of Mental Health.
First, M., Gibbon, M., & Spitzer, R. (1996). Structured clinical interview for DSM-IV axis II disorders. New York NY: Biometrics Research Dept, NewYork State Psychiatric Institute.
Ware, J, Jr, Kosinski, M., & Keller, S. D. (1996). A 12-Item Short-Form Health Survey: Construction of scales and preliminary tests of reliability and validity. Medical Care, 34(3), 220–233.
Collegium Internationale Psychiatriae Scalarum (CIPS). (2005). Internationale Skalen für Psychiatrie. Göttingen: Beltz Test.
Ware, J. E., Kosinski, M., & Keller, S. D. (1995). SF-12: How to score the SF-12 physical and mental health summary scales (2nd ed.). Boston: The Health Institute, New England Medical Center.
CIPS. (2005). International scales for psychiatry. Göttingen: Beltz Test GmbH.
Cohen, J. (1992). A power primer. Psychological Bulletin, 112(1), 155–159.
Seemüller, F., Riedel, M., Obermeier, M., Bauer, M., Adli, M., Kronmüller, K., et al. (2010). Outcomes of 1014 naturalistically treated inpatients with major depressive episode. European Neuropsychopharmacology, 20(5), 346–355.
Daly, E. J., Trivedi, M. H., Wisniewski, S. R., Nierenberg, A. A., Gaynes, B. N., Warden, D., et al. (2010). Health-related quality of life in depression: A STAR*D report. Annals of Clinical Psychiatry, 22(1), 43–55.
Garcia-Campayo, J., Ayuso-Mateos, J. L., Caballero, L., Romera, I., Aragones, E., Rodriguez-Artalejo, F., et al. (2008). Relationship of somatic symptoms with depression severity, quality of life, and health resources utilization in patients with major depressive disorder seeking primary health care in Spain. Primary Care Companion to the Journal of Clinical Psychiatry, 10(5), 355–362.
Bauer, M., Monz, B. U., Montejo, A. L., Quail, D., Dantchev, N., Demyttenaere, K., et al. (2008). Prescribing patterns of antidepressants in Europe: Results from the Factors Influencing Depression Endpoints Research (FINDER) study. European Psychiatry, 23(1), 66–73.
Peveler, R., Kendrick, T., Buxton, M., Longworth, L., Baldwin, D., Moore, M., et al. (2005). A randomised controlled trial to compare the cost-effectiveness of tricyclic antidepressants, selective serotonin reuptake inhibitors and lofepramine. Health Technol Assess, 9(16), 1–134, iii.
Dunner, D. L., Kwong, W. J., Houser, T. L., Richard, N. E., Donahue, R. M., & Khan, Z. M. (2001). Improved health-related quality of life and reduced productivity loss after treatment with bupropion sustained release: A study in patients with major depression. Primary Care Companion to the Journal of Clinical Psychiatry, 3(1), 10–16.
Kruijshaar, M. E., Hoeymans, N., Bijl, R. V., Spijker, J., & Essink-Bot, M. L. (2003). Levels of disability in major depression: Findings from the Netherlands Mental Health Survey and Incidence Study (NEMESIS). Journal of Affective Disorders, 77(1), 53–64.
Kennedy, N., Foy, K., Sherazi, R., McDonough, M., & McKeon, P. (2007). Long-term social functioning after depression treated by psychiatrists: A review. Bipolar Disorders, 9(1–2), 25–37.
Trivedi, M. H., Rush, A. J., Wisniewski, S. R., Warden, D., McKinney, W., Downing, M., et al. (2006). Factors associated with health-related quality of life among outpatients with major depressive disorder: A STAR*D report. Journal of Clinical Psychiatry, 67(2), 185–195.
Köhler, S., Unger, T., Hoffmann, S., Steinacher, B., Fydrich, T., & Bschor, T. (2013). Comparing augmentation with non-antidepressants over sticking to antidepressants after treatment failure in depression: A naturalistic study. Pharmacopsychiatry, 46(2), 69–76.
Ruhe, H. G., Huyser, J., Swinkels, J. A., & Schene, A. H. (2006). Switching antidepressants after a first selective serotonin reuptake inhibitor in major depressive disorder: A systematic review. Journal of Clinical Psychiatry, 67(12), 1836–1855.
Conflict of interest
There are no competing financial interests in relation to the work described.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Köhler, S., Unger, T., Hoffmann, S. et al. The relationship of health-related quality of life and treatment outcome during inpatient treatment of depression. Qual Life Res 24, 641–649 (2015). https://doi.org/10.1007/s11136-014-0811-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-014-0811-8