Abstract
Examine the unmet needs of people with serious mental illness (SMI) from the perspective of certified peer specialists. 267 certified peer specialists from 38 states completed an online survey (female [73%], 50.9 [SD = 12] years, and non-Hispanic White [79.8%]). Many respondents reported a primary mental health diagnoses (n = 200), 22 respondents reported their diagnosis as schizophrenia spectrum disorder (11%), 46 respondents reported bipolar disorder (22.1%), 47 respondents reported major depressive disorder (22.6%), 29 respondents reported post-traumatic stress disorder (13.9%), 27 respondents reported alcohol/substance use disorder (13%), 2 respondents reported personality disorder (1%), and 12 reported “other” (5.8%). A mixed methods convergence analysis integrated quantitative with qualitative data. Social isolation (n = 160, 59.9%) and feeling lonely (n = 159, 59.6%) were the most highly endorsed unmet need, followed by the need to address chronic health conditions (n = 80, 30%), prevent mental health hospitalization (n = 71, 23.6%), and prevent drug use (n = 66, 24.7%). Four themes emerged: need to address basic necessities, loneliness and social isolation, hope, and addiction. Addressing loneliness and social isolation were identified as the primary unmet needs among people with SMI. Addressing co-morbid health conditions may simultaneously impact other unmet needs. Hope is an important intervention target. Initial insights from this study can be used to guide researchers’ efforts to incorporate certified peer specialists perspectives in developing programs to meet the needs of people with SMI. Future research using participatory research methods can further examine these initial insights.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Impact and Implications
This study examined the unmet needs of people with SMI from the perspective of certified peer specialists. Addressing loneliness and social isolation were identified as unmet needs among people with SMI. Certified peer specialists emphasized the need to address chronic health conditions and prevent drug use among people with SMI. Hope was identified as an important intervention target. Initial insights from this study can be used to guide researchers’ efforts to incorporate certified peer specialists perspectives in developing programs to meet the needs of people with SMI.
Introduction
To address the unmet needs of people with serious mental illness (SMI), both consumers with SMI [1] and national institutes [2] have called for the “co-production of research”. Co-production of research is a practice, in which community members work with professionals as equals in every stage of program development to make services more applicable for communities [3]. Considering the potential of co-production to promote social action and policy reform, including certified peer specialists who represent a large portion of the mental health workforce could bring new energy to addressing unmet needs of consumers with SMI.
Certified peer specialists provide Medicaid reimbursable mental health services and have a unique insight into consumers’ perspective—as they also use mental health services themselves. For example, social impacts on an individuals’ health is based on a complex, interconnected system that not only includes biological and psychological systems but also physical and social environments. As such, certified peer specialists can provide invaluable perspectives towards identifying the unmet needs of similar groups within the context of their own socio-physical environments. The purpose of this report is to examine the unmet needs of people with SMI from the perspective of certified peer specialists.
Methods
A national online survey was developed by the first author (KF) and last author (MS) in consultation with five certified peer specialists from four different states (MA, NH, AZ, PA) to ascertain their perspectives on identifying unmet needs among people with SMI. The first author piloted the online survey with three certified peer specialists to identify additional modifications. Modifications included incorporating homelessness and drug use as potential pressing issues and changing the grade level of the survey from 8th grade level to 4th grade level using the Flesch–Kincaid grade level readability test.
We used a parallel convergent mixed methods design (i.e., qualitative and quantitative data are collected simultaneously analyzed independently, and data is combined to produce an in-depth examination of the research topic) [4]. Respondents were asked to “rank the issues impacting people with mental illness in order of what you think is the most pressing issue?”. Possible responses were derived from input from certified peer specialists and included the following: “being lonely”, “being able to schedule an appointment with a doctor”, “being able to afford health insurance”, “chronic health conditions (like diabetes or obesity)”, “drug use”, “dying early (around 50 years old)”, “homelessness”, “mental health hospitalizations”, “not having any friends or family around (social isolation)”, “physical health hospitalizations”, and “Other”. Respondents who responded “other” were encouraged to include text on issues impacting people with mental illness. Their notes were systematically recorded and analyzed alongside the qualitative interviews.
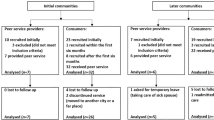
Study eligibility included: (1) peer support certification, (2) residence in the United States, and (3) an age of at least 18 years or older. From February 2018 to April 2018, respondents were invited to participate in the survey via announcements posted on websites, e-mail lists, and newsletters associated with certified peer specialist organizations. A total of 289 respondents started the survey, with 22 respondents (<10%) excluded from the final dataset due to missing data. The final sample size was 267 respondents, of whom responded and ranked the issues impacting people with SMI. Thirty-eight people from this sample also provided “other” qualitative responses. All 267 were included in the analysis.
The Institutional Review Board approved this study. Respondents were recruited to complete the 20-min online survey on the Qualtrics platform. Prior to beginning the survey, the survey homepage included an informed consent with information on the study purpose including the voluntary and confidential nature of the survey.
Analytic Plan
We used descriptive statistics to characterize the sample. All analyses were performed using SAS 9.4. Qualitative data analysis was informed by the “grounded theory” approach [5]. The codebook consisted of codes inductively derived from qualitative data [5]. The first (KF) and fourth author (AW) read qualitative data. Codes were independently assigned to text, grouped, and checked for themes. Thematic analysis was used to organize themes. Analyses included within group consensus or disagreement. Member checking with two certified peer specialists was used to verify and/or resolve any incongruent findings.
Results
A total of 267 certified peer specialists completed the survey. On average, the respondents were female (73%), 50.9 (SD = 12) years of age, and non-Hispanic White, (79.8%). Of which, more than half (n = 184, 82.1%) were currently working as a certified peer specialist. Many reported a primary mental health diagnoses (n = 200), 22 respondents reported their diagnosis as schizophrenia spectrum disorder (11%), 46 respondents reported bipolar disorder (22.1%), 47 respondents reported major depressive disorder (22.6%), 29 respondents reported post-traumatic stress disorder (13.9%), 27 respondents reported alcohol/substance use disorder (13%), 2 respondents reported personality disorder (1%), and 12 reported “other” (5.8%).
Quantitative Data
Social isolation (n = 160, 59.9%) and feeling lonely (n = 159, 59.6%) were the most highly endorsed unmet needs, followed by the need to address chronic health conditions (n = 80, 30%), preventing mental health hospitalization (n = 71, 23.6%), and preventing drug use (n = 66, 24.7%). The least endorsed unmet needs included helping consumers schedule medical and psychiatric appointments (n = 49, 18.4%), preventing consumers from dying young (n = 27, 10.1%), and preventing physical health hospitalizations (n = 12, 4.5%).
Qualitative Data
“Other” responses were used to provide depth into identifying unmet needs impacting people with SMI. Four themes emerged from the “other” responses, including the need to address basic necessities, loneliness and social isolation, promote hope, and addiction (emerging theme).
Basic necessities were described as access to adequate safe housing, food, clothing, services, transportation, and community resources. The second theme, loneliness and social isolation, arose from respondents’ accounts of being socially isolated. One respondent wrote “it is the ‘dispiritedness’ or dis-connectedness from meaningful relational living that most characterizes the suffering of individuals with substance use and/or mental health disabilities”. The third theme of hope encompassed respondents’ feelings of finding hope in their own recovery and the need to include “hope” as study outcomes. One respondent wrote “finding HOPE that life could be different….clinical/funder type of outcomes don’t usually happen due to lack of hope.” Addiction was identified as an emerging theme.
Convergence of Quantitative and Qualitative Data
The mixed methods convergence analysis provided further exploration into the perceptions of certified peer specialists. Quantitative data indicated that social isolation and loneliness were identified as the main unmet needs. Qualitative data confirmed this conclusion, and certified peer specialists proposed social skill training as a potential solution. Both quantitative and qualitative data indicated that addiction was an issue and suggested the integration of substance use, primary care, and mental health services. Unmet needs not identified in the quantitative data emerged from the qualitative data including the need for basic necessities and the need to examine “hope” as an intervention outcome.
Conclusions and Implications for Practice
This study examined the unmet needs of people with SMI from the perspective of certified peer specialists. Addressing loneliness and social isolation were identified as unmet needs among people with SMI. Certified peer specialists emphasized the need to address chronic health conditions and prevent drug use among people with SMI. Hope was identified as an important intervention target. Initial insights from this study can be used to guide researchers’ efforts to incorporate certified peer specialists perspectives in developing programs to meet the needs of people with SMI.
Loneliness was identified as the leading unmet need among people with SMI. People with SMI experience loneliness at approximately twice the rate of the general population [6]—due to impaired social skills, lack of opportunities to participate in social activities, and social stigma linked to mental illness [6]. Loneliness is an often unrecognized social determinant of health that has serious implications for cardiovascular health and mortality [7]. Loneliness is a modifiable risk factor, and thus, a potential intervention target. Certified peer specialists recommended relationship building skills, which is an accepted strategy to address loneliness in people with SMI [6]. As certified peer specialists potentially have lived experience with loneliness and relationship building skills to the world outside of the clinical mental health environment, they may be the ideal person to support consumers in addressing loneliness; however, limited research has been conducted on interventions that address loneliness among people with SMI.
Addressing social isolation among people with SMI is of great importance to certified peer specialists. While loneliness and social isolation may be experienced side-by-side, they are not synonymous. Social isolation is when an individual has no physical connection to other members of society [8]. A significantly higher proportion of people with SMI experience social isolation compared to the general population [9]—commonly due to stigma, alienation, and loneliness [10]. Social isolation reduces quality of life and also exacerbates physical health conditions [10]. As health technology interventions such as virtual reality, asynchronous smartphone applications, anonymous text messaging are emerging as treatment options that rely on machine algorithms to interact with consumers, intervention researchers should consider the importance of human connection for people with SMI.
Certified peer specialists prioritized the need to address co-morbid health conditions among people with SMI. Compared to the general population, adults with SMI are disproportionately impacted by medical comorbidities and have a decreased life expectancy of 11–30 years primarily due to these comorbidities [11]. Addressing co-morbid health condition will simultaneously impact other unmet needs identified by certified peer specialists (i.e., early death, mental health hospitalizations, and physical health hospitalizations). Research in peer-supported integrated medical and psychiatric self-management has shown promising evidence of simultaneously addressing health behaviors that impact co-morbid health conditions [12].
Certified peer specialists emphasized the importance of preventing drug use (n = 66, 24.7%) among people with SMI. Approximately 8% of people have a co-occurring mental health and substance use disorder. Further, people who have a lived experience of SMI are significantly more likely to smoke cigarettes, use illicit drugs, misuse opioids, and binge drink compared to people without SMI [13]. It is important to understand the complexities and interactions of multiple co-morbidities to ensure optimal outcomes. As such, research on “whole health” for people with SMI may advance to integrate mental health, physical health, and substance abuse.
Hope is an important intervention target. Many empirical psychosocial intervention studies examine clinical outcomes, such as symptom reduction or hospitalization rates—not outcomes that are important to consumers. “Hope” can act as a mechanism that impact clinical outcomes. For example, without hope, a person may not engage in a treatment, thus symptom reduction or hospitalization rates will not be impacted. Thus, developing interventions that target the construct of “hope” as an intervention target may prove to be invaluable; however, limited research has been conducted on interventions that address “hope” among people with SMI.
Limitations should be considered in interpreting results. First, the results may involve reporting bias as the online survey was self-report. However, due to the geographic heterogeneity of certified peer specialists, an online survey using a convenience sample methodology is commonly used to reach this population [14, 15]. As such, this method produced qualitative and quantitative data from sample size that is fully-powered for our analysis and also consistent with other national studies of certified peer specialists [14, 15]. As this study provides initial insights into the perspective of certified peer specialists using convenience sample methodology and a non-participatory research approach —future research should include empirically supported participatory research approaches and rigorous methods such as randomized sampling procedures and in-depth qualitative interviewing to explore these initial findings. Second, the sample was majority female with males underrepresented and predominant identified as non-Hispanic White; however, this is the typical make-up of certified peer specialists [15]. In addition, it is important to note that few peer specialists in the sample identified as certified veteran peer specialists (n = 22), while the Veterans Health Administration remains one of the largest employers of peer specialists in the United States; future research should examine the perspectives of certified veteran peer specialists.
Certified peer specialists’ identified important unmet needs of consumers within the context of their own socio-physical environments. Certified peer specialists highlighted unmet needs of people with SMI that have historically been under-researched, yet are of great importance. Initial insights from this study can be used to guide researchers’ efforts to incorporate certified peer specialists perspectives in developing programs to meet the needs of people with SMI. As the movement to include certified peer specialists in the co-production of research in partnership with scientists is gaining momentum [16], future research using participatory research methods such as the Peer Support Specialists-Academic Partnership [17] can further examine these initial insights.
References
Stroul BA: Community support systems for persons with long-term mental illnesses: a conceptual framework. Psychosocial Rehabilitation Journal 1989;12(3):9–26.
National Institutes of Health. The all of us research program announces first community partner awards Available at: http://www.nih.gov/news-events/news-releases/all-us-research-program-announces-first-community-partner-awards. Accessed 10 Jan 2019.
Bason C. Leading public sector innovation: co-creating for a better society. Bristol: Policy Press; 2010.
Creswell J. Qualitative inquiry and research design: choosing among five approaches. 2nd ed. Thousand Oaks: Sage; 2007.
Martin P, Turner B. Grounded theory and organizational research. J Appl Behav Sci. 1986;22:141–57.
Perese E, Wolf M. Combating loneliness among persons with severe mental illness: social network interventions' characteristics, effectiveness, and applicability. Issues Ment Health Nurs. 2005;26:591–609.
Ong A, Rothstein J, Uchino B. Loneliness accentuates age differences in cardiovascular responses to social evaluative threat. Psychol Aging. 2011;27:1.
Institute of medicine (US) division of health promotion and disease prevention. In: Berg RL, Cassells JS, editors. The second fifty years: Promoting health and preventing disability. Washington (DC): National Academies Press (US); 1992.
Badcock J, Shah S, Mackinnon A, et al. Loneliness in psychotic disorders and its association with cognitive function and symptom profile. Schizophr Res. 2015;169:268–73.
Linz S, Sturm BA. The phenomenon of social isolation in the severely mentally ill. Perspect Psychiatr Care. 2013;49:243–54.
Walker E, McGee R, Druss B. Mortality in mental disorders and global disease burden implications: a systematic review and meta-analysis. JAMA Psychiat. 2005;72:334–41.
Druss B, Singh M, von Esenwein S, et al. Peer led self-management of general medical conditions for patients with serious mental illnesses: a randomized trial. Psychiatr Serv. 2018;69:529–35.
Substance Abuse and Mental Health Services Administration. (2018). Key substance use and mental health indicators in the United States: Results from the 2017 National Survey on Drug Use and Health (HHS Publication No. SMA 18–5068, NSDUH Series H-53). Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration. Retrieved from https://www.samhsa.gov/data/. Accessed 10 Jan 2019.
Fortuna K, Aschbrenner K, Lohman M, et al. Smartphone ownership, use, and willingness to use smartphones to provide peer-delivered services: results from a national online survey. Psychiatry Q. 2018;89:947–56.
Salzer M, Schwenk E, Brusilovskiy E. Certified peer specialist roles and activities: results from a national survey. Psychiatr Serv. 2010;61:520–3.
Chinman M, McInnes DK, Eisen S, et al. Establishing a research agenda for understanding the role and impact of mental health peer specialists. Psychiatr Serv. 2017;68:955–7.
Fortuna K, Barr P, Goldstein C, Walker R, Brewer L, Zagaria A, et al. Application of community-engaged research to inform the development and implementation of a peer-delivered mobile health intervention for adults with serious mental illness. J Participat Med. 2019;11(1):e12380. https://doi.org/10.2196/12380.
Funding
This study was funded by the Health Promotion Research Center at Dartmouth, funded by a grant from the United States Centers for Disease Control and Prevention (Cooperative Agreement U48 DP005018). Additional support was received from the National Institute of Mental Health (T32 MH073553–11). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Dr. Muralidharan is supported by VA Rehabilitation Research and Development Career Development Award IK2RX002339.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
All authors declare that he/she has no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Disclosure
The views expressed in this article are those of the authors and do not necessarily reflect the position of policy of the Department of Veterans Affairs or the United States government.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Fortuna, K.L., Ferron, J., Pratt, S.I. et al. Unmet Needs of People with Serious Mental Illness: Perspectives from Certified Peer Specialists. Psychiatr Q 90, 579–586 (2019). https://doi.org/10.1007/s11126-019-09647-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11126-019-09647-y